Abstract
In this case report, we present a novel presentation of acute epiglottitis in a patient with severe acute respiratory syndrome—coronavirus 2 (SARS-CoV-2) who presented to the emergency room in extremis and respiratory failure requiring emergent cricothyrotomy. Epiglottitis has become less common since the introduction and widespread use of the Haemophilus influenzae type B (Hib) vaccine. This reduction in cases has shifted demographics of the disease from the pediatric population towards adults with comorbid conditions. Interestingly there is a high degree of overlap between many of the comorbidities between epiglottitis and COVID-19. The novel severe acute respiratory syndrome—coronavirus 2 (SARS-CoV-2), also referred to as coronavirus disease 19 (COVID-19), has been reported to affect the gastrointestinal tract and neural tissue and has been implicated in necrotizing encephalitis. We report the first known case of the novel SARS-CoV-2 virus presenting with acute epiglottitis.
Keywords: COVID, coronavirus, epiglottitis, cricothyrotomy
BACKGROUND
The novel severe acute respiratory syndrome—coronavirus 2 (SARS-CoV-2), also referred to as coronavirus disease 19 (COVID-19), primarily affects the respiratory tract but has been reported to affect other systems such as gastrointestinal and neural tissues [1].
OBJECTIVE
To describe a unique presentation of acute epiglottitis in a COVID-19 PCR-positive patient with a recent history of E-cigarette use.
CASE REPORT
A 60-year-old Caucasian obese male, BMI 45.78 kg/m2, with past medical history of well-controlled hypertension presented to the emergency department with acute dysphagia, hoarseness of voice, shortness of breath and stridor.
He was in his normal state of health until that morning when he was awoken by a sore throat and difficulty breathing. Incidentally, he had used an e-cigarette with cannabis oil for the first time the previous evening, hours prior to presentation.
On presentation, the patient’s temperature was 37.2°C, blood pressure 152/94 mm Hg, heart rate 133 beats per minute, respiratory rate 28 breaths per minute and oxygen saturation 93% while the patient was breathing ambient air. He was observed to be in mild respiratory distress and sitting upright for comfort. His posterior oropharynx was erythematous with enlarged tonsils which prompted immediate imaging.
The chest X-ray (Fig. 1A) showed minimal blunting of the left costophrenic angle.
Figure 1.
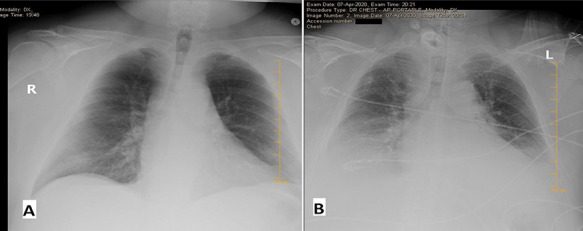
Chest X-ray (CXR) on the day of admission (A) versus Day 3 of admission (B). Initially relatively unremarkable except for minimal blunting of the left costophrenic angle. On Day 3—obtained due to increased PEEP—CXR revealed new bibasilar lung opacities suspicious for COVID-19 pneumonia.
Computed tomography soft tissue neck with IV contrast (Fig. 2) revealed a nearly complete airway obstruction due to marked epiglottic enlargement and pre-epiglottic edema consistent with epiglottitis.
Figure 2.
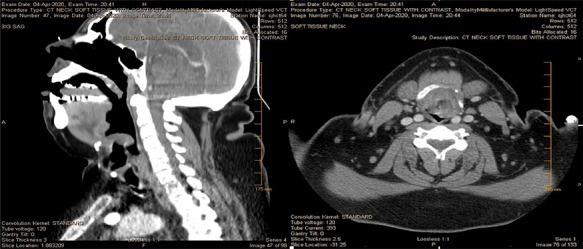
CT of the head/neck on the day of admission, sagittal and axial views. Imaging reveals a nearly complete airway obstruction with thumb sign (seen on the left) due to marked epiglottic enlargement and without tonsillar enlargement or abscesses.
Intubation was unsuccessfully attempted, limited by the severely erythematous, friable and purulent epiglottis. He promptly underwent an emergency cricothyroidotomy and was transferred to the intensive care unit where he was started on empiric ampicillin–sulbactam and azithromycin.
Labs on presentation revealed a white blood cell count of 25.7 k/mm with 84% segmented neutrophils. Platelets were 383 k/mm, and the complete metabolic panel was in normal range.
