Abstract
Objectives
Hot flashes and night sweats are the most common and annoying consequences of menopause. The present study aimed to investigate the effect of a combined herbal capsule (black cohosh, soy, potato, chaste tree, and burdock) on hot flashes and night sweats in postmenopausal women.
Methods
The present study was a randomized clinical trial conducted on postmenopausal women who were referred to Hamadan health centers in 2018–2019. The patients were distributed randomly in two groups of 85 individuals using the permuted block technique. The intervention group received the Menohelp capsule 550 mg twice daily for eight weeks and those in the control group received placebo. Data was obtained using a demographic questionnaire and a night sweat checklist one week before and eight weeks after the intervention. Data analysis was done using Stata 13.
Results
Data analysis revealed that means of hot flashes duration, frequency and intensity did not significantly decrease in the postintervention phase as compared to the pre-intervention phase in both the groups (P > 0.05). Comparative analyses of frequency and intensity of night sweats in the two groups revealed that both variables decreased after intervention with the Menohelp capsule (P < 0.05).
Conclusions
This study revealed that combined herbal medicine (Menohelp) was effective in reducing the frequency and intensity of night sweats. Therefore, it can be used to reduce night sweats in postmenopausal women.
Keywords: Herbal medicine, Hot flashes, Postmenopause, Sweat
INTRODUCTION
Menopause is a stage of development in women all of whom experience it at older age; and this phenomenon causes vast changes in women. Menopause, which means the permanent cessation of menstruation occurs at age 51 on average [1]. Every year, 25 million women enter the menopause stage worldwide, and a third of them experience severe symptoms of menopause. Menopausal symptoms include vasomotor symptoms (sweating and hot flashes), decreased physical and mental functioning (fatigue, depression, decreased libido, cardiovascular diseases, and joint and bone disorders), genitourinary symptoms (vaginal dryness and urinary incontinence). Hot flashes and sweating are common symptoms of this period, and more than 88% of women experience them during the menopause [2]. Hot flash is a description of the sudden onset of redness of head, neck and chest skin, which is accompanied by a feeling of intense heat in the body, and sometimes ends in severe sweating. The symptoms are more severe at night causing the night sweats and impaired sleep [3].
The main treatment of hot flashes is the replacement of hormone with estrogen and progesterone in minimum doses and time [4]. Some side effects of hormone replacement therapy are as follows: increased risk of breast cancer, increased risk of thrombophlebitis, increased blood pressure, vaginal bleeding, and gall-bladder diseases, leading to the replacement of nonhormonal treatments by such therapy [5]. Among the alternative medicines, herbs, and among them, the plants with estrogen, are more appropriate therapies [6]. One of these herbal remedies is Menohelp herbal compound which has phytoestrogenic properties. This plant product contains ingredients such as extract of black cohosh (Actaea racemosa L.), burdock (Arctium lappa L.), chaste tree (Vitex agnus-castus), potato (Dioscorea villosa), and soy (Glycine max) that are used to improve symptoms of hot flashes and night sweats in postmenopausal women. One of the ingredients used in the Menohelp is black cohosh. Studies have shown that black cohosh extract, called BNO 1055, prevents the spread of osteoporosis. This extract reduces the main symptoms of menopause in postmenopausal women, similar to estrogen conjugation, and significantly more than placebo [7]. Effective compounds in Menohelp are likely to mimic the nature of neurotransmitters due to their dopaminergic, noradrenergic, serotonergic and GABAergic effects [8]. And this herbal composition includes chlorogenic acid, diosgenin, and agnosid. These evidence strengthen the role of this herbal drug as an alternative for the hormone replacement therapy [9].
Given the high prevalence of hot flashes and the importance of its suitable treatment and the lack of sufficient research in this area, the researcher sought to investigate the effect of Menohelp herbal drug on hot flashes and night sweats as a surrogate for current chemical drugs.
MATERIALS AND METHODS
The present study was a randomized clinical trial conducted in health centers of Hamadan during a year from May 22, 2018 to May 22, 2019. The values required to determine the sample size were calculated using a study by Sadeghi et al. [10] according to the following formula.
