Abstract
Located in the uterine cervix, cervical invasive stratified mucin-producing carcinoma (i-SMILE) is a rare, recently-identified tumor about which little is known. In extremely rare cases, other kinds of invasive carcinoma can accompany i-SMILE, such as squamous cell carcinoma (SCC) and adenocarcinoma, with different proportions. Here, we report a case of cervical carcinoma coexisting with i-SMILE, mucinous carcinoma, non-specific type (NOS), and SCC. We review the pathological diagnosis and describe the clinical pathological characteristics.
Keywords: Invasive stratified mucin-producing carcinoma, histopathology, immunophenotype
Introduction
Invasive stratified mucin-producing carcinoma (i-SMILE) was first described in 2015 by Lastra [1] and was named in 2016. Its precursor, stratified mucin-producing intraepithelial lesion (SMILE), was included in the 2014 WHO Classification of Tumours of Female Reproductive Organs [2]. i-SMILE is a rare type of cervical invasive adenocarcinoma [3]. We found a limited number of cases in the medical literature after searching PubMed and China National Knowledge Infrastructure, and most of the articles we retrieved were case reports or studies with small sample sizes. Given the paucity of understanding and the recent identification of the disease, i-SMILE can easily be misdiagnosed by pathologists and gynecologists, and even under-recognized [4]. As part of their daily work, pathologists are asked to pay attention to new tumors. Nonetheless, the biological behavior and molecular genetics of i-SMILE remain unclear and require more research. Here, we report several cases of uterine cervical carcinoma, that is, the coexistence of i-SMILE, mucinous carcinoma, NOS, and squamous cell carcinoma (SCC). We review the pathological diagnosis and describe the clinical pathological characteristics. We carried out immunophenotyping to provide detailed information about i-SMILE.
Case report
On 8 January 2020, a 49-year-old female, gravid 5, para 2, came to our hospital complaining of contact bleeding for three months. Eight months earlier, the pap smear from her routine physical examination at a local hospital showed atypical squamous cells (ASCUS). A colposcopic exam and a cervical biopsy reported chronic cervicitis with inflammatory polyps and atypical glands. An HPV-DNA test showed she was positive for genotype HPV-18. The patient received no treatment prior to visiting our hospital.
The patient underwent an outpatient gynecological procedure, and the gynecological examination revealed cervical hypertrophy, smooth and easy bleeding, mild cervical erosion, but no pain. B ultrasonography was advised and completed later. The results indicated several non-echo areas located in the uterine cervix, which suggested Nessler cysts in the cervix and adenomyosis in the uterus body. The hysteroscopy findings suggested no clear lesion in the uterine cavity or the endocervix, but richness in blood vessels in the endocervix and the posterior wall of the uterus. Fractional curettage was done, followed by hysteroscopy. Histologically, the secretory phase endometrium and endocervical glands were present, a part of which was moderately-severe atypical.
Conization was performed. Macroscopically, the cervix of the uterus showed partial hyperemia with a smooth surface and papillary hyperplasia in the endocervical canal (Figure 1). Histologically, high-grade squamous intraepithelial lesions (CIN III) were seen on the surface with overlying koilocytosis. The full thickness of the squamous epithelia showed immaturity, irregular polarity, and numerous mitoses. One part also showed infiltration of the stroma by SCCs. SMILE was noted as well, composed of stratified epithelia containing mucin in the form of discrete vacuoles or as cytoplasmic clearing throughout all the cell layers. HE staining showed atypical nuclear changes, concentrated nuclei, karyokinesis, and apoptotic bodies. Part of the tumor exhibited infiltrative sheets and nests of cells with mucinous differentiation and peripheral palisading structures. Other parts of the tumor exhibited invasive mucinous adenocarcinoma, which was definite proof of the mucinous differentiation, but without specific characteristics of signet-ring-cells, both the intestinal and gastric types. An immunohistochemical assay showed that the SMILE and i-SMILE tumor cells were positive for P16, CEA, CK, and CK7, weakly positive for PAX-8, but negative for CK5/6, CK7, ER, PR, PTEN, P53, vimentin, CD10, and GATA3. The SCCs tumor cells were partly positive for P40, and the Ki-67 proliferation index was 60% (Figure 2).
Figure 1.
