Abstract
Introduction
Computer-based video training (CBVT) of surgical skills overcomes limitations of 1:1 instruction. We hypothesized that a self-directed CBVT program could teach novices by dividing basic surgical skills into sequential, easily-mastered steps.
Methods
We developed a 12 video program teaching basic knot tying and suturing skills introduced in discrete, incremental steps. Students were evaluated pre- and post-course with a self-assessment, a written exam and a skill assessment.
Results
Students (n = 221) who completed the course demonstrated significant improvement. Their average pre-course product quality score and assessment of technique using standard Global Rating Scale (GRS) were <0.4 for 6 measured skills (scale 0–5) and increased post-course to ≥3.25 except for the skill tying on tension whose GRS = 2.51. Average speed increased for all skills. Students’ self-ratings (scale 1–5) increased from an average of 1.4 ± 0.7 pre-elective to 3.9 ± 0.9 post-elective across all skills (P < 0.01).
Conclusion
Self-directed, incremental and sequential video training is effective teaching basic surgical skills and may be a model to teach other skills or to play a larger role in remote learning.
Keywords: Surgical education, Knot tying, Suturing, Basic surgical skills, Computer-based video training, Remote training
Graphical abstract
A computer-based sequential and incremental video training program was effective in teaching 221 pre-clincal medical students basic knot tying and suturing skills surgical skills without faculty involvement. Students demonstrated marked improvement in technique, speed and the end product for a number of skills as assessed by a blinded practical skill exam.
Introduction
Teaching surgical skills has traditionally followed an apprenticeship model in which experienced practitioners taught trainees one-on-one or in small groups. Such training often occurs in the operating room. A disadvantage of this approach is that the trainee’s learning is limited by instructor availability and the impetus to timely conduct operative procedures. Furthermore, as training paradigms shorten, and the complexity of surgical procedures increase, surgical residents are under pressure to demonstrate competency with fewer training hours.1, 2, 3 Thus it behooves medical schools and training programs to teach basic skills as early as possible, optimally prior to exposure in an operating room. Early training would allow the trainee to focus time in the operating room on the conduct of the operation and the acquisition of more complex skills.
Video instruction has been used to teach a variety of surgical skills.4, 5, 6, 7, 8 Delivering this instruction via a computer platform, so called computer-based video training (CBVT), is especially advantageous because it offers flexible opportunities for trainees to learn and practice on their own in a self-paced manner. Teaching basic surgical skills using CBVT has been shown to be equally effective as faculty instruction in a variety of settings.4, 5, 6 Existing reports using CBVT, however, have been limited both in the scope of skills taught or the number of trainees studied.4, 5, 6, 7, 8, 9 Some curricula required establishment of a skills lab staffed with knowledgeable instructors.10, 11, 12, 13 More complex training has been described but it has typically taught a focused skill to those with prior surgical experience.14
The recent COVID-19 pandemic has reinforced the need to develop programs for remote self-directed education.15 Medical schools and residency training programs are struggling to overcome the practical and logistical challenges created by this health crisis.15 , 16 For more than 10 years, medical schools have been developing a curriculum that has replaced standard classroom lectures with multidisciplinary and multimedia education.17
In this report we describe the development, implementation, assessment, and results of a novel, video-based course for teaching fundamental knot-tying and suturing skills to pre-clinical medical students. Our objective was to create a program which could train a large number of students without the need for a skills lab or any one-on-one instruction.
Materials and methods
Computer-based video design
The authors (NK, VQ) developed a novel curriculum containing a total of 12 stepwise tutorial videos which averaged 8 min (range, 3–15 min). Videos included didactic information on use of instruments, suture, and needles, demonstration of one or more related focused skills, best-practice tips, information about use of the skill in surgical practice, advice on practicing the skill, and addressed common mistakes and questions (Table 1 . Representative videos can be accessed: Knot-Tying 3 at https://youtu.be/elOryNu91QY and Suturing 2 at https://youtu.be/elOryNu91QY). In creating the videos, we sought to divide each skill into basic components which could be easily learned. A number of basic steps were introduced sequentially to allow for the acquisition of a specific skill. Each video reinforced the skills and hand movements of prior videos and introduced a limited number of new hand movements and skills.
Table 1.
