Abstract
Datasets highlighting effects of ketogenic diet (KD) in a glycogen storage disease type IIIa patient is presented with the longest patient follow up report to date. Now a 15-year old girl with GSD type IIIa, diagnosed at 1 year of age, had initially introduced treatment with diet high carbohydrates, according to the recommendations. Progressively she developed left ventricular obstructive hypertrophy, hepatomegaly and skeletal myopathy. At the age of 11 years, she was introduced KD and continuous ketosis has been maintained for over 4 years providing longest reported follow up to date. KD introduction lead to a normalization of left ventricular parameters and ventricular mass and to an improvement in hepatic injury markers and decrease in liver size.
We provided a table with biochemical parameters, a table providing detailed diet composition, tables with cardiac and hepatic measures and figures depicting cardiac NMR images; all the tables/figures are provided referring to the KD introduction (values prior/after). Interpretation of this data can be found in a case report article titled “Normalization of obstructive cardiomyopathy and improvement of hepatopathy on ketogenic diet in patient with glycogen storage disease (GSD) type IIIa”.
Keywords: Inborn Genetic Diseases; Glycogen storage disease; Glycogen Storage Disease Type III; Cardiomyopathy, Hypertrophic; Diet, Ketogenic
Specifications Table
| Subject | Endocrinology, Diabetes and Metabolism |
|---|---|
| Specific subject area | Inborn errors of metabolism; Glycogen storage diseases |
| Type of data | Table Image |
| How data were acquired | NMR, Ultrasound, Laboratory, Dietary plans. |
| Data format | Raw |
| Parameters for data collection | Blood samplings were periodically taken in fasting state. Cardiac NMR was made at the 11 years old and repeated at the age of 15 with a high definition MRI machine. Abdominal ultrasound was developed by a image specialist. Dieticians calculated and constituted the diet therapy, indicated the dietary plan to the patient and checked her adherence. |
| Description of data collection | All the data were provided at the UMC - University Children's Hospital Ljubljana, Slovenia. The blood sampling, ultrasounds and dietary counselling were performed at the UMC - University Children's Hospital Ljubljana, Slovenia at the regular visits of patient. The NMR was performed in the UMC - Clinical Institute of Radiology Ljubljana, Slovenia. All the data (biochemical, imaging) have been recorded and obtained from the electronic medical record. |
| Data source location | UMC - University Children's Hospital Ljubljana. Ljubljana Slovenia 3G3C+MM Ljubljana, Slovenia |
| Data accessibility | Repository name: Mendeley Data Direct URL to data: DOI: 10.17632/6xxrvndt2m.2 https://data.mendeley.com/datasets/6xxrvndt2m/2 |
| Related research article [1] | T. Marusic, M. Zerjav Tansek, A. Sirca Campa, A. Mezek, P. Berden, T. Battelino; U. Groselj. Normalization of obstructive cardiomyopathy and improvement of hepatopathy on ketogenic diet in patient with glycogen storage disease (GSD) type IIIa. Molecular Genetics and Metabolism Reports. (2020)24:100628. https://doi.org/10.1016/j.ymgmr.2020.100628 |
Value of the Data
-
•
The data could be important in the process of gaining evidence about ketogenic diet (KD) as a treatment for patients with GSD type IIIa.
-
•
The data might inform clinicians in prospective cases, it can add to the scientific reviews gaining evidence on KD in GSD type IIIa and could also be instrumental in designing the research protocols in the issue.
-
•
Laboratory findings and cardiac MRI results could be used for a cases series publication or for designing a prospective clinical trial. Dietitians and clinicians could also apply the dietary plan provided as a tool for other comparable GSD patients.
-
•
The data about KD in patients with GSD type IIIa might be encompassed into the recommendations on GSD type IIIa management strategies or updated guidelines for prospective patients and also to inform future research.
-
•
As a very rare disease, each new case report brings value to the global medical community.
-
•
It is worth mentioning that our reported study has the longest follow-up to date.
