Abstract
Background
Supercapsular Percutaneously Assisted total hip arthroplasty (SuperPATH approach) is a relatively new minimal invasive approach which has been associated with encouraging postoperative outcomes. The aim of this study is to compare the minimal invasive (MIS) SuperPATHapproach with the standard modified Hardinge approach at the base of muscle damage due to serum markers, functional results and other perioperative and postoperative data.
Material and methods
Forty eight (48) consecutive patients undergone primary total hip arthroplasty (THA) by the same surgeon (GD), were enrolled in our study. From this study population, the modified Hardinge approach was performed in 23 patients and the SuperPATH approach was performed in 25 patients. Soft tissue impairment was studied based on three representative markers, C-reactive-protein (CRP) and two enzymes, creatine kinase (CK) and lactate dehydrogenase (LDH). We measured these markers 10 min after surgery, on 1st and 2nd postoperative day. The levels of the perceived pain were evaluated according to the Visual Analog Scale/Numerical Rating Scale (VAS/NRS) score which was registered 6 h, 12 h, 1 day and 2 days postoperatively. The functional and clinical evaluation of the patients was achieved with Harris Hip Score (HHS), Charnley's Hip score, EuroQol (EQ-5D)-(EQ-100), Patient Health Questionnaire (PHQ-9) and neuropathic pain questionnaire (DN-4) 6 months and 1 year postoperatively. The rest of the collected data included patient's age, gender, body mass index (BMI), other comorbitities, the American Society of Anesthiologists score (ASA), Charlson Index score, the pre-operative diagnosis, implant positioning through radiographic evaluation, the type of anesthesia, the days of hospitalization, the operating time, incision length, blood loss and blood transfusion requirements and complication rates.
Results
SuperPATH approach was related with statistically considerable lower levels of CRP at 10 min (p = 0,001) and at 24 h (p = 0,047) postoperatively, as well as lower LDH levels in all time points postoperatively. It was also associated with shorter incision length (p < 0.001), longer operating time (p < 0.001), higher mean cup inclination p < 0.001, decreased postoperative pain levels the first 6 and 12 h (p < 0.001) and relatively better clinical and functional results 6 months after surgery, but not at 12 months.
Conclusion
Our study revealed some advantages in favor of the SuperPATH approach comparing with the standard modified Hardinge approach, mainly in terms of less muscle damage and less perceived pain postoperatively. More research is required in order to further elucidate its efficacy.
Keywords: Total hip replacement, Total hip arthroplasty, Minimal invasive surgery, SuperPATH approach, Hardinge approach, Muscle damage, Serum markers
1. Introduction
Total Hip Replacement has become one of the most successful orthopaedic procedures, optimizing patients’ life quality and postoperative mobility.1,2
Ας THA has evolved, approaches according to Minimally Invasive Surgery (MIS) have been applied. These approaches have been initiated as alteration of traditional approaches or they were established as MIS approaches from inception. There are several points worth considering in favor of MIS approaches, such as the small incision and the confinement of soft tissue impairment.3,4 Furthermore, they aim at the reduction of postoperative pain and of blood loss as well as the enhanced postoperative functional results.5, 6, 7 All these advances are regarded as very contributory factors for the acceleration of patients’ recuperation and the final success of THA.8
Nevertheless, opponents of MIS approaches argue that they are related with eventual wrong implementation of femoral stem and acetabular cup, longer operative time, higher blood loss and higher rates of postoperative complications.9, 10, 11, 12
SuperPATH is a relatively new MIS approach consisted by the combination of Superior Capsulotomy described initially by Murphy in 200413 and the percutaneously assisted total hip arthroplasty (PATH) described by Penenberg et al., in 2008.14,15 (Fig. 1).
Fig. 1.
The SuperPATH approach. A: the Superior Capsulotomy approach, and B: the PATH part.
The lateral approach was initially described by McFarland and Osborne16 modified by Bauer17 and Hardinge.18
The measurement of serum and inflammatory markers consists an objective method regarding the evaluation of muscle and soft tissue damage after THA and several humeral mediators have been proposed.19
The aim of this study was to compare SuperPATH and Hardinge approaches in THR patients in terms of muscle damage according to serum markers, clinical, functional and radiological results.
2. Material and Methods
This is a comparative prospective study including 48 patients underwent primary THR by the same surgeon (GD). The SuperPATH approach was applied in 25 patients and the lateral (modified Hardinge) approach in 23 patients.
The study was approved by the Ethics Committee of the University General Hospital of Alexandroupolis (approval number:839/September 13, 2017). Written informed consent was obtained from all patients.
Data collected prospectively and included (a) patients’ demographic concerning age, gender, body mass index (BMI), (b) comorbidities, Charlson Index score,20 the American Society of Anesthiologists score (ASA),21 diagnosis, (c) peri-operative data concerning the type of anesthesia, operating time, incision length, and (d) post-operative data including length of hospital stay (LOS), blood loss22,23 and blood transfusion requirements. Postoperative complications were categorized as major or minor, local or systemic complications.24
2.1. Functional and other scores
Functional and clinical condition of the patients was assessed with Harris hip Score (HHS),25 and Charnley’s Hip score, general health was assessed with EuroQol (EQ-5D)-(EQ-100),26 Patient Health Questionnaire (PHQ-9) which depicts the patients’ depression status and neuropathic pain questionnaire (DN-4). The levels of the perceived pain were specifically evaluated according to the Visual Analog Scale/Numerical Rating Scale (VAS/NRS) score.27
The above mentioned scores and scales were collected pre-operatively, at 6 and 12 months postoperatively. Pain was also registered at 6 h, 12 h, 1 day and 2 days postoperatively.
2.2. Radiographic evaluation
Standard pelvis anteroposterior and lateral radiographs postoperative and at 12 months were studied using the “IMPAX 6.March 5, 3009” software. The cup inclination, the cup anteversion, the stem alignment and the leg length discrepancy were evaluated. Anteversion was estimated as it was described by Gross et al28,29 An ellipse shape was matched to the border of the cup. The proportion between the minor and major axes determined the extent of the cup anteversion. Cup inclination was designated using the angle between the longitudinal axis of the body and the acetabular axis.29,30 Leg length discrepancy was calculated as the difference between the intervals from the teardrop line to the center of the lesser trochanter of each femur.31,32 The stem alignment was assessed using the angle between the axis of the femoral stem and the axis of the femoral shaft.32,33
2.3. Serum and inflammatory markers
In our study, the extent of muscle and soft tissue damage was evaluated with the measurement of three common serum and inflammatory markers.
