Abstract
Background: Group interventions are effective for addressing the transition from cancer treatment to survivorship but are not widely available outside of urban areas. In addition, minimal training is available for group facilitators outside of the mental healthcare discipline. Telehealth as a medium can facilitate conversation and interactive learning and make learning accessible to individuals in areas that lack resources for traditional classroom teaching. Little is known, however, regarding the feasibility and acceptability of a telehealth training program for group leaders. This project aimed to investigate the utility of a telehealth training program for the delivery of a copyrighted, manualized psychosocial group intervention, Cancer Transitions: Moving Beyond Treatment. Materials and Methods: Nine group leaders attended one in-person orientation, four telehealth training classes, and four telehealth supervision sessions, completing self-report measures of content knowledge, quality satisfaction, and self-confidence. Following the completion of their last Cancer Transitions facilitation, group leaders participated in a focus group to provide qualitative feedback regarding their experiences in training for and leading the respective groups in eight urban and rural North Carolina communities. Results: Group leaders rated the training program highly across the domains of content knowledge, quality satisfaction, and self-confidence. Satisfaction with the technology itself was equivocal. Conclusions: Telehealth represents a feasible avenue for training and supporting leaders of psychosocial interventions. In addition, telehealth is particularly well suited to the need for training group leaders in areas outside urban centers or academic communities.
Key words: : cancer survivorship, group, training, telehealth
Introduction
The number of patients completing treatment for cancer worldwide has grown significantly, with estimates that the United States alone is home to nearly 14 million cancer survivors.1 Delivering effective healthcare services to survivors requires attention to the long-term effects of cancer and its treatment on patients as well as addressing the psychosocial needs of underserved and disadvantaged populations.2 An important step toward achieving these priorities is to provide targeted training and support for community-based providers of cancer survivorship care.3,4
In general, group interventions have proven to be a cost-effective venue for offering a number of healthcare services across cancer populations.5–7 However, despite the accumulating evidence of the effectiveness of educational, wellness, and psychosocial programs for patients during and after cancer treatment,8–10 the delivery of these services for most patients remains woefully inadequate.11 Additionally, although group healthcare programs may be typically offered in large cancer centers and academic hospital settings, these services are not accessible by the large majority of American cancer survivors receiving their cancer care in rural areas.12
One factor potentially limiting the accessibility of group interventions to cancer patients is the minimal training available for group leaders (GLs) of educational and psychosocial interventions.13–15 One literature review found no publications describing empirically based trainings or specific interventions for cancer support GLs; the majority of resources were limited to written guides, books, manuals, and Web-based information resources.16 A further challenge to GLs administering interventions in the area of cancer treatment and survivorship is the need for knowledge or expertise beyond the discipline in which they were trained. Oncology nurses, for example, are trained to provide patients with cancer-related information but often lack experience and confidence managing group dynamics. In contrast, mental health providers are typically trained to lead psychoeducational groups but may not feel prepared to address cancer-specific aspects of survivorship. The inclusion of content experts (e.g., dieticians, medical specialists, fitness experts, and mental health professionals)17 in group interventions can address this need for a broad knowledge and skills base, but such a range of expertise may not be available in settings outside academic institutions or urban centers.
Recent literature highlights the areas GLs feel less equipped to manage in their work with cancer patients and survivors.18 Specific topics identified include developing leader behaviors important for successful group facilitation, addressing pessimism or negative thinking, preventing personal burnout, establishing the credibility of the group with relevant community health services, managing the isolation of running a group in a rural area, and attending to ethical or legal issues (such as confidentiality).16,18 Providing such training, facilitating development, and sustaining effective leaders as they work in communities is necessary to optimize the benefits patients receive from such interventions during survivorship.19
Providers from multiple disciplines express preferences for ongoing education and training. Telehealth has received growing attention for its potential to provide specialized education from a distance.20,21 One investigation with a sample of physical therapists learning five hand assessment skills found no significant difference between participants being taught in-person and those learning via telehealth in the mastery of skills, although there were significant differences between those learning through self-study and those in in a group format (either in-person or a telehealth group).22 Another study of the videoconference delivery of a course for radiology residents at multiple training sites suggested that this medium facilitated adequate conversation and interactive learning and made learning accessible to trainees at centers that lacked the resources for traditional classroom teaching.23
With these examples in mind, we examined the potential of telehealth to provide accessible and targeted training for group facilitation through the use of a brief, structured didactic and supervision model used in psychotherapy training. In the following discussion, we describe the development and implementation of a telehealth program to train GLs to deliver a manualized intervention for cancer survivors.