Additional workup included a rapid streptococcus screening test, monospot test, sputum and blood cultures, Streptococcus pneumoniae and Legionella urine antigen, MRSA PCR of nares, HIV 1 and 2 Ab/Ag and a BioFire respiratory viral panel—all which resulted negative.
On Day 1 after admission, the initial COVID-19 high-sensitivity PCR nasopharyngeal swab came back as negative. However, postoperatively, high positive end expiratory pressure of 14 mmHg on mechanical ventilation was noted, and this combined with his repeat CXR (Fig. 1B) was suspicious of COVID-19 infection. This prompted a repeat test, which on Day 2 was COVID-19 high-sensitivity PCR positive.
On Day 3, the cricothyrotomy was surgically converted to a tracheostomy, and on Day 7 he was successfully weaned off the ventilator, with completion of antibiotics and continued progress.
DISCUSSION
Epiglottitis is an inflammation of the epiglottis which can rapidly progress to a potentially life-threatening airway obstruction. Persons at greater risk for severe epiglottitis include those with older age, male sex, body mass index (BMI) >25.0 kg/m2, diabetes mellitus, epiglottic cyst and pneumonia [2].
Active SARS-CoV-2 replication has been identified in throat swabs [3] and has been described to manifest upper respiratory symptoms such as sore throat [1, 3]. In fact, a number of viral agents have previously been implicated as pathogens causing epiglottitis [4], and therefore it is plausible for SARS-CoV-2 to be the cause for acute epiglottitis in the above case.
Given our patient’s incidental use of an e-cigarette with cannabis oil, another cause of epiglottitis could be noninfectious. We suspect that our patient may have had an underlying COVID-19 infection and the isolated use of the e-cigarette may have in conjunction triggered a localized inflammatory response leading to this dramatic hospital presentation. To our knowledge there is one case report of epiglottitis associated with intermittent e-cigarette use [5].
There is limited understanding of the host epiglottic inflammatory response to COVID-19 infection or e-cigarette use. We suspect that this will not be an isolated case, and further investigation should be considered.
The purpose of sharing this case is to alert the medical community to carry a high index of suspicion for COVID-19 when presented with a similar case and to adhere to the highest level of personal protective gear.
We welcome insight from the ENT community and hope this case may guide safe practices going forward.
Contributor Information
Alexander Fondaw, General Surgery, AMITA Health Saint Joseph Hospital, Chicago, IL 60657, USA.
Muzamil Arshad, Internal Medicine, AMITA Health Saint Joseph Hospital, Chicago, IL 60657, USA.
Saba Batool, Internal Medicine, AMITA Health Saint Joseph Hospital, Chicago, IL 60657, USA.
Brenton Robinson, General Surgery, AMITA Health Saint Joseph Hospital, Chicago, IL 60657, USA.
Toral Patel, Internal Medicine, AMITA Health Saint Joseph Hospital, Chicago, IL 60657, USA.
References
- 1. McIntosh K. Coronavirus disease 2019 (COVID-19): Epidemiology, virology, clinical features, diagnosis, and prevention. In: Hirsch MS, ed. UpToDate. Waltham, MA: UpToDate, 2020. www.uptodate.com. (25 April 2020, date last accessed). [Google Scholar]
- 2. Suzuki S, Yasunaga H, Matsui H, Fushimi K, Yamasoba T. Factors associated with severe epiglottitis in adults: analysis of a Japanese inpatient database. Laryngoscope 2015;125:2072–8. doi: 10.1002/lary.25114. [DOI] [PubMed] [Google Scholar]
- 3. Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Muller MA, et al. . Virological assessment of hospitalized patients with COVID-2019. Nature 2020;581:465–9. [DOI] [PubMed] [Google Scholar]
- 4. Woods CR. Epiglottitis (Supraglottitis). Clinical features and diagnosis. In: Edwards MS, Isaacson GC, Fleisher GR, eds. UpToDate; Waltham, MA: UpToDate, 2020. www.uptodate.com (25 April 2020, date last accessed). [Google Scholar]
- 5. Bozzella M, Magyar M, DeBiasi RL, Ferrer K. Epiglottitis associated with intermittent E-cigarette use: the vagaries of Vaping toxicity. Pediatrics 2020;145:e20192399. [DOI] [PubMed] [Google Scholar]