The first, the C-reactive-protein (CRP) is an acute-phase plasma protein which is primarily produced by liver. Its levels increase in trauma, inflammation or infection.34 The elevation of its levels consists a contributory factor in the host’s immune defense system.35 CRP has a short half-time and its serum concentration depends on the intensity of the stimulus reflecting the rate of synthesis.36 Recently, CRP has been widely used in order to determine the invasiveness of different approaches in THA.19
The second serum marker, the creatinekinase (CK), regulates the cellularATP concentration, because it catalyzses the ATP-dependent phosphorylation of creatine.37,38 Intensive exercise and inherent muscle dysfunction could lead to the increase of CK levels.37 CK has also been used as a serum marker in several studies, investigating soft tissue injury in THA.19
Lastly, lactate dehydrogenase (LDH) is an enzyme that catalyzes the anaerobic alteration of pyruvate to lactate.37,38 Other studies used LDH to determine the invasiveness of the approaches in THA.19 Yet, both CK and LDH have been used extensively as humeral mediators to detect soft tissue damage.39
The serum markers were obtained on routine vein blood samples once preoperatively as a baseline. Thereafter, they were recorded 10 min after surgery, at 1st and 2nd postoperative day.
2.4. Implants
In both approaches the same implants were implanted; uncemented femoral stem Profemur® TL classic femoral stem (Microport, 5677 Airline Road/Arlington, TN 38002), ELEC® ceramic 32 mm diameter femoral head and cementless acetabulum component (OHST Medizinetechnik AG, 14712 Rathenow, Germany)(Fig. 2).
Fig. 2.
Bilateral THA using SuperPATH approach on the right side and Hardinge approach on the left hip.
2.5. Perioperative patient’s management
All patients followed the same fast-track regime.
Pre-operatively Hb was checked at 4 week pre-operatively and patients with anemia were excluded from this study. Patients were instructed and commenced the exercises program preoperatively and in continuity.
Intra-operatively transamine 2 gr diluted in 100 ml normal saline was used topically in all patients and local infiltration of Ropivacaine 1% (maximum dose 3 mg/kgr). Regarding postoperative antibiotic prophylaxis, cefoxitine 2 gr was administered every 6 h for 24 h. No drains were used.
Peri-operative multimodal analgesia included pregabaline 75 mg every 12 h starting the night before the operation and continued postoperatively, paracetamol 1 gr every 6 h and parecoxib 40 mg when the patients perceived the increase of the pain levels. Opioids were used as rescue analgesia.
Patients were mobilized out of bed next morning continuing the exercise program that they were instructed preoperatively under the supervision of a physiotherapist. They were discharged home as soon as they fulfilled the same discharged criteria.
2.6. SuperPATH description
A skin incision approximately 9 cm was performed, starting from great trochanter and extended proximally (Fig. 3.1). The superior part of hip joint capsule was exposed. A capsulotomy parallel to the skin incision was performed between the base of the greater trochanter and the acetabular edge (Fig. 3.2).
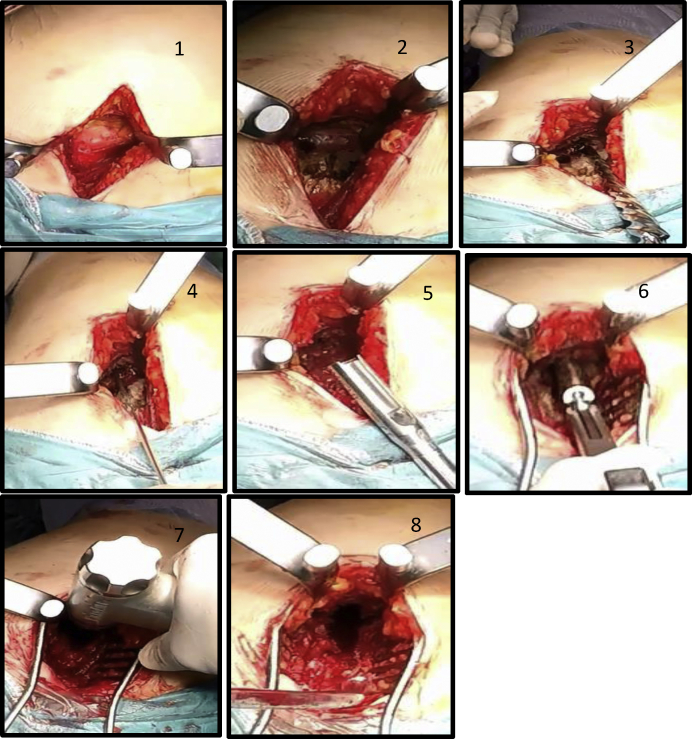
Fig. 3.
Supercapsular approach: 1. Skin incision 2. Superior part of hip joint capsule - capsulotomy 3. A reamer was used to create the initial canal 4. A canal feeler was placed in the bone lumen in order to determine the direction of the canal 5. A cylindrical osteotome was used to form the canal 6. Successive rasps were inserted into the femur 7. Femoral neck osteotomy 8. The acetabular cavity came into view.
The entry point was the anterior side of the piriformis fossa. A reamer was used to create the initial canal (Fig. 3.3). A canal feeler was placed in the bone lumen in order to determine the direction of the canal (Fig. 3.4). A cylindrical osteotome was used to form the canal (Fig. 3.5). Successive rasps were inserted into the bone until the final configuration of the femur cavity according to the size of the suitable femoral stem (Fig. 3.6). A femoral neck osteotomy was performed in line with the superior aspect of the final rasp-trial stem (Fig. 3.7). The femoral head was extracted after careful manipulations with the assistance of two Schanz pins and the acetabulum came into view (Fig. 3.8).
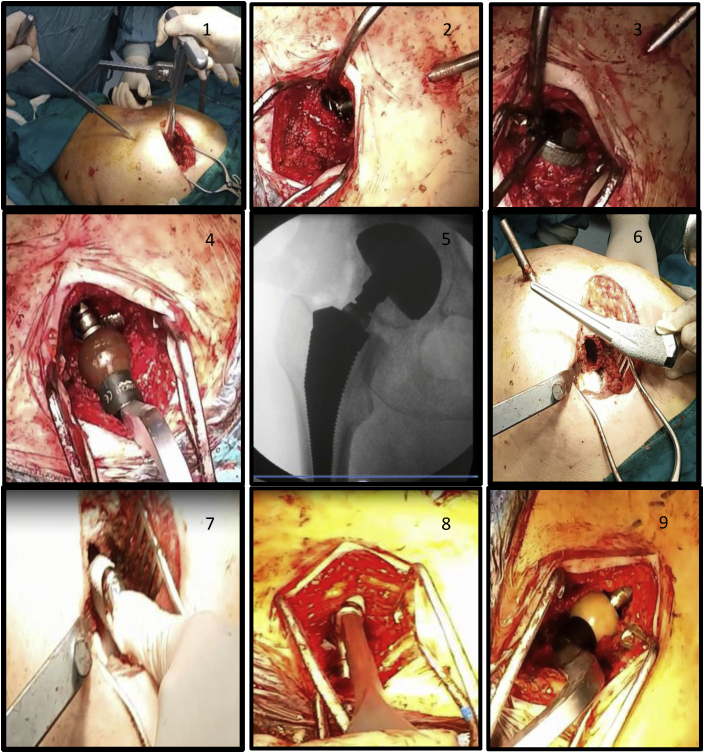
An entryway setting guide was utilized in order to designate the entry point of the reaming tube narrowly to the posterior border of the great trochanter (Fig. 4.1). Consecutive acetabular reamers were located until the suitable formation of the acetabular cavity (Fig. 4.2). The acetabular reamers were conjoined with the reamer guide shaft through the tube. Therefore, the external rotators of the femur remained intact. The final acetabular cup and the polyethylene liner were implanted (Fig. 4.3). A trial head and neck were located and the reduction of the hip joint was accomplished (Fig. 4.4). The patient was undergone X-rays intra-operatively in order to make certain the correct implementation of the components (Fig. 4.5). The final femoral stem and femoral head were inserted and the final reduction of the hip joint was performed (Fig. 4.6–4.9).
