Abstract
Background
Coil occlusion has become the standard treatment for many ruptured aneurysms. However, specific aneurysm structures pose technical difficulties and may require the use of adjunctive neck-bridging devices, which necessitate the use of dual antiplatelet therapy. The hydrophilic polymer coating (pHPC, phenox) is a surface modification that inhibits platelet adhesion.
Objective
To present initial experience with the pCONUS HPC device as an adjunct to coil embolization for ruptured aneurysms using single antiplatelet therapy (SAPT).
Methods
All patients who were treated with the pCONUS HPC for ruptured aneurysms using SAPT were retrospectively identified. The occurrence of thromboembolic and hemorrhagic complications was recorded together with the angiographic and clinical follow-up details.
Results
Fifteen patients were identified (nine female) with a median age of 54 years (range 27–81). Six aneurysms were located at the anterior communicating artery, five at the middle cerebral artery bifurcation, two at the basilar artery bifurcation, one at the posterior communicating artery, and one involving the intradural internal carotid artery. Ten patients (66.6%) achieved modified Raymond–Roy classification I or II at post-treatment angiography, with 45.5% of patients having adequate occlusion (defined as complete occlusion or neck remnant) at follow-up. All patients received acetylsalicylic acid (ASA) as SAPT before and after the procedure. Intraprocedural thrombus formation was seen in three patients (20%), resolving in two patients after a bolus dose of eptifibatide, and one treated with mechanical aspiration. No clinical or radiological consequences were seen. There were no recurrent aneurysm ruptures. One patient died owing to cerebral vasospasm.
Conclusion
This initial clinical experience highlights the possibility and limitations of using the pCONUS HPC device in the treatment of complex ruptured aneurysm with ASA as SAPT. Randomized trials with longer follow-up in larger cohorts are underway.
Keywords: aneurysm, coil, device, intervention, stent
Introduction
Since the 1990s, endovascular treatment (EVT) with detachable coils has been a widely accepted, safe, and effective method for treating ruptured aneurysms in patients with acute subarachnoid hemorrhage (SAH).1 Beyond that, EVT has become the first-line treatment of ruptured aneurysms since the publication of the results of the International Subarachnoid Aneurysm Trial (ISAT) in 2002.2 Surgical clipping remains an option for complex aneurysms with unfavorable anatomy for coiling; however, advancements in techniques and devices have increased the number of aneurysms endovascularly treatable. Some of these devices include the pCON3US (phenox, Bochum, Germany), the PulseRider4 (Pulsar Vascular, Los Gatos, California, USA), and the eCLIPs5 (Evasc Medical Systems, Vancouver, Canada). Although stents and stent-like devices have facilitated the treatment of complex aneurysms, their use in patients with SAH remains controversial as dual antiplatelet therapy (DAPT) is needed to prevent thromboembolic complications, which may expose the patient to an increased hemorrhagic risk. Alternatively, intrasaccular devices, such as the Woven EndoBridge6 (WEB; MicroVention, Aliso Viejo, California, USA), are also a promising alternative in such cases since the use of DAPT is not mandatory.
The hydrophilic polymer coating (pHPC, phenox, Bochum, Germany) is a new glycan-based multilayer polymer that has been shown to have significant antithrombogenic properties when tested in vitro.7 8
In this retrospective study, we evaluated our initial clinical experience with the use of the pCONUS HPC device under single antiplatelet therapy (SAPT) exclusively in ruptured aneurysms, and present details of the success rate, complication rates, and clinical and angiographic findings.
Material and methods
Device description
The first generation of the pCONUS device (pCONUS1) is an electrolytically detachable laser-cut stent with a distal crown and four petals deployed inside the aneurysm with its base at the level of the aneurysm neck. The second-generation device (pCONUS2) features further design modifications aimed at improving functionality and ease of use. The device is also a laser-cut stent with a distal crown, which emanates from three centralized struts. There are six petals with radio-opaque markers to allow accurate positioning within the aneurysm. The design of the pCONUS-2 allows the crown to articulate and hence accommodate steep angles between the longitudinal axis of the parent vessel and the aneurysm, and the more substantial metal coverage centrally within the device is designed to minimize the risk of coil protrusion into the parent vessel (figure 1).
Figure 1.
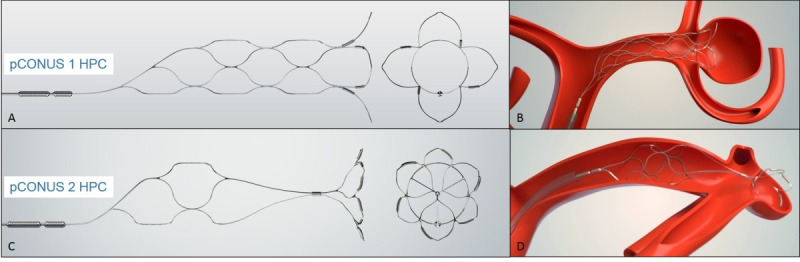
pCONUS device in its original version (pCONUS1) with four distal petals on the crown (A and B). The second version of the device (pCONUS2) has six distal petals on the crown that emanate from a central spur (C and D). The device is coated with a hydrophilic polymer coating (pHPC), which inhibits platelet adhesion.