The test reliability was 95%, test power was 90%, and amount of loss was 20%. The minimum sample size required in each group was then determined to be 85 samples (a total of 170 samples for both groups).
Inclusion criteria: At least a year after the last menstruation; no acute and chronic diseases approved by the physician; not taking any herbal drugs since 3 months before the intervention; no allergy to herbal medicine; and having or a history of breast or genital cancers.
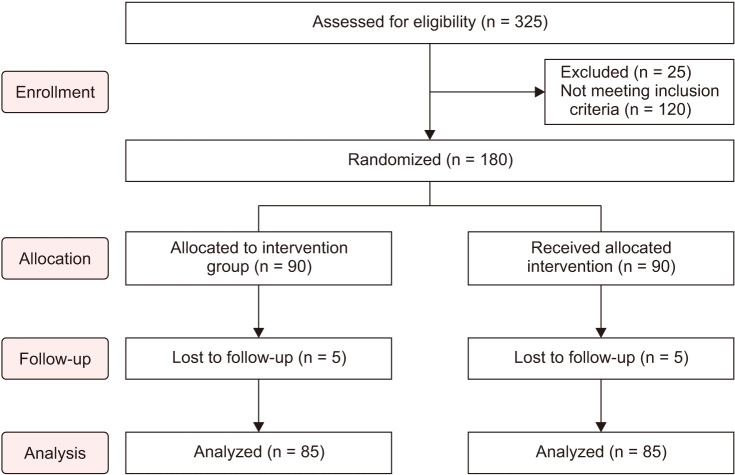
Exclusion criteria: Having acute and chronic diseases during the study; improper use of drugs during the study investigates by the researcher by weekly telephone follow-up. Hamadan was geographically divided into 4 districts after obtaining permission from Hamadan Health Center and the Research Ethics Committee (IR. UMSHA.REC.1396.822) and conducting the necessary coordination. Two health centers were randomly selected from each of north, south, east and west districts using the draws; and 8 health centers were selected. Then, the menopausal list of these centers was obtained, and allocation sequences were determined using 4th randomized blocking (Fig. 1). The sequences of individuals were assigned to two groups of 85 people (Menohelp, placebo). It should be noted that each participant was then given a closed packet based on the sequence containing either Menohelp or placebo. After describing the mentioned aims and the proposed method for women that included the inclusion criteria, they were asked to participate in the written consent study.
Fig. 1. The process of selecting samples.
Eligible individuals who were willing to participate in the study were invited to participate in the study and visit the health center on a specific day and time. The present study was single-blind, performed by the researcher who gave the medication to women and was not aware of types of medication. The demographic questionnaire was researcher-made; and the researcher completed the hot flashes and night sweats questionnaire. Wiklund Vasomotor Symptom Subscale score was used to measure hot flashes and night sweats. It check duration, intensity and frequency of hot flashes and night sweats. And it was a tool developed by the U.S. Food and Drug Administration, and was frequently used by Newton et al. [11] and Nahidi et al. [12] in different studies. The reliability of this checklist was confirmed in previous studies. For each hot flash, a sign is recorded in the special column. The intensity of hot flashes is classified into three degrees: 1, mild (sense of heat without sweating); 2, moderate (sense of heat with sweating); and 3, severe (sense of heat with sweating and intervention with normal activities). Women chose a column, depending on the status quo. Duration of hot flashes were less than 30 seconds, 30–60 seconds, 1–3 minutes, 3–5 minutes, and more than 5 minutes and they were evaluated and recorded in quantity. And on this scale, the intensity of night sweats was classified into three degrees of mild (it did not wake you up, but when you wake up for another reason you found your clothes or bed were wet), moderate (it woke you up, but not enough to do anything), severe (it woke you up and you took measure to solve it). The form was given to the volunteers to complete in case of night sweats in the morning and after night sleep. Women were asked to complete the checklist form a week before the intervention. The participants were treated with medication for 8 weeks. The intervention was as the consumption of the Menohelp capsule (550 mg) twice daily. This drug has been developed and manufactured by Barij Essence Pharmaceutical Co. (Kashan, Iran). Forty milligrams of total phenolic content (TPC) in terms of daidzein and at least 3 mg of diosgenin were available in each Menohelp capsule. The placebo capsule was made by the Faculty of Pharmacy and similar to the Menohelp that was given to eligible participants twice daily. Correct drug use was monitored weekly by phone. In addition, the researcher's phone number was given to samples in order to be contacted with the researcher. The comparative results were statistically analyzed at the end of 8 weeks.