Content in each video.
| Video | Title | Contents |
|---|---|---|
| Knot-tying 1 | 2-Handed Tie: Basic Mechanics | How to make square knots, cross hands, perform overhand and underhand half hitch (using rope) |
| Knot-tying 2 | 2-Handed Tie: Tying Concepts 1 | Tying using a rail, making knot come down flat, sliding knot down on rail, locking knot, hand movements to adjust suture length when tying (using rope) |
| Knot-tying 3 | 2-Handed Tie: Tying Concepts 2 | Using suture: tying multiple knots, tying on tension, introduction to suture size and material |
| Knot-tying 4 | 2-Handed Tie: Tying concepts 3 | Tying at faster speeds, tying with finer suture, tying into depth |
| Knot-tying 5 | 1-Handed Tie: Basic Mechanics | How to perform overhand and underhand half hitch |
| Knot-tying 6 | 1-Handed Tie: Tying Concepts 1 | Making knot come down flat, securing knot, tying on rail, sliding knot, square knot, tying on tension, tying at faster speeds |
| Knot-tying 7 | 1-Handed Tie: Tying Concepts 2 | Tying with finer suture with and without tension, tying into depth |
| Suturing 1 | Introduction to Instruments | Using forceps, hand motion to hold, secure and release clamps or needle driver |
| Suturing 2 | Needle Handling | Passing suture needle through tissue, capture and reload needle on needle driver, improved needle driver mechanics |
| Suturing 3 | Simple Interrupted Suture | How to perform simple interrupted suture, change orientation, two-bite and single-bite technique, forehand and backhand mechanics |
| Suturing 4 | Other Interrupted Sutures | How to perform vertical and horizontal mattress, figure of 8, buried knot |
| Suturing 5 | Running Suture | How to perform running suture, spacing, tension, change orientation, two-bite and single-bite technique, forehand and backhand mechanics |
The program used a series of relatively short videos which taught individual skills in a progressive manner. The videos were released sequentially, with students being given access to two videos every two weeks. Students were required to watch the videos and submit practice material before access to the next set of videos was provided. This design encouraged students to master the material before progressing.
Computer-based video course
In September 2016, we began a new semester-long, elective course at Case Western Reserve University School of Medicine in Cleveland, Ohio for preclinical medical students entitled “Self-Directed Surgical Skills”. The goals of the elective were: 1) To teach basic knot-tying and suturing skills using CBVT and self-directed practice and 2) to familiarize students with basic surgical instruments and sutures.
Preclinical medical students voluntarily enrolled in the elective. They were given access to an internal online platform, where videos were released two at a time every two weeks. Students provided practice samples to demonstrate that they had watched the video and practiced in order to gain access to the next set of videos. These samples were not graded.
Materials
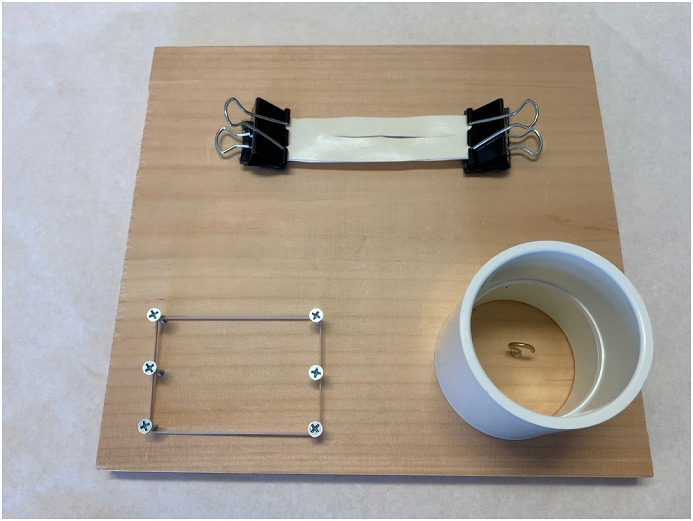
Students were given a homemade practice skills board (Fig. 1 ). Silk ligatures (0, 2-0, 3-0, 4-0) and silk sutures (2-0 and 4-0) were provided as a courtesy by Covidien (Minneapolis, MN). Students were further provided braided clothes line, a bag of #33 rubber bands (Office Depot), and Microfoam Surgical Tape (3 M, Minneapolis, MN). We found that a double layer of Microfoam tape formed by opposing the adherent sides acted as a suitable skin substitute. Students purchased the recommended 7-inch DeBakey type forceps and 7-inch Mayo Hegar needle driver.
Fig. 1.
Sample practice board measures 10 × 10 inches. It is equipped with a 5/8-inch cup hook screw (lower right) on which to tie free suture knots. A removable segment of PVC pipe (2 ½ inch inner diameter x 3-inch long) can be used to practice tying knots into depth. A rubber band can be placed around the 6 screws (lower left) at varying tension to practice tying knots on tension. The 2 columns of screws are located 3 inches apart and each row of screws is 1 inch apart. Binder clips are attached to the board to secure material to be sutured.