In the pCONUS1 HPC or pCONUS2 HPC, the device is coated with a newly developed glycan-based multilayer hydrophilic polymer coating (pHPC), which inhibits platelet adhesion. The instructions for use allow the implantation under SAPT if justified by clinical circumstances.
Patient selection
We retrospectively reviewed our database of prospectively collected data to identify all patients who presented to our department with acute SAH and underwent pCONUS HPC assisted coil occlusion using SAPT.
For each patient, we recorded demographic data, clinical presentation, location and size of the ruptured aneurysm, size of the device, procedural and general complications as well as clinical and radiological follow-up data.
Endovascular treatment was carried out as an emergency measure and, whenever possible, explained to the patients, relatives, or legal representatives. The decision on the treatment strategy was in all cases based on an interdisciplinary discussion between a senior vascular neurosurgeon and a senior neurointerventionalist. Arguments in favor of EVT were poor clinical condition after SAH (Hunt and Hess IV-V) or expected surgical difficulty due to aneurysm location or morphology.
Endovascular treatment and antiplatelet regimen
All patients were treated under general anesthesia using biplane DSA systems (Axiom Artis, Siemens, Erlangen, Germany) and via either a 6 F (posterior circulation aneurysms) or an 8 F (anterior circulation aneurysms) right femoral artery approach. Standard Towne’s and lateral angiographic images, as well as rotational angiograms with 3D reconstruction, were acquired for all patients to ascertain the anatomy of the aneurysm accurately, and determine the most suitable working projection to allow visualization of the afferent and efferent arteries. Calibrated images were used to size the pCONUS HPC device correctly. In all patients, the pCONUS HPC was delivered first, and then the device crossed with the coiling catheter. The pCONUS HPC was not detached until satisfactory coiling of the aneurysm had been achieved (figure 2).
Figure 2.
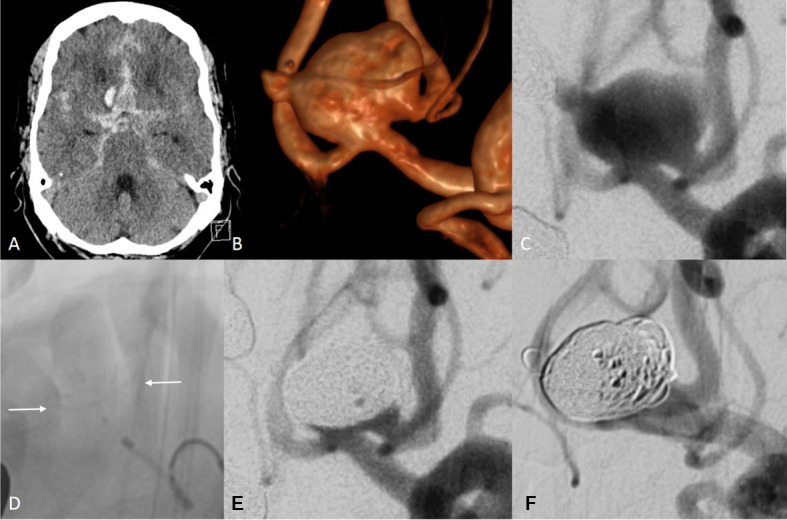
Subarachnoid hemorrhage (Fisher grade IV) on the CT scan (A) from a large wide-neck anterior communicating artery aneurysm with a likely rupture bleb (B–C). The ruptured aneurysm was treated with a 4-15-10 mm pCONUS2 HPC device ((D) white arrows point to the intra-aneurysmal pCONUS markers) and coiling with near total occlusion seen at the end of the procedure (E). Follow-up angiography performed at 6 months showed some coil compaction with a larger neck remnant (F).
As soon as the decision was made to use the pCONUS HPC and after checking the need for external ventricle drainage (EVD), a loading dose of 500 mg acetylsalicylic acid (ASA; aspirin IV 500 mg, Bayer Vital, Leverkusen, Germany) was administered intravenously before treatment. Adequate platelet response to ASA was tested 30 min after the loading dose using the Multiplate Analyzer (Roche Diagnostics, Mannheim, Germany) and the VerifyNow (Accriva, San Diego, California, USA). If there was sufficient inhibition, EVT was then initiated. If platelet inhibition was insufficient, a second loading dose of 500 mg ASA IV was given in addition to the loading dose mentioned above, and the platelet inhibition was tested again 30 min later.
Patients were temporarily heparinized during the procedure (typically with a bolus of 3000 IU unfractionated heparin IV). Additionally, all flushing solutions, including the guiding catheters and microcatheters, were heparinized (5000 IU unfractionated heparin/L). If thrombus formation occurred during the procedure, 4 mg eptifibatide (Integrilin, GlaxoSmithKline, Munich, Germany) was administrated intra-arterially through the microcatheter, and the rest of a weight-adapted bolus was then administrated intravenously.
The maintenance dose of ASA from the day after treatment (usually starting with a standard dose of 500 mg ASA IV once daily) was guided by repeated daily testing of the effectiveness using both Multiplate and VerifyNow. If there proved to be insufficient platelet inhibition with this dose (confirmed by Multiplate and VerifyNow), the maintenance dose was increased to 500 mg ASA IV twice a day. The platelet function continued to be checked every day thereafter. In the post-acute phase, and as far as the patient was extubated and able to swallow properly, conversion from IV to PO medication and reduction of the maintenance dose was initiated (monitored by daily response testing). Before discharge, a standard dose of 100 mg ASA PO twice a day was maintained for at least 3 months after treatment, followed by a daily lifetime dose of 100 mg ASA PO. In patients with poor clinical condition before discharge, in which the transition from IV to PO medication was not possible, medication was also kept IV during the rehabilitation period. The management of antiplatelet therapy is summarized in figure 3.
