Abstract
With confirmed coronavirus disease 2019 (COVID-19) cases surpassing the 18 million mark around the globe, there is an imperative need to gain comprehensive understanding of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Although the main clinical manifestations of COVID-19 are associated with respiratory or intestinal symptoms, reports of neurological signs and symptoms are increasing. The etiology of these neurological manifestations remains obscure, and probably involves several direct pathways, not excluding the direct entry of the virus to the central nervous system (CNS) through the olfactory epithelium, circumventricular organs, or disrupted blood–brain barrier. Furthermore, neuroinflammation might occur in response to the strong systemic cytokine storm described for COVID-19, or due to dysregulation of the CNS rennin-angiotensin system. Descriptions of neurological manifestations in patients in the previous coronavirus (CoV) outbreaks have been numerous for the SARS-CoV and lesser for Middle East respiratory syndrome coronavirus (MERS-CoV). Strong evidence from patients and experimental models suggests that some human variants of CoV have the ability to reach the CNS and that neurons, astrocytes, and/or microglia can be target cells for CoV. A growing body of evidence shows that astrocytes and microglia have a major role in neuroinflammation, responding to local CNS inflammation and/or to disbalanced peripheral inflammation. This is another potential mechanism for SARS-CoV-2 damage to the CNS. In this comprehensive review, we will summarize the known neurological manifestations of SARS-CoV-2, SARS-CoV and MERS-CoV; explore the potential role for astrocytes and microglia in the infection and neuroinflammation; and compare them with the previously described human and animal CoV that showed neurotropism to propose possible underlying mechanisms.
Keywords: glia, central nervous system, COVID-19, SARS, MERS, coronavirus
The coronavirus disease 2019 (COVID-19) was originated in Wuhan, China in December 2019, and the etiological agent was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The outbreak quickly turned into a global pandemic with more than 18 million reported cases around the globe and more than 700,000 deaths (World Health Organization [WHO] Report COVID-19). The SARS-CoV-2 outbreak is not the first coronavirus (CoV) epidemic to emerge in the 21st century: Both the 2002 SARS-CoV and the 2012 Middle East respiratory syndrome coronavirus (MERS-CoV) have been included in this classification. Compared with other CoV (HCoV-229E, HCoV-OC43, HCoV-NL63), that are pathogenic to humans but present only mild clinical symptoms, SARS-CoV-2 resembles both MERS-CoV and SARS-CoV in their potential to cause a more severe disease and also in the fact that they are able to infect both the upper and lower respiratory tract (Lu et al., 2020b). Most COVID-19 patients present mild signs, or even show asymptomatic disease progression. The main clinical symptoms are fever, dry cough, fatigue, and dyspnea (Yang et al., 2020a).
A mounting body of reports from SARS-CoV-2-affected patients is showing that about 30% to 40% of patients develop serious central nervous system (CNS) symptoms, with neurological and neuroradiological alterations confirmed in a large number of cases (Alam et al., 2020; Helms et al., 2020; Jasti et al., 2020; Kremer et al., 2020; Mao et al., 2020; Najjar et al., 2020; Pryce-Roberts et al., 2020; Román et al., 2020; Romero-Sánchez et al., 2020; Xiong et al., 2020; and several others). Plasma biomarkers of CNS injury have been shown to be increased in a group of patients with moderate and severe COVID-19 disease (Kanberg et al., 2020). The finding of viral antigens, viral genomic sequences or specific antibodies against SARS-CoV-2 in cerebrospinal fluid (CSF) is less common; however, the contribution of diagnostic complications (i.e., false-negative results) or insufficient CSF viral load to be detected by real-time polymerase chain reaction should not be excluded (Benameur et al., 2020; Moriguchi et al., 2020; Najjar et al., 2020; Virhammar et al., 2020; Wu et al., 2020).
Intensive research during the past two decades has demonstrated that CNS neurons would not be able to survive without the support of glial cells in matters of metabolic balance, energy supply, immune response, and even effective neurotransmission. We now recognize that astrocytes are complex, heterogenic glial cells that encompass several important and versatile functions that include maintenance of CNS homeostasis, structural and metabolic support, modulation of synaptogenesis and synaptic transmission, participation in immune response in cooperation with microglia, regulation of blood flow, and maintenance of the blood–brain barrier (BBB; reviewed in Barres, 2008; Sofroniew and Vinters, 2010; Clarke and Barres, 2013; Ramos, 2016; Zorec et al., 2019). When astrocytes sense stimuli associated to injury or disease, including viral infection, they respond with a process called astrogliosis that profoundly alters astrocytic biology. Reactive gliosis is a fine graded and highly conserved mechanism of astroglial response to injury, and, in general terms, it is supposed to be aimed to improve neuronal survival, to restore BBB, and to isolate the injured area by providing glial scar formation (Sofroniew and Vinters, 2010; Anderson et al., 2016; Verkhratsky et al., 2019). However, under certain not yet completely defined circumstances, but probably involving proinflammatory microglial activation and toll-like/NF-κB/STAT3-dependent pathways, astrocytes may engage into a proinflammatory gene expression program also called maladaptive reactive astrogliosis that transforms astrocytes into proinflammatory and proneurodegenerative cells (Pekny et al., 2016; Liddelow et al., 2017; Rosciszewski et al., 2018, 2019; Zorec et al., 2019). Transcriptomic analyses of reactive astrocytes have also identified this spectrum of possible activation profiles ranging between two extreme phenotypes that were simplistically defined as the proinflammatory proneurodegenerative A1 phenotype and the proneuronal survival immunomodulatory A2 phenotype, but these studies also showed mixed reactive profiles characterized by the expression of PAN-reactive genes (Hamby et al., 2012; Zamanian et al., 2012; Anderson et al., 2016; Burda and Sofroniew, 2017; Liddelow and Barres, 2017; Liddelow et al., 2017; Clarke et al., 2018). Intensive research from our group and others has shown that astroglial engagement in the proinflammatory-neurodegenerative gene expression program is facilitated by astroglial exposure to pathogen-associated molecular patterns (PAMP), damage-associated molecular patterns (DAMP), and to microglial-derived proinflammatory cytokines (Rothhammer et al., 2016; Liddelow et al., 2017; Rosciszewski et al., 2018, 2019). It is also proposed that persisting reactive gliosis, as shown in neurodegenerative diseases, as well as infectious agents reaching the CNS, facilitate the proinflammatory program in reactive astrocytes (reviewed in Pekny et al., 2016; Zorec et al., 2019).
Microglia are the professional immune cells in the CNS and thus are the first responders to brain injury or infection. However, current knowledge shows that microglia are also a highly heterogeneous cell population, with sex- and region-specific differences that exert a plethora of physiological roles in healthy CNS including patrolling of brain parenchyma, clearing apoptotic cells and other debris, regulating neuronal plasticity by participating in synaptic pruning, and responding to signals from peripheral immune system (Wilton et al., 2019; Ewald et al., 2020; Gerrits et al., 2020). Following CNS viral infection, microglial cells become rapidly activated and release proinflammatory molecules and reactive oxygen species, recruit cells of the peripheral immune system, and activate astrocytes (Ransohoff and Perry, 2009; Chatterjee et al., 2013; Wheeler et al., 2018).
Previous experiences with SARS-CoV and MERS-CoV, as well as experimental data on neurotropic CoVs, have shown that CoV can reach the CNS and infect it (Steardo et al., 2020). We here performed a comprehensive review on the CNS cell types known to be affected by CoV infections with a special focus on the role of astrocytes and microglia and the consequences for brain physiology.
Middle East Respiratory Syndrome
MERS-CoV has been identified as a cause of severe respiratory infection in humans since the 2012 outbreak, being the second highly pathogenic CoV to rapidly spread into human populations. The number of laboratory-confirmed cases reported by the WHO until January 2020 was of 2,519 cases globally, with a mortality rate of 34.3% (WHO, 2019). Although the MERS-CoV infection was asymptomatic in some patients, many cases present pneumonia and severe symptoms that can result in multiorgan failure and death (WHO MERS-CoV Research Group, 2013).
There are a number of reports of MERS-CoV patients showing neurological symptoms (Arabi et al., 2015; Kim et al., 2017), although the overall number of reports showing neurological manifestations in MERS patients is low compared with the present knowledge on SARS-CoV-2. However, MERS-CoV belongs to lineage C of the genus Betacoronavirus, whose species are known to be potentially neuroinvasive (Desforges et al., 2014). Reported neurological symptoms in MERS-CoV infection mostly come from case reports, and findings include neuropathy, delirium, and seizures (Saad et al., 2014; Arabi et al., 2015; Algahtani et al., 2016; Kim et al., 2017). However, the number of reports is quite low probably due to the significant comorbidities and the severe critical condition of complicated MERS-CoV patients.
In spite of their similarity, MERS-CoV does not share with SARS-CoV and SARS-CoV-2 the mechanism to gain access to cells. MERS-CoV utilizes exopeptidase, dipeptidyl peptidase 4 (DPP4), as a receptor to enter host cells. Human DPP4 (hDPP4) expression is a requirement to make nonsusceptible species, such as rodents, become susceptible to MERS-CoV infection (van Doremalen and Munster, 2015). MERS-CoV has also shown increased mortality in obese patients, and the finding has been related to increased expression of DPP4 in obese people (Al-Hameed, 2017).
MERS-CoV has the potential ability to enter microglia, astrocytes, and neurons, considering that all these cell types express DPP4 (Király et al., 2018; Elkjaer et al., 2019). Among these CNS cells, glial fibrillary acidic protein-positive (GFAP+) astrocytes seem to show the largest DPP4 basal expression, and inflammation significantly increased the expression of the viral receptor (Király et al., 2018), thus allowing a feed-forward loop that increases MERS-CoV access to glial cells. Moreover, DPP4 was also found in brain microvasculature (Kenny and Bourne, 1991; Zeng et al., 2019) turning endothelial cells into another MERS-CoV potential target.
Studies in transgenic mice expressing hDPP4 or adenoviral-based expression of hDPP4 in mice have shown that intranasal exposure to MERS-CoV resulted in illness and high mortality rates (reviewed in van Doremalen and Munster, 2015). In these mice, viral RNA was detected in several organs including lungs and brain. While dramatic lesions were found in the lungs of these hDPP4-expressing mice, no gross pathological changes were observed in the brain; however, viral antigen expression was found in brain microglia, astrocytes, and neuronal cells, together with increased proinflammatory cytokines and chemokines (Agrawal et al., 2015; Zhao et al., 2015; Tao et al., 2016). Indeed, Tao et al. (2016) were able to recover viral particles from brain tissue and detected viral antigen expression in neurons and glia of the hDPP4 mice. In silico modeling of common marmoset DPP4 showed high similarity with hDPP4, and, as was predicted, this resulted in high susceptibility of marmosets to MERS-CoV (Raj et al., 2013; Falzarano et al., 2014). Infected marmosets showed severe illness, and viral RNA was detected in all tested organs including lungs and brain (van Doremalen and Munster, 2015). There is, however, another report using transgenic hDPP4 mice that found no evidence of MERS-CoV viral infection in the brain, although these authors used a hDPP4 promoter that rendered negative hDPP4 expression in neurons and glia (Iwata-Yoshikawa et al., 2019).