Study participation
Students who enrolled in the elective were asked to participate in this study which measured the effectiveness of training. Students consented to be evaluated pre and post course with a written exam and a practical skills exam. Videos were uploaded to an internal online platform (Echo360, Reston, VA) which allowed monitoring of individual student usage. After each video, students completed a survey rating the content and instruction quality on a Likert scale (1–5). They also reported their estimated number of hours practiced per video. At the end of the course, each student completed a post-elective evaluation reporting their Likert rating (scale 1–5) of the course and provided open-ended feedback. Study participation was not mandatory although every student agreed to participate. Students who did not complete the elective were not included in the study. The study was performed under a Case Western Reserve University Institutional Review Board-exempted protocol.
Student assessment
Students were assessed before and after completing the course with a Likert scale (1–5) self-rating of their ability to perform each of the knot-tying and suturing skills demonstrated during the course (listed in Table 2 ), a 10-question multiple-choice exam testing knowledge of surgical instruments, materials and techniques, and a practical skill exam.
Table 2.
Skills Taught: Pre- and Post-Elective: Average Self Rating of Ability (scale 1–5) expressed as mean ± SD.
| Self-ratings of ability (scale 1–5) | Pre | Post | P value |
|---|---|---|---|
| Two-handed knot | 1.70 ± .88 | 4.34 ± .72 | p < 0.01∗ |
| One-handed knot | 1.37 ± .71 | 4.21 ± .80 | p < 0.01∗ |
| Tying against tension | 1.19 ± .54 | 3.81 ± .85 | p < 0.01∗ |
| Tying into deep space | 1.11 ± .38 | 3.29 ± 1.1 | p < 0.01∗ |
| Instrument tie | 1.47 ± .90 | 4.07 ± .90 | p < 0.01∗ |
| Simple interrupted suture | 1.67 ± 1.0 | 4.26 ± .77 | p < 0.01∗ |
| Vertical mattress | 1.31 ± .62 | 3.79 ± .86 | p < 0.01∗ |
| Horizontal mattress | 1.25 ± .58 | 3.77 ± .87 | p < 0.01∗ |
| Figure of 8 | 1.13 ± .41 | 3.70 ± .94 | p < 0.01∗ |
| Buried knot | 1.17 ± .42 | 3.44 ± 1.0 | p < 0.01∗ |
| Running suture | 1.51 ± .89 | 4.00 ± .83 | p < 0.01∗ |
Practical skill exam
Students were assessed with a pre- and post-course practical skill exam for six selected knot-tying and suturing skills (using 4-0 silk) as follows:
-
1)
tying two-handed knots on flat surface
-
2)
tying one-handed knots on flat surface
-
3)
tying against tension with a #33 rubber band placed on the most distant screw pegs creating a 2x3-inch rectangle
-
4)
tying into depth by forming knots on the board’s cup hook inside of a piece of 2 ½ inch inner diameter, 3-inch segment of PVC pipe
-
5)
simple interrupted suture of doubled Microfoam tape
-
6)
running suture of doubled Microfoam tape
The practical skill exams yielded three measured scores:
Global Rating Scale
The skill exams were videotaped and graded in a blinded fashion by a single reviewer (ED). We assessed knot tying and suturing technique using a modified assessment tool based upon the ACS/APDS Surgery Resident Skills Curriculum Global Rating Scale (GRS).18 The GRS measures economy of movement, dexterity of hand movements, and coordination. Students received a grade from 0 to 5 for each skill.
Speed
Speed was measured from the videos or in real time. During the practical skill exam students were given 1 min to tie knots and 2 min to place sutures. Speed is reported in knots tied per minute or sutures placed in 2 min.
Product quality score
A Product Quality Score (PQS) was generated by assessing de-identified knot and suture products from the practical skill exam. Samples were graded by a single reviewer (NK). The PQS was rated on a scale of 0–5 as follows:
| 0 = Unable to attempt |
| 1 = Attempted but not appropriately executed |
| 2 = Executed to an unsatisfactory degree |
| 3 = Executed to a satisfactory degree |
| 4 = Executed to an above average degree |
| 5 = Executed to an expert degree |
Statistical analysis
Data is expressed as mean ± standard deviation (SD). Statistical significance was defined as P < 0.05. Data was analyzed using paired t-tests and ANOVA. Statistical analyses were performed using Microsoft Excel and JMP Pro statistical software (version 14; SAS Institute, Cary, NC).