Figure 3.

Flow chart illustrating the management of antiplatelet medication when using pCONUS HPC in the acute setting of SAH. ARU, aspirin reaction units; ASA, acetylsalicylic acid; ASPI, acetylsalicylic platelet inhibitor; EVD, external ventricular drainage; HPC, hydrophilic polymer coating; SAH, subarachnoid hemorrhage
Data collection and follow-up
Patient age and gender, location of the aneurysms, size, status at presentation, degree of occlusion and technical and clinical complications during or after the treatment were evaluated retrospectively.
The need for an EVD and the incidence of EVD-related hemorrhagic complications during the postoperative period were recorded. Minor EVD-related hemorrhage was defined as new small areas of hyperdensity on CT scan immediately adjacent to and/or including the catheter trajectory, which did not require any surgical intervention.9 Major EVD-related hemorrhage was defined as a large hematoma requiring surgical intervention.
Neurological assessment was carried out after the treatment, at discharge, and at every follow-up. Morbidity and mortality were scored using the modified Rankin Scale (mRS).10 The initial angiographic follow-up was performed between 3 and 6 months after treatment with a further follow-up performed at 12 months. The angiographic results obtained at the end of the treatment and follow-up were recorded using the modified Raymond-Roy classification (mRRC).11
Adherence to ethical standards
All patients or legal representatives agreed to the data collection, analysis, and anonymous publication. Local ethics committee approval was obtained for the retrospective data analysis and publication (Reference No.: F-2019–023).
Results
Fifteen patients (nine female, six male) who presented with acute SAH secondary to aneurysmal rupture were treated in the acute phase with adjunctive use of the pCONUS HPC device. The median age of the patients was 54 years (range 27–81). Aneurysms ranged in size and location, with the median aneurysm dome width being 10 mm (range 3–24 mm), and the median neck width being 6 mm (range 4–10 mm). The anterior communicating artery was the most common aneurysm location (n=6), followed by the middle cerebral artery (n=5), the basilar tip (n=2), and single cases involving the posterior communicating artery, and the intradural internal carotid artery (ICA). All the patients presented with hemorrhage, with 13 patients presenting with subarachnoid hemorrhage, and the other two patients presenting with both intracerebral and subarachnoid hemorrhage. The clinical condition on presentation was good (Hunt and Hess (HH) I-II) in 5 (33.3%) patients, moderate (HH III) in 3 (20%) patients, and poor (HH IV-V) in 7 (46.7%) patients. A single pCONUS HPC device was used in all patients. Deployment and detachment of the device were successful in all cases. The results are summarized in table 1.
Table 1.
Intracranial aneurysms treated with pCONus hydrophilic polymer coating (HPC) device: clinical and anatomical findings in 15 patients
| Patient | Hunt and Hess |
Fisher score | Aneurysm location | Neck width (mm) |
Dome width (mm) |
EVD | Medication before treatment (IV ASA) |
Multiplate (ASPI)/VerifyNow (ARU) before treatment | Postmedication - from day 1 after treatment (IV ASA) |
pCONUS HPC | Complications | Immediate mRRC | FU (months) | mRRC at FU | Final mRS score |
| 1 | II | IV | BA | 3.8 | 4.5 | Y – pre | 1×500 mg | 37 U / 422 | 1×100 mg | pCONUS1 - 3-20-4 |
– | I | Dead | Dead | 6 |
| 2 | I | III | MCA | 6.5 | 7 | N | 1×500 mg | 10 U / 420 | 1×100 mg | pCONUS2 - 4-15-8 |
Stroke | II | 2 | IIIb | 0 |
| 3 | IV | IV | AcomA | 5.4 | 8.1 | Y – pre bilateral | 1×500 mg | 23 U / 413 | 1×500 mg | pCONUS2 - 4-15-6 |
– | II | 8,7 | II | 4 |
| 4 | II | III | MCA | 5 | 18 | N | 2×500 mg | 7 U / 452 | 2×500 mg | pCONUS2 - 4-15-6 |
– | II | 4,3 | II | 1 |
| 5 | II | III | AcomA | 8.3 | 12 | Y – pre | 1×500 mg | 55 U / 447 | 1×500 mg | pCONUS2 - 4-15-10 |
– | II | 6,7 | II | 3 |
| 6 | III | IV | AcomA | 4.6 | 6 | N | 1×500 mg | 20 U / 402 | 1×500 mg | pCONUS2 - 4-15-6 |
– | II | 9,1 | IIIa | 5 |
| 7 | IV | IV | MCA | 4.5 | 5 | Y – pre | 1×500 mg | 24 U / 428 | 2×500 mg | pCONUS1 - 4-20-5 |
– | IIIa | Not yet | Not yet | N/A |
| 8 | III | II | MCA | 4.7 | 12 | N | 2×500 mg | 2 U / 478 | 1×500 mg | pCONUS2 - 4-15-6 |
Thrombus formation | II | 3,4 | II | 1 |
| 9 | V | IV | MCA | 6.5 | 8 | Y – pre | 1×500 mg | 14 U / 446 | 1×500 mg | pCONUS2 - 4-15-8 |
– | IIIa | 0,7 | IIIb | 2 |