Among the MERS-CoV patient case reports describing neurological symptoms (Saad et al., 2014; Arabi et al., 2015; Algahtani et al., 2016; Kim et al., 2017), it is interesting to note that MRI findings obtained by Arabi et al. (2015) were rather supportive of primary viral neuropathology resembling an acute disseminated encephalomyelitis (Marin and Callen, 2013). The study lacks, however, a confirmatory test for brain infection, such as could have been the positive detection of MERS-CoV in brain tissue or CSF (Arabi et al., 2015).
Taken together, the published evidence shows that we still lack confirmatory studies demonstrating the presence of MERS-CoV viral particles in the CNS of human patients; however, the brain imaging findings (Arabi et al., 2015), together with clinical findings (Saad et al., 2014; Arabi et al., 2015; Algahtani et al., 2016; Kim et al., 2017), are highly indicative of a direct effect of MERS-CoV on the CNS. Experiments using hDPP4 expression in animals have shown that MERS-CoV has the ability of infecting and proliferating in microglia, astrocytes, or even in neurons (Agrawal et al., 2015; Zhao et al., 2015; Tao et al., 2016), but this seems to be highly dependent on DPP4 expression in these cell types (Iwata-Yoshikawa et al., 2019).
Severe Acute Respiratory Syndrome
The first reported outbreak of a human CoV producing SARS, named SARS-CoV, emerged in November 2002 in Guangdong Province, China. Since then, until the mysterious disappearance of SARS-CoV cases 6 months later, the outbreak resulted in 8,098 SARS-CoV cases, with 774 deaths, a 9.56% mortality rate (WHO, 2004). As both the present SARS-CoV-2 and MERS-CoV, SARS-CoV belongs to the Coronavirinae subfamily, genera betacoronaviruses (Ng Kee Kwong et al., 2020).
SARS-CoV patients usually referred high fever associated with chills, headache, muscular pain, and sometimes diarrhea. Most patients develop respiratory symptoms and pneumonia, with 10% to 20% of the patients requiring mechanical ventilation.
Several case reports showing neurological symptoms were documented for SARS-CoV. Among the neurological symptoms, the most abundant were those showing an effect on the CNS such as seizures, dysphoria, vomiting, and deliria, (Hung et al., 2003; Lau et al., 2004; Tsai et al., 2005; Xu et al., 2005) as well as stroke (Umapathi et al., 2004; Xu et al., 2005). In spite of the low number of patients showing neurological clinical presentation, the finding of viral RNA in both CSF (Hung et al., 2003; Lau et al., 2004) as well as in autopsied human brain tissue (Xu et al., 2005) reflects the potential neurotropism of SARS-CoV.
Xu et al. (2005) have shown that viral SARS-CoV proteins were expressed in the brain of a SARS-CoV patient who presented severe neurological symptoms. In addition, the authors also recovered infective viral particles from autopsy brain preparations of this patient. Brain sections showed an intense inflammation with CD68+ macrophages infiltration, neuronal necrosis, diffuse brain edema, and reactive gliosis. Moreover, viral proteins were detected by immunohistochemistry in brain neurons and astrocytes (Xu et al., 2005).
In a series of patients who died from SARS-CoV infection, Ding et al. (2004) systematically analyzed the SARS-CoV presence in different organs, and they found that the virus was present not only in the respiratory organs but also in isolated cerebral cortical neurons (Ding et al., 2004). SARS-CoV particles in cortical and hypothalamic neurons as well as important signs of neuronal degeneration and brain edema were also detected by Gu et al. (2005) in a series of patients who died from SARS.
Interestingly, SARS-CoV isolated from human patients was shown to be able to infect mice (Glass et al., 2004; Subbarao et al., 2004), ferrets, domestic cats, and various species of monkeys (Martina et al., 2003; Haagmans et al., 2004). After intranasal inoculation, SARS-CoV infection in mice was initially present in the respiratory tract, then reaching different organs, including the brain (Glass et al., 2004). Mice brains showed a large increase of cells with SARS-CoV sequences, and authors could also isolate infective viral particles from these mice brains (Glass et al., 2004), in a striking similarity to the human reported cases (Ding et al., 2004; Xu et al., 2005). In SARS-CoV-infected mice, viral-positive cells were predominantly observed in brain hippocampus in the pyramidal cell layer of the hippocampal CA1 region and in the dentate gyrus (Glass et al., 2004). In addition, evidence of neuroinflammation was confirmed by the elevated cytokine expression in the brains of SARS-CoV-infected mice (Glass et al., 2004).
SARS-CoV was the first human CoV reported to bind to human angiotensin-converting enzyme 2 (ACE2) to infect host cells through interaction with SARS-CoV spike protein (Li et al., 2003; Prabakaran et al., 2004; Wang et al., 2004). The ACE2 expression profile was characterized in detail by Hamming et al. (2004) using human biopsies (Hamming et al., 2004). As expected, they found ACE2 expression in the lung alveolar epithelial cells and enterocytes of the small intestine, but they also found that ACE2 was present in arterial and venous endothelial cells and arterial smooth muscle cells in all of the organs studied. Specifically in the brain, the authors found that ACE2 is expressed in endothelium and vascular smooth muscle cells (Hamming et al., 2004), while others later reported ACE2 expression in neurons and glia (Gallagher et al., 2006; Matsushita et al., 2010; Gowrisankar and Clark, 2016; Xu et al., 2017; de Morais et al., 2018). In mice, ACE2 neuronal expression was described to be present in both areas involved in the central regulation of cardiovascular function, as well as in noncardiovascular nuclei (Doobay et al., 2007; Lin et al., 2008).
SARS-CoV outbreak stopped suddenly; therefore, studies of human brains from SARS-CoV-infected patients with CNS symptoms are lacking, and most studies used the approach of humanizing the ACE2 in mice. For example, McCray et al. (2007) developed transgenic mice that express the human ACE2 receptor under the control of the cytokeratin 18 promoter (K18-hACE2 mice). Intranasal infection of K18-hACE2 mice with SARS-CoV resulted in a fatal disease, directly related to the number of copies of hACE2 transgene and hACE2 mRNA levels (McCray et al., 2007). Histopathological analysis of these animals showed extensive virus replication not only in the lungs but also in the brain (McCray et al., 2007; Tseng et al., 2007).
Netland et al. (2008) performed experiments analyzing the temporal dynamics of brain infection following intranasal SARS-CoV administration in hACE2 mice. The authors showed that SARS-CoV N protein was detectable and surprisingly widespread in brain regions, and subsequent viral clearance was associated with neuronal loss in these areas (Netland et al., 2008). Time course studies showed a pattern of viral infection that was strongly suggestive of an entry via the olfactory nerve, with subsequent transneuronal spreading (Netland et al., 2008). Netland et al. (2008) did not detect reactive astrogliosis in SARS-CoV-infected hACE2 mice. This is surprising when considering that this apparent astroglial unresponsiveness to viral infection is accompanied by an increased number of Iba1+ microglia and interleukin (IL)-6 overexpression, a cytokine that is mainly produced by astrocytes and microglia. Moreover, overexpression of a plethora of proinflammatory cytokines was observed in the brain of SARS-CoV-infected mice, most notably IL-6, interferon (IFN)-γ, chemokine (C-C motif) ligand (CCL)-2, and CCL12 (Glass et al., 2004; McCray et al., 2007; Tseng et al., 2007) and also in cases reported in humans (Xu et al., 2005). We now know that astrocytes are highly sensitive to increased proinflammatory mediators and that this stimulus induce a proinflammatory gene expression program in astrocytes (Liddelow and Barres, 2017; Rosciszewski et al., 2019; Verkhratsky et al., 2019).
Taken together, the accumulated evidence from patients who died from severe SARS with CNS compromise as well as the experimental data from wild-type or transgenic hACE2 animal models show that SARS-CoV is able to effectively reach and infect CNS cells, express viral proteins, and produce neurodegeneration. The hypotheses about the pathways utilized by SARS-CoV to reach the brain are essentially (a) the olfactory bulb/transsynaptic pathway or (b) the hematogenous spread from heavily infected lungs and airways. This latter alternative is facilitated by systemic inflammation that increases BBB permeability and astroglial/microglial proinflammatory response due to circulating cytokines and/or due to local viral replication in the CNS.
When analyzing the potential glial role in SARS-CoV infection, in addition to the possibility that the virus replicates in glial cells, we should also consider the glial role in the strong neuroinflammatory response that can be induced by viral invasion or that can be attributed to the increased peripheral cytokine levels. Astrocytes and microglia are sensitive to peripheral cytokines, and their activation and engagement into a proinflammatory gene expression program could also increase BBB permeability. Proinflammatory astrocytes seem to have a main role in SARS-CoV infection by recruiting peripheral macrophages and lymphocytes to the brain parenchyma, thus increasing edema and cytotoxicity in these conditions (Xu et al., 2005). Specifically, an increased expression of IFN-γ was found in glial cells of a patient that developed severe CNS invasion by SARS-CoV (Xu et al., 2005). In addition, the possibility that SARS-CoV infection alters the brain microvasculature is likely, either by a direct effect on the endothelium and glial cells due to viral invasion, or secondary to the strong inflammatory response elicited in either human or animal hosts (Glass et al., 2004; Xu et al., 2005).
Other Human CoV That Show Neurotropism
CoVs are widely known as human pathogens causing respiratory tract infections. In addition to SARS-CoV, MERS-CoV, and SARS-CoV-2, other human CoV (HCoV) have been described in the past decades, including HCoV-229E, HCoV-NL63, HCoV-OC43, and HCoV-HKU1 (Gaunt et al., 2010; Zlateva et al., 2013; Desforges et al., 2019).
Although HCoV are usually restricted to the airways in immunocompetent patients, several studies showed evidence of neurotropic and neuroinvasive capacities of some HCoV strains (reviewed in Desforges et al., 2014, 2019). Early findings from Arbour et al. (2000) have shown a high prevalence of HCoV-229E and HCoV-OC43 in human brain autopsy samples of patients affected with multiple sclerosis and other neurological diseases (Arbour et al., 2000). In addition, neurological symptoms have been described in association with both HCoV-HKU1 and HCoV-NL63 infections (Severance et al., 2011).
Experimental studies have shown that HCoV strains have the ability of replicating in glial cells in vitro. In fact, the HCoV-229E and HCoV-OC43 have shown to infect glial and neuronal cell lines as well as primary human astrocytic cultures (Bonavia et al., 1997; Arbour et al., 1999a, 1999b; Jacomy et al., 2006). In vivo, HCoV-OC43 is naturally neuroinvasive and promotes chronic encephalitis in mice, with clustering of microglial cells and neuronal loss (Jacomy et al., 2006).
Taken together, the present data point out to a neuroinvasive potential of HCoV-OC43 and HCoV-229E, where astrocytes, microglia, and/or neurons could be the cell targets of the infection (Malone et al., 2006; Hwang and Bergmann, 2018). Again, the potential routes for HCoV are the hematogenous spread during viremia or the retrograde neuronal route (revised in Desforges et al., 2019).
