Dear Editor:
The incidence of thyroid cancer in the United States increased exponentially between 1974 and 2013, at a rate of 3.6% per year (1). Rates of thyroid cancer diagnosis have been found to be highly sensitive to clinical behavior, such as how widely diagnostic imaging is used. This was most clearly demonstrated by the South Korean experience, where screening asymptomatic persons with thyroid ultrasound led to a nearly 15-fold surge in thyroid cancer incidence for an 18-year period (1993–2011), and subsequently in 2014, a rapid decrease of 30% after public education on overdiagnosis and overtreatment (2). In the United States, the incidence of thyroid cancer plateaued for the first time in 2014–2016, possibly reflecting changes in diagnostic intensity (3). In 2009, the American Thyroid Association (ATA) clinical practice guidelines first recommended against biopsy of most subcentimeter or small, radiographically low-risk thyroid nodules (4). Subsequently, in 2015, ATA published revised guidelines further refining this recommendation (5). In this study, we examined if thyroid cancer incidence in the United States has changed in recent years.
The Weill Cornell Medicine Institutional Review Board deemed this study exempt from review. Annual thyroid cancer incidence (all histological types, stratified by size) between 2000 and 2017 was obtained from the Surveillance, Epidemiology, and End Results (SEERs) 18 registry using SEER*Stat (National Cancer Institute). SEER-18 captures cancers diagnosed in ∼27% of the U.S. population. Segmented log-linear regression was used to identify breakpoints in incidence trends and mean annual percentage change (APC) over time segments. p-Values represent two-tailed probabilities of the t-distribution of APC, including 0.
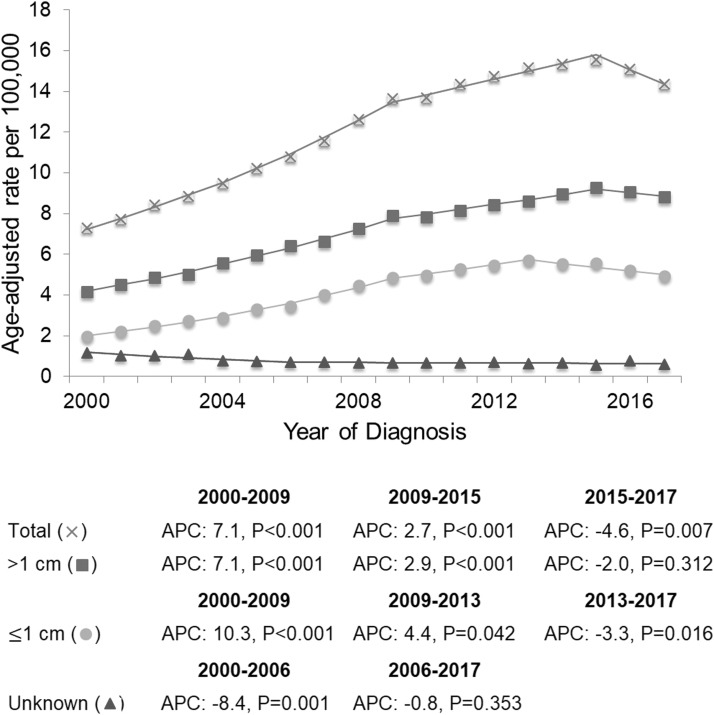
Thyroid cancer incidence (Fig. 1) increased from 7.5 per 100,000 (age-adjusted to the 2000 U.S. population) in 2000 to 13.5 per 100,000 in 2009 (APC: 7.1%, 95% confidence interval [CI 6.8–7.5%], p < 0.001). The rate of increase slowed from 2009 to 2015 (APC: 2.7% [CI 2.0–3.4%], p < 0.001), reaching an incidence of 14.9 per 100,000, and for the first time, decreased at a statistically significant rate from 2015 to 2017 (APC: −4.6% [CI −7.5% to −1.6%], p = 0.007), reaching an incidence of 13.7 per 100,000. After stratifying by size, a statistically significant decrease was seen in cancers ≤1 cm from 2013 to 2017 (APC: −3.3 [CI −5.8% to −0.8%], p = 0.016), but not in cancers >1 cm from 2015 to 2017 (APC: −2.0 [CI −6.0% to 2.2%], p = 0.312).
