Abstract
Background
Rates of fatal overdose (OD) from synthetic opioids rose nearly 60 % from 2016 to 2018. 911 Good Samaritan Laws (GSLs) are an evidenced-based strategy for preventing OD fatality. This study describes patrol officers’ knowledge of their state’s GSL, experience with OD response, and their perspectives on strategies to prevent and respond to opioid OD.
Methods
An electronic survey assessed officers’ knowledge of state GSLs and experiences responding to OD. Descriptive statistics and hierarchical linear modeling were generated to examine differences in knowledge, preparedness, and endorsement of OD response efforts by experience with OD response.
Results
2,829 officers responded to the survey. Among those who had responded to an OD call in the past six months (n = 1,946), 37 % reported administering naloxone on scene and 36 % reported making an arrest. Most (91 %) correctly reported whether their state had a GSL in effect. Only 26 % correctly reported whether that law provides limited immunity from arrest. Fifteen percent of officers who had responded to an OD work in departments that do not carry naloxone. Compared with officers who had not responded to any OD calls, those who reported responding OD calls at least monthly and at least weekly, were significantly less likely to endorse OD response efforts.
Conclusion
Officers who respond to OD calls are generally receiving training and naloxone supplies to respond, but knowledge gaps and additional training needs persist. Additional training and strategies to relieve compassion fatigue among those who have more experience with OD response efforts may be indicated.
Keywords: Opioids, Overdose, Police, Naloxone, Good Samaritan Law, Compassion fatigue
1. Background
The U.S. opioid overdose (OD) epidemic is still escalating. Between 2016 and 2018, the age-adjusted rate of fatal OD from synthetic opioids other than methadone grew from 6.2 to 9.9 deaths per 100,000 people (Hedegaard et al., 2020). Today, emerging evidence indicates that OD rates are surging further amidst the COVID-19 pandemic (American Medical Association, 2020). 911 Good Samaritan Laws (GSLs) are an evidenced-based strategy for decreasing the number of unintentional ODs resulting in death (Carroll et al., 2018a; McClellan et al., 2018; Nguyen and Parker, 2018). Though the precise content of GSL legislation varies from state to state, such laws generally provide limited immunity from arrest, charges, or prosecution for drug possession for those experiencing or calling first responders to the scene of an OD (Prescription Drug Abuse Policy System, 2018). The purpose of these laws is to counteract fear of arrest, loss of parole, or other forms of police reprisal, which are known barriers to calling 911 during a suspected OD event (Baca and Grant, 2007; Deonarine et al., 2016; Tobin et al., 2005). Alongside the establishment of GSLs across the U.S., standing orders for naloxone (Prescription Drug Abuse Policy System, 2019), a life-saving drug that reverses the effect of opioid OD, have been widely established, creating the legal framework for lay-persons to obtain, carry and administer naloxone to others when witnessing a suspected OD (Lambdin et al., 2018; Meyerson et al., 2018). Law enforcement officers and other non-medical first responders are among those who have increased access to naloxone under those standing orders (Davis et al., 2015; Kitch and Portela, 2016).
Quantitative evaluations of structured training sessions on OD response for law enforcement officers in the U.S. states of Connecticut and Rhode Island have demonstrated that such training can effectively equip first responders with the skills and knowledge needed to apply these new fatal OD prevention strategies when responding to calls for service (Saucier et al., 2016). However, qualitative assessments have highlighted the emotional burden of implementing these new strategies (often resulting in compassion fatigue or “burnout”) among law enforcement (Bessen et al., 2019) as well as growing concern among first responders that such strategies may enable riskier substance use (Saunders et al., 2019).
To our knowledge, only two studies to date have conducted cross-sectional evaluations of law enforcement knowledge of and experiences with GSLs and their implementation (Banta-Green et al., 2013; Green et al., 2013), both of which were conducted in a limited geographic area (in Seattle, Washington, and in the state of Rhode Island, respectively). The purpose of this study is (1) to assess, across multiple states, the extent to which officers who respond to calls for service correctly understand their state’s GSL and (2) to describe officers’ experiences with and perspectives on evidence-based OD prevention strategies when responding to opioid OD calls in their respective jurisdictions.
2. Methods
2.1. Data collection
High Intensity Drug Trafficking Areas (HIDTAs) are law enforcement initiatives funded by the U.S. Office of National Drug Control Policy that operate in regions implicated in narcotics trafficking. HIDTAs are designated to dismantle and disrupt such illicit drug markets (National HIDTA Assistance Center, 2019). In September and October 2017, representatives of eight HIDTAs operating in 20 states approached law enforcement leaders in HIDTA-designated counties to distribute an electronic survey to officers who respond to calls for service in their departments. In most states, only one department was approached by HIDTA staff for participation in the survey, producing a non-representative, convenience sample.
The survey tool (Supplement 1) captured officers’ knowledge of, perspectives about, and experience with OD response and state GSLs. The survey was anonymous; names, IP addresses, and other potentially identifying information were not collected. Surveys were self-administered and conducted online. Officers received an invitation to participate in the survey via email, which supplied a general web-link to all potential participants. The survey instrument and resulting data was collected and maintained at the National HIDTA Assistance Center.
Analysis of this HIDTA-owned data for this study was determined to be exempt from review by the Institutional Review Board at Elon University (Elon, NC).