Fig. 4.
Percutaneously Assisted Total Hip Arthroplasty (PATH). Technique- Instruments. 1. Entryway setting guide for the acetabular reaming tube 2. Acetabular reaming 3. The final acetabular cup 4. A trial head and neck were located for the reduction of the hip joint 5. Intra-operative radiographic evaluation 6–8. The implementation of the final femoral stem 9. The insertion of the femoral head and the final reduction of the hip joint.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.jor.2020.08.003.
The following is the supplementary data related to this article:
2.7. Statistical analysis
Initially, Kolmogorov-Smirnov test was applied in order to determine the normality of the distribution of continuous data. Normally distributed continuous variables are expressed as mean ± standard deviation while non-normally distributed variables as median and range of Q1 - Q3 quartiles. Categorical variables are shown as absolute and relative (percentage) frequencies. Differences in continuously and normally distributed variables between the two approaches were compared using Student’s t-test, while in non-normally distributed variables were compared with the Mann-Whitney test. Chi-square test and Fisher’s exact test were used to compare differences between categorical variables. Pearson or Spearman correlation coefficients tests were used to identify correlations between continuous variables.
For all tests performed, statistical significance was established at two-sided p value <0.050. Statistical analysis was carried out with the SPSS version 21.0 statistical software package for Windows (IBM – SPSS Inc., USA).
3. Results
3.1. Patients’ characteristics
All the preoperative demographic features of the patients are shown in (Table 1). The two cohorts are well matched in terms of age (p = 0,462), gender (p = 0,703), ASA (p = 0,094), the presence of other comorbitities (p = 0.664) and the preoperative levels of hemoglobin (p = 0,116).
Table 1.
Pre-operative patients’ demographic characteristics in SuperPath and Hardinge groups. The values are given as the mean with the standard deviation ± and the percentage rate in parentheses.
| SuperPath group N (%) | Hardinge group N (%) | P value | |
|---|---|---|---|
| No. of patients | 25 | 23 | |
| Diagnosis | 0.025 | ||
| Osteoarthritis | 20 (80.0) | 9 (39.1) | |
| Dysplasia | 5 (20.0) | 11 (47.8) | |
| Protruzio | 0 (0.0) | 1 (4.3) | |
| Osteonecrosis | 0 (0.0) | 2 (8.7) | |
| Age (years) | 70 ± 7 | 68 ± 8 | 0.462 |
| Gender (female) | 20 (80.0) | 20 (87.0) | 0.703 |
| BMI (kg/m2) | 29.38 ± 4.22 | 32.86 ± 5.00 | 0.012 |
| ASA grade | |||
| I | 6 (24.0) | 1 (4.3) | 0.155 |
| II | 18 (72.0) | 21 (91.3) | |
| III | 1 (4.0) | 1 (4.3) | |
| Charlson Comorbidity Index | |||
| 1 | 21 (84.0) | 23 (100.0) | 0.134 |
| 2 | 3 (12.0) | 0 (0.0) | |
| 3 | 1 (4.0) | 0 (0.0) | |
| Pain score | 3.0 ± 1.5 | 7.0 ± 1.8 | < 0.001 |
| Comorbidities | 0.664 | ||
| Up to 3 | 20 (90.9) | 18 (81.8) | |
| 4 or 5 | 2 (9.1) | 4 (18.2) | |
| Hemoglobin (g/dL) | 13.45 ± 1.2 | 14.0 ± 1.3 | 0.116 |
| Hematocrit | 40.6 ± 3.8 | 42.5 ± 3.5 | 0.089 |
On the other hand, the BMI was significantly higher (p = 0,012), as well as the Charlson Index Score (p = 0,048) in the conventional group.
Finally, there was observed significant difference in the preoperative diagnosis between the two groups (p = 0,015). Specifically, in the SuperPATH group the majority of the impaired hip joints (80%) were diagnosed with osteoarthritis and only (20%) with dysplasia. On the contrary, in the Hardinge group, the majority of the patients were diagnosed with dysplasia (47,8%). Nine patients (39,1%) had hip osteoarthritis, 1 patient (4,3%) was diagnosed with protrusio and two patients (8,6%) had osteonecrosis of the head of the femur.
3.2. Perioperative data
Comparison of the perioperative patients’ data indicated that the MIS SuperPATH approach was related with significantly longer operative time (p < 0,001) and shorter incision length (p < 0,001). Conversely, both cohorts revealed similar rates in terms of the amount of blood loss, postoperative transfusions and the duration of hospitalization. (Table 2, Fig. 5).
Table 2.
Peri-operative patients’ data. NA: Non-available.
| SuperPath group | Hardinge group | P value | |
|---|---|---|---|
| Operation time (min) | 108 ± 25 | 80 ± 13 | < 0.001 |
| Incision length (cm) | 9.44 ± 1.01 | 12.63 ± 1.39 | < 0.001 |
| Blood loss (ml) | 1.0 (0.7–3.1) | 0.9 (0.7–1.6) | 0.765 |
| Blood Volume change (ml ± sd) * | 1.010 ± 0.17 | 1.030 ± 0.21 | 0.803 |
| Length of stay(days)a | 3 ± 1 | 3 ± 1 | 0.852 |
| Anesthesiab | 0.027 | ||
| Spinal | 14 (56.0) | 20 (87.0) | |
| General | 11 (44.0) | 3 (13.0) | |
| Transfusion rateb | 1 (4.0) | 0 (0.0) | NA |
| Complications (yes)b | 1 (4.0) | 1 (4.3) | 1.000 |
| Deep Venous Thrombosis | 1 | 1 |
The values are given as the mean with the standard deviation ±.
The values are given as the mean with the standard deviation the percentage rate in parentheses.
Fig. 5.
Comparison of perioperative data of both approaches. SuperPATH approach was associated with shorter incision and longer operating time. Similar results were recorded between the two cohorts.
Additionally, patients receiving the MIS approach reported considerably lower levels of perceived pain in the first 24 h (Table 3, Fig. 6).
Table 3.
