Abstract
Introduction:
Patellar involvement by osteoid osteoma is very rare. Osteoid osteomas that present as anterior knee pain are frequently misdiagnosed which leads to initial delay in treatment. Plain radiology has poor diagnostic yield. A combination of high index of suspicion, appropriate imaging, and complete ablation of the lesion is necessary to achieve good outcomes.
Case Report:
A 16-year-old male presented with insidious onset anterior knee pain for the past 2 years. The pain was intermittent and mild; however, it increased progressively in intensity and frequency, which was worse at night. Examination reveals minimal effusion in the suprapatellar pouch, full range of motion of the knee, and wasting of the quadriceps. Serum biochemistry parameters were in normal limits. Plain radiographs did not reveal any significant abnormality. On magnetic resonance imaging, a hypointense, punctate lesion surrounded by a small hyperintense zone was noted at medial aspect of patella. A computed tomography scan showed the lesion with a central nidus, surrounded by a sclerotic rim, confirming the diagnosis of osteoid osteoma. Radiofrequency ablation was carried out without any post-procedural complications. The patient was pain free a few days after the procedure. At 14-month follow-up, there was no recurrence of symptoms.
Conclusion:
Osteoid osteomas that present as anterior knee pain are frequently misdiagnosed. Plain radiology has poor diagnostic yield. A combination of high index of suspicion, appropriate imaging, and complete ablation of the lesion is necessary to achieve good outcomes.
Keywords: Osteoid osteoma, patella, anterior knee pain, radiofrequency ablation, patellar tumor, patellofemoral pain
Learning Point of the Article:
Patellar osteoid osteomas are rare and can present with intractable knee pain; thin slice CT scan or bone scan are necessary to clinch the diagnosis and most lesions can be managed by percutaneous radiofrequency ablation’.
Introduction
Osteoid osteoma is a benign bone-forming tumor, first described by Jaffe, in 1935 [1]. The predominant sites of affliction are the diaphysis of femur and tibia, though any bone may be involved. Osteoid osteomas of the long bones are readily diagnosed on the basis of typical clinical presentation and visualization of the characteristic nidus on computed tomography (CT) scans or increased uptake on Tc99m bone scan. However, patellar involvement by these tumors is quite rare. In a series of 23000 tumors by Casadei et al. [2], patellar tumors accounted for only 0.2% of all tumors, of which osteoid osteoma contributed to 17% of all patellar tumors. Therefore, the rarity of this presentation, coupled with atypical clinical features, can result in misdiagnoses and unwarranted surgical interventions. This may eventually delay the correct diagnosis.
We report a rare case of osteoid osteoma of the patella in an adolescent male who presented with intractable anterior knee pain and was successfully treated with percutaneous, CT-guided radiofrequency ablation. We also present a systematic review of literature on this rare entity.
Case Report
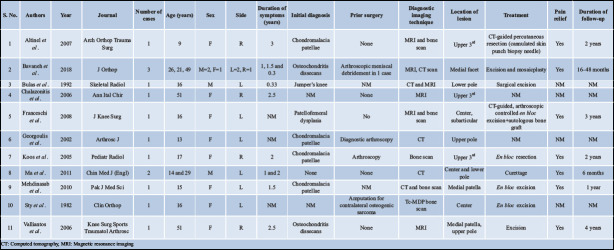
A 16-year-old male of Asian ethnicity presented with insidious onset anterior knee pain for the past 2 years. To begin with, the pain was intermittent and mild; however, it increased progressively in intensity and frequency. At the time of consultation, he had moderate-to-severe continuous pain, which was worse at night. He had only modest response to nonsteroidal anti-inflammatory medications. Examination did not reveal any specific tenderness; there was minimal effusion in the suprapatellar pouch, full range of motion of the knee, and wasting of the quadriceps. Serum biochemistry parameters were with normal limits. Plain radiographs of the knee did not reveal any significant abnormality. On magnetic resonance imaging (MRI), a hypointense, punctate lesion surrounded by a small hyperintense zone (edema) was noted at medial aspect of patella, close to its articular surface (Fig. 1). A CT scan was done next, which showed the lesion with a central nidus, surrounded by a sclerotic rim, confirming the diagnosis of osteoid osteoma (Fig. 2).