Materials and Methods
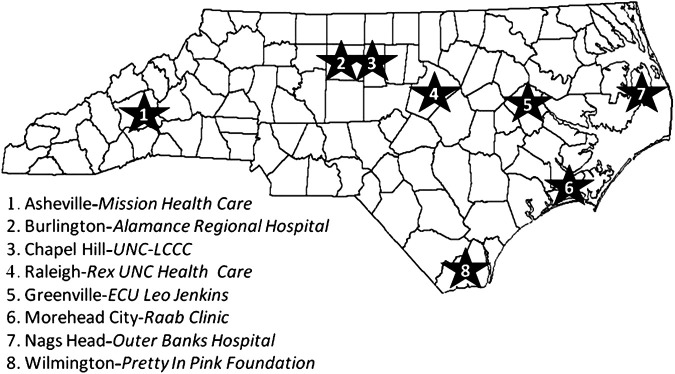
This proof-of-concept study was carried out between August 2011 and August 2012 and was approved by the Institutional Review Board of the University of North Carolina at Chapel Hill (UNC-CH). The project was based at UNC-CH with eight satellite sites serving 10 counties throughout North Carolina (Fig. 1). GLs from the study sites were recruited by community outreach coordinators with the UNC-CH Lineberger Comprehensive Cancer Center's Survivorship Program.
Fig. 1.
Study sites. Group facilitators in eight counties in North Carolina benefited from the Cancer Transitions telehealth training program. ECU, Eastern Carolina University; UNC, University of North Carolina; UNC-LCCC, University of North Carolina Lineberger Comprehensive Cancer Center.
Cancer Transitions: Moving Beyond Treatment (CT), a copyrighted program, was chosen for the intervention. CT is a structured and manualized group psychoeducational intervention developed to help survivors transition from active cancer treatment to posttreatment care that has been evaluated in multiple sites in the United States and Canada by the Cancer Support Community and LIVESTRONG.24 The closed group program is delivered in six 2½-h meetings, with dual aims to educate and empower survivors in the first 2 years posttreatment to take control of their health management through improving health behaviors and interpersonal communications with their healthcare team.25
Participants
Ten GLs were recruited, and nine completed the training program from eight sites (one site had two GLs who co-facilitated the CT program). Table 1 summarizes the characteristics of this group. Travel expenses to the in-person training were reimbursed, and those completing the 24-week study received $500 compensation for their time.
Table 1.
Group Leader Demographics
| GROUP LEADERS (N=9) | |
|---|---|
| Median (range) age (years) | 52 (43–64) |
| Race | |
| White | 9 (100%) |
| Other | 0 (0%) |
| Education | |
| High school/GED or less | 1 (11%) |
| Technical/vocational school | 0 (0%) |
| College graduate | 2 (22%) |
| Graduate degree | 6 (67%) |
| Previous/concurrent support group experience | 6 (67%) |
Group leaders were all female, with varied education and previous group experiences.
Technology
Videoconferencing was conducted on the Polycom™ (San Jose, CA) platform. Polycom technology allows meeting attendees to see, in mosaic fashion, all who are participating. Trainers at UNC-CH connected via computer and a large flat screen monitor; CT GLs connected on iPad® (Apple, Cupertino, CA) tablets from either their home or worksite. A back-up conference line was provided for GLs who had no Internet access at the meeting time or experienced connection difficulties, and each training session was recorded and accessible to GLs for review. All supplementary materials were e-mailed to GLs in anticipation of the training as the screen view was preserved for face images. GLs completed all study measures on the iPads through Qualtrics (Provo, UT) software licensed to UNC-CH (2013). In addition, a project Web site was created for GLs to access materials and share information or comments, and GLs had contact information for the project director and supervisors for between-session needs.