In general terms, microglia and astrocytes play a critical role in RNA virus infection (Soung and Klein, 2018). The HIV is another RNA virus of great importance in public health where neurotropism, and especially the glial role in infection and chronicity, is being rapidly unveiled. HIV-1 exploits the Trojan Horse Strategy to reach the CNS parenchyma, where infected T cells and monocytes cross the BBB, transferring infection to microglia and CNS perivascular macrophages (González-Scarano and Martín-García, 2005; Elbirt et al., 2015). While macrophages and microglia exhibit productive infection and can release viral particles, astrocytes become infected, but they show restricted HIV-1 replication and nonproductive infection (reviewed in Churchill and Nath, 2013; Zorec et al., 2019). However, this is a double-edged sword; on one hand, nonproductive astroglial infection reduces brain damage, which would be otherwise a devastating CNS disorder, but on the other hand, it allows for HIV-1 to latently persist in the brain parenchyma even in successfully treated patients with low viral load (reviewed in Pandey and Seth, 2019). Moreover, in patients with HIV-associated dementia, more than 19% of astrocytes have HIV sequences, and the abundance is higher in astrocytes that are in close proximity to macrophages, especially at the perivascular regions (Churchill et al., 2009; reviewed in Pandey and Seth, 2019). In addition, it is not clear how viral persistence affects the normal homeostatic functions of astrocytes that are essential for the CNS functionality. Surviving, but persistently infected astrocytes could be suffering a pathological remodeling or an astrogliopathology that reduces the neuronal-supportive pathways that sustain CNS homeostasis.
Animal CoV That Show Neurotropism
HCoV are molecularly and structurally related to several neuroinvasive animals CoV. Specifically, mouse hepatitis virus (MHV) has been extensively studied, and both the John Howard Muller MHV (JHM-MHV) and the MHV-A59 strain, when inoculated intracranially or intranasally, are neurovirulent (Bender and Weiss, 2010; Cowley and Weiss, 2010). In general terms, after nasal inoculation, neurotropic strains of MHV reach the CNS through a transneuronal route up to the olfactory bulbs, from where viral particles spread into the brain parenchyma (Perlman et al., 1990; revised in Cowley and Weiss, 2010).
In rats, MHV infection promotes a primary stage of neuronal and glial infection, severe inflammation, and destructive lesions mainly in the gray matter, followed by a secondary stage of demyelination with chronic inflammation, astrogliopathology with astroglial loss and axonal pathology (Nagashima et al., 1978, 1979; Zimprich et al., 1991).
Since the JHM-MHV strain is highly lethal in mice, a larger number of studies have been performed using the sublethal glia tropic variant of the JHM-MHV, designated v2.2-1 (Savarin and Bergmann, 2018). Both sublethal MHV-59 and JHM-MHV v2.2-1 viruses are able to produce an acute encephalomyelitis that turns into a persistent infection causing demyelinating lesions with presence of viral RNA, but absence of infective viral particles (Savarin and Bergmann, 2018). Infection of Lewis rats with JHM-MHV CoV induces viral particle incorporation by astrocytes and reactive astrogliosis at the surroundings of demyelinated lesion plates (Barac-Latas et al., 1997).
The murine JHM-MHV strain was shown to infect astrocytes in vitro and in vivo, and astrocytes apparently constitute a viral reservoir in asymptomatic JHM-MHV-infected mice (Perlman and Ries, 1987). These early reports are consistent with the hypothesis that astrocytes can not only be hosts of the CoV but can also behave as reservoirs of CoV in the brain parenchyma. In culture, MHV infects astrocytes and microglia promoting a proinflammatory conversion of both cell types evidenced by an increase in proinflammatory cytokines such as tumor necrosis factor (TNF)α, IL-1β, and IL-6. Such phenomenon has been also evidenced in vivo during encephalitis and demyelination of spinal cord in mice models (Sun et al., 1995; Gonzales et al., 2004; Li et al., 2004). Moreover, following intranasal inoculation with JHM-MHV, microglia become rapidly activated; release proinflammatory IL-6, TNFα, and IFN-α/β; phagocytize infected cells; and recruit peripheral monocytes/macrophages by secreting the chemokine CCL2 (Wheeler et al., 2018). This major role of microglia in the primary response to JHM-MHV CoV is supported by the fact that microglial depletion exacerbated viral replication and dissemination in the mice brain (Wheeler et al., 2018).
The less aggressive JHM-MHV variant v2.2-1 also infects microglia, astrocytes, and oligodendrocytes. Here, major histocompatibility class I and II complexes are upregulated in microglial cells and astrocytes in response to IFNγ, while oligodendrocytes may serve as a reservoir for viral persistence (Suzumura et al., 1986; Malone et al., 2006).
After intranasal exposure in mice, MHV-A59 produces acute hepatitis, meningitis, and encephalitis followed by a chronic phase of inflammatory demyelinating disease. It is clear that the acute phase involves active viral replication in liver and brain, while in the chronic phase, viral RNA persist in the brain, but without evidence of viral replication or viral antigen expression (Lavi and Cong, 2020). Infection with MHV-A59 induces upregulation of several proinflammatory cytokines in astrocytes as well as the IFNα, IFNβ, and IFNγ (Lavi and Cong, 2020). On the other hand, the same authors showed that in microglia, MHV-59 induces the expression of IL-6 and of all the members of the IFN and TNF family. Interestingly, the nonencephalitic MHV strain (MHV-2), that does not produce acute or chronic encephalitis, failed to induce cytokine expression in astroglial or microglial cultures (Lavi and Cong, 2020). These important findings reinforce the concept that engagement of reactive astrocytes and microglia in a proinflammatory response is a key event in CoV infections. The downside of this activation is the neural detrimental effects of such proinflammatory environment that may contribute to cognitive impairments in neurotropic CoV infections. In agreement, the fine tuning of the cytokine storm in these CoV infections with anti-inflammatory cytokines or regulatory T-cells (Tregs) adoption reduces secondary demyelinating lesions (Trandem et al., 2010; Blanc et al., 2014; Savarin and Bergmann, 2018).
However, the switch to a proinflammatory gene expression program seems not to be the unique astroglial and microglial response to neurotropic virus, and especially to neurotropic CoV. Astrocytes and microglia are the CNS-resident cells most prominently involved in the innate immunity responses, as they are able to respond to PAMP that interact with pattern recognition receptors highly expressed in microglia and also expressed in lower level in astrocytes (Farina et al., 2007; Russo and McGavern, 2015; Hwang and Bergmann, 2018; Rosciszewski et al., 2018, 2019). Recent findings have shown that astrocytes mount a delayed but robust antiviral response to the neurotropic MHV-A59 CoV in vivo in the rodent encephalitis model (Hwang and Bergmann, 2018). In this model, astrocytes upregulated the IFN-α/β pathway to a greater extent than microglia. Concomitantly, the specific ablation of interferon-α/β receptor (IFNAR) in astrocytes using a transgenic mGFAPcre IFNARfl/fl mice resulted in severe encephalomyelitis, increased neutrophil and decreased T-cell infiltration, uncontrolled viral spread in the CNS parenchyma, and increased lethal effects in deficient mice (Hwang and Bergmann, 2018). As mentioned before, IFNγ, one of the type 2 interferons (IFN-II), is a key molecule in the response of glial cells to viral infection, and it is produced by cells that are not brain residents. However, type 1 interferons (IFN-I) and the astroglial IFNAR also play a major role in responses to neurotropic viral infection, including CoV (Malone et al., 2006; Owens et al., 2014; Hwang and Bergmann, 2018).
In addition to the astroglial role in preventing CNS spreading of MHV-A59, microglia seem also to be required to control neurotropic CoV infection. A recently published article showed that depletion of microglia using PLX5622, an inhibitor of colony-stimulating factor 1 receptor (CSF1R), in animals exposed to JHM-MHV increased mortality, impaired control of viral replication, altered CD4+ and CD8+ T-cell infiltration, increased demyelination, and decreased neuro-repair (Mangale et al., 2020).
The Janus-faced astroglial and microglial role in neurotropic CoVs infection, with a required suppressive effect on CoV replication, but a proinflammatory detrimental role in the demyelinating late phase, highlights the importance of a timely control of the cytokine storm in CoV infections. These lessons should be critically considered when developing novel clinical approaches to prevent neurological complications in COVID-19 patients (see later).
Severe Acute Respiratory Syndrome-2
While the hallmarks of COVID-19 moderate clinical presentation are fever, respiratory symptoms including dry cough and dyspnea, and diarrhea, a more severe respiratory condition termed acute respiratory distress syndrome can eventually develop, and it includes the cytokine release syndrome (cytokine storm). Neurological manifestations of SARS-CoV-2 infection are starting to be systematically recorded and reported, with several initiatives to consolidate and record clinical findings (Ferrarese et al., 2020; Román et al., 2020; Romero-Sánchez et al., 2020). Between 30% and 40% of the SARS-CoV-2 patients present neurological symptoms; these can go from mild symptoms including olfactory and gustatory disorders, dizziness, headache, confusion, to a more severe cerebrovascular disease, encephalitis, seizures, or the Guillain–Barré syndrome (Asadi-Pooya and Simani, 2020; Kremer et al., 2020; Mao et al., 2020). The presence of SARS-CoV-2 viral particles in the CNS has been evidenced in some cases (Benameur et al., 2020; Moriguchi et al., 2020; Wu et al., 2020), with reports showing SARS-CoV-2 presence in CSF (Finsterer and Stollberger, 2020). Other authors also found SARS-CoV-2 viral particles in neural and capillary endothelial cells of frontal lobe brain sections of a COVID-19 patient (Paniz-Mondolfi et al., 2020), while the plasma biomarkers of CNS damage GFAP and neurofilament light chain have been shown to be increased in a group of moderate and severe COVID-19 cases (Kanberg et al., 2020). In several patients, SARS-CoV-2 infection has been associated with ischemic stroke, and this has been originally attributed to excessive inflammation, hypoxia, or diffuse intravascular coagulation (Lu et al., 2020a; Mao et al., 2020; Yang et al., 2020b), but a SARS-CoV-2 direct role in these clinical presentations is also possible.
SARS-CoV-2 is a single-stranded positive-sense RNA virus sharing 79% and 50% identity with SARS-CoV and MERS-CoV, respectively (Lu et al., 2020b). The spike (S) protein of CoV is known to engage cell surface receptors to facilitate viral entry into the cells. It has been determined, as seen for SARS-CoV, that SARS-CoV-2 spike S protein also uses ACE2 as entry receptor (Hoffmann et al., 2020). Taking into account that SARS-CoV-2 shares the ACE2-mediated mechanism of entrance to the cells, it is highly possible that these molecular mechanisms would also help explain the more severe forms of the disease, including the possibility of a disbalanced renin-angiotensin system (RAS), as was demonstrated for SARS-CoV (Imai et al., 2005; Kuba et al., 2005; see later).