Post-operative levels of perceived pain in patients undergoing Total Hip Arthroplasty via SuperPath or Hardinge approaches.Numerical Rating Score (NRS).
| Time | SuperPath group | Hardinge group | P value | |
|---|---|---|---|---|
| Pain | 6 h | 2.1 ± 1.8 | 4.5 ± 2.1 | < 0.001 |
| 12 h | 2.4 ± 1.8 | 4.7 ± 1.9 | < 0.001 | |
| 24 h | 2.1 ± 0.9 | 3.1 ± 1.7 | 0.004 | |
| 48 h | 1.4 ± 0.9 | 1.6 ± 1.0 | 0.348 |
The values are given as the mean with the standard deviation ±
Fig. 6.
Preoperative and postoperative pain levels according to Visual Analog Scale/Numerical Rating Scale in patients from both cohorts.
One patient of each cohort was diagnosed with deep vein thrombosis (DVT) soon after surgery. Both patients received the appropriate treatment. No cases of deep wound infections or other indications for revisions were recorded.
3.3. Serum and inflammation markers
As stated above, one of our basic goals was the assessment of muscle damage in terms of three specific markers between the two approaches.
SuperPATH approach was related with statistically considerable lower levels of CRP at 10 min (p = 0,001) and at 24 h (p = 0,047) postoperatively. Similarly, patients who underwent the conventional Hardinge approach had significantly increased levels of LDH all times postoperatively than the SuperPATH approach. Conversely, there were recorded no notable discrepancies in terms of CPK levels all times postoperatively between the two approaches (Table 4, Fig. 7).
Table 4.
Perioperative levels of serum markers indicating muscle damage.
| CRP |
CPK |
LDH |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| SuperPath group | Hardinge group | P value | SuperPath group | Hardinge group | P value | SuperPath group | Hardinge group | P value | |
| Pre-operative | 0.48 ± 0.32 | 0.60 ± 0.30 | 0.187 | 88 ± 39 | 95 ± 71 | 0.664 | 201 ± 50 | 235 ± 40 | 0.035 |
| 10-min post-op | 0.42 ± 0.30 | 0.91 ± 0.49 | 0.001 | 180 ± 76 | 173 ± 74 | 0.776 | 204 ± 58 | 236 ± 46 | 0.041 |
| 24-h post-op | 7.20 ± 3.44 | 9.08 ± 2.87 | 0.047 | 649 ± 464 | 827 ± 538 | 0.224 | 193 ± 48 | 263 ± 57 | < 0.001 |
| 48-h post-op | 12.00 ± 5.42 | 14.20 ± 3.83 | 0.115 | 726 ± 499 | 793 ± 409 | 0.613 | 202 ± 35 | 238 ± 65 | 0.044 |
The values are given as the mean with the standard deviation ±
Fig. 7.
Serum markers' fluctuation. CRP levels were statistically significant lower at 10 min and 24 h postoperatively in the SuperPATH approach. Similarly, LDH was considerably higher all time points perioperatively. CPK levels relatively lower 24 and 48 h postoperatively, but without statistical significance.
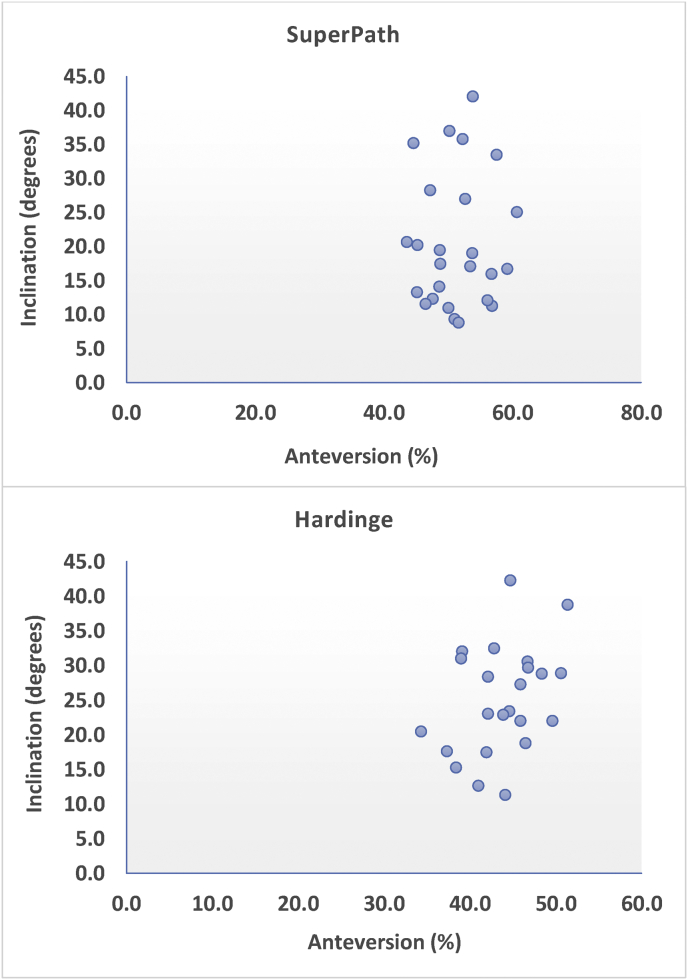
3.4. Radiological results
Radiographic assessment revealed statistically significant smaller average cup inclination in the Hardinge group (43,7°) than in the SuperPATH group (51,2°, p < 0,001). Furthermore, the SuperPATH approach was related with smaller mean cup anteversion (20,5 ± 9,8) compared with Hardinge approach (25 ± 7,9) but without statistically significance (p = 0,086).
For the SuperPATH group, the mean leg length discrepancy was (4,6 ± 3,5) and for the Hardinge group was (3,1 ± 2,5, p = 0,108). The mean stem alignment variance was within accepted limits for both group with similar results (p = 0,986). However, in MIS group the majority of stems were located in varus position (68,2%), as opposed to the conventional group where most of the stems were positioned in valgus site (71,4%). (Table 5, Fig. 8).
Table 5.
Radiologic assessment of the position of the implants.
| SuperPath group | Hardinge group | P value | |
|---|---|---|---|
| X-RAY - cup inclination/degrees | 51.2 ± 4.8 | 43.7 ± 4.4 | < 0.001 |
| X-RAY - cup anteversion (x/y) % | 20.5 ± 9.8 | 25.0 ± 7.9 | 0.086 |
| X-RAY -Leg length discrepancy/mm | 4.6 ± 3.5 | 3.1 ± 2.5 | 0.108 |
| X-RAY - stem degrees | 1.3 ± 0.9 | 1.3 ± 0.8 | 0.986 |
| Stem alignment | 0.009 | ||
| Varus | 15 (68.2) | 6 (28.6) | |
| Valgus | 7 (31.8) | 15 (71.4) |
The values are given as the mean with the standard deviation ± and the percentage rate in parentheses.
Fig. 8.
Scatter plot contrasting the fluctuation of the acetabular components' positioning in both approaches.
3.5. Functional and other scores
The mean HHS at the baseline was higher (51,2 ± 16,5) in the MIS cohort compared with the conventional group (44,2 ± 15,6, p < 0,001). Concerning EQ-5D score, patients in the Hardinge group mentioned considerably worse condition at the categories of self care (p = 0,011) and pain/discomfort (p = 0,013). On the other hand, no significant discrepancies in Chanley's score, EQ-100, DN-4, PHQ-9 were recorded preoperatively between the two groups.