2.2. Measurements
2.2.1. Demographics
Specific demographic information collected in surveys was limited to sex, age range (in 10-year increments), state of employment, type of jurisdiction (city, town, village, county, or state), years of experience in public safety (less than 10, 10–20, or more than 20), and whether their department carries naloxone.
2.2.2. Experience with OD response
Survey respondents indicated how many times in the past 6 months they responded to the scene of an OD. This variable was operationalized first as dichotomous, indicating whether the officer had or had not responded to an OD call for service in the past 6 months. It was secondarily operationalized as a categorical variable, indicating the frequency of OD response in the past six months (none, less than monthly, 1–4 times/month, and weekly or more). Dichotomous (yes/no) variables for experience with naloxone administration and arrest of an OD survivor or bystander at the scene were also created based on responses to these questions: “How many times in the past six months have you administered naloxone (also called Narcan) on the job to a victim at the scene of an OD?” and “Of all the suspected OD calls you have responded to in the past six months, how many resulted the arrest of an OD victim or witness for any offense?”
2.2.3. Personal Experience with OD
Officers were asked, separately, whether they know anyone personally, outside of their duty as a law enforcement officer, who has experienced an opioid use disorder (OUD) or who has experienced an OD (yes/no).
2.2.4. Knowledge of GSL
Officers were further asked whether their state has a GSL and, if so, whether the provisions of that law offer OD survivors and bystanders limited protections from (1) arrest or (2) criminal charges. Responses were compared with characteristics of state GSLs at the time the survey was administered (The Network for Public Health Law, 2019).
2.2.5. Training
Receipt of training was assessed using the yes/no question: “Have you received training in the past two years on how to respond to suspected opioid ODs?” Respondents were also asked if training in any of the following areas would be useful: 1) identifying and responding to opioid ODs; 2) the safe handling of opioids or other illicit substances; 3) the clinical science and psychology of OUD; 4) effective treatments for OUD; 5) their state’s GSL; and 6) services for people with addiction and their families.
2.2.6. Perceptions of OD prevention strategies
Participants were asked to respond on a 4-point Likert scale (strongly agree, agree, disagree, strongly disagree) to five statements designed to capture endorsement of OD response efforts: 1) “911 Good Samaritan Laws save lives”; 2) “Programs that train and distribute naloxone to lay community members to treat OD save lives”; 3) “911 Good Samaritan Laws may encourage more opioid use by sending the message that drug use is OK”; 4) “Programs that train and distribute naloxone to lay community members may encourage opioid use by sending the message that drug use is OK”; and 5) “Training community members how to identify and respond to an OD may send the message that opioid drug use is OK.”
To explore possible associations between these attitudes and other characteristics of knowledge or behavior, the last three items capturing negative perspectives towards OD response efforts were reverse coded and summed with the remaining items to create an endorsement of OD response efforts scale and modeled as a continuous variable (range 0−15). Though not a validated endorsement scale, we interpreted a higher score as an indication of greater endorsement of OD response efforts in this exploratory analysis. The Cronbach’s alpha for the endorsement of OD response efforts scale was 0.74, which is higher than the cutoff of 0.70, indicating the items in the scale are adequately correlated and the scale has internal consistency (DiIorio, 2005).
2.3. Analysis
Descriptive statistics were generated for demographic variables and experience responding to OD calls. Participants were stratified according to whether or not they had responded to at least one OD call in the past six months. Chi-squared tests were used to assess differences in knowledge/perspectives measures across these two strata. Of the participants who had responded to at least one OD call, descriptive statistics were produced to indicate the proportion that had administered naloxone and made an arrested of an OD survivor or bystander at the scene.
The final step of the analysis explored differences in officers’ endorsement of OD response efforts knowledge/behavior measures. To account for the nested structure of the data (officers nested within states), a hierarchical linear regression model was constructed. This accounted for some, but not all, of the clustering at the department level. Two-level, random intercepts linear regression models using the PROC GLIMMIX SAS procedure were fitted in which states were treated as clusters and the endorsement of OD response efforts scale was modeled as a continuous dependent variable. Both the categorical and dichotomous OD response variables, along with the knowledge and perspective variables, were modeled as independent variables in individual models. The variables for the multilevel analysis were reasonably complete as less than 2% of data were missing. Therefore, missing data were eliminated in the multilevel analysis. All analyses were conducted in SAS v9.4 (Cary, North Carolina).
3. Findings
Below, we present the following findings: (1) the study population; (2) rates of naloxone carry and OD response; (3) protocols, training, and field experience responding to OD calls; and (4) attitudes toward OD prevention strategies.