Training
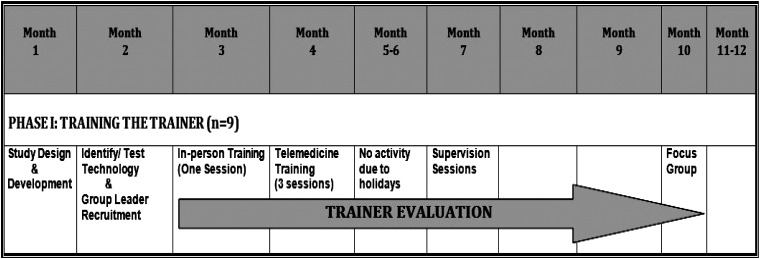
All GLs and study staff attended one 6-h, in-person orientation at the primary study site (UNC-CH), followed by three 2-h bimonthly telehealth sessions (Fig. 2). Four 1-h bimonthly telehealth meetings providing supervision began after the GLs facilitated their first class. Two of the study investigators (an advanced practice nurse and a clinical psychologist) co-facilitated the training and supervision telehealth sessions. To identify strengths and areas for improvement in the training, supervision, and delivery of the CT program, at the conclusion of the project GLs participated in a focus group led by a doctoral-level qualitative researcher with two decades of experience in focus group interviews.
Fig. 2.
Training timeline. Preparation and implementation of the Cancer Transitions telehealth training program was completed within 12 months.
The training addressed psychological processes as well as established cancer survivorship issues.26 Group facilitation processes included leader behaviors (e.g., nonjudgmental stance, providing structure, managing assumptions and expectations about effectiveness) and group behaviors (e.g., stages of group formation, establishing norms).27
The six modules of the CT program were taught to GLs over three training telehealth sessions. Before each session, GLs received (by e-mail) worksheets outlining the CT class material to be covered and listing essential leader behaviors. Included was a “checklist” of class-unique tasks that could be used as they were facilitating the CT series, such as discussing boundaries and confidentiality in the first class. In addition, GLs received training materials published by the Cancer Support Community and LIVESTRONG.24,28
Supervision followed a “teaching laboratory” model in which core competencies essential to CT program material were explored in a group format in close succession to the actual CT classes.29 For most GLs, the first supervisory telehealth session was held within 2 weeks of leading the first two CT classes. These supervisory sessions were structured to process the objectives of the classes that had been held already and to prepare GLs for the next classes they were scheduled to lead. Although formal supervision was discontinued at study end, GLs were encouraged to maintain a relationship with the UNC-CH Lineberger Comprehensive Cancer Center community liaison for ongoing support needs.
Measures
Quantitative measures are described in Table 2. In addition to the quantitative measures, all GLs participated in a focus group at study end. To allow in-depth exploration of the topics under investigation, the professional focus group moderator followed a semistructured topic guide that permitted additional questions for clarification where indicated.30,31 The 90-min focus group began by inquiring about GL reactions to the initial in-person training session.
Table 2.
Measures Administered
| GROUP LEADER MEASURES | DESCRIPTION | RESPONSE STYLE | POTENTIAL TOTAL SCORE |
|---|---|---|---|
| Training Content Evaluationa | Understanding of emotional and physical survivorship components highlighted in CT | 14 items, Likert, 5 point | Sum of all items: range, 14–70; higher=better understanding |
| Group Leader Confidence Scalea | Self-efficacy regarding group facilitation, adapted from the General Self-Efficacy Scale by adding a neutral option | 10 items, Likert, 5 point | Sum of all items: range, 10–50; higher=better self-efficacy |
| Group Training Satisfaction Rating Scaleb | Satisfaction of training program | 9 items, Likert, 5 point | Sum of all items: range: 9–45; higher=more satisfied |
| Group Leader Weekly Supervision Satisfaction Scalec | Satisfaction of supervision sessions while conducting CT program | 9 items, Likert, 5 point | Sum of all items: range, 9–45; higher=more satisfied |
| Cancer Transitions Program Quality Evaluationd | Quality of CT program | 10 items, Likert, 5 point | Sum of all items: range, 10–50; higher=better quality |
Five self-report measures were adapted to assess the content, utility, quality, and satisfaction of trainers with the Cancer Transitions (CT) telehealth training program.
Baseline, posttraining, and post–Cancer Transitions series leadership.
After each telemedicine training session (three times).
After each telemedicine supervision session (four times).
At the end of the study.
Statistical Methods
Statistical analyses were conducted with SAS (Cary, NC) statistical software version 9.3. Descriptive statistics are reported, and changes between time points were evaluated using Wilcoxon signed-rank tests.
Qualitative data obtained from the focus group were systematically analyzed, and verbatim quotes were assigned to a content category from one of the constructs from the topic guide (Table 3). First, the quotes in each category were independently reviewed, with prevailing points of view forming the strongest themes and particular attention given to lessons learned for future training using telehealth technology. The list of themes was then shared and discussed among research team members; disagreement was resolved via discussion.