2. Data Description
We observed the impact of ketogenic diet (KD) on a 15- years old female patient with GSD IIIA. First, we presented a timeline, showing laboratory values before and after the KD onset (setting 0 months as the KD introduction) and focused on selected cardiac and hepatic-metabolic biochemical biomarkers (Table 1). Alkaline phosphatase and LDH, as non-specific cellular injury markers, sharply decreased within two months of KD onset. AST and ALT, hepatic injury markers, decreased more than twice soon after KD introduction. CK and myoglobin -muscle injury markers- and CK-MB and ProBNP -related to cardiac injury- decreased soon after KD introduction. Triglycerides and LDL-C decreased at the beginning, with a slight later increase, related to a high fat diet. Finally, Hydroxybutyrate, a measurable ketonic body for KD monitoring, fluctuated over time but remained elevated throughout the follow-up.
Table 1.
The impact of ketosis on selected cardiac and hepatic-metabolic biochemical biomarkers, setting 0 months as the KD introduction. S-LDH = Serum Lactate dehydrogenase. AST = Aspartate transaminase. ALT = alanine aminotransferase. CK = creatine kinase. CK-MB = creatine kinase myocardial band. ProBNP = Prohormone of brain natriuretic peptide. LDL-C = low-density lipoprotein cholesterol.
| Months | -1 | -1 | -1 | 0 | 0 | 2 | 3 | 4 | 5 | 7 | 9 | 12 | 15 | 17 | 25 | 28 | 33 | 36 | 39 | 42 | 47 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AGE | 11.3 | 11.3 | 11.4 | 11.4 | 11.4 | 11.6 | 11.7 | 11.7 | 11.8 | 12.0 | 12.2 | 12.4 | 12.6 | 12.9 | 13.5 | 13.7 | 14.2 | 14.4 | 14.6 | 14.9 | 15.4 |
| DATE | 3/6/2015 | 15/6/2015 | 22/6/2015 | 23/6/2015 | 22/7/2015 | 3/9/2015 | 8/10/2015 | 10/11/2015 | 11/12/2015 | 11/2/2016 | 6/4/2016 | 28/6/2016 | 29/9/2016 | 22/12/2016 | 26/7/2017 | 9/11/2017 | 18/4/2018 | 26/6/2018 | 25/9/2018 | 15/1/2019 | 21/6/2019 |