At 6-month follow-up clinical evaluation, distinct better outcomes were registered in Charnley's hip score at the category of walking (p = 0,047) and in EQ-5D at the category of self care (p = 0,03) on behalf of MIS group.
At 1 year follow-up examination the postoperative results were essentially improved accordingly regarding both cohorts. Finally, no statistically noteworthy discrepancies were found concerning all clinical scores. (Table 6).
Table 6.
Comparison of the functional patients’ data.
| SuperPath group | Hardinge group | P value | |
|---|---|---|---|
| Pre-operative | |||
| Harris Hip Score | 51.2 ± 16.5 | 44.2 ± 15.6 | < 0.001 |
| Charnley Score | |||
| Pain | 3 (1–5) | 3 (1–4) | 0.575 |
| Activity | 4 (1–5) | 3 (1–5) | 0.085 |
| Walking | 2 (1–5) | 3 (1–4) | 0.456 |
| EQ-5D-5L | |||
| Mobility | 2 (2–3) | 2 (2–3) | 0.540 |
| Self-care | 2 (1–3) | 2 (1–3) | 0.011 |
| Usual activities | 2 (1–3) | 2 (1–3) | 0.068 |
| Pain/discomfort | 2 (1–3) | 3 (2–3) | 0.013 |
| Anxiety/depression | 2 (1–3) | 2 (1–3) | 0.611 |
| EQ 100 | 66 ± 10 | 66 ± 15 | 0.985 |
| DN4 | 2.6 ± 2.1 | 3.2 ± 2.0 | 0.311 |
| PHQ9 | 3.9 ± 3.8 | 4.9 ± 3.7 | 0.326 |
| 6-month follow-up | |||
| Harris Hip Score | 85.6 ± 10.4 | 81.8 ± 9.3 | 0.192 |
| Charnley's Score | |||
| Pain | 5 (4–6) | 5 (4–6) | 0.161 |
| Activity | 4 (3–6) | 4 (3–5) | 0.189 |
| Walking | 5 (4–6) | 5 (3–6) | 0.047 |
| EQ-5D-5L | |||
| Mobility | 1 (1–3) | 1 (1–3) | 0.438 |
| Self-care | 1 (1–3) | 2 (1–3) | 0.030 |
| Usual activities | 1 (1–3) | 2 (1–3) | 0.281 |
| Pain/discomfort | 2 (1–2) | 1 (1–2) | 0.775 |
| Anxiety/depression | 2 (1–3) | 2 (1–3) | 0.412 |
| EQ 100 | 80 (50–100) | 80 (60–100) | 0.578 |
| DN4 | 1.6 ± 1.6 | 1.5 ± 1.7 | 0.800 |
| PHQ9 | 2.2 ± 3.1 | 2.6 ± 2.2 | 0.642 |
| 1-year follow up | |||
| Harris Hip Score | 92.1 ± 5.5 | 90 ± 4.9 | 0.238 |
| Charnley Score | |||
| Pain | 6 (5–6) | 5 (5–6) | 0.132 |
| Activity | 5 (4–6) | 5 (4–5) | 0.919 |
| Walking | 6 (4–6) | 5 (4–6) | 0.223 |
| EQ-5D-5L | |||
| Mobility | 1 (1–1) | 1 (1–2) | 0.076 |
| Self-care | 1 (1–2) | 1 (1–2) | 0.129 |
| Usual activities | 1 (1–2) | 1 (1–2) | 0.841 |
| Pain/discomfort | 1 (1–2) | 1 (1–2) | 0.352 |
| Anxiety/depression | 2 (1–3) | 2 (1–2) | 0.378 |
| EQ 100 | 80 (70–100) | 80 (60–90) | 0.172 |
| DN4 | 0.7 ± 1.0 | 1.0 ± 1.4 | 0.634 |
| PHQ9 | 1.5 ± 2.2 | 1.7 ± 1.7 | 0.266 |
The values are given as the mean with the standard deviation ±.
Non-normally distributed variables are expressed as median and range of Q1 - Q3 quartiles in parenthesis.
4. Discussion
One of the main features which characterizes each approach is the muscle and soft tissue impairment which can cause, as it is expressed by serum markers. In several studies, MIS approaches are correlated with lower levels of inflammation markers comparing with standard approaches.40, 41, 42 Yet, the interaction of muscle damage and other postoperative results is still debatable.
SuperPATH approach is considered a muscle-sparing approach, because except of a small incision of gluteus maximus, it takes advantage of the interval between gluteus medius and the piriformis to reach the superior hip joint capsule.43
In light of recent literature, the advantages of SuperPATH approach were depicted, as it allows staving off any possible complications after primary THA. Specifically, it is related with low levels of postoperative perceived pain, reduced levels of blood loss, faster rehabilitation and less hospitalization.43, 44, 45, 46, 47
Hardinge approach is deemed an established, traditional approach with efficient postoperative results.48 However, the gluteal deficit, higher rate of generated Trendelenburg sign and inferior postoperative functional outcomes at the early-postoperative period have been recorded as possible drawbacks of this approach.49, 50, 51
4.1. Muscle damage
In our study, we found a definite difference concerning the increase of CRP levels between the two groups. SuperPATH approach was associated with statistically considerable lower levels 10 min and 24 h postoperatively. Similarly, at 48 h postoperatively, we recorded lower levels of CRP in patients who underwent the MIS approach, but the discrepancy was not statistically significant. Respectively, we recorded significantly lower levels of LDH at all times postoperatively regarding SuperPATH approach. Conversely, although the CPK levels were lower at the MIS group 24 h and 48 h postoperatively, this difference was not important in order to underline noteworthy discrepancy in soft tissue impairment between the two cohorts. From our results, we maintain that we can verify our initial assumption and highlight the less invasiveness of the MIS SuperPATHapproach, as it is expressed by serum and inflammatory markers.
Another recent study presented opposite results, because relatively higher CRP, CK and ESR levels were found postoperatively for SuperPATH approach comparing with posterolateral approach.52
Several studies have also recorded muscle and soft tissue damage using CRP, CPK and LDH as serum and inflammatory markers in different approaches for THA.10,53, 54, 55, 56, 57 Some studies recorded the efficacy of MIS approaches, but in some others no differences were registered between MIS and conventional approaches.
4.2. Functional results
We found the SuperPATH approach to be associated with considerable better results at 6 months postoperatively regarding the category of walking in Charnley's hip score and the category of self-care in EQ-5D. Relatively better outcomes were observed in HHS but without statistical significance.