Table 3.
Focus Group Guide
| Training questions |
| 1. What stood out to you about the training? |
| 2. What, if anything, did you gain from the training? |
| 3. Was any of the information confusing—or hard to understand? |
| 4. Overall how satisfied are you about the use of telemedicine to deliver the training? |
| 5. How do you feel the training related to the actual process of leading the group? |
| 6. What are your thoughts about the Cancer Transitions publications? |
| 7. How did you find the measures we asked you to fill out? |
| Supervision questions |
| 8. How did you feel about the supervision sessions after each group? |
| Group questions |
| 9. Was leading the group harder than you thought? Easier than you thought? |
| 10. Was there anything that seemed easy when the trainer discussed it that was hard when you did the group? |
| 11. What is your comfort level with doing this group on your own? |
| 12. When/if you do the group again, how would you change it? |
| 13. What are your thoughts about this grant ending? |
| 14. Any other comments? |
The focus group was facilitated by a trained focus group leader (unaffiliated with the study) who initiated discussion with the following guided inquiries.
Results
Satisfaction
Nine GLs attended the in-person orientation and all four telehealth training sessions and attended at least two of the four telehealth supervision sessions. Satisfaction with the three group training sessions was high; the median Group Training Satisfaction Rating Scale score was 44 (range, 40–45). Qualitatively, most GLs believed the in-person training was an excellent experience that provided relevant information, helped them become comfortable videoconferencing via the iPad, and provided opportunities to meet other GLs and the research team. GLs expressed satisfaction with the demonstration of group leadership techniques, especially the use of video clips. Some GLs felt overwhelmed by the amount of information they received during the in-person training, whereas others would have liked to learn more about the CT program content. The wish for additional time for professional networking was also voiced.
Satisfaction with the four supervision sessions conducted over the course of the CT program was also high. The median GL Weekly Supervision Satisfaction Scale scores following each of the four supervision sessions were 42, 43, 44, and 41, respectively, and never dropped below 40 (range, 30–45). GLs characterized their training as effective in teaching them the necessary skills to successfully lead the CT program. All GLs, even those with prior experience leading groups, said they became better facilitators as a result of the training and the experience with their CT groups.
Understanding of CT and Confidence in Group Facilitation
GLs began the training with good understanding of the CT program content and knowledge regarding the experience of cancer (Training Content Evaluation median, 55; range, 46–70). The posttraining leadership median score was also high (61; range, 42–70).
GL self-confidence in the ability to facilitate their CT groups was also high pretraining, with a baseline median GL Confidence Scale score of 42 (range, 38–49). Seven leaders (78%) reported growth in confidence from baseline to last time point, with a significant median increase in score of 3 points (p=0.023). The final median score was 47 (range, 41–50).
Perceptions about Program Quality
GLs evaluated the CT program and their own experience of participating as GLs as highly positive. The median CT Program Quality Evaluation score was 45 (range, 38–50).
Perceptions about Technology
At the first training session, responses to the inquiry “I think telecommunications for the purpose of training individuals is an efficient way to train” were variable (“Exactly true,” n=3; “Moderately true,” n=3; “Neutral,” n=2; and “Hardly true,” n=1). Following the third (final) training session, GLs reflected agreement that the method was efficient (“Exactly true,” n=5; “Moderately true,” n=4). Similar responses were received on the item “Using telecommunications is easy.” After the first session, five leaders reported either “Neutral” or “Hardly true,” whereas after the third session, eight reported “Extremely true,” and one rated the item “Moderately true.”
“Saving the drive” was identified as the key advantage of telehealth delivery for training. Those GLs from rural communities with limited resources for continuing education believed telehealth provided a training opportunity that otherwise would not exist. One nurse said, “We're here in the middle of nowhere… So it's a wonderful way to get the training ….”
The majority of GLs found telehealth particularly suitable for the supervision sessions, helping GLs to stay connected with each other and to “know what others are doing,” which helped them organize their own CT sessions. Although GLs had the option of using the telephone to call in for training, those who by necessity did so found it less effective. One stated, “…phone was awful, I didn't get anything out of it.” The GLs found sharing and discussion about difficult moments in their groups most valuable: “I'll never forget one GL talking about a patient who cried the whole time. That made me think about what I would do if that happens in my session.”
