Abstract
Herniation through the foramen of Winslow is rare, with a non-specific clinical presentation and his diagnosis may be difficult. A 44-year-old female was admitted with an acute epigastric abdominal pain. A computed tomography showed an internal hernia of the colon in the lesser sac. Laparoscopic reduction of the herniated contents and the fixation of the ascending colon with several non-absorbable sutures were performed. Twenty months after surgery, the patient has not experienced any recurrence. Computed tomography helps practitioners to the preoperative diagnosis of herniation through the foramen of Winslow, to the viability of the herniated contents and presence of occlusion. In case of herniation through the foramen of Winslow favored by a mobile ascending colon with a misapposition of the right Told fascia, the fixation of the colon with a non-absorbable suture was safe and may prevent the risk of recurrent internal hernia and colonic volvulus.
Keywords: internal hernia, foramen of Winslow, laparoscopy, surgery, colon
INTRODUCTION
Herniation through the foramen of Winslow (HFW) is rare and accounts for 0.1% of all abdominal hernias and 8% of all internal hernias [1]. Small bowel is the most frequently involved organ, followed by the terminal ileum and cecum [2]. Clinical presentation of HFW is non-specific and his diagnosis may be difficult [3]. A delayed diagnosis exposed to the risk of viscus ischemia and perforation leading to a high morbidity and mortality rate [1, 3]. The emergency treatment requires a surgical reduction of the herniated contents, in laparoscopy when possible. Methods to prevent recurrent herniation remain a question. The aim of this case was to report a patient presenting a HFW of the colon, with a laparoscopic management of herniation and with the fixation to the lateral wall of the right colon to prevent recurrent herniation.
CASE REPORT
A 44-year-old female patient, without prior abdominal surgery, was admitted to the emergency department with an acute epigastric abdominal pain, without nausea. She presented similar episodes of pain in the past, without having ever requested a medical opinion. Physical examination revealed an acute epigastric pain without signs of peritonitis. Laboratory analyses were within normal limits. A computed tomography showed an internal hernia of the colon in the lesser sac, going back from the liver pedicle (Fig. 1). There were neither occlusion nor ischemia. We performed immediately a diagnostic laparoscopy with one 11-mm umbilical port and two 5-mm ports (one in the left lumbar and one in the hypogastrium). Exploration confirmed that the ascending colon and the right colonic flexure had herniated through the foramen of Winslow (Fig. 2). The colon was reduced with an atraumatic Johann’s graspers and was viable, cecum, ascending colon and the right colonic flexure was mobile due to a misapposition of the right Told fascia. To prevent recurrent herniation we performed the fixation to the lateral wall of the cecum, ascending colon and right colonic flexure with several non-absorbable sutures (Fig. 3). We did not perform the closure of the Winslow’s hiatus. Postoperatively, the patient recovery was uneventful and was discharged home 2 days later. A computed tomography was performed 1 month later for another reason, showing a good result of the right colon fixation on the lateral wall (Fig. 4). Twenty months after surgery, the patient totally recovered and has not experienced any recurrence or occlusion.
Figure 1.
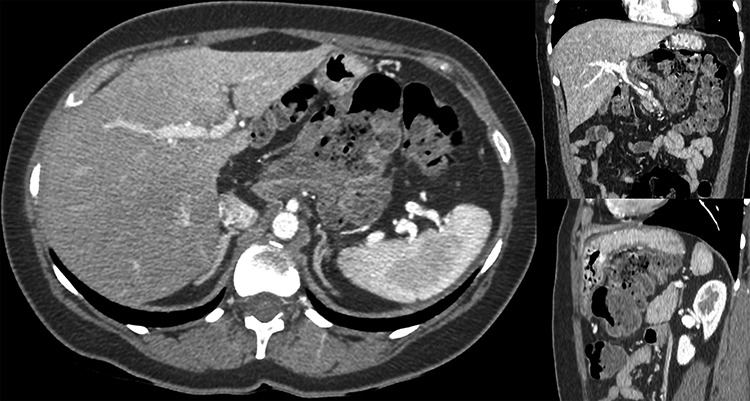
Computed tomography showed an internal hernia of the colon in the lesser sac, going back from the liver pedicle.