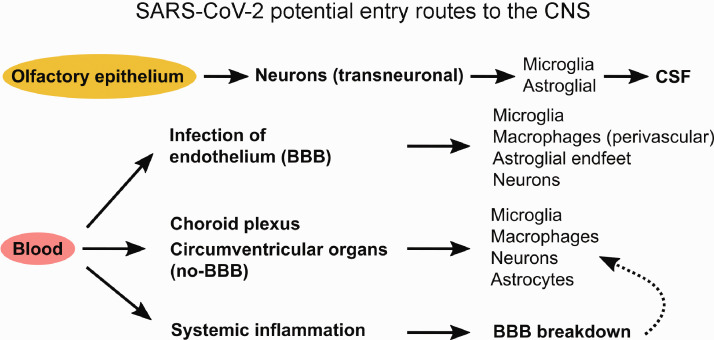
There are several hypotheses as to how could SARS-CoV-2 reach and affect the CNS. Neuronal retrograde dissemination has been observed in other CoV (see earlier), and taking into account the presence of the virus in nose swabs, hyposmia symptoms in some patients, and the expression of ACE2 in the nasal mucosa (Hou et al., 2020), a transneuronal pathway involving olfactory epithelium>olfactory bulb>olfactory nucleus in the pyriform cortex cannot be ruled out (Figure 1). In addition, other authors proposed that SARS-CoV-2 could be reaching the CNS using the vagus nerve traveling through lung–gut–brain axis (Alam et al., 2020). Another possible way for SARS-CoV-2 to enter the CNS is the hematogenous route during viremia in severe affected patients. SARS-CoV-2 could enter through the circumventricular organs, which lack BBB, or through altered BBB where endothelial cells and astroglial end-feet could have a major role (Figure 1). Endothelial cells express ACE2 and are thus potential targets to be infected by SARS-CoV-2 (Hamming et al., 2004; Feng et al., 2010b). Although there is no present data of SARS-CoV-2 presence in astrocytes, increased level of soluble GFAP in plasma of COVID-19 patients has been reported (Kanberg et al., 2020), and a large body of data support that astrocytes are target of neurotropic CoV as commented in the previous sections (Sun et al., 1995; Gonzales et al., 2004; Li et al., 2004; Xu et al., 2005; Jacomy et al., 2006; Desforges et al., 2019; Steardo et al., 2020; Figure 2).
Figure 1.
SARS-CoV-2 Potential Entry Routes to the CNS. SARS-CoV-2 may reach CNS using two main routes: the olfactory epithelium or the hematogenous (blood) routes. When entering through the olfactory epithelium, viral particles would have access to the CNS using transneuronal/synaptic pathways. Following neuronal infection, viral particles released may infect microglia and astrocytes. In the hematogenous entry route, endothelial cells may become infected, followed by perivascular astrocytes and perivascular macrophages. Secondarily, viral particles may reach microglia and neurons. Also during viremia in severe affected patients, SARS-CoV-2 can reach choroid plexus and circumventricular organs, which lack of BBB, and subsequently entering to brain parenchyma. A third possibility of CNS infection may arise after BBB breakdown as a consequence of systemic inflammation and cytokine release. Increased BBB permeability could facilitate SARS-CoV-2 entrance to the CNS.
SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2; CNS = central nervous system; CSF = cerebrospinal fluid; BBB = blood–brain barrier.
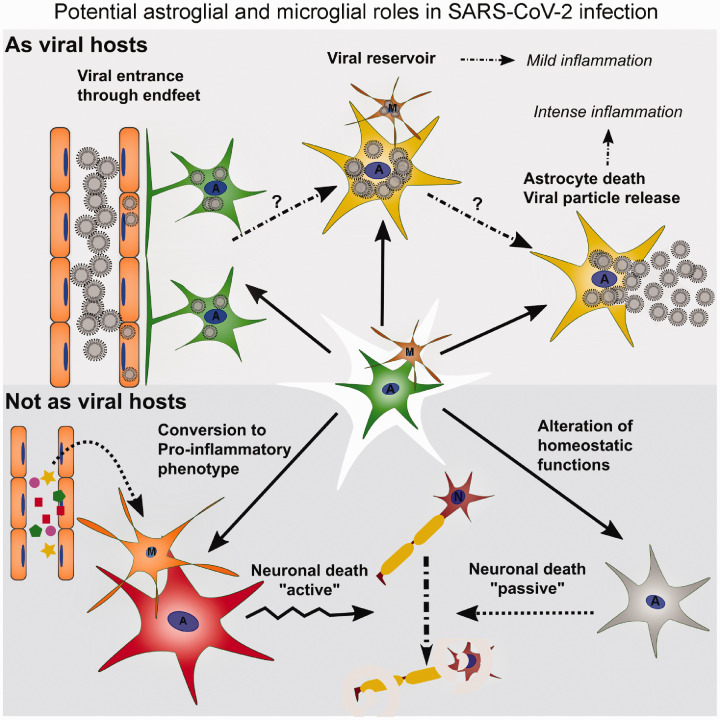
Figure 2.
Potential Astroglial and Microglial Roles in SARS-CoV-2 Infection.
Astrocytes and microglia are viral hosts: Perivascular astrocytes may incorporate viral particles by direct contact with infected endothelial cells. However, BBB breakdown may also lead to viral infection of nonperivascular astrocytes and microglia. In both situations, infected cells may act as viral hosts giving nonproductive infection with mild inflammatory response and with microglia acting as antigen-presenting cells; or astrocytes may give rise to a productive infection, with destruction of astroglial network. This latter possibility is more unlikely based on clinical findings.
Astrocytes and microglia are not viral hosts: Astrocytes and microglia are not primary targets of viral infection, but they are responsive to proinflammatory signals from endothelial cells, macrophages, and/or neurons. In such case, astrocytes and microglia may engage in a proinflammatory gene expression program that would expand neuroinflammation. This maladaptive reactive astrogliosis would reduce neuroprotective and metabolic support to neurons which secondarily may degenerate by lack of nutrients and neurotrophic factors.
A = astrocytes; M = microglia; N = neurons.
In addition to being potential targets for SARS-CoV-2, both astrocytes and microglia are highly sensitive to systemic proinflammatory cytokines (Perry et al., 2007; Teeling and Perry, 2009; Murta et al., 2015; Murta and Ferrari, 2016). Indeed, the massive release of inflammatory cytokines described for severe COVID-19 patients could be enough to destabilize the tight junctions of the BBB endothelial cells and astrocytes, thus facilitating viral entry (Li et al., 2015; Swanson and McGavern, 2015; Figure 2). Furthermore, as explained in the earlier sections, astrocytes and microglia are part of the local neuroinflammatory response of the CNS and express pattern recognition receptors, the cellular receptors needed to initiate and/or amplify innate immune responses within the CNS (Farina et al., 2007; Russo and McGavern, 2015; Hwang and Bergmann, 2018; Rosciszewski et al., 2018, 2019). As part of the BBB, astrocytes would rapidly receive the proinflammatory signals from endothelial cells, in addition to microglial-derived cytokines. Microglia have been demonstrated to closely interact with monocytes and lymphocytes in viral infections affecting the CNS (see, e.g., Hwang and Bergmann, 2018; Mangale et al., 2020). Moreover, it has been shown that the presence of reactive proinflammatory microglia, the exposure to proinflammatory cytokines such as IL-1β, TNFα, and IL-6, or the exposure to PAMP/DAMP can induce in astrocytes the expression of proinflammatory genes that facilitates neuroinflammation and neurodegeneration (Liddelow et al., 2017; Rosciszewski et al., 2018, 2019; Figure 2).
As commented in the previous sections, microglial cells are highly heterogenic and have a plethora of functions in the healthy CNS that are likely to be affected by the SARS-CoV-2 entrance to the brain, or by the cytokine storm originated in the periphery. This line of reasoning allowed some authors to propose that SARS-CoV-2-induced proinflammatory microglial phenotype might contribute to the development of neurodegenerative disorders (Alam et al., 2020; Mahalaxmi et al., 2020). Furthermore, the proinflammatory priming of microglia achieved by the direct SARS-CoV-2 infection, or by the peripheral cytokine storm, could contribute to the development of neuropsychiatric symptoms (Lavi et al., 2020) or to exacerbate previous clinical or even subclinical signs and symptoms of neurodegenerative diseases.
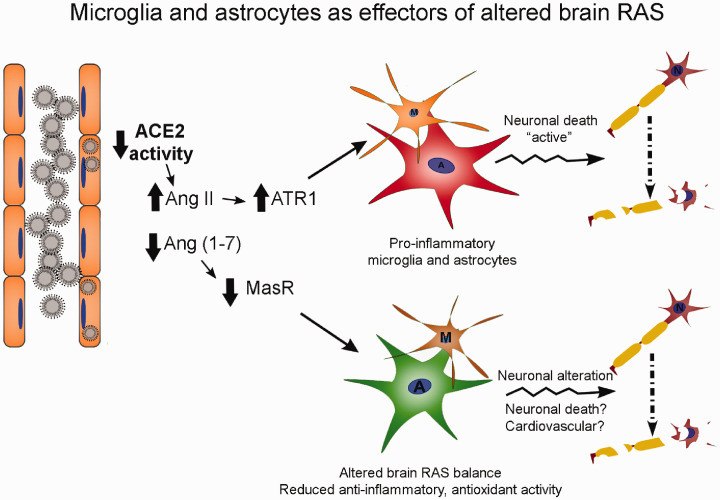
The clinical relevance of the RAS in cardiovascular function has been well established. Angiotensin II (Ang II), acting through type 1 receptor (ATR1), promotes vascular contractility, inflammation, and oxidative stress, while Angiotensin (1–7) (abbreviated as Ang (1–7)), produced by ACE2, activates mitochondrial assembly receptor receptors (MasR) counteracting the effects of the Ang II/AT1R axis (Feng et al., 2008, 2010a, 2010b). As described in previous sections, SARS-CoV-2 and its predecessor SARS-CoV exploit the ACE2 receptor to enter to host cells, and it is proposed that decreased ACE2 level occurs in COVID-19 patients. This fact may justify the severe complications in patients with hypertension, diabetes, and cardiovascular disease (Abbasi Pashaki et al., 2020; Gan et al., 2020; and others). Specifically in the brain, Ang (1–7)/MasR pathway favors vasodilatation, anti-inflammation, antioxidant, and antiapoptotic pathways (reviewed in Xia and Lazartigues, 2008; Arroja et al., 2016; Abiodun and Ola, 2020). Since Ang II and Ang (1–7) have opposing effects, and ACE2 catalyzes the conversion of Ang II into Ang (1–7), the role of ACE2 in the maintenance of brain RAS equilibrium is critical. Showing some regional and anatomical variations, and being enriched in cardiovascular regulatory regions of the brain, all RAS components are present in the brain (Sriramula et al., 2017; Xu et al., 2017; de Morais et al., 2018). Astrocytes are the main source of angiotensinogen and express ATR1 and MasR; neurons express ATR1, ACE2, and MasR, and microglia respond to ATR1 activation (Shi et al., 2014; de Morais et al., 2018). Indeed, the brain is the organ with the highest MasR expression, and high Ang (1–7) concentrations have been detected in the brain (Huber et al., 2017). ACE2 is expressed in brain endothelium, neurons, and probably in glial cells (Hamming et al., 2004; Gallagher et al., 2006; Matsushita et al., 2010; Gowrisankar and Clark, 2016; Xu et al., 2017; de Morais et al., 2018). The proposed SARS-CoV-2-induced depletion of ACE2 has the potential to induce severe consequences in brain RAS system by altering the ATR1/MasR balance toward the neuroinflammation. For example, ATR1 activation on microglia activates NF-κB and the release of proinflammatory cytokines (Shi et al., 2014; de Morais et al., 2018) that may induce subsequent astroglial proinflammatory response (Figure 3). Indeed, reduced activity of the Ang (1–7)/MasR pathway would decrease the antioxidant and anti-inflammatory mediators in the brain parenchyma (Figure 3). In fact, brain RAS has been involved in seizures and epilepsy where hyperactivation of Ang II/ATR1 signaling in astrocytes and microglia have been observed (Krasniqi and Daci, 2019). Reduced brain blood flow and ischemia are other known consequences of altered RAS activity and could also be the result of reduced endothelial ACE2 expression caused by the SARS-CoV-2 infection (reviewed in Najjar et al., 2020). Both seizures and brain ischemia have been reported as neurological symptoms in critical COVID-19 patients.