3.1. Study population
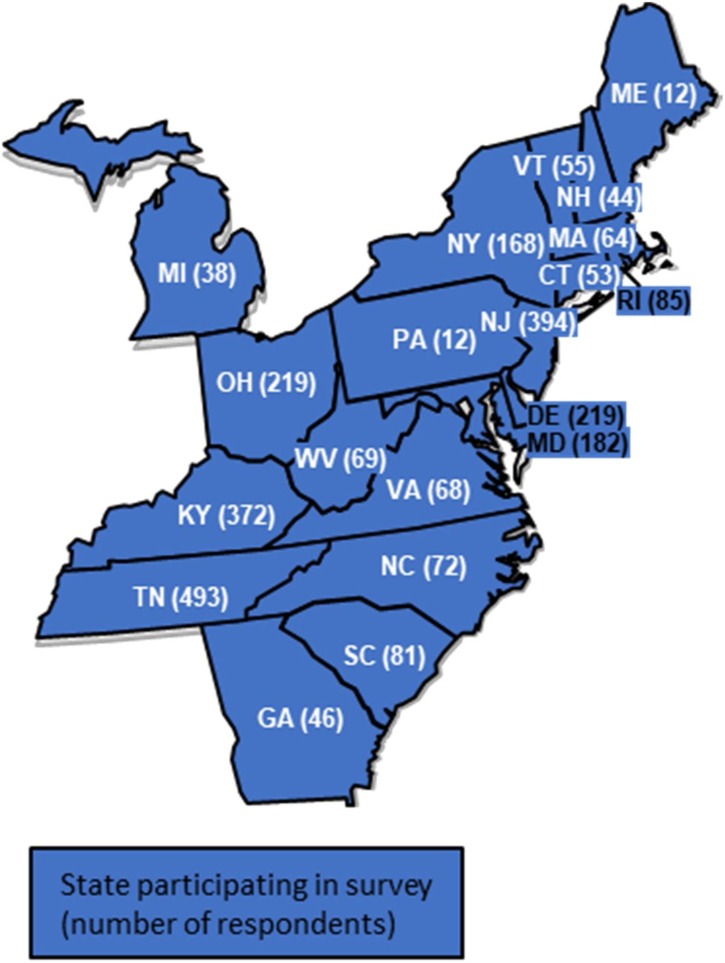
A total of 2,994 individuals responded to the survey. Of these, 102 were identified through free-text responses as ineligible for this study (i.e. a respondent wrote “n/a this question doesn’t apply to me, because I am an administrator” in text boxes for clarify “other” responses) and were excluded. The remaining 2829 (94 %) were identified as sworn officers who respond to calls for service in 20 states (Fig. 1 ) and included in this analysis. The included respondents were overwhelmingly male (90 %), and most (65 %) were 35 years or older (Table 1 ). Approximately twice as many participants reported working in a city department (39 %) than in a state (18 %), county (23 %), or town/village (20 %) department.
Fig. 1.
Number of patrol officer responses to a Good Samaritan Law survey by state, 2017 (N = 2,829).
Table 1.
Characteristics of patrol officers responding to a GSL survey, 2017 (N = 2,829).
| Total sample (n = 2829) |
||
|---|---|---|
| N | % | |
| Gender | ||
| Male | 2371 | (90.02) |
| Female | 263 | (9.98) |
| Age | ||
| Under 35 | 955 | (34.90) |
| 35−44 | 912 | (33.33) |
| 45 or older | 869 | (31.76) |
| Jurisdiction | ||
| Town/Village | 552 | (19.82) |
| City | 1095 | (39.32) |
| County | 630 | (22.62) |
| State | 508 | (18.24) |
| Size of Department | ||
| 99 or fewer officers | 1048 | (37.56) |
| 100−499 officers | 619 | (22.19) |
| 500 or more officers | 1123 | (40.25) |
| Years in public safety | ||
| Less than 10 | 980 | (34.64) |
| 10−20 years | 1165 | (41.18) |
| 20+ years | 684 | (24.18) |
| Working in department that carries naloxone | 2087 | (76.95) |
| Knows state has GSL | 2462 | (90.51) |
| Received OD response training in past 2 years | 2339 | (83.93) |
| Identified at least one area where additional training would be useful | 1847 | (65.29) |
| Has responded to an OD in the past 6 months | ||
| Yes | 1974 | (72.28) |
| Administered naloxone at the scene of an OD in the past 6 months | 715 | (36.80) |
| Arrested at least one individual who experienced a non-fatal OD or witnessed an OD and called 9-1-1at the scene of that OD in past 6 months | 463 | (35.75) |
GSL: Good Samaritan Law; OD: Overdose.
Columns may not sum to total due to missing values.
3.2. Naloxone carry and OD response
Most participants reported working in a department in which officers who respond to calls for service carry naloxone (77 %) and reported knowing whether their state had enacted a GSL (91 %) (Table 1). Most participants had responded to at least one OD in the past 6 months (73 %) and had received training on OD response within the past two years (84 %). More than half (63 %) responded that additional training in at least one area related to OUD, OD, or OD response efforts would be useful to them.
3.3. Protocols, training, and field experience among officers who respond to OD
Among only those officers who had responded to at least one OD in the past 6 months (n = 1974), approximately one-third (37 %) reported administering naloxone at least once during that time (Table 1). Of these same officers, 36 % reported making at least one arrest for any reason at the scene of an OD in the past 6 months.