| Alkaline phosphatase (ukat/L) | 11.64 | ketonic diet | 6.19 | 4.58 | 5.02 | 5.76 | 6.11 | 6.51 | 6.51 | 5.17 | 5.48 | 5.91 | 5.25 | 6.95 | 6.15 | 5.59 | 6.34 | 3.97 | 6.14 | ||
| S-LDH (ukat/L) | 13.61 | 14.22 | ketonic diet | 8.73 | 5.36 | 5.62 | 5.41 | 4.54 | 5.18 | 4.99 | 4.49 | 4.11 | 3.91 | 4.92 | 4.09 | 4.66 | 4.73 | 5.53 | 5.77 | ||
| AST (ukat/L) | 4.97 | 4.74 | 6.78 | ketonic diet | 4.3 | 3.23 | 2.11 | 3.01 | 2.69 | 1.5 | 2.47 | 2.49 | 2.26 | 2.64 | 2.56 | 3.95 | 2.8 | 2.42 | 3.15 | 3.4 | 2.48 |
| ALT (ukat/L) | 5.44 | 4.15 | 6.6 | ketonic diet | 3.85 | 2.69 | 2.03 | 2.92 | 2.43 | 1.69 | 2.57 | 2.52 | 2.37 | 3 | 3.52 | 4.03 | 3.15 | 2.95 | 2.99 | 3.44 | 4.19 |
| GGT (ukat/L) | 0.97 | 0.77 | ketonic diet | 0.6 | 0.34 | 0.3 | 0.4 | 0.42 | 0.62 | 0.64 | 0.61 | 0.65 | 0.92 | 1.15 | 1.24 | 0.93 | 0.73 | 0.81 | 0.67 | 1.06 | |
| CK (ukat/L) | 53.10 | 65.70 | 64.70 | ketonic diet | 41.60 | 32.90 | 16.60 | 13.60 | 16.00 | 7.60 | 14.20 | 7.10 | 12.29 | 8.82 | 9.54 | 25.66 | 13.66 | 13.24 | 14.48 | 17.93 | 26.46 |
| CK-MB (ukat/L) | 2.17 | 2.50 | ketonic diet | 1.09 | 0.73 | 0.42 | 0.27 | 0.25 | 0.11 | 0.16 | 0.10 | 0.13 | 0.08 | 0.10 | 0.17 | 0.18 | 0.17 | 0.16 | 0.20 | 0.35 | |
| Mioglobin (nmol/L) | 22.35 | 21.42 | ketonic diet | 10.51 | 9.91 | 6.87 | 8.39 | 4.21 | 4.62 | 4.76 | 4.29 | 2.97 | 5.18 | 5.44 | 6.25 | 7.87 | 5.77 | 6.80 | 8.31 | ||
| Triglicerid (mmol/L) | 2.6 | 4.1 | ketonic diet | 2 | 1.3 | 2.4 | 2.1 | 1.4 | 1.4 | 2.5 | 1.9 | 1.3 | 1.6 | 1.6 | 2.6 | 1.3 | 1.7 | 2.7 | 2.7 | 4.5 | |
| LDL (mmol/L) | 3.3 | 1.5 | 2.4 | ketonic diet | 1.7 | 1.9 | 1.6 | 2 | 2.1 | 2.2 | 2.5 | 2.4 | 1.9 | 2.7 | 2.5 | 4.2 | 2.9 | 2.7 | 4 | 5.1 | 4.6 |
| ProBNP (pmol/L) | 36.2 | ketonic diet | 10.0 | 13.4 | 12.9 | 14.0 | 10.0 | 4.3 | 5.6 | 6.3 | 3.1 | 6.9 | 11.0 | 7.7 | 2.9 | 5.8 | |||||