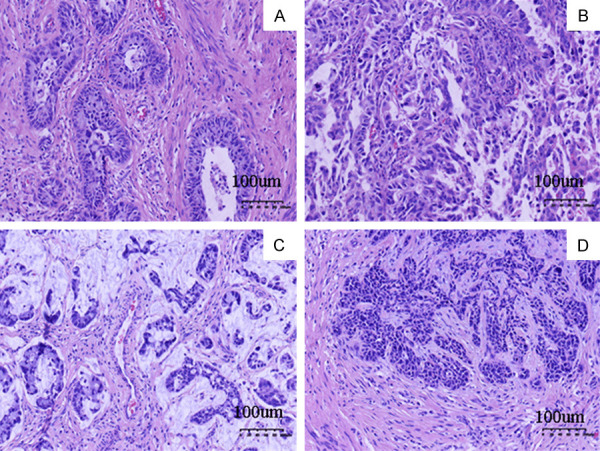
HE staining results. A. Stratified mucin-producing intraepithelial lesion (SMILE); B. Invasive stratified mucin-producing carcinoma; C. Mucinous carcinoma, NOS; D. Squamous cell carcinomas.
Figure 2.
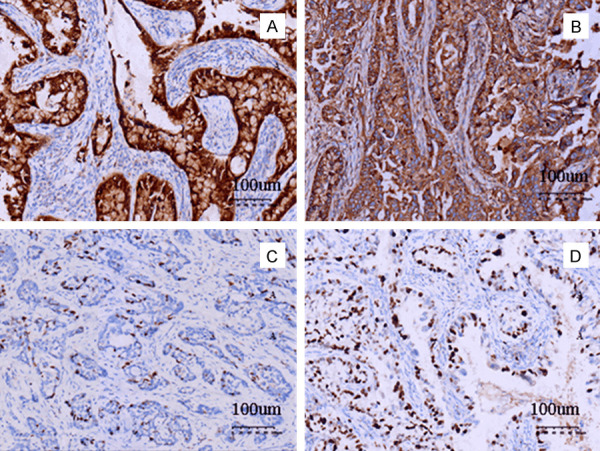
Immunohistochemical staining results. A. The tumor cells of i-SMILE were positive for P16; B. The tumor cells of i-SMILE were positive for CEA; C. The tumor cells of SCC were positive for P40; D. Proliferation index of Ki-67 for the tumor cells.
Based on these results, the patient was diagnosed with coexisting i-SMILE, mucinous carcinoma, NOS, and SCC of the uterine cervix. A total hysterectomy with double appendages and pelvic lymphadenectomy were done immediately after the diagnosis. The tumor was infiltrating into a third of the cervical wall, but no metastatic lymph nodes were found.
Post-operation, the patient had a favorable recovery without complications. After the operation, the patient had no significant abnormalities during the follow-up consultations to date.
Discussion
i-SMILE is recently reported and classified as a distinctive variant of cervical adenocarcinoma. A clinical epidemiological study with a large cohort has not been carried out because of its scarcity. Therefore, we reported an interesting case of i-SMILE, that is, the coexistence of i-SMILE, mucinous carcinoma, NOS, and SCC. We analyzed the pathological diagnosis and the clinical pathological characteristics.
SMILE is believed to be the precancerous lesion of i-SMILE because of their similar origin: embryonic cells located in the transformation zone of the squamous and glandular epithelia [5]. The occurrence of i-SMILE is related to carcinogenesis which is associated with high-risk HPV [6]. Similar to adenocarcinoma, NOS and villoglandular carcinoma, i-SMILE is HPV-associated adenocarcinoma, so a diffused positivity of tumor cells for P16 was observed. That persistent HPV infection is an important cause of cervical cancers is generally known, and i-SMILE is no exception. Of the 40 HPV types, 14 are considered high-risk viruses. Presently, whether high-risk HPV contributes to the development of i-SMILE is unclear because of the limited number of clinical specimens [7].
The clinical features of i-SMILE are unclear. The mean age of presentation is in the fourth decade, ranging from 29 to 66 years old [8]. Abnormal uterine bleeding and mass lesions are present in approximately 80% of cases. The mean age of SMILE patients is 31 years old, 10 years before invasive lesions, and ranging in age from 20 to 58 years old.
Macroscopically, the mean size of an i-SMILE lesion is roughly 4 cm, but the lesions range from 1.2 to 6.4 cm [9]. Exophytic growth patterns are often found, such as papillary or polypoid patterns. A smaller percentage shows surface ulceration. The cut surface of this tumor has a soft, white to tan appearance with foci of hemorrhages and necrosis.