| 10 | V | IV | AcomA | 4.7 | 4.6 | Y – pre | 1×500 mg | 15 U / 562 | 1×500 mg | pCONUS1 - 4-20-5 |
Thrombus formation | II | 5,6 | II | 0 |
| 11 | V | IV | ICA | 6.7 | 24.2 | Y – pre | 2×500 mg | 14 U / 415 | 2×500 mg | pCONUS2 - 4-15-10 |
ICA dissection | IIIa | 7,9 | IIIa | 3 |
| 12 | IV | IV | AcomA | 7 | 13.8 | Y – pre | 2×500 mg | 20 U / 404 | 2×500 mg | pCONUS2 - 4-15-15 |
– | II | 5,4 | IIIa | 5 |
| 13 | II | I | BA | 8.7 | 10 | N | 1×500 mg | 18 U / 502 | 2×500 mg | pCONUS2 - 4-15-10 |
– | IIIa | 3 | IIIb | 1 |
| 14 | III | III | PcomA | 9.8 | 13 | N | 2×500 mg | 21 U / 402 | 2×500 mg | pCONUS2 - 4-15-15 |
– | IIIb | Not yet | Not yet | N/A |
| 15 | V | IV | AcomA | 6 | 3.5 | Y – pre | 2×500 mg | 18 U / 469 | 2×500 mg | pCONUS2 - 4-15-6 |
Thrombus formation | I | Not yet | Not yet | N/A |
AcomA, anterior communicating artery; ARU, aspirin reaction units; ASA, acetylsalicylic acid; ASPI, acetylsalicylic platelet inhibitor; BA, basilar artery; EVD, external ventricular drainage; FU, follow-up; ICA, internal carotid artery; IV, intravenously; MCA, middle cerebral artery; mRRC, modified Raymond-Roy classification; mRS, modified Rankin Scale; N/A, non-available; PcomA, posterior communicating artery.
Antiplatelet therapy
All patients received ASA as SAPT at a single loading dose of 500 mg IV. In six patients (40%), the second dose of 500 mg ASA IV had to be administered before treatment to achieve sufficient platelet inhibition. In the postoperative period, the maintenance dose was monitored by repeated testing. Two patients (13.3%) showed sufficient platelet inhibition with a standard dose of 1×100 mg ASA IV daily, six patients (40%) required a daily dose of 1×500 mg ASA IV, while the remaining seven patients (46.7%) required increased dose of ASA (2×500 mg ASA IV daily).
Thromboembolic complications
Procedure or device-related complications (including asymptomatic) were recorded in four cases (26.7%) and included three cases of intraprocedural thrombus formation (20%) and one postprocedural stroke (6.7%).
Intraoperative thrombus formation was seen after coil occlusion at the level of the neck coming out from the aneurysm in two patients (13.3%), both completely resolving after a bolus dose of eptifibatide (patients Nos 8 and 15). In one patient (patient No 10), thrombus formation was observed at the proximal part of the device (6.7%), which was treated with mechanical aspiration using a SOFIA catheter (MicroVention, Aliso Viejo, California, USA) as the thrombus did not change after a bolus dose of eptifibatide. There were no clinical or radiological consequences of these thrombus formations (figure 3).
Patient No 2 presented transient aphasia after the treatment due to multiple ischemic lesions confirmed by MRI, although thrombus formation was not observed angiographically during the treatment. The symptoms resolved entirely within 2 days (mRS score 0 at discharge). No case of postoperative or delayed in-stent thrombosis was observed.
Further adverse events and early angiographic results
EVD was needed for 10 patients (66.7%). In each case, the EVT was inserted before initiating the antiplatelet therapy, in one of them (patient No 3) bilaterally. Minor hemorrhage along the EVD track was noticed on postprocedural imaging in one patient (patient No 10). In this patient, postprocedural CT was performed on day 6 after the EVT. There were, however, no records of major hemorrhagic complications requiring surgical intervention. One patient (patient No 9) required a decompressive craniectomy on day 1 after treatment owing to increased intracranial pressure, which was performed under ASA IV without complications.
An iatrogenic dissection of the cervical ICA was seen in patient No 11 at the end of the procedure, which was initially treated conservatively. Seven days later, CT angiography performed owing to vasospasm showed high-grade vasospasm with a huge left-hemispheric perfusion deficit. DSA confirmed the suspected vasospasm as well as high-grade stenosis at the level of the previous ICA dissection. In order to improve the perfusion of the left cerebral hemisphere in the setting of vasospasm, the ICA was reconstructed with a single 5×30 mm Carotid Wallstent (Boston Scientific, Marlborough, Massachusetts, USA) after loading the patient with 180 mg ticagrelor via a nasogastric tube. Until that moment, the patient had been receiving a maintenance dose of 500 mg ASA IV twice a day, and no thrombus formation or stenosis was observed along with the pCONUS HPC device.