| β-hydroxy-butyrate (µmol/L) | ketonic diet | 2439 | 2043 | 1470 | 3033 | 1099 | 1155 | 1204 | 1305 | 212 | 1135 | 1190 | 616 |
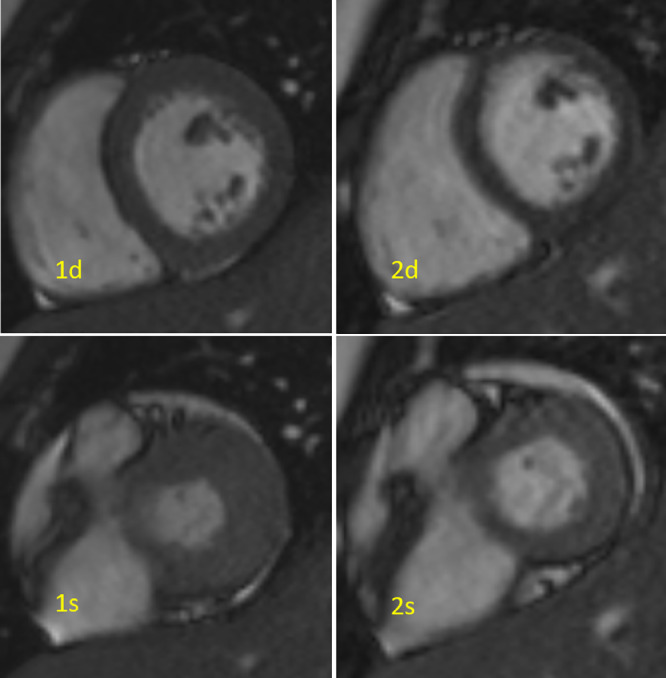
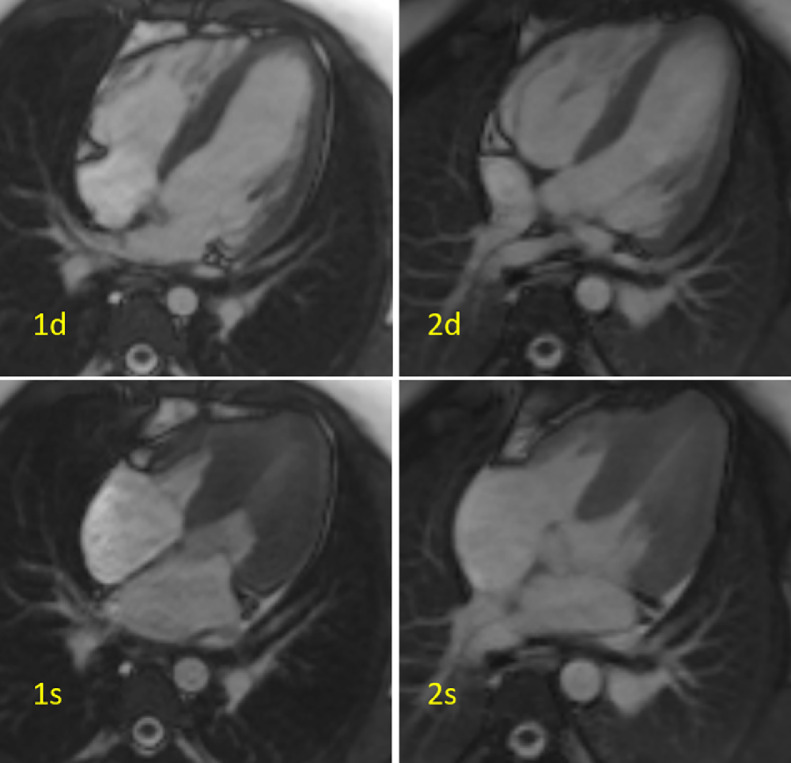
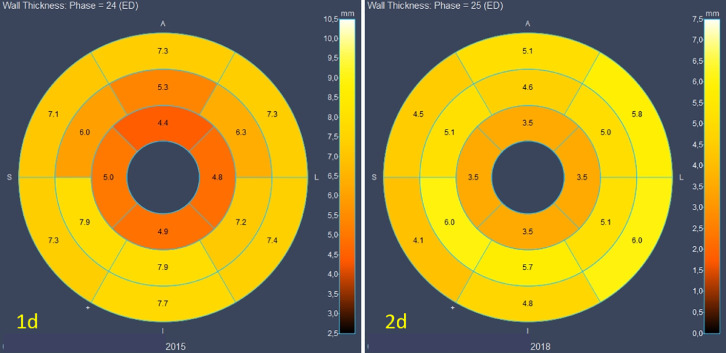
On the other hand, we observed the effect of the KD in cardiac MRI at the onset of the KD and after 16 months of maintaining ketosis (Table 2 and Images 1–2). It shows a decrease of total left ventricular mass index (LVMI) (from 58 g/m2 to 37 g/m2) and thickness of left ventricular walls (lateral wall from 10 to 5 cm, septal wall from 9 to 5 cm and inferosental wall from 10 to 7 cm). The end systolic and diastolic volume, and the ejection fraction were calculated, showing no residual outflow obstruction. Finally, no fibrosis was observed in cardiac tissue, but a normalization of obstructive cardiomyopathy. In addition, the 17- segment plots proposed by AHA (American Heart Association) -representing the myocardium in diastole from cardiac short axis cine MRI- shows a decrease in thickness of left ventricle walls 3 years after the onset of KD (Image 3).
Table 2.
Cardiac MRI results at the onset of ketogenic diet (KD), after 16 months and after 40 months of maintaining ketosis. LVMI = Left ventricular mass index.
| Cardiac MRI parameters | At onset of KD | After 16 months | After 40 months |
|---|---|---|---|
| Lateral wall | 9 mm | 4–5 mm | 4–5 mm |
| Septum wall | 8–9 mm | 5–6 mm | 5–6 mm |
| Inferoseptal wall | 10 mm | 6 mm | 7 mm |
| Myocardial mass | 70 g (58 g/m2) | 35 r (30 g/m2) | 50 g (37 g/m2) |
| End diastolic volume | 75 ml (63 ml/m2) | 64 ml (52 ml/m2) | 80 ml (62 ml/m2) |
| End systolic volume | 10 ml (8,4 ml/m2) | 15 ml (12 ml/m2) | 25 ml (19 ml/m2) |
| Ejection fraction | 87% | 76% | 69% |
| Fibrosis signs | none | none | none |
| Myocardial hypertrophy | obstructive | none | none |
Fig. 1.