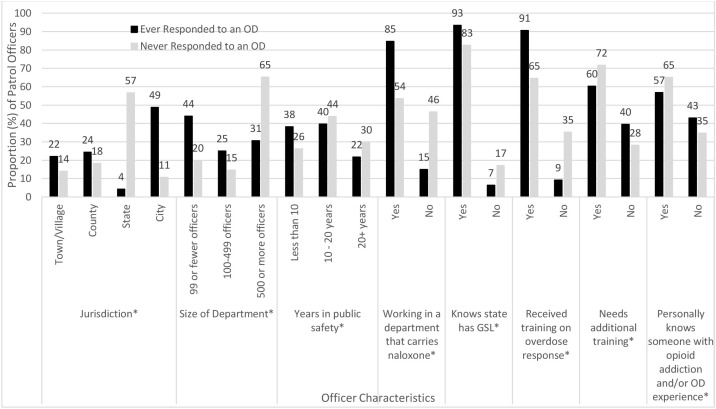
A majority of all participating officers reported receiving training on OD identification and response within the past two years (84 %). In chi-squared analysis (Fig. 2 ), reported training was significantly more common among officers who had responded to at least one OD in past 6 months than among those who had not (91 % vs. 65 %, respectively). Officers who had responded to an OD were also significantly more likely than those who had not to report working in a department where officers regularly carry naloxone (85 % vs. 54 %, respectively).
Fig. 2.
Characteristics of patrol officers responding to a Good Samaritan Law survey, by experience with OD response in past six months, 2017 (N = 2,829).
GSL: Good Samaritan Law; OD: Overdose.
*Indicates significant (p < 0.5) difference (using chi-square test) by ever/never responded to OD in the past 6 months.
The majority of all officers reported knowing someone personally, outside of their role as a first responder, who is living with a OUD and/or who has experienced an OD (57 % of officers who had responded to an OD vs 65 % of those who had not). This difference was statistically significant (Fig. 2).
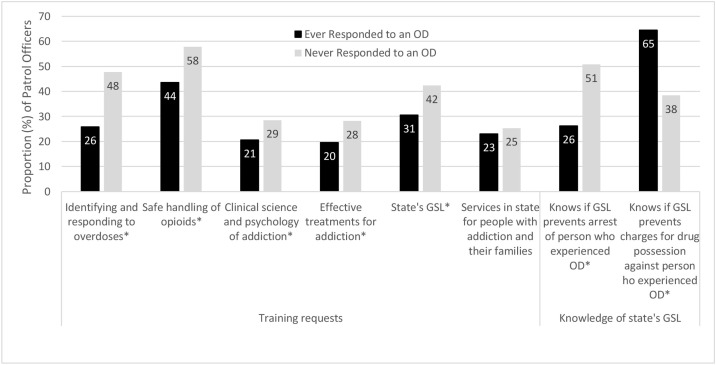
Most officers reported that some form of additional training in at least one area related to addiction, OD, or OD response efforts would be useful to them. Such reports were significantly less common among officers who had responded to an OD compared with those who had not (60 % vs. 72 %, respectively) (Fig. 2). The training domains most commonly identified as useful by officers who had responded to an OD were: the safe handling of opioids (44 %); their state’s 911 GSL (31 %); and identifying and responding to OD (26 %) (Fig. 3 ).
Fig. 3.
Training requests and knowledge of state’s GSL among patrol officers who responded to an OD call in the past 6 months, a GSL survey, 2017 (N = 1,974).
GSL: Good Samaritan Law; OD: Overdose.
*Indicates significant (p < 0.5) difference (using chi-square test) by ever/never not responded to OD in the past 6 months.
Officers who had responded to at least one OD in the past 6 months were statistically more likely than those who had not responded to correctly identify whether their state had enacted a GSL (93 % vs. 83 %, respectively) (Fig. 2). Of those who had responded to an OD, about a quarter (26 %) correctly knew whether their state’s law protects individuals who survived or witnessed the OD and called 911 from arrest, compared to about half (51 %) of officers who had not responded. Conversely, two-thirds (65 %) of officers who had responded correctly knew whether the law similarly protects OD survivors and bystanders from drug-related charges, compared to 38 % of officers who had not responded (Fig. 3).
3.4. Perspectives on OD response strategies reported by patrol officers who respond to OD
Individual responses of agreement or disagreement to statements about OD prevention and response strategies were mixed. Specifically, a minority of participants reported exclusively positive (27 %) or exclusively negative (11 %) perspectives on OD response strategies (data not shown in figures). The average score on the endorsement of OD response efforts scale was 7.62 (interquartile range 6–10; data not shown in figures).
In regression analysis, officers who had made an arrest at the scene of an OD in the past 6 months, who work in a department where officers responding to service calls carry naloxone, and who had received no training on OD response in the past 6 months had lower scores of endorsement, on average, but these differences were not statistically significant (Table 2 ). Significantly lower scores on average were observed among officers who did not know whether their state had enacted a GSL, who did not indicate a need for additional training, and who had responded to at least one OD in the past 6 months.
Table 2.
Estimated average score on endorsement of OD response efforts scale and 95 % confidence intervals (CI) for by patrol officer characteristics, based on hierarchical linear regression models, a GSL survey, 2017 (N = 2731).
| Characteristic | Average Score on Endorsement of OD Response Efforts Scale (Range 0−15) | (95 % CI) | p-value |
|---|---|---|---|
| Ever responded to an OD in the past 6 months* | |||
| Yes | 7.47 | (7.12, 7.82) | <0.01 |
| No | 8.40 | (7.53, 8.38) | |
| Made arrest at scene of OD | |||
| Yes | 7.33 | (6.90, 7.78) | 0.14 |
| No | 7.59 | (7.19, 7.99) | |
| Working in department that carries naloxone | |||
| Yes | 7.50 | (7.13, 7.87) | 0.17 |
| No | 7.72 | (7.29, 8.15) | |
| Knows state has GSL | |||
| Yes | 7.60 | (7.24, 7.97) | <0.05 |
| No | 7.19 | (6.69, 7.69) | |
| Received training on OD response | |||
| Yes | 7.58 | (7.21, 7.95) | 0.36 |
| No | 7.43 | (6.89, 7.88) | |
| Needs additional training | |||
| Yes | 7.87 | (7.53, 8.21) | <0.01 |
| No | 6.90 | (6.60, 7.34) | |
OD: Overdose; GSL: Good Samaritan Law.