At the end of the procedure, two patients (13.3%) showed complete occlusion of the aneurysm (mRRC I), eight patients (53.3%) showed a neck remnant (mRRC II), four patients (26.7%) showed filling between the interstices of the coils (mRRC IIIa), and the remaining patient (6.7%) showed filling between the coil ball mass and the wall of the aneurysm (mRRC IIIb).
No periprocedural or postprocedural aneurysm rerupture occurred. One patient died in our cohort (6.7%) owing to vasospasm.
Clinical and angiographic follow-up
One patient died owing to cerebral vasospasm during the postoperative period. Of the surviving 14 patients, mid-term angiographic and clinical follow-up was performed in 11 patients (78.6%) at an average of 5 months after treatment (range 1–9). In three patients, imaging follow-up is still pending. Of the 11 patients with angiographic follow-up, five had neck remnants (45.5%; all of them being initially mRRC II), and recurrence was seen in the remaining six patients (54.4%; two who were initially mRRC II and four who were already initially mRRC III). No intimal hyperplasia or in-stent-thrombosis was seen at follow-up.
All patients showing incomplete occlusion at follow-up were additionally treated with coiling. Access through the implanted pCONUS was again possible, and coil retention was as reliable as it was during the initial procedure (figure 4).
Figure 4.

Ruptured aneurysm of the left middle cerebral artery (A–B). Positioning of a 4-15-6 mm pCONUS2 HPC device across the aneurysmal neck (C). After coil occlusion of the aneurysm, angiography showed a non-occlusive thrombus formation at the level of the neck (D, white arrows). This was treated with a bolus dose of eptifibatide, with complete resolution of the thrombus and no clinical or radiological evidence of infarction (E). A follow-up angiogram obtained at 3 months showed stable occlusion of the aneurysm, modified Raymond-Roy classification II (F).
All patients available for angiographic follow-up were also clinically evaluated based on mRS score. Six patients showed functional recovery after the SAH with a mRS score ≤2 (60%), and four patients presented a mRS score >2 (40%; two patients with mRS score 5, and single patients with mRS scores of 4 and 3, respectively).
Discussion
The use of stents and stent-like devices for the treatment of acutely ruptured aneurysms is still controversial even though several studies have demonstrated that the complication risk of stent-assisted coiling is comparable to both simple coiling and clipping.12 13 Recently, Roh et al compared their experience with stent-assisted and no-stent-assisted coil embolization in the treatment of ruptured aneurysms and found similar clinical and angiographic outcomes between both techniques.14 Nevertheless, some series have reported that the complications rate of stent-assisted coiling in ruptured aneurysms is much higher than that in stent-assisted coiling of unruptured aneurysms.15 16
Patients with SAH are in a hypercoagulable status with activated platelet function, and a higher tendency for clotting.17 Heparinization in combination with intravenous aspirin usually is insufficient to prevent in-stent thrombosis. DAPT is mandatory when using a stent. However, the need for DAPT remains a matter of concern as it may expose the patient to an increased hemorrhagic risk, which is even more critical in those patients with acutely ruptured aneurysms where additional interventions, such as EVD placement, decompressive craniectomy or tracheostomy, are often required.18 For all these reasons, stenting is generally avoided in the treatment of ruptured aneurysms in favor of clipping or other endovascular techniques in which DAPT would not be necessary. Recently, several devices have been specifically developed to deal with the complexity of wide-neck aneurysms, including the pCONUS, the PulseRider, and the WEB device.
The pCONUS is the most extensively used neck-bridging device. Several publications have examined the use of this device in both ruptured and unruptured aneurysms. A recently performed meta-analysis showed that intracranial aneurysms could be treated with the pCONUS device with a technical success rate of 100% and no technical complications.3 Perioperative morbidity and mortality rates were low (7% and 0%, respectively). So far, only one series has focused on the use of the pCONUS exclusively in acutely ruptured aneurysms.19 In that series of 21 patients, intraoperative complications without permanent morbidity were seen in two patients (one thromboembolic and one hemorrhagic).
Similar to the pCONUS, the PulseRider device also bridges the aneurysm neck. Although the official recommendation for its use is with DAPT, it has been hypothesized that it has a lower risk of thromboembolic complications as the device has 90% less metal on the parent artery than using Y-stenting.20 However, Folzenlogen et al presented a small series of four ruptured basilar artery aneurysms treated acutely with the PulseRider and observed two cases of non-occlusive thrombus formation during coiling (50%), although the patients received DAPT before treatment.21
The WEB is an intrasaccular alternative developed for the treatment of wide-neck aneurysms without the need for antiplatelet therapy (APT), which makes it a promising option in SAH. However, there is no consensus about the use of APT in ruptured aneurysms. Van Rooij et al reported no use of anti-aggregation during or after treatment in their series of 100 ruptured aneurysms treated with the WEB,22 whereas Liebig et al reported 44% use of 250–500 mg of ASA during the intervention, and 38.5% and 13.5% use of either SAPT or DAPT after treatment.23 Thromboembolic complications were seen in 9% and 6.4% of the patients, respectively.