Cardiac MRI, cine short axis view at mid-segment level. 1- before treatment, 2- after treatment. Myocardial thickening before treatment, normal myocardium after treatment. d = diastolic phase, s = systolic phase.
Fig. 2.
Cardiac MRI, cine four chamber view. 1- before treatment, 2- after treatment. Myocardial thickening before treatment, normal myocardium after treatment. d = diastolic phase, s = systolic phase.
Fig. 3.
AHA (American Heart Association) 17- segment plots of myocardial thickness in diastole from cardiac short axis cine MRI, 1d- before treatment, 2d- after treatment. ED = end diastole. A = anterior. L = lateral. I = inferior. S = septal.
Furthermore, liver sizes at the onset of KD and after 6 months of maintaining ketosis were calculated on ultrasound (Table 3). The standard liver measures sharply decreased in 6 months after the incorporation of KD (sternal line 129 to 110 mm; medioclavicular line 162 to 137 mm; anterior axillary line 167 to 146 mm) and sustained in normal range after 4 years.
Table 3.
Liver measures at the onset of ketogenic diet (KD) and after 6 months of maintaining ketosis.
| Liver measures | At the onset of KD | After 6 months |
|---|---|---|
| Sternal line | 129 mm | 110 mm |
| Medioclavicular line | 162 mm | 137 mm |
| Anterior axillary line | 167 mm | 146 mm |
Finally, we present a diet therapy timeline, registered from 2004 to 2019 at the dietician visits and in the food diary (Table 4). In 2015 the patient started with the KD. The timeline shows anthropometric characteristics, the diet composition, total and relative energy intakes, and notes showing the patient's adherence.
Table 4.
Diet therapy over time, from 2004 to 2019. In 2015 the patient started with the ketogenic diet (KD). BMI = body mass index.
| Year | Age | Height | Weight | BMI | Diet basic | Meals | Energy | Carb | Proteins | Fat | Cornstarch | Notes | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2009/04 | 5 years | Diet therapy | Classic diet GSD IIIa | 5 meals (interval 3 h) -all meals energy and nutritional equal- + 1 night meal 20 g oatmeal + 200 ml Prosure drink | 1370 kcal | 178.0 g (53%) | 78.1 g (23%) | 35.0 g (23%) | |||||
| 2009/11 | Food diary analysis | 8-10 meals (interval 1–3 h) + 1 night meal 20 g oatmeal + 100 ml Prosure drink | 1580 kcal | 244.9 g (62%) | 79.0 g (20%) | 31.6% (18%) | 20 g oatmeal + 100 ml Prosure at 23:00 | Lot of simple sugars | |||||
| 2010/03 | 6 years | Diet therapy | Classic diet GSD IIIa | 5 meals (interval 3 h) -all meals energy and nutritional equal- + 1 night meal 20 g oatmeal + 200 ml Prosure drink | 1500 kcal | 200.0 g (53%) | 86.2 g (23%) | 38.3 g (23%) | |||||
| 2010/11 | Food diary analysis | 8–10 meals (interval 1–3 h) + 40 g cornstarch at 23:00 | 1842 kcal | 303 g (66%) | 50.6 g (11%) | 47.1 g (23%) | 30 g corn starch + 100 ml Supportan dink at 23:00 | Lot of simple sugars. Supplement Supportan drink 200 ml / day | |||||
| 2011/04 | 7 years | 117.1 cm (5p) | 23.4 kg (30p) | 17 (66p) | Diet therapy | Classic diet GSD IIIa | 5 meals (interval 3 h) -all meals energy and nutritional equal- + 1 night meal 30 g corn starch | 1600 kcal | 210 g (53%) | 92 g (23%) | 41 g (23%) | ||