Figure 1.

(a-d) Anteroposterior and lateral radiographs of the knee in a young male with anterior knee pain. No gross abnormality was detectable. (c) T2-weighted sagittal magnetic resonance imaging (MRI) section showing patellar edema. (d) T2-weighted axial MRI section showing a hypointense punctate lesion surrounded by a small hyperintense zone near the medial border of patella, close to its articular surface (arrow).
Figure 2.
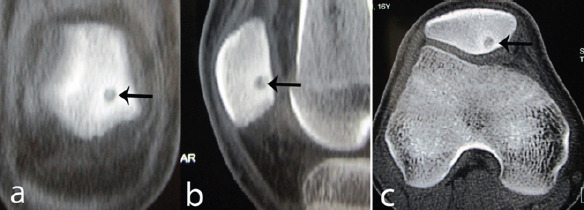
(a and b) Computed tomography scan of the patient (a) coronal reformat, (b) sagittal reformat, and (c) axial cut showing central nidus surrounded by minimal sclerosis.
The patient was planned for percutaneous CT-guided radiofrequency ablation. Dispersive grounding pads were placed under both thighs with good skin contact. Under spinal anesthesia, the lesion was localized on multidetector CT scan. A 1.2 mm K-wire was gradually advanced from the dorsal surface of the patella into the lesion under CT guidance using a combination of drilling and gentle hammering. Care was taken not to breach the patellar articular cartilage. Once the K-wire was in place, it was replaced with a radiofrequency ablation probe, 0.7 cm in diameter and 14.4 cm long (Cool-tipTM, Medtronic) (Fig. 3).
Figure 3.
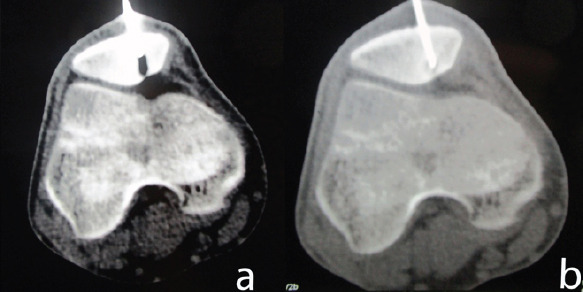
(a and b) Percutaneous computed tomography-guided radiofrequency ablation (a) insertion of guide wire through the dorsal approach, (b) the guide wire is in position and would be replaced by the radiofrequency probe.
Radiofrequency ablation was carried out at 90° for 5 min. No post-procedural complications were noted. The patient was administered analgesics for the next 3 days and permitted full weight-bearing. The patient was pain free a few days after the procedure. At 14-month follow-up, there was no recurrence of symptoms. The quadriceps wasting had improved significantly and he had full range of motion (Fig. 4).
Figure 4.

(a-c) At 1-year follow-up, the patient has no quadriceps wasting, no extensor lag, and full flexion of the knee.
Discussion
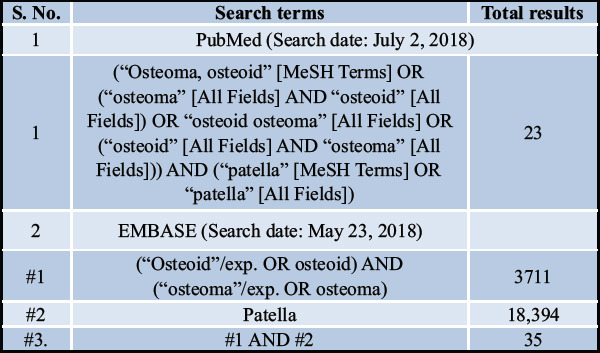
We conducted a systematic review of literature using the PubMed and the EMBASE databases for the primary searches. The detailed search strategy for both databases is presented in Table 1.