Figure 2.
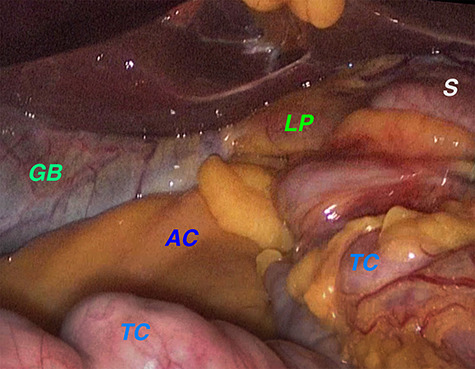
Laparoscopic exploration confirmed that the ascending colon and the right colonic flexure had herniated through the foramen of Winslow. Legend: AC: ascending colon, GB: gallbladder, LP: liver pedicle, S: stomach, TC: transverse colon.
Figure 3.
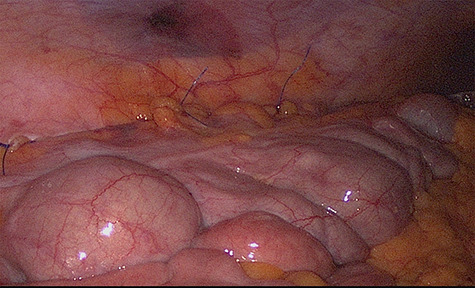
Fixation to the lateral wall of the ascending colon with several non-absorbable sutures.
Figure 4.

Postoperative computed tomography (coronal section) showed a good result of the right colon fixation on the lateral wall.
DISCUSSION
Clinical signs of HFW are often related to small bowel obstruction and usually include an isolated epigastric pain or associated with nausea, vomiting and jaundice (by compression of the extra-hepatic biliary tract) [2]. This non-specific presentation makes preoperative accurate diagnosis difficult and can lead to delayed diagnosis and therefore delayed surgical care. A computed tomography helps practitioners to the diagnosis of HFW and to the viability of the herniated contents [4, 2], which allows the surgeon to consider a laparoscopic approach. Despite this, HFW is diagnosed preoperatively in less than 10% of the cases [5, 6]. Laparoscopic management in case of internal hernia can be used as much as diagnostic than therapeutic, when possible, and propose enhanced recovery after surgical intervention. In case of intestinal necrosis, an intestinal resection is necessary [3]. In case of difficulties during reduction, the Winslow’s foramen needs to be enlarged by performing a Kocher manoeuvre, by performing a colo-epiploic detachment or needle decompression of the involved bowel [1, 3]. In this case, there were no occlusion and the reduction was easily performed in laparoscopy. After reduction, when herniated content is viable, there is no consensus concerning the prevention of hernia recurrence. There are three main contributing factors in the HFW genesis [3], excessive viscera mobility, enlargement of the foramen of Winslow and an increased intra-abdominal pressure. Some others anatomical risk factors favoured HFW like a long small bowel mesentery or an atrophic greater omentum [2, 4]. The cause of the HFW should be investigated and treated, avoiding increased morbidity. In our case cecum, ascending colon and the right colonic flexure were mobile due to misapposition of the right Told fascia and the patient had a constipation that may increase intra-abdominal pressure. This presentation lead to performed the fixation of the cecum, ascending colon and right colonic flexure to the lateral abdominal wall with non-absorbable sutures to prevent the risk of recurrent internal hernia and colonic volvulus and to treat his constipation post-operatively. Some teams [1] have proposed a preventative segmental resection if the bowel lacks anatomical fixation, but can expose to anastomotic leakage. In this case we do not close the foramen because we treated the predisposing factor of HFW. The usefulness of the closure of the foramen of Winslow is debated, some surgeons were favourable to close the foramen of Winslow via suture [7], whereas others were unfavourable due the risk of vascular wounds and portal vein thrombosis [8, 9]. Other teams pack the foramen with the greater omentum [8, 1]. To date, with or without foramen closure, there has not been a report of recurrence [3], possibly due to adhesions obliterating the foramen or because the foramen is kept closed by normal intra-abdominal pressure [3, 9].