Results
There were 227 students who enrolled in the course, six of whom did not complete it. Thus, 221 students were included in the study which collected data over 6 semesters between September 1, 2016 and April 30, 2019. Student average age was 24.0 ± 2.3 years. 110 students were female, 107 were male, and 4 did not declare. There were 121 first-year medical students, 97 s-year medical students, and 3 were other. The majority of students who participated had a surgical career interest; pre-course average student Likert scale self-rating (scale 1–5) of a desire pursuing surgical training was 3.9 ± 1.1.
Curriculum evaluation
Students watched each video an average of 2.6 ± 0.3 times and reported practicing the skills from each video an average of 1.2 ± 1.3 h (Table 3 ). On average, students rated each video a Likert scale rating of 4.2 ± 1.0 on the basis of educational quality and effectiveness. Students found each video in the curriculum to be an effective learning tool and spent similar amounts of time watching and practicing material from each video.
Table 3.
Individual video usage, self-reported estimates of practice time, and video rating (scale 1–5) expressed as mean ± SD.
| Video | # times viewed | Self-reported estimated hours practiced | Video rating Scale 1-5 |
|---|---|---|---|
| Knot tie 1 | 3.3 ± 1.8 | 1.1 ± 0.9 | 4.50 ± .62 |
| Knot tie 2 | 3.0 ± 1.7 | 1.3 ± 2.5 | 4.46 ± .65 |
| Knot tie 3 | 3.0 ± 2.1 | 1.3 ± 0.9 | 4.30 ± .87 |
| Knot tie 4 | 2.2 ± 1.5 | 1.0 ± 1.0 | 4.04 ± 1.0 |
| Knot tie 5 | 3.2 ± 1.6 | 1.3 ± 0.9 | 4.41 ± .74 |
| Knot tie 6 | 2.5 ± 1.5 | 1.4 ± 2.7 | 4.26 ± .84 |
| Knot tie 7 | 1.9 ± 1.0 | 1.40 ± 2.8 | 3.95 ± 1.1 |
| Suture 1 | 2.1 ± 1.2 | 0.96 ± 1.6 | 3.69 ± 1.3 |
| Suture 2 | 2.1 ± 1.2 | 1.1 ± 1.0 | 3.95 ± .95 |
| Suture 3 | 3.0 ± 1.6 | 1.4 ± 1.3 | 3.85 ± 1.1 |
| Suture 4 | 2.7 ± 1.3 | 1.8 ± 2.7 | 4.26 ± .87 |
| Suture 5 | 2.2 ± 1.1 | 1.61 ± 2.2 | 4.32 ± .77 |
Students rated the elective on average 4.3 ± 0.7 for being “well-organized”, 4.4 ± 0.7 for being “a valuable use of their time”, and 4.6 ± 0.7 for providing resources that they will look at again. The majority of students (98%) reported that they would recommend this course to other medical students interested in a surgical career.
Student self-ratings
Students significantly improved based on their own ratings of their ability to execute each of 11 specific skills (Table 2). Average self-ratings (scale 1–5) increased from an average of 1.4 ± 0.7 pre-elective to 3.9 ± 0.9 post-elective across all skills (P < 0.01).
Student performance
Students’ scores on the 10-question multiple-choice exam testing knowledge of surgical instruments, materials and techniques significantly improved from a pre-elective average of 54% to a post-elective average of 87% (P < 0.01). Only two students (0.9%) did not achieve at least a passing score of 70% on the post-elective multiple-choice exam. Completing the course increased students’ basic knowledge of identifying instruments and proper technique to perform certain skills.