Flow diversion has also emerged as an alternative treatment option of acutely ruptured aneurysms. However, the use of flow diversion in patients with SAH has been limited by the need for DAPT, which may increase the risk of hemorrhagic complications. One recent meta-analysis reported a 9% rate of hemorrhagic complications, and a 5% rate of ischemic complications,24 and another meta-analysis reported rates of thromboembolic and hemorrhagic complications of 8% and 7%, respectively.25
The development of low-thrombogenic devices with a reduced need for APT may represent a leap forward for the EVT of intracranial aneurysms, especially ruptured aneurysms. However, and despite numerous efforts, it has not yet been possible to develop optimized antithrombogenic vascular implants. Phosphorylcholine and pHPC are probably the most promising candidates.26 pHPC is a glycan-based hydrophilic multilayer polymer coating, which can be applied to nitinol surfaces. It is designed to mimic the biological properties of the glycocalyx, the coverage that can be found on the luminal surface of the endothelium of the arterial wall, making the coated surface hydrophilic and, consequently, less thrombogenic.7 In vivo studies have shown that the pHPC has no pharmaceutical effect and is biocompatible in both dogs and rabbits, with no evidence of acute inflammatory response.27–29 These in vivo studies comparing coated and uncoated devices showed no difference in the rate of neo-endothelialization, which implies that pHPC reduces the thrombogenicity of the device but does not inhibit its endothelialization. Until now, only one series has reported the clinical use of pHPC. Bhogal et al reported the use of the p48MW HPC in treating five patients with unruptured aneurysms using only prasugrel as SAPT. They reported no thromboembolic complications while one patient experienced a minor hemorrhage from the treated aneurysm 2 weeks postoperatively.30
Whether the pCONUS device itself will be superior, inferior, or equal to other treatment modalities remains unclear, as the rate of adequate occlusion (defined as complete occlusion or neck remnant) at follow-up in our series was low (45.5% of the aneurysms). This rate is lower than shown with the meta-analysis of Sorenson et al, where the late-term (at last imaging follow-up) complete occlusion rate was 60% (95% CI 52% to 69%). A possible explanation may be the larger dome-to-neck ratio of the aneurysms included in our series (mean dome-to-neck ratio 1.6 and 1.45, respectively) and the level of complexity of the included aneurysms, since five aneurysms showed residual filling at the end of the procedure (33.3%). Another explanation may be that no dense coil packing was achieved in all the patients owing to prompt thrombosis of the sac. This loose packing, added to higher dose of ASA during the post-acute period, may lead to early reperfusion of aneurysms previously occluded (eg, patient No 2, figure 5). However, our study showed that the pCONUS HPC can be used under SAPT with ASA in ruptured aneurysms. Although the overall rate of thromboembolic complications in our series was high (26.7%), these complications consisted mainly of minor thromboembolic events, with three intraprocedural thrombus formations and one patient showing transient symptoms after treatment, none of which resulted in permanent clinical sequelae. No intraprocedural aneurysmal ruptured occurred, and most importantly, no rerupture or other hemorrhagic complications occurred during the postprocedural period. A recent systematic review and meta-analysis, including more than 2000 patients, demonstrated that the overall incidence of DWI positive for thromboembolic events following EVT of intracranial aneurysms is approximately 50%, with no significant difference between coiling with and without adjunct devices.31 Additionally, Chalouhi et al reported the results of 508 patients with 552 aneurysms treated with stent-assisted coiling. Forty-seven patients (9%) were treated in the setting of SAH. They showed that the setting of acutely ruptured aneurysms was associated with higher hemorrhagic and thromboembolic complications compared with that of unruptured aneurysms, with overall complications seen in 25% of patients (morbi-mortality 12.7%) and 4.7% (morbi-mortality 1.9%) respectively.16
Figure 5.

Subarachnoid hemorrhage (Fisher grade III) on a CT scan (A) from a wide-neck bifurcation aneurysm of the left middle cerebral artery (B). Positioning of a 4-15-8 mm pCONus 2 hydrophilic polymer coating device across the aneurysmal neck (C). Angiographic run after deployment of two coils showed occlusion of the distal sac of the aneurysm with a neck remnant (D). No further coiling was then possible. Follow-up performed at 3 months showed reperfusion of the aneurysm (E), which was re-treated with coils (F).
The intravenous application of ASA has been shown to be safe during EVT of both ruptured and unruptured aneurysms, with a significant reduction of thromboembolic events without increasing intraoperative bleedings.32 ASA has also the advantage in that it can be administered intravenously in many countries, which may be useful in patients with SAH who usually are intubated and have decreased enteral motility and absorption.33 34 However, the accelerated platelet function recovery created as a consequence of a stressful state, such as SAH, may lead to suboptimal platelet inhibition to ASA and explains why increased doses were required in all but two patients in our series to maintain an adequate platelet inhibition after treatment.35 Cangrelor could also be suitable for the stent-assisted coiling of ruptured aneurysms under SAPT as it is the only P2Y12 inhibitor available in IV form. Its 'on–off' activity (rapid onset and offset of action) makes it an attractive alternative, but the need for careful management to guarantee a continuous IV infusion and the high price are known drawbacks.36
Our study has several limitations, including its single-center retrospective design and the relatively small number of patients. Selection bias is seen in the clinical severity of the patients and the complexity of the aneurysms, which may confound the evaluation of clinical outcomes. These data are considered preliminary, and further investigation is necessary to evaluate the safety and efficacy of SAPT in the setting of pCONUS HPC implantation.