Independent t test was used to compare quantitative and demographic variables with normal distribution; and Mann–Whitney test was used to compare quantitative variables with abnormal distribution. The chi-square and the Fisher's exact tests were also used to compare the categorized variables in groups. Analysis of data relating to the main outcome of the study was performed by the ANOVA/ANCOVA; and the back-transformation was utilized to report averages. The Stata 13 was used to analyze research data (StataCorp LLC, College Station, TX, USA). Significance level was considered to be 0.05 in all tests.
RESULTS
The participants' mean age was 55.86 ± 5.22 years (mean ± standard deviation) in the placebo group, and 54.70 ± 4.78 years in the Menohelp capsule group; and the difference was not statistically significant (P = 0.13). The mean age of onset of menopause was 48.59 ± 5.28 years in the Menohelp capsule group; and 50.08 ± 4.76 years in the placebo group. The mean duration of menopause was also higher in the placebo group than the intervention group, but the difference was not statistically significant (P > 0.05). The majority of people in both groups had primary school education and more than 90% were housewives. Comparison of the body mass index status among three groups indicated almost a half of participants were overweight, and there was no significant difference between two groups. There was no significant difference between the groups in terms of chronic underlying disease (P > 0.05) (Table 1).
Table 1. Baseline characteristics of study patients.
| Variable | Menohelp group | Placebo group | Test statistics | P value | |
|---|---|---|---|---|---|
| Age (y) | 54.70 ± 4.78 | 55.86 ± 5.22 | −1.51 | 0.13a | |
| Age of onset of menopause (y) | 48.59 ± 5.28 | 50.08 ± 4.76 | −1.07 | 0.28b | |
| Duration of menopause (y) | 6.04 ± 5.90 | 6.95 ± 5.02 | −1.63 | 0.10b | |
| Parity | 4.10 ± 1.95 | 4.27 ± 2.18 | −0.54 | 0.59a | |
| Number of children alive | 3.85 ± 1.69 | 3.79 ± 1.83 | 0.22 | 0.82a | |
| Educationd | Illiterate | 16 (18.8) | 14 (16.9) | 0.89 | 0.93c |
| Primary | 34 (40.0) | 33 (39.8) | |||
| High school | 15 (17.6) | 18 (21.7) | |||
| Diploma | 15 (17.6) | 15 (18.1) | |||
| Academic | 5 (5.9) | 3 (3.6) | |||
| Occupationd | Employed | 5 (6.0) | 7 (8.4) | 0.38 | 0.53c |
| Unemployed | 79 (94.0) | 76 (91.6) | |||
| Body mass indexd | Normal | 17 (20.0) | 16 (19.5) | 0.46 | 0.79c |
| Overweight | 49 (57.6) | 44 (53.7) | |||
| Obese | 19 (22.4) | 22 (26.8) | |||
| History of chronic medical illnessd | Yes | 54 (63.5) | 60 (72.3) | 1.47 | 0.22c |
| No | 31 (36.5) | 23 (27.7) | |||
Data are presented as mean ± standard deviation or number (%).
Body mass index categories: Normal, 18.5–24.9 kg/cm2; Overweight, 25–29.9 kg/cm2; Obese, 30 kg/cm2.
aIndependent t test, bMann–Whitney test, cChi-square test.
dThere is included missing data due to some participants did not answer the questions.