| 2011/11 | Food diary analysis | 8–10 meals (interval 1–3 h) + 40 g corn starch at 23:00 | 1932 kcal | 313.9 g (65%) | 72.4 g (15%) | 43.0 g (20%) | 30 g cornstarch + 100 ml Supported dink at 23:00 | Lot of simple sugars. Supplement Supportan drink 200 ml / day | |||||
| 2012–2013 | 8–9 years | 118.3 cm (3p) | 23.7 kg (23p) | 16.9 (66p) | no data | ||||||||
| 2014/4 | 10 years | 129.9 cm (3p) | 34.15 kg (46p) | 20.4 (87p) | Food diary analysis | 8–10 meals (interval 1–3 h) + 40 g corn starch at 23:00 | 2408 kcal | 363 g (61%) | 97.0 g (15%) | 59.1 g 22%) | 40 g corn starch + 100 ml Fresubin protein drink at 23:00 | Lot of simple sugars. Supplement Supportan drink 200 ml / day | |
| 2014/04 | Diet therapy | Classic diet GSD IIIa | 5 meals (interval 3 h) -all meals energy and nutritional equal- + 1 night meal 30 g corn starch | 1800 kcal | 178.0 g (53%) | 78.1 g (23%) | 35.0 g (23%) | ||||||
| 2015/5 | 11 years | 135 cm | 39.1 kg | 21.4 (91p) | Food diary analysis | 11–14 meals (interval 1–1.5 h) + 40 g corn starch at 23:00 | 2549 kcal | 347 g (55%) | 114.0 g (18%) | 75.3 g (27%) | 40 g corn starch at 23:00 + 100 ml Fresubin protein drink | Lot of simple sugars. Supplement Supportan drink 200 ml / day + Fresubin Energy 200 ml / day | |
| 2015/05 | 11 years | 135 cm | 39.1 kg | 21.4 (91p) | Diet therapy | Transition to ketogenic diet | 6 meals (interval 3.5 h), last meal at 23:00 in the ratio 4: 1 | 2000 kcal | 11.7 g (2%) | 61.0 g (11%) | 204.2 g (87%) | Ketocal 4: 1 for night meal | |
| 2016/6 | 12 years | 138.5 cm (3p) | 36.4 kg (20p)) | 19.0 (59p) | Food diary analysis | Ketogenic diet 2.5: 1 | 6 meals (interval 3.5 h), last meal at 23:00 in a ratio of 4: 1 | 2123 kcal | 11.7 g (2%) | 61.0 g (11%) | 204, 2 g (87%) | Ketocal 4: 1 for a night meal | Follows the diet |
| 2016/09 | Diet therapy | Ketogenic diet 2.5: 1 | 6 meals (interval 3.5 h) last meal at 23:00 in a ratio of 4: 1 | 2000 kcal | 10.0 g (2%) | 60,0 g (12%) | 190,0 g (86%) | Ketocal 4: 1, for a night meal | |||||
| 2018/9 | 14 | 145,3 cm (1p) | 43.3 kg (12p) | 20.4 (59p) | Food diary analysis | Ketogenic diet 2.8: 1 | 6 meals (interval 3.5 h) last meal at 23:00 in a ratio of 4: 1 | 1800 kcal | 10.0 g (2%) | 51.9 g (12%) | 175.0 g (86%) | Ketocal 4: 1 for night meal | Follows the diet |
| 2018/09 | Diet therapy | Ketogenic diet 2.5: 1 | 6 meals (interval 3.5 h) last meal at 23:00 in a ratio of 4: 1 | 2000 kcal | 10.0 g (2%) | 60.0 g (12%) | 190 0g (86%) | Ketocal 4: 1 for night meal | |||||
| 2019/6 | 15 years | 147.7 cm (1p) | 43.8 kg (5p) | 19.8 (44p) | Food diary analysis * | Ketogenic diet 1.5: 1 * desserts | 4–5 meals (interval 3.5 h) last meal at 23:00 in a ratio of 4: 1 | 1700 kcal * | 148 g (35%) * | 63.7 g (15%) * | 94.4 g (50%) * | Ketocal 4: 1 for a night meal | Tired of the diet |
| 2019/06 | Diet therapy | Ketogenic diet 2.5: 1 | 6 meals (interval 3.5 h) last meal at 23:00 in a ratio of 4: 1 | 2000 kcal | 10.0 g (2%) | 60.0 g (12%) | 190.0 g (86%) | Ketocal 4: 1 for night meal |
Does not reflect the real situation (elevated TG, fallen ketone bodies)
All the data was also added to the Mendeley repository (http://dx.doi.org/10.17632/6xxrvndt2m.2).