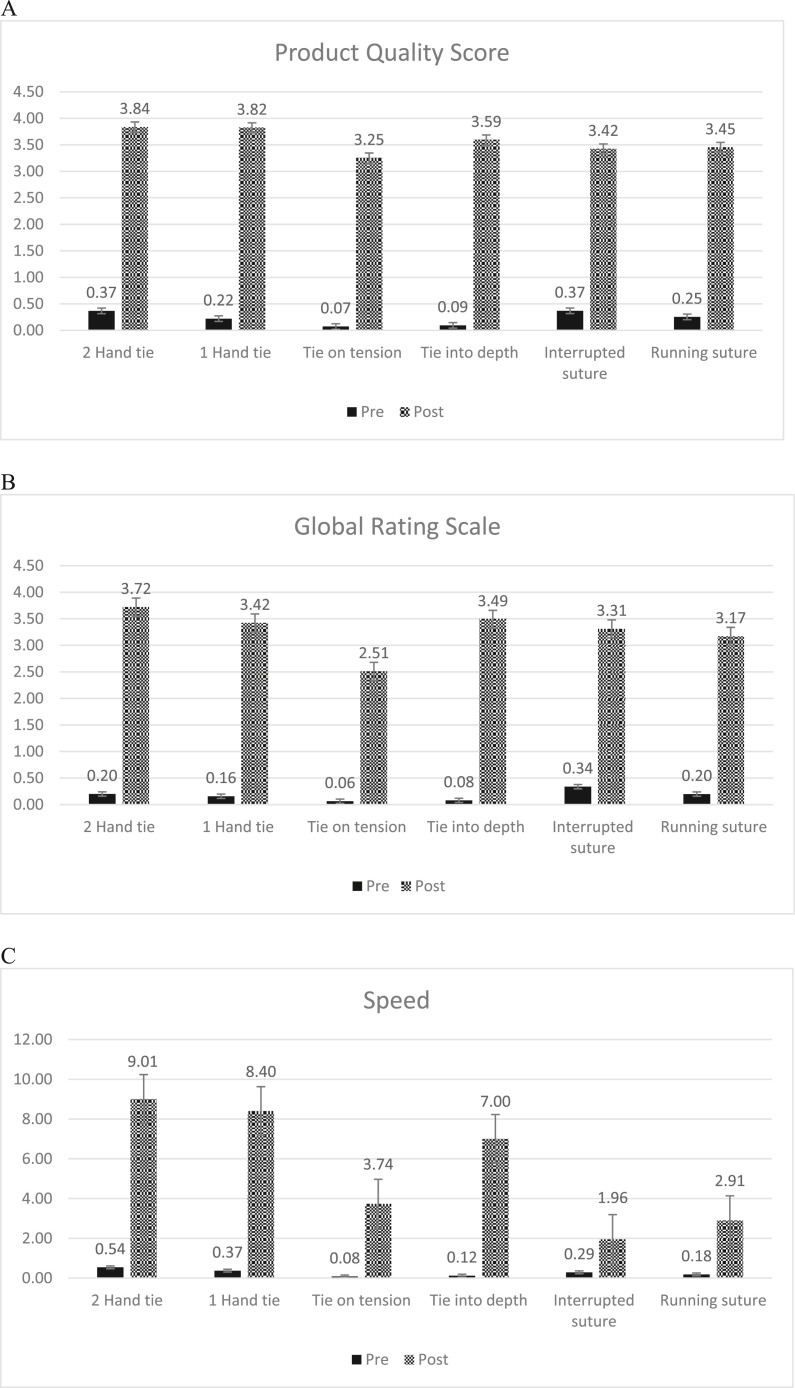
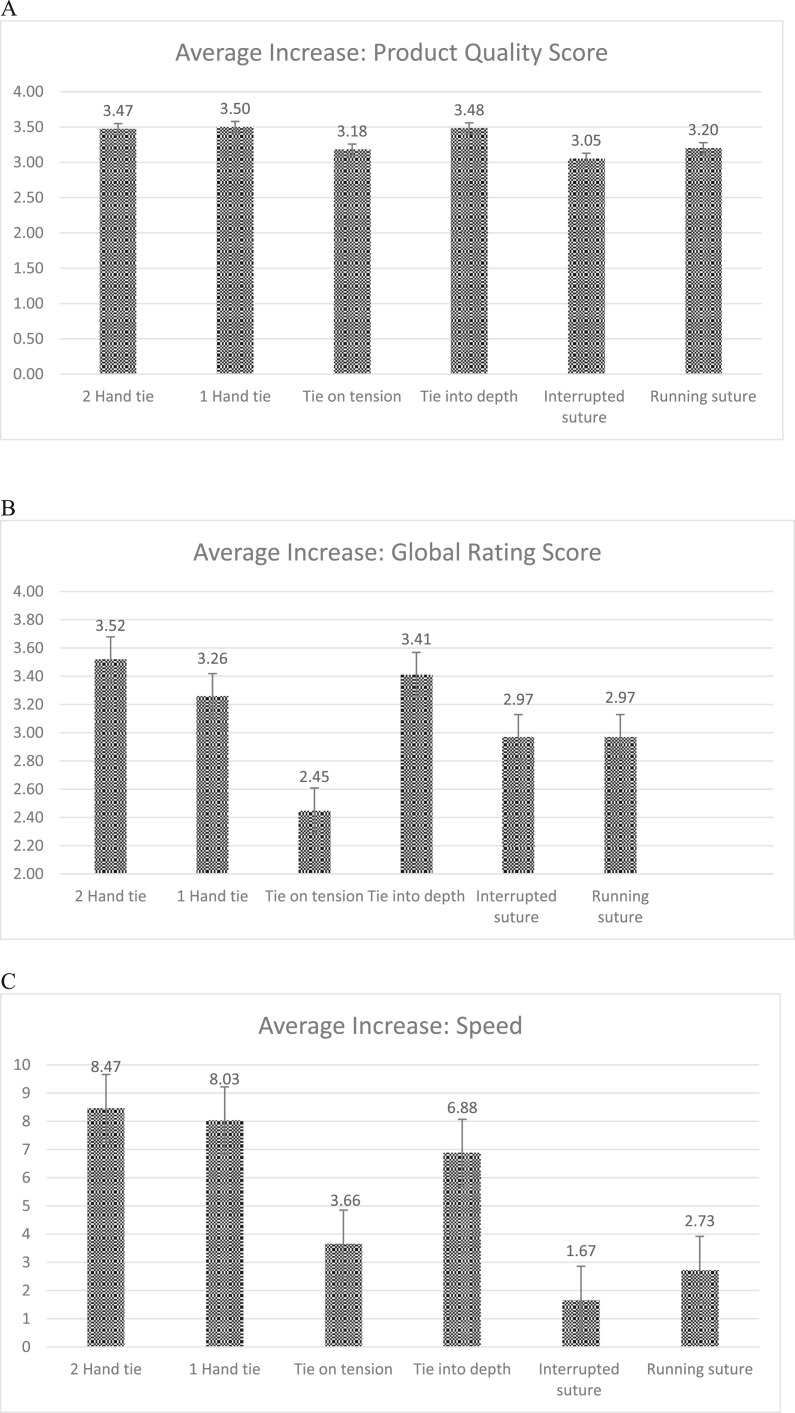
Every student who completed the course demonstrated a significant increase in their Product Quality Score (PQS), technique as measured by the Global Rating Scale (GRS), and speed for each of 6 skills assessed. The increase from pre-to post-course is significant for all 6 skills assessed by each of the three measures, P < 0.01 (Fig. 2 ). We similarly assessed the pre-course to post-course change for PQS, GRS and speed score for each student for each of the 6 skills. Average score increase across all 3 measures for all 6 skills are shown in Fig. 3 . Average pre-course PQS and GRS were <0.4 for all 6 measures and increased post-course to an average ≥ 3.25 except for the skill tying on tension GRS which increased only to 2.51.
Fig. 2.
Average scores pre- and post-course for each of the six skills assessed by the Practical Skills Exam. A) The observed quality of the knots and sutures as assessed with the Product Quality Scores. B) Technique as rated by a Global Rating Scale. C) Speed as measured in knots per minute or sutures placed in 2 min. The increase from pre-to post-course is significant for all 6 skills assessed by each of the three measures (P < 0.01).
Fig. 3.
Average increases in scores from pre-to post-course for each of the six skills assessed by the Practical Skills Exam. A) The observed quality of the knots and sutures as assessed with the Product Quality Scores. B) Technique as rated by a Global Rating Scale. C) Speed as measured in knots per minute or sutures placed in 2 min.
Our data suggested that the most difficult skill to master was tying against tension (Fig. 3). Despite a significant increase from pre-course scores, we found a lower average increase in PQS (P = 0.027), GRS (P < 0.0010) and speed (P < 0.001) for the tying on tension skill compared to the other knot tying skills, which were not significantly different from each other. Both suturing skills showed similar average increases in PQS (P = 0.18) and GRS (P < 0.72). As expected, running suture was faster than interrupted, yielding a higher increased speed (P < 0.001).
Discussion
Using a traditional apprenticeship model to teach procedural skills has numerous drawbacks. It requires one-on-one or small group instruction. This training often takes place in the operating room which places the learner under pressure to execute skills quickly and without error. In addition, limits on resident work hours and the introduction of shorter residency training paradigms have left residents with less time to acquire an increasingly complex set of skills.2 , 3 It is, therefore, advantageous for medical students and junior trainees to learn basic skills outside the operating room in order to maximize their operative experience.
A variety of courses, skill labs, “boot camps” and other curricula have been proposed, introduced, or studied to teach basic skills to senior medical students or junior residents.10, 11, 12 , 19 , 20 Numerous national organizations have stressed the importance of early training of medical students and junior residents including the American Association of Medical Colleges, American College of Surgeons, Association of Program Directors in Surgery, Association for Surgical Education, and Accreditation Council for Graduate Medical Education.10 , 21 , 22 Implementation of these initiatives has been variable, potentially due to their requirement of an available skill lab, establishing the program curricula, need for experienced faculty for training and the time and expense to initiate and maintain the program. These training sessions take both the faculty and the trainee away from their typical daily responsibilities. It is our assertion that basic surgical skills may be better learned and practiced by the trainee on their own time and at their own pace.