The mean score of duration of hot flashes before the intervention was 4.76 in the combined capsule of Menohelp, and 4.61 ± 0.67 in the placebo group. According to the controlled effect of hot flash duration score in the pre-intervention phase, the mean post-intervention hot flash duration was slightly higher in the intervention group than the placebo group, but the difference was not statistically significant. The mean frequencies of hot flashes before the intervention were 7.61 ± 3.78 and 6.93 ± 2.38 in the Menohelp and the placebo group respectively. According to the controlled effect of hot flashes frequencies in the pre-intervention phase, the mean frequency of post-intervention hot flashes was lower in the intervention group than the placebo group, but the difference was not statistically significant. The mean intensities of hot flashes before the intervention were 2.71 ± 0.54 in the Menohelp, and 2.66 ± 0.59 in the placebo group. According to the controlled effect of mean intensity of hot flashes in the pre-intervention phase, the mean of this variable was slightly higher in the intervention group in the post-intervention phase than the placebo group, but the difference was not statistically significant (Table 2).
Table 2. Comparison of duration of hot flashes per minute in the study groups before and after intervention.
| Outcome | Group | Before intervention mean | Adjusted meana | Cohen's d 95% CIb | ANOVA/ANCOVA | |
|---|---|---|---|---|---|---|
| F | P value | |||||
| Duration of hot flashes per minute | Menohelp | 4.76 ± 0.47 | 4.32 ± 2.62 | 0.07 (−0.23 to 0.37) | 1.96 | 0.16 |
| Placebo | 4.61 ± 0.67 | 4.13 ± 2.74 | ||||
| Frequency of hot flashes | Menohelp | 7.61 ± 3.78 | 2.43 ± 3.77 | 0.02 (−0.33 to 0.28) | 0.14 | 0.71 |
| Placebo | 6.93 ± 2.38 | 2.3 ± 4.07 | ||||
| Intensity of hot flashes | Menohelp | 2.71 ± 0.54 | 2.02 ± 1.67 | 0.06 (−0.24 to 0.37) | 0.95 | 0.33 |
| Placebo | 2.66 ± 0.59 | 1.91 ± 1.74 | ||||
Data are presented as mean ± standard deviation.
CI: confidence interval.
aAdjusted for before intervention score. bCohen's d effect size: 0.20–0.40 considered small, 0.50–0.70 considered moderate, 0.80 ≤ considered large.
The comparison of night sweats frequencies indicated that there was no statistical significant difference between both groups in the pre-intervention phase, but the comparison of research groups in terms of frequencies of night sweats at the post-intervention stage indicated that 18.7% of individuals, who consumed Menohelp, reported no night sweats, but about 40% of individuals in the placebo group reported high night sweats during a week. These differences were statistically significant (P < 0.001). The Menohelp was more effective in reducing the frequency of sweats than the placebo (Table 3).
Table 3. Comparison of the number of night sweats before and after the intervention between two groups.
| Evaluation time | Number of night sweats | Menohelp | Placebo | χ2 | P value |
|---|---|---|---|---|---|
| Before intervention | Without | 0 (0) | 1 (1.2) | - | 0.07a |
| Low | 4 (4.4) | 1 (1.2) | |||
| Moderate | 24 (26.4) | 34 (41.0) | |||
| High | 63 (69.2) | 47 (56.6) | |||
| After intervention | Without | 17 (18.7) | 0 (0) | 93.64 | < 0.001 |
| Low | 52 (57.1) | 6 (7.2) | |||
| Moderate | 22 (24.2) | 44 (53.0) | |||
| High | 33 (39.8) | 0 (0) |
Data are presented as number (%).
aFisher's exact test.
The comparison of sweating intensity among the groups showed no significant difference between the groups, but the post-intervention results indicated that 4.4% of individuals in the Menohelp had severe sweating; and about 60% had mild sweating, while, 9.6% of people reported mild sweating in the placebo group. The differences were statistically significant (P < 0.001); hence, the sweating intensity was reduced to a greater extent in a group of Menohelp compared with the placebo group (Table 4).