Table 1.
Search strategy.
For the secondary search, we screened the reference lists of included articles, as well as any relevant review articles identified by the primary search. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [3] for the purpose of this systematic review. We included studies and case reports if they reported clinicoradiological features of patellar osteoid osteomas. Review articles, conference abstracts, reports in languages other than English, reports not describing the clinical features, and tumors other than patellar osteoid osteomas were excluded from the study. Search results were imported into a reference management software (Zotero, version 4.0.29.5). After deduplication, the results were independently screened by two authors (SS and RR) for inclusion using the pre-specified inclusion and exclusion criteria. Any conflicts were resolved by mutual agreement. Following this, full texts of the relevant articles were obtained and data were collected in a pre-specified data entry sheet.
Using our pre-defined search strategy, a total of 58 results were identified, of which 14 cases from 11 studies [4-14] were included in the qualitative analysis (Fig. 5). The details of the included studies are presented in Table 2.
Figure 5.
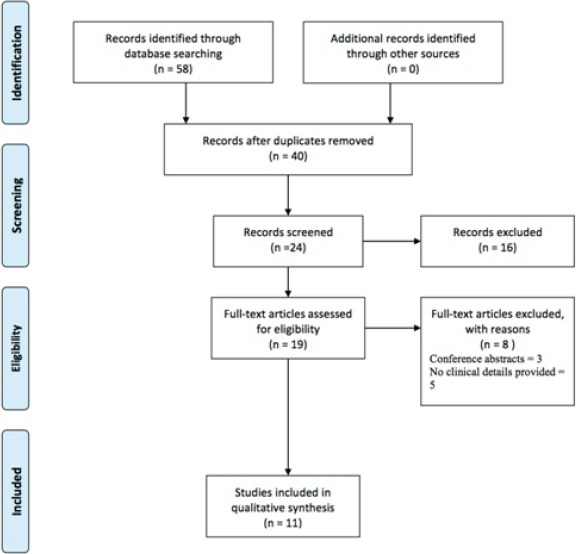
Preferred reporting items for systematic reviews and meta-analyses flowchart.
Table 2.
Results of the systematic review.
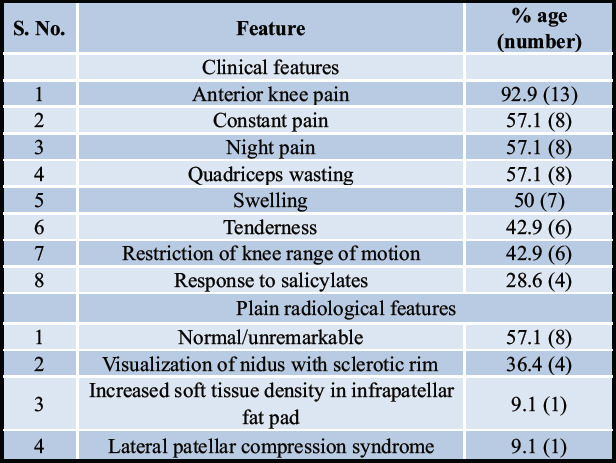
The mean age of patients included in the review was 24.5 ± 14.89 years (range 9–51 years). There were nine females and five males. The right side was involved in five patients whereas the left side was involved in nine patients. Delay in diagnosis was reported by eight authors [4- 6, 10-14]; the average delay in diagnosis was 1.8 ± 0.84 years (range 0.3–2.5 years). The condition was misdiagnosed as chondromalacia patellae in four reports [4, 8, 12, 13], osteochondritis dissecans in two reports [10, 14], and jumper’s knee [5] and patellofemoral dysplasia [7] in one report each. In three reports [8, 12, 14], prior arthroscopy had been performed but failed to diagnose the condition. All cases, except one which was asymptomatic, had anterior knee pain. The only asymptomatic patient in the review was a 16-year-old girl in whom amputation of the contralateral side had been performed for osteogenic sarcoma and the osteoid osteoma was detected incidentally on follow-up technetium 99m methylene diphosphonate (Tc-MDP) bone scan [9]. The most prevalent clinical features were constant nature of pain, night pain, quadriceps wasting, and swelling around the knee. Plain radiographs revealed the diagnosis in only 36.4% of all cases (Table 3).