Conclusion
In this small initial series, the pCONUS HPC was used to treat acutely ruptured aneurysms with only ASA as SAPT. Overall, the pCONUS HPC appears to be a suitable treatment option for complex aneurysms with unfavourable anatomy for coiling. However, thromboembolic events remain a problem and adequate management of the SAPT before and after treatment is still essential. Large registries and randomized trials examining safety and efficacy with longer clinical and angiographic follow-up are underway.
Footnotes
Twitter: @marta__aguilar
Contributors: Conceptualization: MAP, HH. Data collection: MAP, MA, VH. Investigation: MAP, MA, VH. Supervision: HB, OG, HH. Angiographic results assessment: CW. Writing – original draft: MAP, HH. Writing – review, editing: CW, OG, HB, HH.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: MAP and VH have a consulting agreement with phenox GmbH. HH is co-founder and shareholder of phenox GmbH.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No data are available.
References
- 1. Siddiq F, Chaudhry SA, Tummala RP, et al. . Factors and outcomes associated with early and delayed aneurysm treatment in subarachnoid hemorrhage patients in the United States. Neurosurgery 2012;71:670–8. 10.1227/NEU.0b013e318261749b [DOI] [PubMed] [Google Scholar]
- 2. Molyneux A, Kerr R, Stratton I, et al. . International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 2002;360:1267–74. 10.1016/S0140-6736(02)11314-6 [DOI] [PubMed] [Google Scholar]
- 3. Sorenson TJ, Iacobucci M, Murad MH, et al. . The pCONUS bifurcation aneurysm implants for endovascular treatment of adults with intracranial aneurysms: a systematic review and meta-analysis. Surg Neurol Int 2019;10:24 10.4103/sni.sni_297_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Spiotta AM, Derdeyn CP, Tateshima S, et al. . Results of the answer trial using the PulseRider for the treatment of broad-necked, bifurcation aneurysms. Neurosurgery 2017;81:56–65. 10.1093/neuros/nyx085 [DOI] [PubMed] [Google Scholar]
- 5. Chiu AH, De Vries J, O'Kelly CJ, et al. . The second-generation eCLIPs endovascular clip system: initial experience. J Neurosurg 2018;128:482–9. 10.3171/2016.10.JNS161731 [DOI] [PubMed] [Google Scholar]
- 6. Tau N, Sadeh-Gonik U, Aulagner G, et al. . The Woven EndoBridge (WEB) for endovascular therapy of intracranial aneurysms: update of a systematic review with meta-analysis. Clin Neurol Neurosurg 2018;166:110–5. 10.1016/j.clineuro.2018.01.025 [DOI] [PubMed] [Google Scholar]
- 7. Lenz-Habijan T, Bhogal P, Peters M, et al. . Hydrophilic stent coating inhibits platelet adhesion on stent surfaces: initial results in vitro. Cardiovasc Intervent Radiol 2018;41:1779–85. 10.1007/s00270-018-2036-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lenz-Habijan T, Brodde M, Kehrel BE, et al. . Comparison of the thrombogenicity of a bare and antithrombogenic coated flow diverter in an in vitro flow model. Cardiovasc Intervent Radiol 2020;43:140–6. 10.1007/s00270-019-02307-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Maniker AH, Vaynman AY, Karimi RJ, et al. . Hemorrhagic complications of external ventricular drainage. Neurosurgery 2006;59:ONS419–24. 10.1227/01.NEU.0000222817.99752.E6 [DOI] [PubMed] [Google Scholar]
- 10. Wilson JTL, Hareendran A, Grant M, et al. . Improving the assessment of outcomes in stroke: use of a structured interview to assign grades on the modified Rankin Scale. Stroke 2002;33:2243–6. 10.1161/01.str.0000027437.22450.bd [DOI] [PubMed] [Google Scholar]
- 11. Raymond J, Guilbert F, Weill A, et al. . Long-term angiographic recurrences after selective endovascular treatment of aneurysms with detachable coils. Stroke 2003;34:1398–403. 10.1161/01.STR.0000073841.88563.E9 [DOI] [PubMed] [Google Scholar]
- 12. Frontera JA, Moatti J, de los Reyes KM, et al. . Safety and cost of stent-assisted coiling of unruptured intracranial aneurysms compared with coiling or clipping. J Neurointerv Surg 2014;6:65–71. 10.1136/neurintsurg-2012-010544 [DOI] [PubMed] [Google Scholar]
- 13. Hong Y, Wang Y-J, Deng Z, et al. . Stent-assisted coiling versus coiling in treatment of intracranial aneurysm: a systematic review and meta-analysis. PLoS One 2014;9:e82311 10.1371/journal.pone.0082311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Roh H, Kim J, Bae H, et al. . Comparison of stent-assisted and no-stent coil embolization for safety and effetiveness in the treatment of ruptured intracranial aneuryms. J Neurosurg 2019;30:1–7. [DOI] [PubMed] [Google Scholar]
- 15. Bechan RS, Sprengers ME, Majoie CB, et al. . Stent-assisted coil embolization of intracranial aneurysms: complications in acutely ruptured versus unruptured aneurysms. AJNR Am J Neuroradiol 2016;37:502–7. 10.3174/ajnr.A4542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chalouhi N, Jabbour P, Singhal S, et al. . Stent-assisted coiling of intracranial aneurysms: predictors of complications, recanalization, and outcome in 508 cases. Stroke 2013;44:1348–53. 10.1161/STROKEAHA.111.000641 [DOI] [PubMed] [Google Scholar]