Figure 3.
Microglia and Astrocytes as Effectors of Altered Brain RAS.
RAS-mediated proinflammatory priming: SARS-CoV-2 utilizes ACE2 as an entry route and reduces ACE2 availability and activity in endothelial cells. Reduced ACE2 activity increases Ang II levels and consequently ATR1 activity in microglial cells that respond with activation of NF-κB and proinflammatory gene expression. Astrocytes respond to proinflammatory microglial mediators expanding neuroinflammation and neurodegeneration.
Reduced anti-inflammatory and antioxidant activity: Decreased ACE2 activity reduces Ang (1-7) concentration and MasR activity in astrocytes and other cell types. Reactive oxygen species and proinflammatory mediators increase in CNS parenchyma and also in brain blood vessels. Neuronal malfunction or even neuronal death may occur in this situation.
A = astrocytes; M = microglia; N = neurons.
Conclusions on the Role of Astrocytes and Microglia in SARS-CoV-2 Infection
The accumulated knowledge on human and animal CoVs supports the hypothesis that astroglia and microglia could have a major role in neurological symptoms in COVID-19 patients.
Glial Cells as SARS-CoV-2 Targets
Some clinical findings and extensive research on other CoVs show that this possibility may exist, with infected glial cells supporting productive infection or persisting as nonproductive reservoirs of SARS-CoV-2 as observed for animal CoVs (Figure 2). Astroglial-productive SARS-CoV-2 infection is unlikely, since the destruction of the astroglial network would have catastrophic effects in the CNS, together with a massive proinflammatory response due to cell death. On the other hand, the productive infection of microglia would give rise to a focal depletion of this highly heterogenic population of microglial cells and exacerbated proinflammatory response. The present clinical evidence of neurological symptoms in SARS-CoV-2 patients does not fully support these possibilities. Much more likely is that a nonproductive glial infection, even in part of glial population (i.e., perivascular), may turn astrocytes and microglia to a mild proinflammatory phenotype, causing a malfunction of astrocytes and disturbing microglial functions, with detrimental consequences for neuronal homeostasis and survival (Figure 2).
Glial Cells as Proinflammatory Effectors
It is highly probable that glial cells have an important role in initiating/expanding neuroinflammation in the SARS-CoV-2-infected brain (Figure 2). This scenario does not require that SARS-CoV-2 infects the CNS, since endothelial cells may transfer the proinflammatory signals from periphery to the CNS parenchyma activating the inflammatory response in microglia and astrocytes, worsening the clinical outcome and neurovirulence.
Glial Cells Involved in Brain RAS Alterations
SARS-CoV-2 and its predecessor SARS-CoV share the unique feature that is the binding to ACE2. Astrocytes are main players in brain RAS system, and microglia respond to increased Ang II levels secreting proinflammatory cytokines (Figure 3). Thus, downregulation in ACE2 level induced by SARS-CoV-2 could have detrimental effects both by reducing anti-inflammatory and antiapoptotic Ang (1–7) effects, exacerbating ATR1-dependent proinflammatory response and reducing brain blood flow. This may have serious consequences, not only for brain parenchyma but also for the whole organism, due to the main role of brain RAS in regions associated with cardiovascular control.
The present SARS-CoV-2 outbreak has taken the world by surprise and has demanded for rapid implementation of measures that help contain the virus, while scientists all over the world race against the pandemic to find treatments. Taking into consideration the important neurological clinical manifestations stated earlier, and the role of the different CNS cell types, gaining as much knowledge as possible from COVID-19 impact in the nervous system is essential to improve future treatment strategies and therapies.
Acknowledgments
A. J. R., V. M., and A. V. are researchers from CONICET (Argentina). We thank Dr. Carla Bonavita for proofreading the article. We deeply appreciate reviewers’ comments that significantly improved this review.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This wok was supported by grants CONICET PIP, ANPCYT PICT 2015-1451 and 2017-2203, and UBACYT.
ORCID iDs
Veronica Murta https://orcid.org/0000-0001-7830-351X
Alberto J. Ramos https://orcid.org/0000-0003-4009-6337
References
- Abbasi Pashaki P., Habibi Roudkenar M., Rahim F., Ebrahimi A. (2020). From SARS-CoV to SARS-CoV2: A potential guide to better understanding of pathophysiology of the disease and potential therapeutic modality. Eur Rev Med Pharmacol Sci, 24, 7816–7825. [DOI] [PubMed] [Google Scholar]
- Abiodun O. A., Ola M. S. (2020). Role of brain renin angiotensin system in neurodegeneration: An update. Saudi J Biol Sci, 27, 905–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A. S., Garron T., Tao X., Peng B.-H., Wakamiya M., Chan T.-S., Couch R. B., Tseng C.-T. K. (2015). Generation of a transgenic mouse model of Middle East respiratory syndrome coronavirus infection and disease. J Virol, 89, 3659–3670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alam S. B., Willows S., Kulka M., Sandhu J. K. (2020). Severe acute respiratory syndrome coronavirus-2 may be an underappreciated pathogen of the central nervous system. Eur J Neurol Advance online publication. 10.1111/ene.14442 [DOI] [PMC free article] [PubMed]
- Algahtani H., Subahi A., Shirah B. (2016). Neurological complications of Middle East respiratory syndrome coronavirus: A report of two cases and review of the literature. Case Rep Neurol Med, 2016, 3502683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Hameed F. M. (2017). Spontaneous intracranial hemorrhage in a patient with Middle East respiratory syndrome corona virus. Saudi Med J, 38, 196–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson M. A., Burda J. E., Ren Y., Ao Y., O’Shea T. M., Kawaguchi R., Coppola G., Khakh B. S., Deming T. J., Sofroniew M. V. (2016). Astrocyte scar formation aids central nervous system axon regeneration. Nature, 532, 195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arabi Y. M., Harthi A., Hussein J., Bouchama A., Johani S., Hajeer A. H., Saeed B. T., Wahbi A., Saedy A., AlDabbagh T., Okaili R., Sadat M., Balkhy H. (2015). Severe neurologic syndrome associated with Middle East respiratory syndrome corona virus (MERS-CoV). Infection, 43, 495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbour N., Côté G., Lachance C., Tardieu M., Cashman N. R., Talbot P. J. (1999. a). Acute and persistent infection of human neural cell lines by human coronavirus OC43. J Virol, 73, 3338–3350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbour N., Day R., Newcombe J., Talbot P. J. (2000). Neuroinvasion by human respiratory coronaviruses. J Virol, 74, 8913–8921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbour N., Ekandé S., Côté G., Lachance C., Chagnon F., Tardieu M., Cashman N. R., Talbot P. J. (1999. b). Persistent infection of human oligodendrocytic and neuroglial cell lines by human coronavirus 229E. J Virol, 73, 3326–3337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arroja M. M. C., Reid E., McCabe C. (2016). Therapeutic potential of the renin angiotensin system in ischaemic stroke. Exp Transl Stroke Med, 8, 8 10.1186/s13231-016-0022-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asadi-Pooya A. A., Simani L. (2020). Central nervous system manifestations of COVID-19: A systematic review. J Neurol Sci, 413, 116832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barac-Latas V., Suchanek G., Breitschopf H., Stuehler A., Wege H., Lassmann H. (1997). Patterns of oligodendrocyte pathology in coronavirus-induced subacute demyelinating encephalomyelitis in the Lewis rat. Glia, 19, 1–12. [DOI] [PubMed] [Google Scholar]
- Barres B. A. (2008). The mystery and magic of glia: A perspective on their roles in health and disease. Neuron, 60, 430–440. [DOI] [PubMed] [Google Scholar]
- Benameur K., Agarwal A., Auld S. C., Butters M. P., Webster A. S., Ozturk T., Howell J. C., Bassit L. C., Velasquez A., Schinazi R. F., Mullins M. E., Hu W. T. (2020). Encephalopathy and encephalitis associated with cerebrospinal fluid cytokine alterations and coronavirus disease, Atlanta, Georgia, USA, 2020. Emerging Infect Dis, 26, 2016–2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender S. J., Weiss S. R. (2010). Pathogenesis of murine coronavirus in the central nervous system. J Neuroimmune Pharmacol, 5, 336–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanc C. A., Rosen H., Lane T. E. (2014). FTY720 (fingolimod) modulates the severity of viral-induced encephalomyelitis and demyelination. J Neuroinflammation, 11, 138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonavia A., Arbour N., Yong V. W., Talbot P. J. (1997). Infection of primary cultures of human neural cells by human coronaviruses 229E and OC43. J Virol, 71, 800–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burda J. E., Sofroniew M. V. (2017). Seducing astrocytes to the dark side. Cell Res, 27, 726–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee D., Biswas K., Nag S., Ramachandra S. G., Das Sarma J. (2013). Microglia play a major role in direct viral-induced demyelination. Clin Dev Immunol, 2013, 510396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Churchill M., Nath A. (2013). Where does HIV hide? A focus on the central nervous system. Curr Opin HIV AIDS, 8, 165–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Churchill M. J., Wesselingh S. L., Cowley D., Pardo C. A., McArthur J. C., Brew B. J., Gorry P. R. (2009). Extensive astrocyte infection is prominent in human immunodeficiency virus-associated dementia. Ann Neurol, 66, 253–258. [DOI] [PubMed] [Google Scholar]