Table 4. Comparison of the intensity of night sweats before and after the intervention between two groups.
| Evaluation time | Intensity of night sweats | Menohelp | Placebo | χ2 | P value |
|---|---|---|---|---|---|
| Before intervention | Mild | 10 (11.0) | 10 (12.0) | 3.79 | 0.15 |
| Moderate | 53 (58.2) | 58 (69.9) | |||
| Severe | 28 (30.8) | 15 (18.1) | |||
| After intervention | Mild | 54 (59.3) | 8 (9.6) | 48.07 | < 0.001 |
| Moderate | 33 (36.3) | 60 (72.3) | |||
| Severe | 4 (4.4) | 15 (18.1) |
Data are presented as number (%).
Results of Table 5 indicated that there was no statistical significant difference between the two groups in terms of intensity of sleep disorder in the pre-intervention phase. After the intervention, the highest frequency belonged to the group of “no disorder” (57.1%) and the lowest frequency belonged to the severe sleep disorder (3.3%) in the group of Menohelp. Instead, only 6% of individuals in the placebo group had no sleep disorder within a week, and more than a half of them had mild sleep disorder, and the differences were statistically significant (P < 0.001).
Table 5. Comparison of severity of sleep disorder with night sweats before and after the intervention between two groups.
| Evaluation time | Severity of sleep disorder | Menohelp | Placebo | χ2 | P value |
|---|---|---|---|---|---|
| Before intervention | Without | 16 (17.6) | 9 (10.8) | 20.04 | 0.56 |
| Mild | 6 (6.6) | 8 (9.6) | |||
| Moderate | 40 (44.0) | 40 (48.2) | |||
| Severe | 29 (31.9) | 26 (31.3) | |||
| After intervention | Without | 52 (57.1) | 5 (6.0) | 53.16 | < 0.001 |
| Mild | 26 (28.6) | 45 (54.2) | |||
| Moderate | 10 (11.0) | 20 (24.1) | |||
| Severe | 3 (3.3) | 13 (15.7) |
Data are presented as number (%).
DISCUSSION
In our study, the combined Menohelp capsule (black cohosh, soy, potato, chaste tree, and burdock) was not more effective in reducing symptoms of hot flashes because of amount of consumption dose or frequency and method of drug use, but it was more effective in improving symptoms of night sweats than placebo. Despite a few number of studies on the comparison of the herbs, some studies have examined the effectiveness of the plants. Findings of a systematic review study by Kashani et al. [13], who examined herbal medicine affecting hot flashes in 59 studies, indicated that soy, Oenothera, and black cohosh were effective in reducing symptoms of hot flashes in postmenopausal women, but there were no significant differences between herbs and placebo in some studies. They also stated that the definitive effects of these herbs on the improvement of hot flashes were still unclear, and there was a need for closer scrutiny [13]. In a study by Tanmahasamut et al. [14] among postmenopausal women, they concluded that there was no significant difference in the reduction of severity and frequency of hot flashes after treatment with black cohosh. In a double-blind clinical trial study by Geller et al. [15], they evaluated the effects of black cohosh and red clover compared to placebo on relieving the menopausal vasomotor symptoms. Their study indicated that black cohosh and red clover had no effect on vasomotor symptoms compared to the placebo [15]. Saghafi et al. [16] also indicated that black cohosh and fluoxetine were both effective in treating sleep disorder, night sweats, and depression in postmenopausal women. In their study, the mean score of Menopause Rating Scale (MRS) after treatment decreased in both groups under the treatment with Black cohosh and fluoxetine compared to the beginning of study, but the difference was not significant between two groups [16]. And the results of these studies are in line with the results of our study. But in some studies the results are in contrast to ours. Shahnazi et al. [7], who compared black cohosh with placebo group, indicated that the daily consumption of black cohosh could be used as an alternative to the treatment of hot flushes. It might be due to the use of herbal medicine in our study. In a systematic review and meta-analysis study, was conducted by Heydari et al. [17] concluded that soybeans are effective on reducing the severity and frequency of hot flashes. They also found that drugs containing phytoestrogens could be a good choice in the treatment of menopausal hot flashes [17].