One year after surgery the functional outcomes became quite equivalent for both two cohorts and all patients referred discernible enhancement of their mobility and their life quality. Accordingly, in 2017, Yan T et al. registered greater results regarding HHS for SuperPATH approach shortly after the operation until 3 weeks contrasting with Hardinge approach.58 Furthermore, Jun Xie et al., 2017 observed superior functional results with SuperPATH approach comparing with posterior approach 1 month and 3 months postoperatively.47 On the other hand, Meng W et al., 2020 recorded lower levels of HHS 1 year postoperatively to patients who underwent SuperPATH approach comparing with those who underwent posterolateral approach.52
According to our findings, the functional outcomes seem to have a relative interaction with the invasiveness of the two approaches and the soft tissue injury they cause. Therefore, independently to the contradictory results of the recent literature, our study confirmed to some extent our second hypothesis.
4.3. Perioperative and postoperative data
The mean operative time was significantly higher and the incision length was noticeable shorter regarding the SuperPATH approach. Conversely, there were no significant differences in terms of blood loss and transfusion rates between the two approaches. The operating time was also higher concerning this MIS approach in other studies.52,58 Furthermore, MIS approaches were associated with higher levels of blood loss in several studies.9,10,52,58
The perceived pain levels on VAS scorein the SuperPATH cohort were significantly lower comparing to the Hardinge approach in the first 24 h. Our results are consistent to this particular benefit which has been registered in other studies too.47,58
All patients followed the same physical therapy protocol postoperatively. The requisite time for hospitalization was equal for both groups and all patients reached the discharge criteria approximately the same period after the operation.
Finally, similar complication rates were recorded between the two groups. In 2015, Gofton et al. and colleagues underlined the efficacy of the SuperPATH approach because they reported very low complication rates in terms of dislocation, DVT and periprosthetic fractures and not even one case of infection.46
4.4. Radiographic measurements
Correct implant positioning during THAplays a major role in the final success of the operation.59,60 One of the challenges we encountered was the inadequate visibility of the femur and the acetabulum due to the restricted incision, concerning the MIS approach. Therefore, we included to our intra-operative technique fluoroscopy assessment to make certain the right implant location. According to our findings, the only considerable difference was the higher mean cup inclination approximately 7,5° was recorded in the MIS cohort.
Conversely, in terms of cup anteversion, leg length discrepancy and stem alignment, no significant differences were registered between the two cohorts.
Accordingly, in 2017 by Yan T et al. and colleagues estimated noteworthy greater anteversion angle and leg length discrepancy in patients who underwent the SuperPATHapproach contrasting with those who underwent the standard Hardinge approach.58 Recently, Meng W et al., 2020 recorded also significantly decreased abduction angle of the cup component with SuperPATH approach compared with posterolateral approach.52 Conversely, Jun Xie et al., 2017 and colleagues, found no significant differences in component positioning between the SuperPATH approach and the conventional posterior approach.47
The outcomes of our study should be elucidated carefully taking into consideration some limitations. Initially, this study is not a randomized clinical trial. Furthermore, it includes a small number of the two compared cohorts. Therefore, we cannot be certain about the resemblance of complication rates that we found postoperatively. Third, the follow up examination was performed only at 6 months and 1 year postoperatively regarding functional outcomes and radiographic evaluation. Consequently, according to our study, we cannot support the possible superiority of SuperPATH approach shortly postoperatively or in the long term. In addition, we measured only three common and widely accepted serum markers until the second postoperative day in order to evaluate muscle damage. According to recent literature, the answers of which are the most suitable serum markers or which is the appropriate time to assess them have not been clarified. Therefore, we cannot strongly maintain that we have depicted sufficiently the efficacy of the MIS approach regarding less soft tissue impairment.
The results of our study should be carefully interpreted also in light of the duration of the learning curve of the SuperPATH approach which could explain the longer operating time regarding this approach.
To the best of our knowledge, this is the first comparative study between SuperPATH and Hardinge approaches which incorporated data of muscle damage due to serum markers, clinical and functional postoperative results, radiographic evaluation and other perioperative and postoperative data simultaneously.
5. Conclusion
In our comparatives study, we focused on investigating the efficacy of the MIS SuperPATH approach contrasting with the lateral (modified Hardinge) approach. SuperPATH approach was related with shorter incision, longer operating time, higher mean cup inclination, decreased postoperative pain levels, reduced soft tissue damage as it is expressed by serum and inflammatory markers and to some extent better clinical results 6 months after surgery.
The advantages which emerge from our study may depict the efficacy of the SuperPATH approach compared to the conventional lateral (modified Hardinge) approach in the short-term. The long-term results of this approach remain to be investigated. In future, well-designed comparative studies need to be conducted in order to further highlight the distinct benefits of the SuperPATH approach.
Declaration of competing interest
Authors declare that they have no conflict of interest.
Acknowledgement
The authors have no acknowledgement to mention.
Contributor Information
Stylianos Tottas, Email: stottasdoc@hotmail.com.
Christina Tsigalou, Email: ctsigalo@med.duth.gr.
Athanasios Ververidis, Email: athanasios@ververidis.net.
Ioannis E. Kougioumtzis, Email: siritea@yahoo.gr.
Makrina Karaglani, Email: makrina.karaglani@gmail.com.
Konstantinos Tilkeridis, Email: tilkerorth@gmail.com.
Christos Chatzipapas, Email: hatzy@otenet.gr.
Georgios I. Drosos, Email: drosos@otenet.gr.