A measure of ambivalence for telehealth was voiced as well, with a few describing the process as “unsatisfying” and “cold, sterile and lacking in human presence.” These GLs said they felt inhibited and did not contribute as much as they would have liked to the conversations. “[The technology] worked fine, but I felt uncomfortable talking and I wasn't as open as I [could have been]. I was afraid I was going to cut someone off. I couldn't see their body language either, so I was always fearful of jumping in and talking too long.” Another GL added, “You couldn't go ‘uh-huh’ because it would cut someone else off. You had to talk and then stop.” One GL stated, “It's just a Catch-22. The good is also the bad. We don't want to drive but we don't like to feel disconnected.”
The GLs enthusiastically recommended strategies to enhance future training, strongly suggesting an extension of the 1-day in-person training to 2 days so that the use of the iPad, group processes, and the curriculum materials could be more thoroughly reviewed, and so that professional networking and team building could take place. Although the cost would increase, GLs believed that the benefits of extending the initial training by a day would be well worth it. A majority of the GLs said they would have preferred using DVDs, Web links, PowerPoint® (Microsoft, Redmond, WA) presentations, and lectures to absorb most of the training modules' content on their own time, rather than using the telehealth on a workday. GLs also recommended that the training be tailored to individuals' knowledge, skill, and experience. Although the GLs had a high level of initial understanding of group processes, the cancer experience, and the need for group programs for cancer survivors, they were less proficient at recruiting potential group members. Three GLs specifically stated they needed more instruction on marketing the CT program in their respective communities and managing the timing of recruiting for their groups.
Discussion
This pilot study demonstrated the feasibility of using telehealth technology for disseminating information, building skills, and sustaining outreach efforts for group leadership. Overall, the excellent engagement and retention of GLs in this training experience provide evidence of acceptability of the approach. Although GLs rated the program highly regarding CT content preparation, they also experienced difficulties with the telehealth technology. A full-duplex videoconference system was used to enable simultaneous speech, but a slight time lag impeded the natural flow of conversation and incurred periodic awkwardness during the meetings. Dissatisfaction with technology may also have resulted from GL preferences for in-person interactions and limited initial bonding with other GLs during the single in-person training. However, the addition of video to virtual meetings provided a more personal connection than audio alone (as in telephone conferences), and the potential for training efficiency was clear and appreciated by the leaders and trainers.
In addition, although initial reactions to receiving supervision were mixed, final evaluations of the supervision sessions were positive. Mental health professionals are accustomed to models of clinical supervision and seek out clinical or peer supervision throughout their career, but this is not standard in all healthcare professions.32,33 We found that we needed to describe the rationale for supervision prior to the sessions and demonstrate a positive framework for its implementation. The agendas for the supervision sessions always began with processing the positive observations that GLs had from their CT leadership experience and later moved toward areas they might want consultation. Future work might choose to use the term “consultation” rather than “supervision.”
Our small group of GLs also demonstrates the “Goldilocks” challenge to designing a training program that fits a multidisciplinary group of professionals. Some GLs felt they had received too much information during the in-person orientation; others wanted more. Some were very comfortable with technology, using it on a daily basis and easily connecting by remote videoconferencing for the trainings, and others struggled to use skills once every 2 weeks that they did not use daily. Some GLs who had personally experienced cancer were familiar with the program content and believed parts of the trainings to be redundant, but others benefited from reviewing the CT materials in anticipation of leading their own groups. Despite the expressed critiques with these areas, however, the overall satisfaction of the GLs suggests that this area is ripe for development and future research.
Limitations
Data from this pilot project beg cautious interpretation in view of the small sample, limiting the generalizability of the results. Additionally, because protecting the privacy of the community survivors and caregivers was a priority, the groups were not video-recorded for fidelity to the CT model. As a result, there was a strong ceiling effect with most of the measures used in this study. Finally, study investigators did not have reliability or validity ratings of the measures adapted from the CT program; data generated from this project will facilitate this necessary process.
Future Directions for Telehealth Training
Our findings suggest several areas for future research:
1. Emphasize the value of initial in-person training for establishing a cohesive group for subsequent videoconferencing interactions.
2. Explore the value of tailoring the training program according to GLs' varying levels of knowledge and group facilitation skills to maximize their learning experience. This can be accomplished, in part, by providing training materials in other formats (e.g., CD/DVD or Web-based) to facilitate different learning needs in addition to group videoconferencing.
3. Explore methods of training GLs in marketing the group and recruiting participants.
4. Promote realistic expectations of GLs for the training and supervisory experiences using telehealth (both technological considerations and group process challenges).