In a systematic review study by Karimian and Keramat [18], they investigated some herbs that affected hot flashes in the Iranian herbal medicine through a review of 27 studies. Their results also indicated that among the studied herbal compounds, there were numerous papers with high validity on the good effectiveness of soybean and it seemed that soybeans could be used to treat hot flashes in postmenopausal women [18]. And Masoumi et al. [19] used black cohosh in their study for 8 weeks to treat menopausal hot flashes. They found that after four weeks of drug use, the severity of vasomotor symptoms decreased [19]. Side effects were also significantly lower in the black cohosh group than the Fluoxetine group [16].
Furthermore, results of a study by Azimipour et al. [20] indicated that the consumption of black cohosh by postmenopausal women for 8 weeks had a significant effect on reducing sleep disorder, night sweats severity, and palpitations compared to the control group; and it could be used as an herbal medicine in reducing menopausal symptoms [20]. In study of Imhof et al. [21] to evaluate the effect of soy germ extract in the treatment of hot flashes and sweating in postmenopausal women, it was concluded that soy germ extract has moderate effect but statistically significant on the treatment of menopausal vasomotor symptoms.
The reason for the inconsistency of the results of other studies with our study may be due to the following reasons:
1. Our study is the first study to have used a phytoestrogenic compound of 5 herbs (black cohosh, burdock, chaste tree, potato, and soy).
2. As with many studies, we used the 550 mg capsule as one capsule daily. But two capsules a day can also be taken.
Totally, the herbal drug that is to be used as an alternative for hormone replacement therapy should lack estrogenic effects on breast and uterine tissues, but have beneficial effects on menopause symptoms and on the bones. Herbal estrogens have no or little effect on menopause symptoms in low doses, and in higher doses mimic the effects of estrogen. However, further studies are needed to identify the effects of this drug and other phytoestrogenic herbal remedies at different therapeutic doses in reducing menopausal vasomotor symptoms. Therefore, researchers aim for finding other herbal compounds. Menohelp capsule is one of these compounds.
In conclusion, results of the present study indicated that herbal combined capsules (black cohosh, soy, potato, and burdock) were effective in decreasing the frequency and severity of night sweats, but they had no effect on relieving symptoms of hot flashes. Therefore, recommending this herbal medicine may help alleviate some of symptoms associated with the menopause.
ACKNOWLEDGMENTS
This study with the ethical code of IR.UMSHA. REC.1396.822 and grant No. 9703011045 and IRCT20120215009014N210, was conducted in Hamadan University of Medical Sciences and sponsored by the respective organization. We really appreciate the contribution of the staff research department of Hamadan University of Medical Sciences and all those who helped achieving this goal.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Taylor HS, Fritz MA, Pal L, Seli E. Speroff's clinical gynecologic endocrinology and infertility. Philadelphia: Lippincott Williams & Wilkins; 2019. [Google Scholar]
- 2.Miller VM, Kling JM, Files JA, Joyner MJ, Kapoor E, Moyer AM, et al. What's in a name: are menopausal “hot flashes” a symptom of menopause or a manifestation of neurovascular dysregulation. Menopause. 2018;25:700–703. doi: 10.1097/GME.0000000000001065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berek JS. Berek and Novak's gynecology. Philadelphia: Lippincott Williams & Wilkins; 2019. [Google Scholar]
- 4.Sanchez CK, Rumbellow S. Hormone replacement therapy for menopausal symptoms. US Pharm. 2018;43:21–26. [Google Scholar]