Score of endorsement of OD response efforts scale created by summing all items in scale. Average scores created using hierarchical linear regression models with states treated as clusters, patrol officer characteristics treated as categorical dependent variables, and endorsement of OD response efforts scale modeled as continuous independent variable.
Dichotomous version of responded to OD variable.
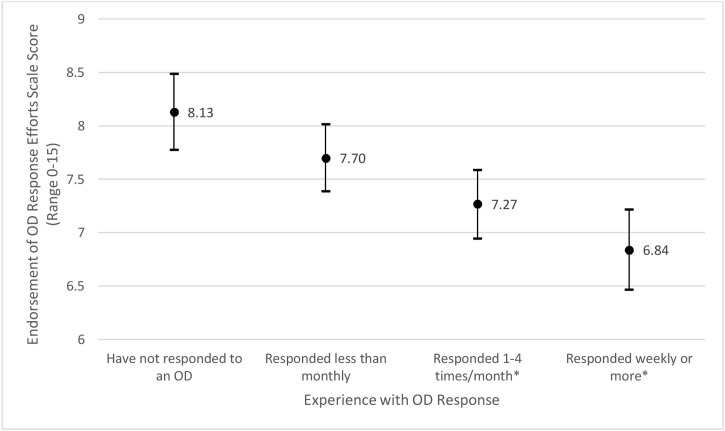
Upon further analysis, the composite endorsement score decreased on average as reported frequency of opioid OD response increased (see Fig. 4 ). Specifically, compared with officers who never responded to an OD call (average scale score of 8.13, 95 %; CI: 7.78–8.49), those who reported responding to 1–4 OD calls per month (average scale score of 7.27, 95 %; CI: 6.95–7.59) and who reported responding to OD calls at least weekly (more than 4 times per month; average scale score of 6.84, 95 %; CI: 6.47–7.22) showed significantly lower composite scores, indicating relatively negative perspectives of OD response strategies in comparison with their counterparts who had not responded to an OD.
Fig. 4.
Estimated average score on endorsement of OD response efforts scale, by history of OD response^ in past six months, based on a hierarchical linear regression model, a Good Samaritan Law survey, 2017 (N = 2,731).
OD: Overdose.
Dots represent point estimates. Bars represent 95 % confidence intervals.
^Categorical version of responded to OD variable.
*Indicates significantly different (p < 0.05) from no response to OD using hierarchical linear regression model with states treated as clusters, history of OD response treated as categorical dependent variable, and endorsement of OD response efforts scale modeled as continuous independent variable.
4. Discussion
This study represents, to the best of our knowledge, the largest survey of law enforcement officers about OD prevention and response strategies to date, as well as the only study to recruit officers who respond to calls for service from across a multiple regions in the U.S. Survey data indicate that the vast majority of officers who respond to OD calls with any degree of regularity are receiving training and are working in departments where some or all officers responding to calls for service are equipped with naloxone. Nevertheless, a minority of officers report ever administering naloxone. Though naloxone access for first responders has generally expanded (Davis and Carr, 2015), 15 % of those who responded to OD calls in this study reported working in a department where naloxone is not regularly carried on patrol. This study did not evaluate barriers to the implementation of this strategy. Future research can explore the prevalence of such barriers, feasible strategies for surmounting those barriers, and the potential public health impacts of doing so.
Though most officers who participated in this survey correctly identified whether their state had enacted a GSL at the time of data collection, nearly one in ten officers (including one in fifteen of those who had ever responded to an OD) responded incorrectly. Further, a minority (26 %) of officers who had responded to at least one OD call in the past 6 months correctly reported whether their state’s GSL afforded OD survivors and bystanders limited protection from arrest. Importantly, this error reflected some officers’ underestimation of the law’s protections (i.e. the GSL protects from arrest, but the officer reported it did not) and others’ overestimation of the law (i.e. the GSL does not protect from arrest, but the officer reported it does).
Troublingly, more than one-third of officers who had responded to OD reported making an arrest at the scene of an OD in the past six months. Current research shows that fear of police harassment is known to deter bystanders from calling 911 (Koester et al., 2017; Latimore and Bergstein, 2017) and that any concern about arrest at the scene of an OD reduces the likelihood that a bystander will call 911 (Baca and Grant, 2007; Deonarine et al., 2016). Therefore, any arrest at the scene of an OD, whether occurring legally and on procedurally valid grounds or as a result of the misapplication of a state GSL, could seriously undermine the public health benefits of the law.