A number of reports support the notion that computer-based video training can be effective in teaching procedural skills.4, 5, 6, 7, 8, 9 Many of these reports are of limited nature, being largely narrow in scope, limited in the number of individuals trained, and in some cases were studies to demonstrate feasibility.4, 5, 6, 7, 8, 9 Many also required a significant skill lab component to conduct training.10, 11, 12, 13
When designing our CBVT course, our goal was to create a program that 1) could train large numbers of students, 2) required little to no direct faculty involvement, 3) had no required skills lab or one-on-one instruction, 4) offered training that could take place anytime or any place the student found convenient, and 5) allow the student to progress and practice without pressure at their own pace.
This study reports the results from the first six semesters of our Self-Directed Surgical Skills elective. We demonstrate that this video-based curriculum can be effective in teaching basic surgical skills of knot tying and suturing to novice preclinical medical students. Students who completed the course became reasonably proficient in executing these basic skills and demonstrated significant improvement in speed, technique and product quality. Moreover, students’ self-assessment of their ability correlated fairly well with their observed execution, suggesting that students can self-monitor their performance and know when they have succeeded.
We believe this CBVT course was successful for several reasons. First, the skills to be learned were broken down into their simplest elements. The program taught simple hand movements one at a time in a progressive manner. Second, the videos were released sequentially, over time. Students were required to learn, absorb and practice the material before progressing. Third, they were required to demonstrate that they had watched the videos and had practiced before they would be given access to a new set of videos. Fourth, each video reinforced what was learned in previous videos to build upon skills already learned. We believe that this repetition in training was valuable.
The development of such a training program may be especially timely given the current COVID-19 pandemic. Shortages of personal protective equipment, the cancellation of elective procedures, and the need to socially distance has curtailed many third- and fourth-year medical student rotations and limited the ability to train surgical housestaff.15 , 16 This has left medical educators at a loss in their ability to educate these individuals.15 , 16 This remote, self-directed learning curriculum could fill part of the void if hospital-based training becomes unsafe or impractical. In this ever-changing landscape, medical education will need to adapt to pressures that may restrict in person instruction. This self-directed CBVT model may be able to be modified or expanded to teach other skills or more complex skills.
Limitations and future directions
In assessing student performance, some of the measured parameters are subjective. Other observers might interpret their execution differently. We believe that the stepwise introduction of material improved the students’ mastery, but this was not directly tested against other paradigms. The long-term effects of this training program are unknown. Students were assessed immediately upon course completion. We don’t know if they are able to retain these skills. These skills are all performed on a table top model. It is unclear if students can perform similarly in a clinical setting. It is furthermore unclear if the sequential release of the videos over time helped the students absorb the material. Based on the results from this study we believe this model could be effective in teaching these skills to a wider audience. We plan on re-formatting these videos for widespread dissemination. Further studies are needed on course design, its long-term benefit and clinical applicability.
Conclusions
This computer-based video training curriculum is effective in teaching basic surgical skills to novice medical students by introducing different knot-tying and suturing techniques in a stepwise progression. Students significantly improved their surgical familiarity, knowledge, and proficiency. We believe that this model can be modified or expanded to teach other, more complex skills. Remote, computer-based training may be a beneficial addition to medical education.
Funding
Supported by the 2016 Case Western Reserve University, School of Medicine Interprofessional Scholars Collaboration in Teaching and Learning (iSCTL) Program Fund which had no role in directing the current study.
Declaration of competing interest
None of the authors have any relevant disclosures or conflicts of interest.
Acknowledgments
We would like to acknowledge the Mt. Sinai Skills and Simulation Center for their assistance in filming the videos and Covidien (Minneapolis, MN) for supplying the silk ligatures and sutures.