Table 3.
Clinicoradiological features of patients included in the review.
The confirmatory modality for diagnosis was either CT, MRI, Tc-MDP bone scan, or a combination of these. Histological confirmation of the diagnosis was done in 10 (71.4%) cases. Treatment consisted of resection in five cases [5, 9, 10, 12, 13], curettage in two cases [11], CT-guided percutaneous resection with biopsy needle in one case [4], CT-guided, arthroscopy controlled excision with bone grafting in one case Franceschi et al. [7], and excision with mosaicplasty in three cases [14]. Two authors did not report the treatment given [6, 8]. Four authors [5, 6, 8, 9] did not report on the final follow-up. In the remaining six reports [4, 7, 10-14], all patients were pain free and had no recurrence at the final follow-up.
Osteoid osteoma is a benign osteoblastic lesion characterized by a central radiolucent nidus along with peripheral zone of sclerosis due to reactive bone formation [15]. Patella is a rare location for this tumor and the invariable presentation is that of anterior knee pain. It is pertinent to mention here that atypical knee pain may also be the presenting complaint in osteoid osteomas around the proximal femur. Georgoulis et al. [8] reported 10 cases of osteoid osteoma that presented as atypical knee pain. Of these, 60% had lesions around the hip or proximal femur. Hence, the possibility of referred pain must always be kept in mind whenever the clinician is faced with a case of atypical knee pain.
As is evident from our review, the clinical features of patellar osteoid osteomas are non-specific, and therefore, a high index of suspicion is necessary to diagnose this condition. Delays and misdiagnosis are common, as evident from this review. Therefore, the clinician should be aware of the “red-flag” signs, which point toward osteoid osteoma and warrant appropriate investigation in the form of CT or bone scan. These include rest pain, pain that is severe at night, pain that has steadily increased in intensity and does not respond to the usual dose of analgesics, and “hard” signs such as significant quadriceps wasting and decreased knee range of motion. The presence of these signs in our case led us to the use of CT scan, which rendered the correct diagnosis.
Plain radiographs are among the initial investigations ordered for anterior knee pain. However, our review has shown that the diagnostic yield of plain radiographs for these lesions is quite low and misdiagnoses are common. Hence, the clinician must be prepared to order additional imaging modalities. CT scan can readily detect the nidus and obviate the need for histopathological diagnosis; however, it is important to order thin sections as the pathology may be missed on conventional sections [16, 17]. Tc-MDP bone scan can also be used as a diagnostic modality. The characteristic features are increased uptake in the center of the lesion (representing the nidus) and a surrounding area of less intense uptake in the periphery (representing the reactive new bone) termed as the “double density” sign [9]. However, it must be remembered that the reactive periosteal reaction is minimal in cancellous bones, and therefore, the utility of this sign in osteoid osteomas of the axial skeleton is limited [2, 7, 16]. Although MRI can detect the nidus, the reactive marrow edema can often mask the lesion itself, thereby making diagnosis difficult [16, 17]. Due to the fact that MRI is considered as the imaging modality of choice for patellofemoral pain, it is easy to miss, or misdiagnose this rare entity as chondromalacia or osteochondritis dissecans [10].