Previous studies have demonstrated the efficacy of various strategies for training law enforcement officers to effectively identify and respond to OD events (Saucier et al., 2016; Wagner et al., 2016). However, the finding that officers who had responded to at least one OD in the past 6 months were less likely to report the need for further training on these topics may indicate the need for more thorough evaluation of knowledge gaps and the adaptation of standardized training strategies to better meet local needs. Future research should explore patterns of over- or under-estimation of the protections provided by these laws by responding officers and how those mis-estimations may affect officer behavior or other outcomes related to OD calls. Also worthy of further investigation is how didactic learning gained from formal training and experiential learning gained from on-the-job experience responding to OD calls may influence, support, or contradict one another.
A notable finding from this study is that higher frequencies of OD response are associated with lower scores on the endorsement of OD response efforts scale. GSLs and enhanced naloxone access are well-studied interventions. Their efficacy at increasing access to care and reducing rates of fatal OD is clearly established in peer reviewed literature (Carroll et al., 2018a; McClellan et al., 2018; Nguyen and Parker, 2018; Rando et al., 2015). Our finding that officers’ experiences in the field may reduce faith in these strategies does not contradict the evidence base supporting their implementation. It does, however, suggest that whatever positive outcomes are reaped by a stronger focus on these evidence-based strategies may not necessarily be perceived by the officers crucial to implementing them. The practical implications of this finding are myriad. Future research should investigate how officers’ perceptions of OD response strategies may influence substance use-related stigma as well as officers’ implementation of GSL laws and discretionary behaviors (i.e. checking for warrants, collecting cellphone data) at the scene.
There may be reason to interpret officers’ lower endorsement of OD response efforts as a sign of professional burnout and compassion fatigue. First and foremost, the endorsement of experiences such as “sense of hopelessness working with clients,” “feel like a ‘failure’ in work,” and “sense of worthlessness associated with work” have been validated as indicators of compassion fatigue in studies in other professional and cultural contexts (Adams et al., 2006; Sun et al., 2016). Low scores on our exploratory endorsement scale may be indicators of these same symptoms of compassion fatigue implicitly manifesting in responses to the somewhat similar yet differently worded prompts.
Another factor which may explain first responders’ negative perspectives on OD response strategies is the perceived failure of those “second responder” systems (i.e. healthcare, treatment, recovery support, social support, etc.) to respond effectively to opioid use in their communities. National data from 2018 indicated that only 42 % of substance use treatment facilities offered medications for OUD (U.S. Substance Abuse and Mental Health Services Administration, 2019). As well, significant waitlists for buprenorphine providers continue to block access to such medications across the U.S. (Carroll et al., 2018b; Fox et al., 2015; Parran et al., 2017). Given these ongoing challenges in the larger healthcare system, it is reasonable to hypothesize that first responders are recognizing (and emotionally responding to) the population effects of insufficient treatment capacity in their own line of work.
Similarly, this study found that patrol officers who have responded to an OD in the past 6 months are significantly more likely to personally know someone who has experienced OUD or an opioid OD. One interpretation of this finding is simply that working and residing in a region more severely impacted by the opioid OD epidemic increases the likelihood that an officer will encounter OUD and OD in both their professional and their personal lives. If so, officers who reside in severely impacted regions may be affected by numerous social and structural factors, as is the case with other service professionals who experience repeated exposure to trauma (Adams et al., 2006; Figley, 2002). These regional factors may also shape officers’ perspectives on the OD response efforts that they are asked to undertake in their professional roles (Andersen and Papazoglou, 2015; Burnett and Wahl, 2015). Future research can explore this hypothesis. Regardless, efforts to support mental health, improve job quality, and combat compassion fatigue among first responders should recognize the myriad environmental drivers of grief that exist across multiple spheres of first responders’ lives (Schwab et al., 2016).
The findings of this study should be interpreted with certain limitations in mind. The dataset analyzed here was originally collected for program improvement purposes with a convenience sample of law enforcement agencies already known to participating HIDTAs. Survey responses provided by officers here may reflect trends in HIDTA-designated counties, which represent approximately 20 % of U.S. counties and 67 % of the U.S. population, thus limiting their generalizability to counties that are not HIDTA-designated (National HIDTA Assistance Center, 2019). The true response rate for this survey is unknown; consequently, response bias in the study population may not have been detected. Neither the departments from which officers were recruited nor the participating officers themselves may be representative of all departments or all patrol officers in their region. Since respondents were nested by state, and not identified by department, there may be systematic variation at the department level for which we could not account. Further, this study was implemented with a cross-sectional design; thus, causal relationships cannot be definitively determined. As the sampling strategy used here generated responses that cannot be taken as representative of each individual state, it is not possible to undertake a deeper analysis of the effect of location on the outcomes of interest than is presented here. Future studies can examine the role played by state and local policy environments as well as local culture in contributing to outcomes related to OD reversal and compassion fatigue.
5. Conclusions
In this cohort of officers who participated in a HIDTA-led survey designed for program improvement, those officers who had responded to at least one OD call in the past 6 months had, generally, received training and naloxone supplies. Nevertheless, important knowledge gaps (both measured and perceived) concerning state policy and OD response continue to exist. Further, overall endorsement of OD prevention and response strategies appears to decline as professional exposure to the impacts of opioid use increases. These findings suggest that additional officer training and the implementation of strategies to promote resilience and minimize compassion fatigue may be indicated. Ongoing efforts to address the opioid OD epidemic more broadly could also lessen the burden carried by first responders.
Desclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Role of funding source
No funding was received to support this study.