References
- 1.Kulaylat A.N., McKinley S.K., Kenning E.M., et al. Surgical education and training at the crossroads between medical school and residency. Bull Am Coll Surg. 2014;99:24–29. http://www.ncbi.nlm.nih.gov/pubmed/25145044 [PubMed] [Google Scholar]
- 2.Sofka C.M. Developments and innovations in resident and fellowship education. HHS J. 2014;10:225–229. doi: 10.1007/s11420-014-9396-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahmed N., Devitt K.S., Itay K., et al. A systematic review of the effects of resident duty hour restrictions in surgery. Ann Surg. 2014;259:1041–1053. doi: 10.1097/SLA0000000000000595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xeroulis G.J., Park J., Moulton C.A., et al. Teaching suturing and knot-tying skills to medical students: a randomized controlled study comparing computer-based video instruction and (concurrent and summary) expert feedback. Surgery. 2007;141:442–449. doi: 10.1016/j.surg.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 5.Jowett N., LeBlanc V., Xeroulis G., et al. Surgical skill acquisition with self-directed practice using computer-based video training. Am J Surg. 2007;193:237–242. doi: 10.1016/j.amjsurg.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 6.Nousiainen M., Brydges R., Backstein D., et al. Comparison of expert instruction and computer-based video training in teaching fundamental surgical skills to medical students. Surgery. 2008;143:539–544. doi: 10.1016/j.surg.2007.10.022. [DOI] [PubMed] [Google Scholar]
- 7.Vaughn C.J., Kim E., O’Sullivan P., et al. Peer video review and feedback improve performance in basic surgical skills. Am J Surg. 2016;211:355–360. doi: 10.1016/j.amjsurg.2015.08.034. [DOI] [PubMed] [Google Scholar]
- 8.Rogers D.A., Regehr G., Howdieshell T.R., et al. The impact of external feedback on computer-assisted learning for surgical technical skill training. Am J Surg. 2000;179:341–343. doi: 10.1016/S0002-9610(00)00341-x. [DOI] [PubMed] [Google Scholar]
- 9.Wright A.S., McKenzie J., Tsigonis A., et al. A structured self-directed basic skills curriculum results in improved technical performance in the absence of expert faculty teaching. Surgery. 2012;151:808–814. doi: 10.1016/j.surg.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 10.Klingensmith M.E., Brunt L.M. Focused surgical skills training for senior medical students and interns. Surg Clin. 2010;90:505–518. doi: 10.1016/j.suc.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Wade T.J., Lorbeer K., Awad M.M., et al. Outcomes of a proficiency-based skills curriculum at the beginning of the fourth year for senior medical students entering surgery. Surgery. 2015;158:962–971. doi: 10.1016/j.surg.2015.07.00. [DOI] [PubMed] [Google Scholar]
- 12.Naylor R.A., Hollett L.A., Castellvi A., et al. Preparing medical students to enter surgery residencies. Am J Surg. 2010;199:105–109. doi: 10.1016/j.amjsurg.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Huang E., Chern H., O’Sullivan P., et al. A better way to teach knot tying: a randomized controlled trial comparing the kinesthetic and traditional methods. Am J Surg. 2014;208:690–694. doi: 10.1016/j.amjsurg.2014.05.028. [DOI] [PubMed] [Google Scholar]
- 14.Jensen A.R., Wright A.S., Levy A.E., et al. Acquiring basic surgical skills: is a faculty mentor really needed? Am J Surg. 2009;197:82–88. doi: 10.1016/j.amjsurg.2008.06.039. [DOI] [PubMed] [Google Scholar]
- 15.Rose S. Medical student education n the time of COVID-19. J Am Med Assoc. 2020;323:2131–2132. doi: 10.1001/jama.2020.5227. [DOI] [PubMed] [Google Scholar]
- 16.+Mousa A. The impact of COVID-19 on vascular training. J Vasc Surg. 2020;72:380–381. doi: 10.1016/j.jvs.2020.04.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Skochelak S.E., Stack S.J. Creating the medical schools of the future. Acad Med. 2017;92:16–19. doi: 10.1097/ACM.0000000000001160. [DOI] [PubMed] [Google Scholar]
- 18.American College of Surgeons/Association of Program Directors in Surgery. Resident Skills Curriculum; Global Rating Scale: 2016. [Google Scholar]
- 19.Fernandez G.L., Page D.W., Coe N.P., et al. Boot cAMP: educational outcomes after 4 successive years of preparatory simulation-based training at onset of internship. J Surg Educ. 2012;69:242–248. doi: 10.1016/jsurg.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 20.Mittal M.K., Dumon K.R., Edelson P.K. Successful implementation of the American College of surgeons/association of program Directors in surgery surgical skills curriculum via a 4-week consecutive simulation rotation. Simulat Healthc J Soc Med Simulat. 2012;7:147–154. doi: 10.1097/SIH.0b013e31824120c6. [DOI] [PubMed] [Google Scholar]
- 21.American Board of Surgery, American College of Surgeons, Association of Program Directors in Surgery Association for Surgical Education. Statement on surgical preresidency preparatory courses. J Surg Educ. 2014;71:777–778. doi: 10.1016/j.jsurg.2014.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Accreditation Council for Graduate Medical Education (ACGME) Program requirements for graduate medical education in general surgery. ACGME. 2014 [Google Scholar]