- Clarke L. E., Barres B. A. (2013). Emerging roles of astrocytes in neural circuit development. Nat Rev Neurosci, 14, 311–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke L. E., Liddelow S. A., Chakraborty C., Münch A. E., Heiman M., Barres B. A. (2018). Normal aging induces A1-like astrocyte reactivity. Proc Natl Acad Sci USA, 115, E1896–E1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowley T. J., Weiss S. R. (2010). Murine coronavirus neuropathogenesis: Determinants of virulence. J Neurovirol, 16, 427–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Morais S. D. B., Shanks J., Zucker I. H. (2018). Integrative physiological aspects of brain RAS in hypertension. Curr Hypertens Rep, 20, 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desforges M., Le Coupanec A., Brison E., Meessen-Pinard M., Talbot P. J. (2014). Neuroinvasive and neurotropic human respiratory coronaviruses: Potential neurovirulent agents in humans. Adv Exp Med Biol, 807, 75–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desforges M., Le Coupanec A., Dubeau P., Bourgouin A., Lajoie L., Dubé M., Talbot P. J. (2019). Human coronaviruses and other respiratory viruses: Underestimated opportunistic pathogens of the central nervous system? Viruses, 12, 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Y., He L., Zhang Q., Huang Z., Che X., Hou J., Wang H., Shen H., Qiu L., Li Z., Geng J., Cai J., Han H., Li X., Kang W., Weng D., Liang P., Jiang S. (2004). Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS-CoV) in SARS patients: Implications for pathogenesis and virus transmission pathways. J Pathol, 203, 622–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doobay M. F., Talman L. S., Obr T. D., Tian X., Davisson R. L., Lazartigues E. (2007). Differential expression of neuronal ACE2 in transgenic mice with overexpression of the brain renin-angiotensin system. Am J Physiol Regul Integr Comp Physiol, 292, R373–R381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbirt D., Mahlab-Guri K., Bezalel-Rosenberg S., Gill H., Attali M., Asher I. (2015). HIV-associated neurocognitive disorders (HAND). Isr Med Assoc J, 17, 54–59. [PubMed] [Google Scholar]
- Elkjaer M. L., Frisch T., Reynolds R., Kacprowski T., Burton M., Kruse T. A., Thomassen M., Baumbach J., Illes Z. (2019). Molecular signature of different lesion types in the brain white matter of patients with progressive multiple sclerosis. Acta Neuropathol Commun, 7, 205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewald A. C., Kiernan E. A., Roopra A. S., Radcliff A. B., Timko R. R., Baker T. L., Watters J. J. (2020). Sex- and region-specific differences in the transcriptomes of rat microglia from the brainstem and cervical spinal cord. J Pharmacol Exp Ther Advance online publication. 10.1124/jpet.120.266171 [DOI] [PMC free article] [PubMed]
- Falzarano D., de Wit E., Feldmann F., Rasmussen A. L., Okumura A., Peng X., Thomas M. J., van Doremalen N., Haddock E., Nagy L., LaCasse R., Liu T., Zhu J., McLellan J. S., Scott D. P., Katze M. G., Feldmann H., Munster V. J. (2014). Infection with MERS-CoV causes lethal pneumonia in the common marmoset. PLoS Pathog, 10, e1004250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farina C., Aloisi F., Meinl E. (2007). Astrocytes are active players in cerebral innate immunity. Trends Immunol, 28, 138–145. [DOI] [PubMed] [Google Scholar]
- Feng Y., Xia H., Bindom S. M., Lazartigues E. (2008). Neuron-targeted expression of ACE2 in the central nervous system prevents angiotensin-II-mediated hypertension. FASEB J, 22, 741.1–741.1. [Google Scholar]
- Feng Y., Xia H., Cai Y., Halabi C. M., Becker L. K., Santos R. A. S., Speth R. C., Sigmund C. D., Lazartigues E. (2010. a). Brain-selective overexpression of human Angiotensin-converting enzyme type 2 attenuates neurogenic hypertension. Circ Res, 106, 373–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Y., Xia H., Santos R. A., Speth R., Lazartigues E. (2010. b). ACE2: A new target for neurogenic hypertension. Exp Physiol, 95, 601–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrarese C., Silani V., Priori A., Galimberti S., Agostoni E., Monaco S., Padovani A., Tedeschi G., & Italian Society of Neurology (SIN). (2020). An Italian multicenter retrospective-prospective observational study on neurological manifestations of COVID-19 (NEUROCOVID). Neurol Sci, 41, 1355–1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finsterer J., Stollberger C. (2020). Update on the neurology of COVID-19. J Med Virol Advance online publication. 10.1002/jmv.26000 [DOI] [PMC free article] [PubMed]
- Gallagher P. E., Chappell M. C., Ferrario C. M., Tallant E. A. (2006). Distinct roles for ANG II and ANG-(1–7) in the regulation of angiotensin-converting enzyme 2 in rat astrocytes. Am J Physiol Cell Physiol, 290, C420–C426. [DOI] [PubMed] [Google Scholar]
- Gan R., Rosoman N. P., Henshaw D. J. E., Noble E. P., Georgius P., Sommerfeld N. (2020). COVID-19 as a viral functional ACE2 deficiency disorder with ACE2 related multi-organ disease. Med Hypotheses, 144, 110024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaunt E. R., Hardie A., Claas E. C. J., Simmonds P., Templeton K. E. (2010). Epidemiology and clinical presentations of the four human coronaviruses 229E, HKU1, NL63, and OC43 detected over 3 years using a novel multiplex real-time PCR method. J Clin Microbiol, 48, 2940–2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerrits E., Heng Y., Boddeke E. W. G. M., Eggen B. J. L. (2020). Transcriptional profiling of microglia; current state of the art and future perspectives. Glia, 68, 740–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass W. G., Subbarao K., Murphy B., Murphy P. M. (2004). Mechanisms of host defense following severe acute respiratory syndrome-coronavirus (SARS-CoV) pulmonary infection of mice. J Immunol, 173, 4030–4039. [DOI] [PubMed] [Google Scholar]
- Gonzales D. M., Fu L., Li Y., Das Sarma J., Lavi E. (2004). Coronavirus-induced demyelination occurs in the absence of CD28 costimulatory signals. J Neuroimmunol, 146, 140–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Scarano F., Martín-García J. (2005). The neuropathogenesis of AIDS. Nat Rev Immunol, 5, 69–81. [DOI] [PubMed] [Google Scholar]
- Gowrisankar Y. V., Clark M. A. (2016). Angiotensin II regulation of angiotensin-converting enzymes in spontaneously hypertensive rat primary astrocyte cultures. J Neurochem, 138, 74–85. [DOI] [PubMed] [Google Scholar]
- Gu J., et al. (2005). Multiple organ infection and the pathogenesis of SARS. J Exp Med, 202, 415–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haagmans B. L., Kuiken T., Martina B. E., Fouchier R. A. M., Rimmelzwaan G. F., van Amerongen G., van Riel D., de Jong T., Itamura S., Chan K.-H., Tashiro M., Osterhaus A. D. M. E. (2004). Pegylated interferon-alpha protects type 1 pneumocytes against SARS coronavirus infection in macaques. Nat Med, 10, 290–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamby M. E., Coppola G., Ao Y., Geschwind D. H., Khakh B. S., Sofroniew M. V. (2012). Inflammatory mediators alter the astrocyte transcriptome and calcium signaling elicited by multiple G-protein-coupled receptors. J Neurosci, 32, 14489–14510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamming I., Timens W., Bulthuis M., Lely A., Navis G., van Goor H. (2004). Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol, 203, 631–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helms J., Kremer S., Merdji H., Clere-Jehl R., Schenck M., Kummerlen C., Collange O., Boulay C., Fafi-Kremer S., Ohana M., Anheim M., Meziani F. (2020). Neurologic features in severe SARS-CoV-2 infection. N Engl J Med Advance online publication. 10.1056/NEJMc2008597 [DOI] [PMC free article] [PubMed]
- Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T. S., Herrler G., Wu N.-H., Nitsche A., Müller M. A., Drosten C., Pöhlmann S. (2020). SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell, 181, 271–280.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hou Y. J., et al. (2020). SARS-CoV-2 reverse genetics reveals a variable infection gradient in the respiratory tract. Cell, 182(2), 429–446.e14. http://www.sciencedirect.com/science/article/pii/S0092867420306759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huber G., Schuster F., Raasch W. (2017). Brain renin-angiotensin system in the pathophysiology of cardiovascular diseases. Pharmacol Res, 125(Pt A), 72–90. [DOI] [PubMed] [Google Scholar]
- Hung E. C. W., Chim S. S. C., Chan P. K. S., Tong Y. K., Ng E. K. O., Chiu R. W. K., Leung C.-B., Sung J. J. Y., Tam J. S., Lo Y. M. D. (2003). Detection of SARS coronavirus RNA in the cerebrospinal fluid of a patient with severe acute respiratory syndrome. Clin Chem, 49, 2108–2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang M., Bergmann C. C. (2018). Alpha/beta interferon (IFN-α/β) signaling in astrocytes mediates protection against viral encephalomyelitis and regulates IFN-γ-dependent responses. J Virol, 92, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai Y., Kuba K., Rao S., Huan Y., Guo F., Guan B., Yang P., Sarao R., Wada T., Leong-Poi H., Crackower M. A., Fukamizu A., Hui C.-C., Hein L., Uhlig S., Slutsky A. S., Jiang C., Penninger J. M. (2005). Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature, 436, 112–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwata-Yoshikawa N., Okamura T., Shimizu Y., Kotani O., Sato H., Sekimukai H., Fukushi S., Suzuki T., Sato Y., Takeda M., Tashiro M., Hasegawa H., Nagata N. (2019). Acute respiratory infection in human dipeptidyl peptidase 4-transgenic mice infected with Middle East respiratory syndrome coronavirus. J Virol, 93, e01818–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacomy H., Fragoso G., Almazan G., Mushynski W. E., Talbot P. J. (2006). Human coronavirus OC43 infection induces chronic encephalitis leading to disabilities in BALB/C mice. Virology, 349, 335–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasti M., Nalleballe K., Dandu V., Onteddu S. (2020). A review of pathophysiology and neuropsychiatric manifestations of COVID-19. J Neurol Advance online publication. 10.1007/s00415-020-09950-w [DOI] [PMC free article] [PubMed]
- Kanberg N., Ashton N. J., Andersson L.-M., Yilmaz A., Lindh M., Nilsson S., Price R. W., Blennow K., Zetterberg H., Gisslén M. (2020). Neurochemical evidence of astrocytic and neuronal injury commonly found in COVID-19. Neurology Advance online publication. 10.1212/WNL.0000000000010111 [DOI] [PubMed]
- Kenny A. J., Bourne A. (1991). Cellular reorganisation of membrane peptidases in Wallerian degeneration of pig peripheral nerve. J Neurocytol, 20, 875–885. [DOI] [PubMed] [Google Scholar]
- Kim J. E., Heo J. H., Kim H. O., Song S. H., Park S. S., Park T. H., Ahn J. Y., Kim M. K., Choi J. P. (2017). Neurological complications during treatment of Middle East respiratory syndrome. J Clin Neurol, 13, 227–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Király K., Kozsurek M., Lukácsi E., Barta B., Alpár A., Balázsa T., Fekete C., Szabon J., Helyes Z., Bölcskei K., Tékus V., Tóth Z. E., Pap K., Gerber G., Puskár Z. (2018). Glial cell type-specific changes in spinal dipeptidyl peptidase 4 expression and effects of its inhibitors in inflammatory and neuropatic pain. Sci Rep, 8, 3490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krasniqi S., Daci A. (2019). Role of the angiotensin pathway and its target therapy in epilepsy management. Int J Mol Sci, 20(3), 726 10.3390/ijms20030726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kremer S., et al. (2020). Neurologic and neuroimaging findings in COVID-19 patients: A retrospective multicenter study. Neurology Advance online publication. 10.1212/WNL.0000000000010112 [DOI] [PubMed]