Author disclosures
Each author contributed to the submission in the following manner. Study Concept: JC, SM, JW, RN, JK, TG Data Management: PM, MP Statistical Analysis: SM Interpretation of data: JC, SM, JW, JK, RK, TG Initial drafting of manuscript: JC, SM Editing/revision of manuscript: JC, SM, JW, RK, JW, PM, MC, TG.
All authors have made significant contributions to this manuscript and have approved this version for submission.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgements
None.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.drugalcdep.2020.108257.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Adams R.E., Boscarino J.A., Figley C.R. Compassion fatigue and psychological distress among social workers: a validation study. Am. J. Orthopsychiatry. 2006;76:103–108. doi: 10.1037/0002-9432.76.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Medical Association . 2020. Issue Brief: Reports of Increases in Opioid-Related Overdose and Other Concerns During COVID Pandemic. [Google Scholar]
- Andersen J.P., Papazoglou K. Compassion fatigue and compassion satisfaction among police officers: an understidied topic. Int. J. Emerg. Ment. Health Hum. Resil. 2015;17:661–663. doi: 10.4172/1522-4821.1000259. [DOI] [Google Scholar]
- Baca C.T., Grant K.J. What heroin users tell us about overdose. J. Addict. Dis. 2007;26:63–68. doi: 10.1300/J069v26n04_08. [DOI] [PubMed] [Google Scholar]
- Banta-Green C.J., Beletsky L., Schoeppe J.A., Coffin P.O., Kuszler P.C. Police officers’ and paramedics’ experiences with overdose and their knowledge and opinions of Washington State’s drug overdose-naloxone-Good Samaritan law. J. Urban Health Bull. N. Y. Acad. Med. 2013;90:1102–1111. doi: 10.1007/s11524-013-9814-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bessen S., Metcalf S.A., Saunders E.C., Moore S.K., Meier A., McLeman B., Walsh O., Marsch L.A. Barriers to naloxone use and acceptance among opioid users, first responders, and emergency department providers in New Hampshire, USA. Int. J. Drug Policy. 2019;74:144–151. doi: 10.1016/j.drugpo.2019.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnett H.J.J., Wahl K. 2015. The Compassion Fatigue and Resilience Conection: a Survey of Reslilience, Compassion Fatigue, Burnour, and Compassion Satisfacton Among Trauma Responders. [Google Scholar]
- Carroll J.J., Green T.C., Noonan R.K. 2018. Evidence-Based Strategies for Prevention Opioid Overdose: What’s Working in the United States. [Google Scholar]
- Carroll J.J., Rich J.D., Green T.C. The more things change: Buprenorphine/naloxone diversion continues while treatment remains inaccessible. J. Addict. Med. 2018;12:459–465. doi: 10.1097/ADM.0000000000000436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis C.S., Carr D. Legal changes to increase access to naloxone for opioid overdose reversal in the United States. Drug Alcohol Depend. 2015;157:112–120. doi: 10.1016/j.drugalcdep.2015.10.013. [DOI] [PubMed] [Google Scholar]
- Davis C.S., Carr D., Southwell J.K., Beletsky L. Engaging law enforcement in overdose reversal initiatives: authorization and liability for naloxone administration. Am. J. Public Health. 2015;105:1530–1537. doi: 10.2105/AJPH.2015.302638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deonarine A., Amlani A., Ambrose G., Buxton J.A. Qualitative assessment of take-home naloxone program participant and law enforcement interactions in British Columbia. Harm Reduct. J. 2016;13 doi: 10.1186/s12954-016-0106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiIorio C.K. John Wiley & Sons; 2005. Measurement in Health Behavior: Methods for Research and Evaluation. [Google Scholar]
- Figley C.R. Compassion fatigue: psychotherapists’ chronic lack of self care. J. Clin. Psychol. 2002;58:1433–1441. doi: 10.1002/jclp.10090. [DOI] [PubMed] [Google Scholar]
- Fox A.D., Chamberlain A., Sohler N.L., Frost T., Cunningham C.O. Illicit buprenorphine use, interest in and access to buprenorphine treatment among syringe exchange participants. J. Subst. Abuse Treat. 2015;48:112–116. doi: 10.1016/j.jsat.2014.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green T.C., Zaller N., Palacios W.R., Bowman S.E., Ray M., Heimer R., Case P. Law enforcement attitudes toward overdose prevention and response. Drug Alcohol Depend. 2013;133:677–684. doi: 10.1016/j.drugalcdep.2013.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H., Miniño A.M., Warner M. National Center for Health Statistics; Hyattsville, MD: 2020. Drug Overdose Deaths in the United States, 1999-2018 (NCHS Data Brief No. 356) [Google Scholar]
- Kitch B.B., Portela R.C. Effective use of naloxone by law enforcement in response to multiple opioid overdoses. Prehospital Emerg. Care. 2016;20:226–229. doi: 10.3109/10903127.2015.1076097. [DOI] [PubMed] [Google Scholar]