- 5.Shakeri F, Taavoni S, Goushegir A, Haghani H. Effectiveness of red clover in alleviating menopausal symptoms: a 12-week randomized, controlled trial. Climacteric. 2015;18:568–573. doi: 10.3109/13697137.2014.999660. [DOI] [PubMed] [Google Scholar]
- 6.Shabanian S, Bahmani M, Asadi-Samani M. The medicinal plants effective on female hormones: a review of the native medicinal plants of Iran effective on estrogen, progesterone, and prolactin. J Chem Pharm Sci. 2016;9:1270–1276. [Google Scholar]
- 7.Shahnazi M, Nahaee J, Mohammad-Alizadeh-Charandabi S, Bayatipayan S. Effect of black cohosh (Cimicifuga racemosa) on vasomotor symptoms in postmenopausal women: a randomized clinical trial. J Caring Sci. 2013;2:105–113. doi: 10.5681/jcs.2013.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen LR, Ko NY, Chen KH. Isoflavone supplements for menopausal women: a systematic review. Nutrients. 2019;11:2649. doi: 10.3390/nu11112649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Вуттке B, Зайдлова-Вуттке Д. Black cohosh (Cimicifuga racemosa) is a non-estrogenic alternative to hormone replacement therapy. Reprod Endocrinol. 2019;(46):72–81. [Google Scholar]
- 10.Sadeghi A, Bakhshi M, Behboodi Z, Goodarzi S, Haghani H. Effect of sage extract on hot flashes in postmenopausal women. Complement Med J Fac Nurs Midwifery. 2013;2:324–335. [Google Scholar]
- 11.Newton KM, Reed SD, LaCroix AZ, Grothaus LC, Ehrlich K, Guiltinan J. Treatment of vasomotor symptoms of menopause with black cohosh, multibotanicals, soy, hormone therapy, or placebo: a randomized trial. Ann Intern Med. 2006;145:869–879. doi: 10.7326/0003-4819-145-12-200612190-00003. [DOI] [PubMed] [Google Scholar]
- 12.Nahidi F, Zare E, Mojab F, Alavi-Majd H. Effects of licorice on relief and recurrence of menopausal hot flashes. Iran J Pharm Res. 2012;11:541–548. [PMC free article] [PubMed] [Google Scholar]
- 13.Kashani L, Khajuei Kermani F, Akhondzadeh S. The efficacy of herbal medicines for treatment of hot flash: a systematic review. J Med Plants. 2017;16:1–20. [Google Scholar]
- 14.Tanmahasamut P, Vichinsartvichai P, Rattanachaiyanont M, Techatraisak K, Dangrat C, Sardod P. Cimicifuga racemosa extract for relieving menopausal symptoms: a randomized controlled trial. Climacteric. 2015;18:79–85. doi: 10.3109/13697137.2014.933410. [DOI] [PubMed] [Google Scholar]
- 15.Geller SE, Shulman LP, van Breemen RB, Banuvar S, Zhou Y, Epstein G, et al. Safety and efficacy of black cohosh and red clover for the management of vasomotor symptoms: a randomized controlled trial. Menopause. 2009;16:1156–1166. doi: 10.1097/gme.0b013e3181ace49b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saghafi N, Mahmoodinya M, Ayati S, Behdani F, Shakeri MT, Rakhshandeh A. Comparison of effects of black cohosh and fluoxetine in treatment of menopausal symptoms. Iran J Obstet Gynecol Infertil. 2012;15:1–7. [Google Scholar]
- 17.Heydari L, Suhrabi Z, Sayehmiri F, Sayehmiri K. Effect of herbaceous medicines effective in hot flashes of menopause women: a systematic review and meta-analysis in Iran. Iran J Obstet Gynecol Infertil. 2014;17:16–25. [Google Scholar]
- 18.Karimian Z, Keramat A. sHot flashes of menopause and herbal medicine in Iran: a systematic review. Iran J Obstet Gynecol Infertil. 2014;17:1–11. [Google Scholar]
- 19.Masoumi SZ, Shayan A, Ahmadinia H, Moradkhani S, Farhadian M, Ebrahimi R, et al. A comparative study on the effect of black cohosh and salvia on hot flashes in postmenopausal women. Iran J Obstet Gynecol Infertil. 2019;22:1–12. [Google Scholar]
- 20.Azimipour A, Loripoor M, Sadeghi T. The effect of black cohosh (Cimicifuga racemosa) on menopausal symptoms: a randomized clinical trial. J Rafsanjan Univ Med Sci. 2017;16:715–726. [Google Scholar]
- 21.Imhof M, Gocan A, Imhof M, Schmidt M. Soy germ extract alleviates menopausal hot flushes: placebo-controlled double-blind trial. Eur J Clin Nutr. 2018;72:961–970. doi: 10.1038/s41430-018-0173-3. [DOI] [PMC free article] [PubMed] [Google Scholar]