Computed tomography helps practitioners to the preoperative diagnosis of HFW, the study of the herniated contents viability and presence of occlusion. These are important in order to propose a laparoscopic approach when possible. The cause of the HFW should be investigated and treated, avoiding increased morbidity. After reduction, in case of HFW favoured by a mobile cecum and ascending colon due to misapposition of the right Told fascia, the fixation of the colon to the lateral abdominal wall with non-absorbable suture was safe, with a low duration of hospitalization and may prevent the risk of recurrent internal hernia and colonic volvulus.
ACKNOWLEDGMENTS
The authors thank Romain Isenbart for his contribution in this paper.
Contributor Information
Cyrille Buisset, Department of Digestive, Endocrine and Metabolic Surgery, Hôpital Robert Schuman - Hôpitaux Privés de Metz, Metz, France.
Agathe Postillon, Department of Digestive, Hepato-Biliary and Endocrine Surgery, University Hospital of Nancy, Vandoeuvre-les-Nancy, France.
Sandrine Aziz, Department of Digestive, Endocrine and Metabolic Surgery, Hôpital Robert Schuman - Hôpitaux Privés de Metz, Metz, France.
Florian Bilbault, Department of Digestive, Endocrine and Metabolic Surgery, Hôpital Robert Schuman - Hôpitaux Privés de Metz, Metz, France.
Guillaume Hoch, Department of Digestive, Endocrine and Metabolic Surgery, Hôpital Robert Schuman - Hôpitaux Privés de Metz, Metz, France.
Jean-Philippe Nesseler, Department of Digestive, Endocrine and Metabolic Surgery, Hôpital Robert Schuman - Hôpitaux Privés de Metz, Metz, France.
Marc Johann, Department of Digestive, Endocrine and Metabolic Surgery, Hôpital Robert Schuman - Hôpitaux Privés de Metz, Metz, France.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- 1. Harnsberger CR, McLemore EC, Broderick RC, Fuchs HF, Yu PT, Berducci M, et al. Foramen of Winslow hernia: a minimally invasive approach. Surg Endosc 2015;29:2385–8. [DOI] [PubMed] [Google Scholar]
- 2. Martin LC, Merkle EM, Thompson WM. Review of internal hernias: radiographic and clinical findings. Am J Roentgenol 2006;186:703–17. [DOI] [PubMed] [Google Scholar]
- 3. Moris D, Tsilimigras DI, Yerokun B, Seymour KA, Guerron AD, Fong PA, et al. Foramen of Winslow hernia: a review of the literature highlighting the role of laparoscopy. J Gastrointest Surg 2019;23:2093–9. [DOI] [PubMed] [Google Scholar]
- 4. Takeyama N, Gokan T, Ohgiya Y, Satoh S, Hashizume T, Hataya K, et al. CT of internal hernias. Radiographics 2005;25:997–1015. [DOI] [PubMed] [Google Scholar]
- 5. Osvaldt AB, Mossmann DF, Bersch VP, Rohde L. Intestinal obstruction caused by a foramen of Winslow hernia. Am J Surg 2008;196:242–4. [DOI] [PubMed] [Google Scholar]
- 6. Downs P, Downes N, Zayshlyy E, Esper C, Guiseppucci P. Internal hernia through the foramen of Winslow. J Surg Case Rep 2018;12:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Garg S, Flumeri-Perez G, Perveen S, DeNoto G. Laparoscopic repair of foramen of Winslow hernia. Int J Angiol 2015;25:064–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tse G, Sollei T, Ali SM, Kukreja N. Caecal herniation through the foramen of Winslow. BJRcase Rep 2016;2:20150330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Leung E, Bramhall S, Kumar P, Mourad M, Ahmed A. Internal herniation through foramen of Winslow: a diagnosis not to be missed. Clin Med Insights Gastroenterol 2016;9:21–33. [DOI] [PMC free article] [PubMed] [Google Scholar]