- Kuba K., et al. (2005). A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med, 11, 875–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau K.-K., Yu W.-C., Chu C.-M., Lau S.-T., Sheng B., Yuen K.-Y. (2004). Possible central nervous system infection by SARS coronavirus. Emerging Infect Dis, 10, 342–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavi, E., & Cong, L. (2020). Type I astrocytes and microglia induce a cytokine response in an encephalitic murine coronavirus infection. Exp. Mol. Pathol, 115, 104474. doi:10.1016/j.yexmp.2020.104474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, F., Wang, Y., Yu, L., Cao, S., Wang, K., Yuan, J., et al. (2015). Viral Infection of the Central Nervous System and Neuroinflammation Precede Blood-Brain Barrier Disruption during Japanese Encephalitis Virus Infection. J. Virol, 89, 5602–5614. doi:10.1128/JVI.00143-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavi E., Cong L. (2020). Type I astrocytes and microglia induce a cytokine response in an encephalitic murine coronavirus infection. Exp Mol Pathol, 115, 104474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Moore M. J., Vasilieva N., Sui J., Wong S. K., Berne M. A., Somasundaran M., Sullivan J. L., Luzuriaga K., Greenough T. C., Choe H., Farzan M. (2003). Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature, 426, 450–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Fu L., Gonzales D. M., Lavi E. (2004). Coronavirus neurovirulence correlates with the ability of the virus to induce proinflammatory cytokine signals from astrocytes and microglia. J Virol, 78, 3398–3406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddelow S. A., Barres B. A. (2017). Reactive astrocytes: Production, function, and therapeutic potential. Immunity, 46, 957–967. [DOI] [PubMed] [Google Scholar]
- Liddelow S. A., et al. (2017). Neurotoxic reactive astrocytes are induced by activated microglia. Nature, 541(7638), 481–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Z., Chen Y., Zhang W., Chen A. F., Lin S., Morris M. (2008). RNA interference shows interactions between mouse brainstem angiotensin AT1 receptors and angiotensin-converting enzyme 2. Exp Physiol, 93, 676–684. [DOI] [PubMed] [Google Scholar]
- Lu, L., Xiong, W., Liu, D., Liu, J., Yang, D., Li, N., Mu, J., Guo, J., Li, W., Wang, G., Gao, H., Zhang, Y., Lin, M., Chen, L., Shen, S., Zhang, H., Sander, JW., Luo, J., Chen, S., & Zhou D.(2020. a). New onset acute symptomatic seizure and risk factors in coronavirus disease 2019: A retrospective multicenter study. Epilepsia, 61(6), e49–e53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu R., et al. (2020. b). Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet, 395, 565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahalaxmi I., Kaavya J., Mohana Devi S., Balachandar V. (2020). COVID-19 and olfactory dysfunction: A possible associative approach towards neurodegenerative diseases. J Cell Physiol Advance online publication. 10.1002/jcp.29937 [DOI] [PMC free article] [PubMed]
- Malone K. E., Ramakrishna C., Gonzalez J.-M., Stohlman S. A., Bergmann C. C. (2006). Glia expression of MHC during CNS infection by neurotropic coronavirus. Nidoviruses, 581, 543–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangale V., Syage A. R., Ekiz H. A., Skinner D. D., Cheng Y., Stone C. L., Brown R. M., O’Connell R. M., Green K. N., Lane T. E. (2020). Microglia influence host defense, disease, and repair following murine coronavirus infection of the central nervous system. Glia. Advance online publication. doi: 10.1002/glia.23844 [DOI] [PMC free article] [PubMed]
- Mao L., Jin H., Wang M., Hu Y., Chen S., He Q., Chang J., Hong C., Zhou Y., Wang D., Miao X., Li Y., Hu B. (2020). Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan, China. JAMA Neurol, 77(6), 1–9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7149362/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin S. E., Callen D. J. A. (2013). The magnetic resonance imaging appearance of monophasic acute disseminated encephalomyelitis: An update post application of the 2007 consensus criteria. Neuroimaging Clin N Am, 23, 245–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martina B. E. E., Haagmans B. L., Kuiken T., Fouchier R. A. M., Rimmelzwaan G. F., Van Amerongen G., Peiris J. S. M., Lim W., Osterhaus A. D. M. E. (2003). Virology: SARS virus infection of cats and ferrets. Nature, 425, 915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsushita T., Isobe N., Kawajiri M., Mogi M., Tsukuda K., Horiuchi M., Ohyagi Y., Kira J. (2010). CSF angiotensin II and angiotensin-converting enzyme levels in anti-aquaporin-4 autoimmunity. J Neurol Sci, 295, 41–45. [DOI] [PubMed] [Google Scholar]
- McCray P. B., Pewe L., Wohlford-Lenane C., Hickey M., Manzel L., Shi L., Netland J., Jia H. P., Halabi C., Sigmund C. D., Meyerholz D. K., Kirby P., Look D. C., Perlman S. (2007). Lethal infection of K18-hACE2 mice infected with severe acute respiratory syndrome coronavirus. J Virol, 81, 813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriguchi T., et al. (2020). A first case of meningitis/encephalitis associated with SARS-coronavirus-2. Int J Infect Dis, 94, 55–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murta, V., & Ferrari, C. (2016). Peripheral Inflammation and Demyelinating Diseases. Adv. Exp. Med. Biol, 949, 263–285. doi:10.1007/978-3-319-40764-7_13 [DOI] [PubMed] [Google Scholar]
- Murta, V., Farias, M. I., Pitossi, F. J., & Ferrari, C. C. (2015). Chronic systemic IL-1beta exacerbates central neuroinflammation independently of the blood-brain barrier integrity. J Neuroimmunol, 278, 30–43. doi:10.1016/j.jneuroim.2014.11.023 S0165-5728(14)00984-9 [pii] [DOI] [PubMed] [Google Scholar]
- Nagashima K., Wege H., Meyermann R., ter Meulen V. (1978). Corona virus induced subacute demyelinating encephalomyelitis in rats: A morphological analysis. Acta Neuropathol, 44, 63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagashima K., Wege H., Meyermann R., ter Meulen V. (1979). Demyelinating encephalomyelitis induced by a long-term corona virus infection in rats. A preliminary report. Acta Neuropathol, 45, 205–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Najjar S., Najjar A., Chong D. J., Pramanik B. K., Kirsch C., Kuzniecky R. I., Pacia S. V., Azhar S. (2020). Central nervous system complications associated with SARS-CoV-2 infection: Integrative concepts of pathophysiology and case reports. J Neuroinflammation, 17, 231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Netland J., Meyerholz D. K., Moore S., Cassell M., Perlman S. (2008). Severe acute respiratory syndrome coronavirus infection causes neuronal death in the absence of encephalitis in mice transgenic for human ACE2. J Virol, 82, 7264–7275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng Kee Kwong K. C., Mehta P. R., Shukla G., Mehta A. R. (2020). COVID-19, SARS and MERS: A neurological perspective. J Clin Neurosci, 77, 13–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens T., Khorooshi R., Wlodarczyk A., Asgari N. (2014). Interferons in the central nervous system: A few instruments play many tunes. Glia, 62, 339–355. [DOI] [PubMed] [Google Scholar]
- Pandey H. S., Seth P. (2019). Friends turn foe-astrocytes contribute to neuronal damage in neuroAIDS. J Mol Neurosci, 69, 286–297. [DOI] [PubMed] [Google Scholar]
- Paniz-Mondolfi A., Bryce C., Grimes Z., Gordon R. E., Reidy J., Lednicky J., Sordillo E. M., Fowkes M. (2020). Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J Med Virol, 92(7), 699–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pekny M., Pekna M., Messing A., Steinhäuser C., Lee J.-M., Parpura V., Hol E. M., Sofroniew M. V., Verkhratsky A. (2016). Astrocytes: A central element in neurological diseases. Acta Neuropathol, 131, 323–345. [DOI] [PubMed] [Google Scholar]
- Perlman S., Evans G., Afifi A. (1990). Effect of olfactory bulb ablation on spread of a neurotropic coronavirus into the mouse brain. J Exp Med, 172, 1127–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry, V. H., Cunningham, C., and Holmes, C. (2007). Systemic infections and inflammation affect chronic neurodegeneration. Nat Rev Immunol, 7, 161–7. doi:nri2015 [pii] 10.1038/nri2015 [DOI] [PubMed] [Google Scholar]
- Perlman S., Ries D. (1987). The astrocyte is a target cell in mice persistently infected with mouse hepatitis virus, strain JHM. Microb Pathog, 3, 309–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prabakaran P., Xiao X., Dimitrov D. S. (2004). A model of the ACE2 structure and function as a SARS-CoV receptor. Biochem Biophys Res Commun, 314, 235–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pryce-Roberts A., Talaei M., Robertson N. P. (2020). Neurological complications of COVID-19: A preliminary review. J Neurol, 267(6), 1870–1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raj V. S., Mou H., Smits S. L., Dekkers D. H. W., Müller M. A., Dijkman R., Muth D., Demmers J. A. A., Zaki A., Fouchier R. A. M., Thiel V., Drosten C., Rottier P. J. M., Osterhaus A. D. M. E., Bosch B. J., Haagmans B. L. (2013). Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature, 495, 251–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos A. J. (2016). Astroglial heterogeneity: Merely a neurobiological question? Or an opportunity for neuroprotection and regeneration after brain injury? Neural Regen Res, 11, 1739–1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransohoff R. M., Perry V. H. (2009). Microglial physiology: Unique stimuli, specialized responses. Annu Rev Immunol, 27, 119–145. [DOI] [PubMed] [Google Scholar]
- Román G. C., Reis J., Spencer P. S., Buguet A., Öztürk S., Wasay M., & World Federation of Neurology Environmental Neurology Specialty Group. (2020). COVID-19 international neurological registries. Lancet Neurol, 19, 484–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romero-Sánchez C. M., et al. (2020). Neurologic manifestations in hospitalized patients with COVID-19: The ALBACOVID registry. Neurology Advance online publication. 10.1212/WNL.0000000000009937 [DOI] [PMC free article] [PubMed]
- Rosciszewski G., Cadena V., Murta V., Lukin J., Villarreal A., Roger T., Ramos A. J. (2018). Toll-like receptor 4 (TLR4) and triggering receptor expressed on myeloid cells-2 (TREM-2) activation balance astrocyte polarization into a proinflammatory phenotype. Mol Neurobiol, 55, 3875–3888. [DOI] [PubMed] [Google Scholar]