- Koester S., Mueller S.R., Raville L., Langegger S., Binswanger I.A. Why are some people who have received overdose education and naloxone reticent to call Emergency Medical Services in the event of overdose? Int. J. Drug Policy. 2017;48:115–124. doi: 10.1016/j.drugpo.2017.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambdin B.H., Davis C.S., Wheeler E., Tueller S., Kral A.H. Naloxone laws facilitate the establishment of overdose education and naloxone distribution programs in the United States. Drug Alcohol Depend. 2018;188:370–376. doi: 10.1016/j.drugalcdep.2018.04.004. [DOI] [PubMed] [Google Scholar]
- Latimore A.D., Bergstein R.S. “Caught with a body” yet protected by law? Calling 911 for opioid overdose in the context of the Good Samaritan Law. Int. J. Drug Policy. 2017;50:82–89. doi: 10.1016/j.drugpo.2017.09.010. [DOI] [PubMed] [Google Scholar]
- McClellan C., Lambdin B.H., Ali M.M., Mutter R., Davis C.S., Wheeler E., Pemberton M., Kral A.H. Opioid-overdose laws association with opioid use and overdose mortality. Addict. Behav. 2018;86:90–95. doi: 10.1016/j.addbeh.2018.03.014. [DOI] [PubMed] [Google Scholar]
- Meyerson B.E., Agley J.D., Davis A., Jayawardene W., Hoss A., Shannon D.J., Ryder P.T., Ritchie K., Gassman R. Predicting pharmacy naloxone stocking and dispensing following a statewide standing order, Indiana 2016. Drug Alcohol Depend. 2018;188:187–192. doi: 10.1016/j.drugalcdep.2018.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National HIDTA Assistance Center . 2019. High Intensity Drug Trafficking Areas [WWW Document] URL http://www.hidtaprogram.org/ (Accessed 3.5.20) [Google Scholar]
- Nguyen H., Parker B.R. Assessing the effectiveness of New York’s 911 Good Samaritan Law-Evidence from a natural experiment. Int. J. Drug Policy. 2018;58:149–156. doi: 10.1016/j.drugpo.2018.05.013. [DOI] [PubMed] [Google Scholar]
- Parran T.V., Muller J.Z., Chernyak E., Adelman C., Delos Reyes C.M., Rowland D., Kolganov M. Access to and payment for office-based buprenorphine treatment in Ohio. Subst. Abuse Res. Treat. 2017;11:1–6. doi: 10.1177/1178221817699247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prescription Drug Abuse Policy System . 2018. Good Samaritan Overdose Prevention Laws [WWW Document] URL http://pdaps.org/datasets/good-samaritan-overdose-laws-1501695153 (accessed 7.31.20) [Google Scholar]
- Prescription Drug Abuse Policy System . PDAPS; 2019. Naloxone Overdose Prevention Laws [WWW Document] URL http://www.pdaps.org/datasets/laws-regulating-administration-of-naloxone-1501695139 (accessed 12.16.19) [Google Scholar]
- Rando J., Broering D., Olson J.E., Marco C., Evans S.B. Intranasal naloxone administration by police first responders is associated with decreased opioid overdose deaths. Am. J. Emerg. Med. 2015;33:1201–1204. doi: 10.1016/j.ajem.2015.05.022. [DOI] [PubMed] [Google Scholar]
- Saucier C.D., Zaller N., Macmadu A., Green T.C. An Initial evaluation of law enforcement overdose training in Rhode Island. Drug Alcohol Depend. 2016;162:211–218. doi: 10.1016/j.drugalcdep.2016.03.011. [DOI] [PubMed] [Google Scholar]
- Saunders E., Metcalf S.A., Walsh O., Moore S.K., Meier A., McLeman B., Auty S., Bessen S., Marsch L.A. “You can see those concentric rings going out”: emergency personnel’s experiences treating overdose and perspectives on policy-level responses to the opioid crisis in New Hampshire. Drug Alcohol Depend. 2019;204 doi: 10.1016/j.drugalcdep.2019.107555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwab D., Napolitano N., Chevalier K., Pettorini-D’Amico S. Hidden grief and lasting emotions in emergency department nurses. Creat. Nurs. 2016;22:249–253. doi: 10.1891/1078-4535.22.4.249. [DOI] [PubMed] [Google Scholar]
- Sun B., Hu M., Yu S., Jiang Y., Lou B. Validation of the Compassion Fatigue Short Scale among Chinese medical workers and firefighters: a cross-sectional study. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2016-011279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Network for Public Health Law . The Network; 2019. Drug Overdose Prevention and Harm Reduction [WWW Document] URL https://www.networkforphl.org/resources/topics__resources/drug_overdose_prevention_and_harm_reduction/ (accessed 12.17.19) [Google Scholar]
- Tobin K.E., Davey M.A., Latkin C.A. Calling emergency medical services during drug overdose: an examination of individual, social and setting correlates. Addict. Abingdon Engl. 2005;100:397–404. doi: 10.1111/j.1360-0443.2005.00975.x. [DOI] [PubMed] [Google Scholar]
- U.S. Substance Abuse and Mental Health Services Administration . U.S. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2019. National Survey of Substance Abuse Treatment Services (N-SSATS): 2018: Data on Substance Abuse Facilities. [Google Scholar]
- Wagner K.D., Bovet L.J., Haynes B., Joshua A., Davidson P.J. Training law enforcement to respond to opioid overdose with naloxone: impact on knowledge, attitudes, and interactions with community members. Drug Alcohol Depend. 2016;165:22–28. doi: 10.1016/j.drugalcdep.2016.05.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.