- 17. Perez P, Lukaszewicz A-C, Lenck S, et al. . Platelet activation and aggregation after aneurysmal subarachnoid hemorrhage. BMC Neurol 2018;18:57 10.1186/s12883-018-1062-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bodily KD, Cloft HJ, Lanzino G, et al. . Stent-assisted coiling in acutely ruptured intracranial aneurysms: a qualitative, systematic review of the literature. AJNR Am J Neuroradiol 2011;32:1232–6. 10.3174/ajnr.A2478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pérez MA, Bhogal P, Moreno RM, et al. . Use of the pCONus as an adjunct to coil embolization of acutely ruptured aneurysms. J Neurointerv Surg 2017;9:39–44. 10.1136/neurintsurg-2016-012508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cardiva Pulse rider. Available: https://www.cardiva.com/products/pulse-rider-2/?lang=en
- 21. Folzenlogen Z, Seinfeld J, Kubes S, et al. . Use of the PulseRider device in the treatment of ruptured intracranial aneurysms: a case series. World Neurosurg 2019;127:e149–54. 10.1016/j.wneu.2019.03.003 [DOI] [PubMed] [Google Scholar]
- 22. van Rooij SBT, Peluso JP, Sluzewski M, et al. . The new low-profile web 17 system for treatment of intracranial aneurysms: first clinical experiences. AJNR Am J Neuroradiol 2018;39:859–63. 10.3174/ajnr.A5608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Liebig T, Kabbasch C, Strasilla C, et al. . Intrasaccular flow disruption in acutely ruptured aneurysms: a multicenter retrospective review of the use of the web. AJNR Am J Neuroradiol 2015;36:1721–7. 10.3174/ajnr.A4347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Madaelil TP, Moran CJ, Cross DT, et al. . Flow diversion in ruptured intracranial aneurysms: a meta-analysis. AJNR Am J Neuroradiol 2017;38:590–5. 10.3174/ajnr.A5030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Cagnazzo F, di Carlo DT, Cappucci M, et al. . Acutely ruptured intracranial aneurysms treated with flow-diverter stents: a systematic review and meta-analysis. AJNR Am J Neuroradiol 2018;39:1669–75. 10.3174/ajnr.A5730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Henkes H, Bhogal P, Aguilar Pérez M, et al. . Anti-thrombogenic coatings for devices in neurointerventional surgery: case report and review of the literature. Interv Neuroradiol 2019;25:619–27. 10.1177/1591019919858000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Martínez Moreno R, Bhogal P, Lenz-Habijan T, et al. . In vivo canine study of three different coatings applied to p64 flow-diverter stents: initial biocompatibility study. Eur Radiol Exp 2019;3:3 10.1186/s41747-018-0084-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bhogal P, Lenz-Habijan T, Bannewitz C, et al. . The pCONus HPC: 30-day and 180-day in vivo biocompatibility results. Cardiovasc Intervent Radiol 2019;42:1008–15. 10.1007/s00270-019-02202-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lenz-Habijan T, Bhogal P, Bannewitz C, et al. . Prospective study to assess the tissue response to HPC-coated p48 flow diverter stents compared to uncoated devices in the rabbit carotid artery model. Eur Radiol Exp 2019;3:47 10.1186/s41747-019-0128-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bhogal P, Bleise C, Chudyk J, et al. . The p48_HPC antithrombogenic flow diverter: initial human experience using single antiplatelet therapy. J Int Med Res 2020;48:030006051987958 10.1177/0300060519879580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bond KM, Brinjikji W, Murad MH, et al. . Diffusion-weighted imaging-detected ischemic lesions following endovascular treatment of cerebral aneurysms: a systematic review and meta-analysis. AJNR Am J Neuroradiol 2017;38:304–9. 10.3174/ajnr.A4989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ries T, Buhk J-H, Kucinski T, et al. . Intravenous administration of acetylsalicylic acid during endovascular treatment of cerebral aneurysms reduces the rate of thromboembolic events. Stroke 2006;37:1816–21. 10.1161/01.STR.0000226933.44962.a6 [DOI] [PubMed] [Google Scholar]
- 33. Soppi V, Kokki H, Koivisto T, et al. . Early-phase pharmacokinetics of enteral and parenteral nimodipine in patients with acute subarachnoid haemorrhage – a pilot study. Eur J Clin Pharmacol 2007;63:355–61. 10.1007/s00228-007-0267-7 [DOI] [PubMed] [Google Scholar]
- 34. Lucena AFde, Tibúrcio RV, Vasconcelos GC, et al. . Influence of acute brain injuries on gut motility. Rev Bras Ter Intensiva 2011;23:96–103. [PubMed] [Google Scholar]
- 35. Lordkipanidzé M, Harrison P. Aspirin twice a day keeps new COX-1 at bay. J Thromb Haemost 2012;10:1217–9. 10.1111/j.1538-7836.2012.04764.x [DOI] [PubMed] [Google Scholar]
- 36. Abdennour L, Sourour N, Drir M, et al. . Preliminary experience with cangrelor for endovascular treatment of challenging intracranial aneurysms. Clin Neuroradiol 2019. 10.1007/s00062-019-00811-2. [Epub ahead of print: 15 Jul 2019]. [DOI] [PubMed] [Google Scholar]