- Rosciszewski G. A., Cadena V., Auzmendi J. A., Cieri M. B., Lukin J., Rossi A. R., Murta V., Villarreal A., Reinés A., Gomes F., Ramos A. J. (2019). Detrimental effects of HMGB-1 require microglial-astroglial interaction: Implications for the status epilepticus-induced neuroinflammation. Front Cell Neurosci Advance online publication. 10.3389/fncel.2019.00380; https://www.frontiersin.org/articles/10.3389/fncel.2019.00380/abstract [DOI] [PMC free article] [PubMed]
- Rothhammer V., et al. (2016). Type I interferons and microbial metabolites of tryptophan modulate astrocyte activity and central nervous system inflammation via the aryl hydrocarbon receptor. Nat Med, 22, 586–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo M. V., McGavern D. B. (2015). Immune surveillance of the CNS following infection and injury. Trends Immunol, 36, 637–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saad M., Omrani A. S., Baig K., Bahloul A., Elzein F., Matin M. A., Selim M. A. A., Al Mutairi M., Al Nakhli D., Al Aidaroos A. Y., Al Sherbeeni N., Al-Khashan H. I., Memish Z. A., Albarrak A. M. (2014). Clinical aspects and outcomes of 70 patients with Middle East respiratory syndrome coronavirus infection: A single-center experience in Saudi Arabia. Int J Infect Dis, 29, 301–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savarin C., Bergmann C. C. (2018). Fine tuning the cytokine storm by IFN and IL-10 following neurotropic coronavirus encephalomyelitis. Front Immunol, 9, 3022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Severance E. G., Dickerson F. B., Viscidi R. P., Bossis I., Stallings C. R., Origoni A. E., Sullens A., Yolken R. H. (2011). Coronavirus immunoreactivity in individuals with a recent onset of psychotic symptoms. Schizophr Bull, 37, 101–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeling, J. L., & Perry, V. H. (2009). Systemic infection and inflammation in acute CNS injury and chronic neurodegeneration: underlying mechanisms. Neuroscience, 158, 1062–1073. doi:10.1016/j.neuroscience.2008.07.031 [DOI] [PubMed] [Google Scholar]
- Shi A., Liu H., Liu L., Hu H., Wang Q., Adhikari B. (2014). Isolation, purification and molecular mechanism of a peanut protein-derived ACE-inhibitory peptide. PLoS One, 9(10), e111188 10.1371/journal.pone.0111188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofroniew M. V., Vinters H. V. (2010). Astrocytes: Biology and pathology. Acta Neuropathol, 119, 7–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soung A., Klein R. S. (2018). Viral encephalitis and neurologic diseases: Focus on astrocytes. Trends Mol Med, 24, 950–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sriramula S., Pedersen K. B., Xia H., Lazartigues E. (2017). Determining the enzymatic activity of angiotensin-converting enzyme 2 (ACE2) in brain tissue and cerebrospinal fluid using a quenched fluorescent substrate. Methods Mol Biol, 1527, 117–126. [DOI] [PubMed] [Google Scholar]
- Steardo L., Steardo L., Zorec R., Verkhratsky A. (2020). Neuroinfection may contribute to pathophysiology and clinical manifestations of COVID-19. Acta Physiol (Oxf ), 229, e13473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbarao K., McAuliffe J., Vogel L., Fahle G., Fischer S., Tatti K., Packard M., Shieh W.-J., Zaki S., Murphy B. (2004). Prior infection and passive transfer of neutralizing antibody prevent replication of severe acute respiratory syndrome coronavirus in the respiratory tract of mice. J Virol, 78, 3572–3577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun N., Grzybicki D., Castro R. F., Murphy S., Perlman S. (1995). Activation of astrocytes in the spinal cord of mice chronically infected with a neurotropic coronavirus. Virology, 213, 482–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzumura A., Lavi E., Weiss S. R., Silberberg D. H. (1986). Coronavirus infection induces H-2 antigen expression on oligodendrocytes and astrocytes. Science, 232, 991–993. [DOI] [PubMed] [Google Scholar]
- Swanson, P. A., & McGavern, D. B. (2015). Viral diseases of the central nervous system. Curr Opin Virol, 11, 44–54. doi:10.1016/j.coviro.2014.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao X., Garron T., Agrawal A. S., Algaissi A., Peng B.-H., Wakamiya M., Chan T.-S., Lu L., Du L., Jiang S., Couch R. B., Tseng C.-T. K. (2016). Characterization and demonstration of the value of a lethal mouse model of Middle East respiratory syndrome coronavirus infection and disease. J Virol, 90, 57–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trandem K., Anghelina D., Zhao J., Perlman S. (2010). Regulatory T cells inhibit T cell proliferation and decrease demyelination in mice chronically infected with a coronavirus. J Immunol, 184, 4391–4400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai L.-K., Hsieh S.-T., Chang Y.-C. (2005). Neurological manifestations in severe acute respiratory syndrome. Acta Neurol Taiwan, 14, 113–119. [PubMed] [Google Scholar]
- Tseng C.-T. K., Huang C., Newman P., Wang N., Narayanan K., Watts D. M., Makino S., Packard M. M., Zaki S. R., Chan T.-S., Peters C. J. (2007). Severe acute respiratory syndrome coronavirus infection of mice transgenic for the human Angiotensin-converting enzyme 2 virus receptor. J Virol, 81, 1162–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umapathi T., Kor A. C., Venketasubramanian N., Lim C. C. T., Pang B. C., Yeo T. T., Lee C. C., Lim P. L., Ponnudurai K., Chuah K. L., Tan P. H., Tai D. Y. H., Ang S. P. B. (2004). Large artery ischaemic stroke in severe acute respiratory syndrome (SARS). J Neurol, 251, 1227–1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N., Munster V. J. (2015). Animal models of Middle East respiratory syndrome coronavirus infection. Antiviral Res, 122, 28–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verkhratsky A., Ho M. S., Vardjan N., Zorec R., Parpura V. (2019). General pathophysiology of astroglia. Adv Exp Med Biol, 1175, 149–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virhammar J., Kumlien E., Fällmar D., Frithiof R., Jackmann S., Sköld M. K., Kadir M., Frick J., Lindeberg J., Olivero-Reinius H., Ryttlefors M., Cunningham J. L., Wikström J., Grabowska A., Bondeson K., Bergquist J., Zetterberg H., Rostami E. (2020). Acute necrotizing encephalopathy with SARS-CoV-2 RNA confirmed in cerebrospinal fluid. Neurology Advance online publication. 10.1212/WNL.0000000000010250 [DOI] [PMC free article] [PubMed]
- Wang P., Chen J., Zheng A., Nie Y., Shi X., Wang W., Wang G., Luo M., Liu H., Tan L., Song X., Wang Z., Yin X., Qu X., Wang X., Qing T., Ding M., Deng H. (2004). Expression cloning of functional receptor used by SARS coronavirus. Biochem Biophys Res Commun, 315, 439–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler D. L., Sariol A., Meyerholz D. K., Perlman S. (2018). Microglia are required for protection against lethal coronavirus encephalitis in mice. J Clin Invest, 128, 931–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2019). MERS Monthly Summary, November 2019 https://www.who.int/emergencies/mers-cov/en/
- WHO (2004). WHO guidelines for the global surveillance of severe acute respiratory syndrome (SARS) Updated recommendations October 2004. Available at: https://www.who.int/csr/resources/publications/WHO_CDS_CSR_ARO_2004_1/en/ [Google Scholar]
- WHO MERS-CoV Research Group. (2013). State of knowledge and data gaps of Middle East respiratory syndrome coronavirus (MERS-CoV) in humans. PLoS Curr, 5. doi:10.1371/currents.outbreaks.0bf719e352e7478f8ad85fa30127ddb8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Report COVID-19. (n.. d.). Coronavirus disease (COVID-19) pandemic https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- Wilton D. K., Dissing-Olesen L., Stevens B. (2019). Neuron-glia signaling in synapse elimination. Annu Rev Neurosci, 42, 107–127. [DOI] [PubMed] [Google Scholar]
- Wu Y., Xu X., Chen Z., Duan J., Hashimoto K., Yang L., Liu C., Yang C. (2020). Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun Advance online publication. 10.1016/j.bbi.2020.03.031 [DOI] [PMC free article] [PubMed]
- Xia H., Lazartigues E. (2008). Angiotensin‐converting enzyme 2 in the brain: Properties and future directions. J Neurochem, 107, 1482–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong W., et al. (2020). New onset neurologic events in people with COVID-19 infection in three regions in China. Neurology Advance online publication. 10.1212/WNL.0000000000010034 [DOI] [PubMed]
- Xu J., Sriramula S., Xia H., Moreno-Walton L., Culicchia F., Domenig O., Poglitsch M., Lazartigues E. (2017). Clinical relevance and role of neuronal AT1 receptors in ADAM17-mediated ACE2 shedding in neurogenic hypertension. Circ Res, 121, 43–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J., Zhong S., Liu J., Li L., Li Y., Wu X., Li Z., Deng P., Zhang J., Zhong N., Ding Y., Jiang Y. (2005). Detection of severe acute respiratory syndrome coronavirus in the brain: Potential role of the chemokine mig in pathogenesis. Clin Infect Dis, 41, 1089–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang C.-L., Qiu X., Zeng Y.-K., Jiang M., Fan H.-R., Zhang Z.-M. (2020. a). Coronavirus disease 2019: A clinical review. Eur Rev Med Pharmacol Sci, 24, 4585–4596. [DOI] [PubMed] [Google Scholar]
- Yang F., Shi S., Zhu J., Shi J., Dai K., Chen X. (2020. b). Analysis of 92 deceased patients with COVID-19. J Med Virol Advance online publication. 10.1002/jmv.25891 [DOI] [PMC free article] [PubMed]
- Zamanian J. L., Xu L., Foo L. C., Nouri N., Zhou L., Giffard R. G., Barres B. A. (2012). Genomic analysis of reactive astrogliosis. J Neurosci, 32, 6391–6410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng X., Li X., Chen Z., Yao Q. (2019). DPP-4 inhibitor saxagliptin ameliorates oxygen deprivation/reoxygenation-induced brain endothelial injury. Am J Transl Res, 11, 6316–6325. [PMC free article] [PubMed] [Google Scholar]
- Zhao G., Jiang Y., Qiu H., Gao T., Zeng Y., Guo Y., Yu H., Li J., Kou Z., Du L., Tan W., Jiang S., Sun S., Zhou Y. (2015). Multi-organ damage in human dipeptidyl peptidase 4 transgenic mice infected with Middle East respiratory syndrome-coronavirus. PLoS One, 10, e0145561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimprich F., Winter J., Wege H., Lassmann H. (1991). Coronavirus induced primary demyelination: Indications for the involvement of a humoral immune response. Neuropathol Appl Neurobiol, 17, 469–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zlateva K. T., Coenjaerts F. E. J., Crusio K. M., Lammens C., Leus F., Viveen M., Ieven M., Spaan W. J. M., Claas E. C. J., Gorbalenya A. E. (2013). No novel coronaviruses identified in a large collection of human nasopharyngeal specimens using family-wide CODEHOP-based primers. Arch Virol, 158, 251–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zorec R., Županc T. A., Verkhratsky A. (2019). Astrogliopathology in the infectious insults of the brain. Neurosci Lett, 689, 56–62. [DOI] [PubMed] [Google Scholar]