Spontaneous resolution of osteoid osteomas has been reported [18], however, this may require prolonged periods of observation along with nonsteroidal anti-inflammatory drugs [15]. Many patients may be unwilling to undergo such treatment till resolution. Therefore, surgical removal is generally considered as the standard of care. The different options for removal can be broadly classified as percutaneous and open modalities. Percutaneous methods include radiofrequency ablation, laser photocoagulation, ethanol injection, drilling, and curettage, which may be accomplished under the guidance of arthroscopy, CT scan, or radionucleotide scan [10, 15, 19]. Minimally invasive techniques, particularly radiofrequency thermoablation, are considered as the treatment of choice since the 1990s, with success rate of around 95% in experienced hands [19]. In addition to high success rates, the procedure can be done under day care basis and patients can resume work early.
“Open” surgical excision and curettage have also been successfully reported, this is usually done through the medial parapatellar approach [5, 10]. The tumor can be visualized and curettage or excision done. However, extensile approaches are not without their shortcomings. Vallianatos et al. [10] reported patella baja in their case of patellar osteoid osteoma, which was managed by open excision, presumably due to scarring of the patellar tendon. Furthermore, the advent of imaging modalities such as CT scan and bone scan permits accurate localization and removal of the lesion, and therefore, open procedures have been largely abandoned in favor of percutaneous methods. Nonetheless, with any technique, it is of utmost importance to preserve the patellar articular cartilage as injury to this could potentially result in early patellofemoral arthrosis. In our case, we chose to approach the lesion through the dorsal, non-articular surface of patella and were careful not to breach the articular cartilage during placement of the guidewire or radiofrequency probe.
Bavaneh et al. [14] reported on three patients with patellar osteoid osteomas in whom they performed en bloc resection of the tumor, along with the articular cartilage through a medial parapatellar arthrotomy and reconstruction by mosaicplasty. All lesions in this series were located very close to the articular cartilage of the medial patellar facet. There was no recurrence of the lesion at a mean follow-up of 31 months and all patients were pain free. Although every effort must be made to preserve the native patellar articular cartilage, en bloc cartilage excision may be the only option for lesions that have a full-thickness cartilage breach. Fortunately, in most of the cases included in this review and also in our case, the lesion is usually subarticular and amenable to cartilage preserving ablation.
Conclusion
Patellar osteoid osteomas are rare and should be always considered in the differential diagnosis of anterior knee pain. The atypical presentation or “red flags” in the form of rest pain, night pain, significant quadriceps wasting, and restriction of knee range of motion should guide the clinician to seek for this diagnosis, by the use of thin-slice CT scan or bone scan. Once the diagnosis has been confirmed, the lesion can be managed by a variety of image-guided, percutaneous ablation techniques. However, utmost care should be taken to avoid damage to the patellar articular cartilage to prevent patellofemoral arthrosis.
Clinical Message.
Patellar involvement by osteoid osteoma is very rare. The presence of atypical clinical features and initial misdiagnosis may delay treatment. Hence, a high index of suspicion an early detailed evaluation is necessary to achieve good outcomes.
Biography



Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that Informed consent of the patient is taken for publication of this case report
References