5. Generate measures to assess fidelity and adherence to the CT model and, fully considering the needs for privacy and confidentiality of survivors, perhaps including audio or visual recordings of actual groups.
Conclusions
These data suggest that telehealth technology represents an exciting, efficient approach to train and support leaders of psychoeducational groups. The current widespread usage of telecommunications technology facilitates this model of training and efficiently addresses the need to expand cancer survivorship programs to areas outside academic medical centers. Because the majority of cancer patients receive their care in community settings, telehealth training is relevant to real-world needs of patients and clinicians around the world.34
Acknowledgments
This study was accomplished with funding from the UNC Lineberger Comprehensive Cancer Center 2011–2012 Health-e-NC Pilot Proposal Grant Award. The authors also acknowledge Carolina Well, funded by LIVESTRONG Survivorship Center of Excellence Network and the V Foundation for Cancer Research.
Disclosure Statement
No competing financial interests exist.
References
- 1.American Cancer Society. Cancer Treatment & Survivorship Facts & Figures 2012–2013. Atlanta: American Cancer Society, 2012 [Google Scholar]
- 2.Doll R, Kazanjian A, Smillie K, Ward A, Chasen M. A call for action in survivorship research and care. Curr Oncol 2012;19:16–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eaton LH, Doorenbos AZ, Schmitz KL, Carpenter KM, McGregor BA. Establishing treatment fidelity in a web-based behavioral intervention study. Nurs Res 2011;60:430–435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doorenbos AZ, Kundu A, Eaton LH, Demiris G, Haozous EA, Towle C, et al. . Enhancing access to cancer education for rural healthcare providers via telehealth. J Cancer Educ 2011;26:682–686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gagnon C, Brown C, Couture C, Kamga-Ngande CN, Hivert MF, Baillargeon JP, et al. . A cost-effective moderate-intensity interdisciplinary weight-management programme for individuals with prediabetes. Diabetes Metab 2011;37:410–418 [DOI] [PubMed] [Google Scholar]
- 6.Goldfield GS, Epstein LH, Kilanowski CK, Paluch RA, Kogut-Bossler B. Cost-effectiveness of group and mixed family-based treatment for childhood obesity. Int J Obes Relat Metab Disord 2001;25:1843–1849 [DOI] [PubMed] [Google Scholar]
- 7.Labus J, Gupta A, Gill HK, Posserud I, Mayer M, Raeen H, et al. . Randomised clinical trial: symptoms of the irritable bowel syndrome are improved by a psycho-education group intervention. Aliment Pharmacol Ther 2013;37:304–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fawzy FI, Fawzy NW. A structured psychoeducational intervention for cancer patients. Gen Hosp Psychiatry 1994;16:149–192 [DOI] [PubMed] [Google Scholar]
- 9.Owen JE, Klapow JC, Hicken B, Tucker DC. Psychosocial interventions for cancer: Review and analysis using a three-tiered outcomes model. Psychooncology 2001;10:218–230 [DOI] [PubMed] [Google Scholar]
- 10.Spiegel D. Effects of psychotherapy on cancer survival. Nat Rev Cancer 2002;2:1–7 [DOI] [PubMed] [Google Scholar]
- 11.Valle CG, Campbell MK, Sherwood E, Manning M, Gellin M. Information and support needs of adult cancer patients in North Carolina: Implications for a comprehensive cancer center survivorship program. Poster presentation at the 31st Annual Meeting & Scientific Sessions of the Society of Behavioral Medicine, Seattle, WA, April 2010 [Google Scholar]
- 12.Cohen G. ASCO Educational Book: Cancer clinical trials: A primer for participation of community physicians. Alexandria, VA: American Society of Clinical Oncology, 2002:283–289 [Google Scholar]
- 13.Zordan RD, Butow PN, Kirsten L, Juraskova I, O'Reilly A, Friedsam J, et al. . The development of novel interventions to assist the leaders of cancer support groups. Support Care Cancer 2012;20:445–454 [DOI] [PubMed] [Google Scholar]