References
- 1.Learmonth I.D., Young C., Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370(9597):1508–1519. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 2.Courpied J.P., Caton J.H. 2011. Total Hip Arthroplasty, State of the Art for the 21st Century; pp. 149–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mirza A.J., Lombardi A.V., Jr., Morris M.J., Berend K.R. A mini-anterior approach to the hip for total joint replacement: optimising results: improving hip joint replacement outcomes. Bone Joint J. 2014;96(11_Supple_A):32–35. doi: 10.1302/0301-620X.96B11.34348. [DOI] [PubMed] [Google Scholar]
- 4.Wojciechowski P., Kusz D., Kopeć K., Borowski M. Minimally invasive approaches in total hip arthroplasty. Ortop Traumatol Rehabil. 2007;9(1):1–7. PMID:17605194. [PubMed] [Google Scholar]
- 5.Kennon R., Keggi J., Zatorski L.E., Keggi K.J. Anterior approach for total hip arthroplasty: beyond the minimally invasive technique. JBJS. 2004;86(suppl_2):91–97. doi: 10.2106/00004623-200412002-00013. [DOI] [PubMed] [Google Scholar]
- 6.Matta J.M., Shahrdar C., Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005;441:115–124. doi: 10.1097/01.blo.0000194309.70518.cb. [DOI] [PubMed] [Google Scholar]
- 7.Berend K.R., Lombardi A.V., Jr., Seng B.E., Adams J.B. Enhanced early outcomes with the anterior supine intermuscular approach in primary total hip arthroplasty. JBJS. 2009;91(Supplement_6):107–120. doi: 10.2106/JBJS.I.00525. [DOI] [PubMed] [Google Scholar]
- 8.Smith T.O., Blake V., Hing C.B. Minimally invasive versus conventional exposure for total hip arthroplasty: a systematic review and meta-analysis of clinical and radiological outcomes. Int Orthop. 2011;35(2):173–184. doi: 10.1007/s00264-010-1075-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Landgraeber S., Quitmann H., Güth S. A prospective randomized peri-and post-operative comparison of the minimally invasive anterolateral approach versus the lateral approach. Orthop Rev. 2013;5(3) doi: 10.4081/or.2013.e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pilot P., Kerens B., Draijer W.F. Is minimally invasive surgery less invasive in total hip replacement? A pilot study. Injury. 2006;37:S17–S23. doi: 10.1016/S0020-1383(07)70007-4. [DOI] [PubMed] [Google Scholar]
- 11.Spaans A.J., Hout J.A.V.D., Bolder S.B. High complication rate in the early experience of minimally invasive total hip arthroplasty by the direct anterior approach. Acta Orthop. 2012;83(4):342–346. doi: 10.3109/17453674.2012.711701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Callanan M.C., Jarrett B., Bragdon C.R. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clin Orthop Relat Res. 2011;469(2):319–329. doi: 10.1007/s11999-010-1487-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murphy S.B. Tissue-Preserving, minimally invasive total hip arthroplasty using a superior capsulotomy. In: Hozack W., editor. Minimally Invasive Total Hip and Knee Arthroplaty. Springer-Verlag; 2004. pp. 101–107. Detailed description of the SuperCap technique and clinical rationale. [Google Scholar]
- 14.Penenberg B.L., Bolling W.S., Riley M. Percutaneously assisted total hip arthroplasty (PATH): a preliminary report. J Bone Joint Surg Am. 2008;90(Suppl 4):209–220. doi: 10.2106/JBJS.H.00673. [DOI] [PubMed] [Google Scholar]
- 15.Drosos G.I. Recent evidence in less invasive approaches and less invasive implants in total hip replacement. Recent AdvArthroplast. 2017;1:1–8. [Google Scholar]
- 16.McFarland B., Osborne G. Approach to the hip: a suggested improvement on Kocher's method. J Bone Jt Surg Br Vol. 1954;36(3):364–367. [Google Scholar]
- 17.Bauer R., Kerschbaumer F., Poisel S., Oberthaler W. The transgluteal approach to the hip joint. Arch Orthop Trauma Surg. 1979;95(1-2):47–49. doi: 10.1007/BF00379169. [DOI] [PubMed] [Google Scholar]
- 18.Hardinge K. The direct lateral approach to the hip. J Bone Jt Surg Br Vol. 1982;64(1):17–19. doi: 10.1302/0301-620X.64B1.7068713. [DOI] [PubMed] [Google Scholar]
- 19.Tottas S., Fiska A., Kougioumtzis I., Ververidis A., Tilkeridis K., Drosos G.I. Muscle damage in different approaches in total hip arthroplasty according to serum markers. Open Orthop J. 2019;13(1) doi: 10.2174/1874325001913010097. [DOI] [Google Scholar]
- 20.Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 21.Owens W.D., Felts J.A., Spitznagel E.L., Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49(4):239–243. doi: 10.1097/00000542-197810000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Nadler S.B., Hidalgo J.U., Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51(2):224–232. [PubMed] [Google Scholar]
- 23.Bourke D.L., Smith T.C. Estimating allowable hemodilution. Anesthesiology. J Am Soc Anesthesiol. 1974;41(6):609–611. doi: 10.1097/00000542-197412000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Parvizi J., Mui A., Purtill J.J., Sharkey P.F., Hozack W.J., Rothman R.H. Total joint arthroplasty: when do fatal or near-fatal complications occur? J Bone Jt Surg Am Vol. 2007;89(1):27–32. doi: 10.2106/jbjs.E.01443. [DOI] [PubMed] [Google Scholar]
- 25.Harris W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Jt Surg Am Vol. 1969;51(4):737–755. PMID:5783851. [PubMed] [Google Scholar]
- 26.Brooks R. On behalf of the EuroQol Group. EuroQol: the current state of play. Health Pol. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. PMID:10158943. [DOI] [PubMed] [Google Scholar]
- 27.Chapman C.R., Casey K.L., Dubner R., Foley K.M., Gracely R.H., Reading A.E. Pain measurement: an overview. Pain. 1985;22(1):1–31. doi: 10.1016/0304-3959(85)90145-9. [DOI] [PubMed] [Google Scholar]
- 28.Gross T.P., Liu F., Webb L. Intraoperative radiographs for placing acetabular components in hip resurfacing arthroplasty. Clin Orthop Relat Res. 2011;469(6):1554–1559. doi: 10.1007/s11999-010-1701-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhao H.Y., Kang P.D., Xia Y.Y., Shi X.J., Nie Y., Pei F.X. Comparison of early functional recovery after total hip arthroplasty using a direct anterior or posterolateral approach: a randomized controlled trial. J Arthroplasty. 2017;32(11):3421–3428. doi: 10.1016/j.arth.2017.05.056. [DOI] [PubMed] [Google Scholar]
- 30.Murray D.W. The definition and measurement of acetabular orientation. J Bone Jt Surg Br Vol. 1993;75(2):228–232. doi: 10.1302/0301-620X.75B2.8444942. PMID:8444942. [DOI] [PubMed] [Google Scholar]
- 31.Woolson S.T., Hartford J.M., Sawyer A. Results of a method of leg-length equalization for patients undergoing primary total hip replacement. J Arthroplasty. 1999;14(2):159–164. doi: 10.1016/s0883-5403(99)90119-5. [DOI] [PubMed] [Google Scholar]
- 32.Goosen J.H., Kollen B.J., Castelein R.M., Kuipers B.M., Verheyen C.C. Minimally invasive versus classic procedures in total hip arthroplasty: a double-blind randomized controlled trial. Clin Orthop Relat Res. 2011;469(1):200–208. doi: 10.1007/s11999-010-1331-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Teet J.S., Skinner H.B., Khoury L. The effect of the “mini” incision in total hip arthroplasty on component position. J Arthroplasty. 2006;21(4):503–507. doi: 10.1016/j.arth.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 34.Pepys M.B., Hirschfield G.M. C-reactive protein: a critical update. J Clin Invest. 2003;111(12):1805–1812. doi: 10.1172/JCI18921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Black S., Kushner I., Samols D. C-reactive protein. J Biol Chem. 2004;279(47):48487–48490. doi: 10.1074/jbc.R400025200. [DOI] [PubMed] [Google Scholar]