- 1.Jaffe HL. Osteoid-osteoma:A benign osteoblastic tumor composed of osteoid and atypical bone. Arch Surg. 1935;31:709–28. [Google Scholar]
- 2.Casadei R, Kreshak J, Rinaldi R, Rimondi E, Bianchi G, Alberghini M, et al. Imaging tumors of the patella. Eur J Radiol. 2013;82:2140–8. doi: 10.1016/j.ejrad.2011.11.040. [DOI] [PubMed] [Google Scholar]
- 3.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Loannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions:Explanation and elaboration. PLoS Med. 2009;6:1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Altinel L, Degirmenci B, Kose KC, Sahin O. Percutaneous resection of a patellar osteoid osteoma using a cannulated skin punch biopsy needle. Arch Orthop Trauma Surg. 2007;127:299–302. doi: 10.1007/s00402-006-0108-7. [DOI] [PubMed] [Google Scholar]
- 5.Bulas RV, Hayes CW, Conway WF, Loughran T. Case report 738:Osteoid osteoma of the patella. Skeletal Radiol. 1992;21:326–9. doi: 10.1007/BF00241775. [DOI] [PubMed] [Google Scholar]
- 6.Chalazonitis AN, Tilentzoglou AC, Condilis N, Tzovara J, Porfyridis P, Ptohis N. Osteoid osteoma of the patella. Case report and review of the literature. Ann Ital Chir. 2006;77:533–6. [PubMed] [Google Scholar]
- 7.Franceschi F, Longo UG, Ruzzini L, Marinozzi A, Rizzello G, Papalia R, et al. En-bloc retrograde resection of an osteoid osteoma of the patella using computed tomography under arthroscopic control. J Knee Surg. 2008;21:136–40. doi: 10.1055/s-0030-1247808. [DOI] [PubMed] [Google Scholar]
- 8.Georgoulis AD, Papageorgiou CD, Moebius UG, Rossis J, Papadonikolakis A, Soucacos PN. The diagnostic dilemma created by osteoid osteoma that presents as knee pain. Arthroscopy. 2002;18:32–7. doi: 10.1053/jars.2002.30010. [DOI] [PubMed] [Google Scholar]
- 9.Sty J, Simons G. Intraoperative 99m technetium bone imaging in the treatment of benign osteoblastic tumors. Clin Orthop Relat Res. 1982;165:223–7. [PubMed] [Google Scholar]
- 10.Vallianatos PG, Tilentzoglou AC, Seitaridis SV, Mahera HJ. Osteoid osteoma of the patella:A case report. Knee Surg Sports Traumatol Arthrosc. 2006;14:161–4. doi: 10.1007/s00167-005-0653-6. [DOI] [PubMed] [Google Scholar]
- 11.Ma K, Zhao HT, Niu XH. Osteoid osteoma of the patella:Report of two cases. Chin Med J. 2011;124:4096–8. [PubMed] [Google Scholar]
- 12.Koós Z, Than P. Rare localization of osteoid osteoma in the patella. Pediatr Radiol. 2005;35:929–30. doi: 10.1007/s00247-005-1476-9. [DOI] [PubMed] [Google Scholar]
- 13.Mehdinasab S, Sarrafan N, Alvavinejad P. Osteoid osteoma of the patella presenting as chronic anterior knee pain case report and review of the literature. Pak J Med Sci. 2010;26(2):490–3. [Google Scholar]
- 14.Bavaneh MK, Kiyak G, Balikci T. A review of literature:Mosaicoplasty as an alternative treatment for resection of patellar osteoid osteoma and cartilage reconstruction. J Orthop. 2018;15:768–71. doi: 10.1016/j.jor.2018.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Atesok KI, Alman BA, Schemitsch EH, Peyser A, Mankin H. Osteoid osteoma and osteoblastoma. J Am Acad Orthop Surg. 2011;19:678–89. doi: 10.5435/00124635-201111000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Athwal P, Stock H. Osteoid osteoma:A pictorial review. Conn Med. 2014;78(4):233–5. [PubMed] [Google Scholar]
- 17.Iyer RS, Chapman T, Chew FS. Pediatric bone imaging:Diagnostic imaging of osteoid osteoma. AJR Am J Roentgenol. 2012;198:1039–52. doi: 10.2214/AJR.10.7313. [DOI] [PubMed] [Google Scholar]
- 18.Yanagawa T, Watanabe H, Shinozaki T, Ahmed AR, Shirakura K, Takagishi K. The natural history of disappearing bone tumours and tumour-like conditions. Clin Radiol. 2001;56:877–86. doi: 10.1053/crad.2001.0795. [DOI] [PubMed] [Google Scholar]
- 19.Lanza E, Thouvenin Y, Viala P, Sconfienza LM, Poretti D, Cornalba G, et al. Osteoid osteoma treated by percutaneous thermal ablation:When do we fail?A systematic review and guidelines for future reporting. Cardiovasc Intervent Radiol. 2014;37:1530–9. doi: 10.1007/s00270-013-0815-8. [DOI] [PubMed] [Google Scholar]