- 14.Zordan RD, Juraskova I, Butow PN, Jolan A, Kirsten L, Chapman J, et al. . Exploring the impact of training on the experience of Australian support group leaders: Current practices and implications for research. Health Expect 2010;13:427–440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Butow P, Beeney L, Juraskova I, Ussher J, Zordan R. The gains and pains of being a cancer support group leader: A qualitative survey of rewards and challenges. Soc Work Healthc 2009;48:750–767 [DOI] [PubMed] [Google Scholar]
- 16.Price M, Butow P, Kirsten L. Support and training needs of cancer support group leaders: A review. Psychooncology 2006;15:651–663 [DOI] [PubMed] [Google Scholar]
- 17.Kazanjian A, Smillie K, Howard AF, Ward A, Doll R. A structured approach to knowledge exchange: Understanding the implementation of a cancer survivor program. Eur J Oncol Nurs 2012;16:399–405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kirsten L, Butow P, Price M, Hobbs K, Sunquist K. Who helps the leaders? Difficulties experienced by cancer support group leaders. Support Care Cancer 2006;14:770–778 [DOI] [PubMed] [Google Scholar]
- 19.Butow P, Ussher J, Kirsten L, Hobbs K, Smith K, Wain G, et al. . Sustaining leaders of cancer support groups: The role, needs, and difficulties of leaders. Soc Work Healthc 2005;42:39–55 [DOI] [PubMed] [Google Scholar]
- 20.Andrusyszyn MA, Cragg CE, Humbert J. Nurse practitioner preferences for distance education methods related to learning style, course content, and achievement. J Nurs Educ 2001;40:163–170 [DOI] [PubMed] [Google Scholar]
- 21.Allen M, Sargeant J, MacDougall E, Proctor-Simms M. Videoconferencing for continuing medical education: From pilot project to sustained programme. J Telemed Telecare 2002;8:131–137 [DOI] [PubMed] [Google Scholar]
- 22.Barden W, Clarke HM, Young NL, McKee N, Regehr G. Effectiveness of telehealth for teaching specialized hand-assessment techniques to physical therapists. Acad Med 2000;75(10 Suppl):S43–S46 [DOI] [PubMed] [Google Scholar]
- 23.O'Regan K, Marsden P, Sayers G, Morrissey M, Hegarty H, Allen M, et al. . Videoconferencing of a national program for residents on evidence-based practice: Early performance evaluation. J Am Coll Radiol 2010;7:138–145 [DOI] [PubMed] [Google Scholar]
- 24.Weiss E, Chew T, Miller K, Schover L, Demark-Wahnefried W, Justice H, et al. . Cancer Transitions: Moving Beyond Treatment,® A program of the Cancer Support Community and LIVESTRONG facilitator guide. Washington, DC: Cancer Support Community, 2009 [Google Scholar]
- 25.Ward A. Cancer survivorship: Creating uniform and comprehensive supportive care programming in Canada. Vancouver, BC, Canada: BC Cancer Agency, 2010 [Google Scholar]
- 26.Plakun EM, Sudak DM, Goldberg D. The Y model: An integrated, evidence-based approach to teaching psychotherapy competencies. J Psychiatr Pract 2009;15:5–11 [DOI] [PubMed] [Google Scholar]
- 27.Corey MS, Corey G, Corey C. Groups: Process and practice, 8th ed. Belmont, CA: Brooks/Cole, Cengage Learning, 2010 [Google Scholar]
- 28.Cancer Support Community and LIVESTRONG. Cancer Support Community Distance Learning Site. 2012. Available at http://online.cancersupportcommunity.org/cscdl/ (last accessed October18, 2012)
- 29.Cabaniss DL, Arbuckle MR. Course and lab: A new model for supervision. Acad Psychiatry 2011;35:220–225 [DOI] [PubMed] [Google Scholar]
- 30.Corbin J. Basics of qualitative research: Techniques and procedures for developing grounded theory. Los Angeles: SAGE Publications, 2008 [Google Scholar]
- 31.Stewart DW. Focus groups: Theory and practice, 2nd ed. Thousand Oaks, CA: SAGE Publications, 2007 [Google Scholar]
- 32.Schofield MJ, Grant J. Developing psychotherapists' competence through clinical supervision: Protocol for a qualitative study of supervisory dyads. BMC Psychiatry 2013;13:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Claveirole A, Mathers M. Peer supervision: An experimental scheme for nurse lecturers. Nurse Educ Today 2003;23:51–57 [DOI] [PubMed] [Google Scholar]
- 34.National Cancer Institute. Why is NCI conducting the NCI Community Cancer Centers Program? 2012. Available at http://ncccp.cancer.gov/Media/FactSheet.htm (last accessed October9, 2013)