FIG. 1.
Thyroid cancer incidence per 100,000 (age-adjusted to the 2000 U.S. population) from the U.S. Surveillance, Epidemiology, and End Results 18 registry, 2000–2017. Individual data markers represent annual thyroid cancer incidence. Lines represent trends in thyroid cancer incidence identified by segmented log-linear regression. p-Values represent two-tailed significance tests of APC against a null hypothesis of zero change. APC, annual percentage change.
After three decades of exponential growth, for the first time, thyroid cancer incidence in the United States has begun to decrease at a statistically significant rate. We caution that observational data alone cannot rule out changes in environmental or other risk factors as causes for these changes. However, the temporal relationship with recent clinical management guidelines (4,5), and the similar reversal of trends in South Korea (2), suggest that changing clinical practices are likely to have led to the recent decline in thyroid cancer diagnoses. A similar reversal was observed with prostate cancer incidence in the 1990s, after adoption and subsequent decrease of widespread prostate-specific antigen screening (6). The reclassification of some cancers as noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) in 2016 may also have contributed to some of the decrease in incidence in the final year of the study (7). In addition, the inclusion of active surveillance of small cancers as an acceptable alternative to surgery in the 2015 ATA guidelines may also have begun to affect some biopsy decisions for small nodules, although the impact of this is not yet known.
The contemporary trends in thyroid cancer incidence parallel the introduction of radiographic features and size as risk-stratification criteria. Future data will help establish if these declining trends remain durable as clinical practice continues to evolve.
Author Disclosure Statement
The Morris laboratory receives research funding from Illumina, Inc. and AstraZeneca for research unrelated to this study.
Funding Information
No funding was received for the preparation of this manuscript.
References
- 1. Lim H, Devesa SS, Sosa JA, Check D, Kitahara CM. 2017. Trends in thyroid cancer incidence and mortality in the United States, 1974–2013. JAMA 317:1338–1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ahn HS, Welch HG. 2015. South Korea's thyroid-cancer “epidemic”—turning the tide. N Engl J Med 373:2389–2390 [DOI] [PubMed] [Google Scholar]
- 3. Powers AE, Marcadis AR, Lee M, Morris LG, Marti JL. 2019. Changes in trends in thyroid cancer incidence in the United States, 1992 to 2016. JAMA 322:2440–2441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM. 2009. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19:1167–1214 [DOI] [PubMed] [Google Scholar]
- 5. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M. 2016. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26:1–133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Etzioni R, Penson DF, Legler JM, Di Tommaso D, Boer R, Gann PH, Feuer EJ. 2002. Overdiagnosis due to prostate-specific antigen screening: lessons from U.S. prostate cancer incidence trends. J Natl Cancer Inst 94:981–990 [DOI] [PubMed] [Google Scholar]
- 7. Nikiforov YE, Seethala RR, Tallini G, Baloch ZW, Basolo F, Thompson LDR, Barletta JA, Wenig BM, Ghuzlan AA, Kakudo K, Giordano TJ, Alves VA, Khanafshar E, Asa SL, El-Naggar AK, Gooding WE, Hodak SP, Lloyd RV, Maytal G, Mete O, Nikiforova MN, Nosé V, Papotti M, Poller DN, Sadow PM, Tischler AS, Tuttle RM, Wall KB, LiVolsi VA, Randolph GW, Ghossein RA. 2016. Nomenclature revision for encapsulated follicular variant of papillary thyroid carcinoma: a paradigm shift to reduce overtreatment of indolent tumors. JAMA Oncol 2:1023–1029 [DOI] [PMC free article] [PubMed] [Google Scholar]