- 36.Bray C., Bell L.N., Liang H. Erythrocyte sedimentation rate and C-reactive protein measurements and their relevance in clinical medicine. Wis Med J. 2016;115(6):317–321. PMID:29094869. [PubMed] [Google Scholar]
- 37.Brancaccio P., Lippi G., Maffulli N. Biochemical markers of muscular damage. Clin Chem Lab Med. 2010;48(6):757–767. doi: 10.1515/CCLM.2010.179. [DOI] [PubMed] [Google Scholar]
- 38.Spriet L.L., Howlett R.A., Heigenhauser G.J. An enzymatic approach to lactate production in human skeletal muscle during exercise. Med Sci Sports Exerc. 2000;32(4):756–763. doi: 10.1097/00005768-200004000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Kristjansson R.P., Oddsson A., Helgason H. Common and rare variants associating with serum levels of creatine kinase and lactate dehydrogenase. Nat Commun. 2016;7:10572. doi: 10.1038/ncomms10572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mouilhade F., Matsoukis J., Oger P., Mandereau C., Brzakala V., Dujardin F. Component positioning in primary total hip replacement: a prospective comparative study of two anterolateral approaches, minimally invasive versus gluteus medius hemimyotomy. Orthop Traumatol Surg Res. 2011;97(1):14–21. doi: 10.1016/j.otsr.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 41.Kwak S., Chun Y., Rhyu K., Cha J., Cho Y. Quantitative analysis of tissue injury after minimally invasive total hip arthroplasty. Clin Orthop Surg. 2014;6(3):279–284. doi: 10.4055/cios.2014.6.3.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mazoochian F., Weber P., Schramm S., Utzschneider S., Fottner A., Jansson V. Minimally invasive total hip arthroplasty: a randomized controlled prospective trial. Arch Orthop Trauma Surg. 2009;129(12):1633–1639. doi: 10.1007/s00402-009-0870-4. [DOI] [PubMed] [Google Scholar]
- 43.Chow J., Penenberg B., Murphy S. Modified micro-superior percutaneously assisted total hip: early experiences & case reports. Curr Rev Musculoskelet Med. 2011 Sep;4:146–150. doi: 10.1007/s12178-011-9090-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Paul K.D., David A.F., James C. Supercapsular percutaneously-assisted total hip arthroplasty: radiographic outcomes and surgical technique. Ann Transl Med. 2015;3(13):180. doi: 10.3978/j.issn.2305-5839.2015.08.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Michael D.C., Wade G., Lindsey E. Early surgical and functional outcomes comparison of the supercapsular percutaneously-assisted total hip and traditional posterior surgical techniques for total hip arthroplasty: protocol for a randomized, controlled study. Ann Transl Med. 2015;3(21):335. doi: 10.3978/j.issn.2305-5839.2015.12.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gofton W., Chow J., Olsen K.D. Thirty-day readmission rate and discharge status following total hip arthroplasty using the supercapsular percutaneously-assisted total hip surgical technique. Int Orthop. 2015;39(5):847–851. doi: 10.1007/s00264-014-2587-4. [DOI] [PubMed] [Google Scholar]
- 47.Xie J., Zhang H., Wang L., Yao X., Pan Z., Jiang Q. Comparison of supercapsular percutaneously assisted approach total hip versus conventional posterior approach for total hip arthroplasty: a prospective, randomized controlled trial. J Orthop Surg Res. 2017;12(1):138. doi: 10.1186/s13018-017-0636-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Putananon C., Tuchinda H., Arirachakaran A., Wongsak S., Narinsorasak T., Kongtharvonskul J. Comparison of direct anterior, lateral, posterior and posterior-2 approaches in total hip arthroplasty: network meta-analysis. Eur J Orthop Surg Traumatol. 2018;28(2):255–267. doi: 10.1007/s00590-017-2046-1. [DOI] [PubMed] [Google Scholar]
- 49.De Anta-Díaz B., Serralta-Gomis J., Lizaur-Utrilla A., Benavidez E., López-Prats F.A. No differences between direct anterior and lateral approach for primary total hip arthroplasty related to muscle damage or functional outcome. Int Orthop. 2016;40(10):2025–2030. doi: 10.1007/s00264-015-3108-9. [DOI] [PubMed] [Google Scholar]
- 50.Yue C., Kang P., Pei F. Comparison of direct anterior and lateral approaches in total hip arthroplasty: a systematic review and meta-analysis (PRISMA) Medicine. 2015;94(50) doi: 10.1097/MD.0000000000002126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Berstock J.R., Blom A.W., Beswick A.D. A systematic review and meta-analysis of complications following the posterior and lateral surgical approaches to total hip arthroplasty. Ann R Coll Surg Engl. 2015;97(1):11–16. doi: 10.1308/003588414X13946184904008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Meng W., Huang Z., Wang H. Supercapsular percutaneously-assisted total hip (SuperPath) versus posterolateral total hip arthroplasty in bilateral osteonecrosis of the femoral head: a pilot clinical trial. BMC Muscoskel Disord. 2020;21(1):1–9. doi: 10.1186/s12891-019-3023-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhao H.Y., Kang P.D., Xia Y.Y., Shi X.J., Nie Y., Pei F.X. Comparison of early functional recovery after total hip arthroplasty using a direct anterior or posterolateral approach: a randomized controlled trial. J Arthroplasty. 2017;32(11):3421–3428. doi: 10.1016/j.arth.2017.05.056. [DOI] [PubMed] [Google Scholar]
- 54.Mjaaland K.E., Kivle K., Svenningsen S., Pripp A.H., Nordsletten L. Comparison of markers for muscle damage, inflammation, and pain using minimally invasive direct anterior versus direct lateral approach in total hip arthroplasty: a prospective, randomized, controlled trial. J Orthop Res. 2015;33(9):1305–1310. doi: 10.1002/jor.22911. [DOI] [PubMed] [Google Scholar]
- 55.Fink B., Mittelstaedt A., Schulz M.S., Sebena P., Singer J. Comparison of a minimally invasive posterior approach and the standard posterior approach for total hip arthroplasty A prospective and comparative study. J Orthop Surg Res. 2010;5(1):46. doi: 10.1186/1749-799X-5-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dienstknecht T., Lüring C., Tingart M., Grifka J., Sendtner E. Total hip arthroplasty through the mini-incision (Micro-hip) approach versus the standard transgluteal (Bauer) approach: a prospective, randomised study. J Orthop Surg. 2014;22(2):168–172. doi: 10.1177/230949901402200210. [DOI] [PubMed] [Google Scholar]
- 57.Nistor D.V., Caterev S., Bolboacă S.D., Cosma D., Lucaciu D.O.G., Todor A. Transitioning to the direct anterior approach in total hip arthroplasty. Is it a true muscle sparing approach when performed by a low volume hip replacement surgeon? Int Orthop. 2017;41(11):2245–2252. doi: 10.1007/s00264-017-3480-8. [DOI] [PubMed] [Google Scholar]
- 58.Yan T., Tian S., Wang Y. Comparison of early effectiveness between SuperPATH approach and Hardinge approach in total hip arthroplasty. Chin J Reparative Reconstr Surg. 2017;31(1):17–24. doi: 10.7507/1002-1892.201609110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Mellon S.J., Liddle A.D., Pandit H. Hip replacement: landmark surgery in modern medical history. Maturitas. 2013;75(3):221–226. doi: 10.1016/j.maturitas.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 60.Pivec R., Johnson A.J., Mears S.C., Mont M.A. Hip arthroplasty. Lancet. 2012;380(9855):1768–1777. doi: 10.1016/S0140-6736(12)60607-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.