3. Experimental Design, Materials and Methods
This is a case report of a now 15-year old girl with GSD type IIIa diagnosed at 1 year of age. At that time she was introduced a high carbohydrates diet (frequent diurnal and nocturnal cornstarch meals); carbohydrates (9 g/kg per day (g/kg/d)) contributed 53% daily calories, proteins (4 g/kg/d) contributed 23% and fats (1.8 g/kg/d) contributed another 23%, according to the recommendations [2]. Progressively she developed left ventricular obstructive hypertrophy, hepatomegaly and skeletal myopathy with highly elevated liver and muscle enzymes, as previously reported [3], [4], [5], [6]. She also presented recurrent hypoglycemic events despite treatment with frequent diurnal and nocturnal meals with cornstarch supplements. Due to progressive obstructive cardiomyopathy, she was introduced to a ketogenic diet at the age of 11. The diet consisted of ketogenic ratios of 2.5:1; fats (5.2 g/kg/d) contributed 87% daily calories, proteins (1.6 g/kg/d) contributed 11% and carbohydrates (0.3 g/kg/d) contributed 2%. Continuous ketosis was maintained for over 4 years. Clinical support by attending physicians and experienced clinical dietitians was provided (e.g. helping with practical dilemmas via e-mail/phone soon after they arise). Periodic abdominal ultrasounds and cardiac MRI were performed. The blood sampling at regular outpatient visits was performed in a fasting state, as recommended [2,7]. For home monitoring, she daily measured the ketones in urine using a semiquantitative test.
4. Ethics Statement
Written informed consent for publication of their clinical details and/or clinical images was obtained from the patient/parent/guardian/relative of the patient.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships which have, or could be perceived to have, influenced the work reported in this article.
Acknowledgments
We would like to thank clinical dietitian Helena Kobe MSc, for her consultations with the family. Study was partly funded by the Slovenian Research Agency project V3-1505 and program P3-0343.
References
- 1.Marusic T., Zerjav Tansek M., Sirca Campa A., Mezek A., Berden P., Battelino T., Groselj U. Normalization of obstructive cardiomyopathy and improvement of hepatopathy on ketogenic diet in patient with glycogen storage disease (GSD) type IIIa. Mol. Genet. Metab. 2020;24 doi: 10.1016/j.ymgmr.2020.100628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kishnani P.S., Austin S.L., Arn P., Bali D.S., Boney A., Case L.E. Glycogen storage disease Type III diagnosis and management guidelines. Gen. Med. 2010;12(7):446–463. doi: 10.1097/GIM.0b013e3181e655b6. [DOI] [PubMed] [Google Scholar]
- 3.Mayorandan S., Meyer U., Hartmann H., Das A.M. Glycogen storage disease type III: modified Atkins diet improves myopathy. Orphanet. J. Rare Dis. 2014;28(9):196. doi: 10.1186/s13023-014-0196-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brambilla A., Mannarino S., Pretese R., Gasperini S., Galimberti C., Parini R. Improvement of Cardiomyopathy after High-Fat Diet in two siblings with glycogen storage disease Type III. JIMD Rep. 2014;17:91–95. doi: 10.1007/8904_2014_343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Francini-Pesenti F., Tresso S., Vitturi N. Modified Atkins ketogenic diet improves heart and skeletal muscle function in glycogen storage disease type III. Acta Myol. 2019;38:17–20. [PMC free article] [PubMed] [Google Scholar]
- 6.Rossi A., Hoogeveen I.J., Bastek V.B., de Boer F., Montanari C., Meyer U. Dietary lipids in glycogen storage disease type III: a systematic literature study, case studies and future recommendations. JIMD. 2020;43(4):770–777. doi: 10.1002/jimd.12224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dagli A., Sentner C.P., Weinstein D.A. Glycogen storage disease Type III. Gene. Rev. 2010 [Google Scholar]