Histopathologically, it is different from HSIL, which sometimes shows focal mucin production, and the mucin globules are clearly visible in the full thickness of the epithelium in SMILE, and they do not even need mucin-specific special stains. The histological structure of SMILE is the same as that of adenocarcinoma in situ (AIS) located in the cervix, such as a glandular configuration. However, important differences are noted: in the apical part of the tumor cells, mucin globules are noticeable. In the case of SMILE, the tumor consists of stratified epithelia with cells containing mucin in the form of discrete vacuoles or as cytoplasmic clearing throughout all cell layers. Nuclear atypia, hyperchromasia, mitoses, and apoptotic bodies are usually present [10,11]. i-SMILE shows both squamous and glandular features. Like in the case of SMILE, i-SMILE reveals stratified, intracytoplasmic mucin (from ‘mucin-rich’ to ‘mucin-poor’) and immature nuclei. Most carcinomas infiltrate as small solid nests without an obvious glandular cavity or keratinization. The tumor cells are well- to moderately differentiated and composed of ovoid and round-shaped cells with peripheral palisading. The mucinous cells are disseminated in the tumor nests in varying amounts. In the background, the infiltration levels of the neutrophil and fibrous tissue vary [12]. i-SMILE often occurs with HSIL and/or AIS which can better explain HPV infection, but sometimes it may appear as an isolated finding. In 75% of i-SMILE cases, i-SMILE coexists with invasive SCC, adenocarcinoma, NOS, mucinous carcinoma, and other kinds of cervical carcinoma. HSIL is the more commonly concomitant lesion (approximately 93% of cases) compared with AIS (nearly 42%) [7]. Neuroendocrine carcinoma is concomitant with cervical adenomatous carcinoma except with i-SMILE and indicates a poor prognosis.
An overlap between i-SMILE and adenosquamous carcinoma is observed in the morphology and immunophenotype. Many i-SMILE cases were misdiagnosed in the past as adenosquamous carcinoma. According to the diagnostic criteria of WHO (2014), adenosquamous carcinoma is a malignant epithelial tumor comprising adenocarcinoma and SCC. Differentiation between adenocarcinomatous and squamous cell carcinoma components should be sufficient (>10%). Recognizable evidence should also be seen, such as intercellular bridges and keratinization. Tumor cells of adenosquamous carcinoma are positive for adenocarcinoma and SCC markers, but negative or locally positive for SCC markers in i-SMILE. In our case, an immunohistochemical study showed that the tumor cells of i-SMILE and SMILE were positive for P16, CEA, CK, and CK7 but negative for CK5/6 and P40. The tumor cells of SCCs were partly positive for P40. We believe that the criteria for adenosquamous carcinoma were not met, and the diagnosis of the coexistence of i-SMILE and SCC was more persuasive. Beyond adenosquamous carcinoma, the typical misdiagnoses include adenoid cystic carcinoma, basaloid squamous carcinoma, and mucoepidermoid carcinoma.
i-SMILE is virtually always associated with HPV. Unsurprisingly, immunohistochemical staining showed that tumor cells strongly expressed P16 in our case. The immunophenotype of the tumor cells were similar to that of glandular epithelia and were found positive for CAM5.2, CK7, CK18, and CA125, weakly positive for ER and PR, and negative for CK5/6 and P63. Generally, the Ki-67 proliferation index is high. Onishi supposed that IMP3 is positive in adenocarcinoma in situ but negative in normal glandular epithelia, which prompts the occurrence of adenocarcinoma in situ [7].
The factors influencing the prognosis of i-SMILE include lymph node metastases, tumor size and local extension, similar to other kinds of cervical neoplasia. The clinical stage is an essential reference for patient prognosis and treatment. The five-year survival rates vary across patients in different clinical stages: 99% for stage IA1, 65% for IIB, and 43% for IIIB. HPV-positive cervical adenocarcinoma has a better survival rate [13]. Relative to other kinds of HPVA, i-SMILE has a poorer outcome and is more aggressive. The average time interval between SMILE to i-SMILE is roughly 15 years, which is identical to the disease timeline of AIS to invasive adenocarcinoma (10-15 years). The time interval mirrors the step-by-step procedure of SMILE to i-SMILE, matching the progression of other kinds of HR-HPV-associated carcinoma.
Conclusion
We presented an interesting and rare case of i-SMILE and analyzed its pathogenesis, features, and prognosis. We hope to increase the awareness of this enigmatic tumor and avoid diagnostic pitfalls.
Acknowledgements
We are grateful to the patient for her cooperation with this study.
Disclosure of conflict of interest
None.
References
- 1.Lastra RR, Park KJ, Schoolmeester JK. Invasive stratified mucin-producing carcinoma and stratified mucin-producing intraepithelial lesion (SMILE): 15 cases presenting a spectrum of cervical neoplasia with description of a distinctive variant of invasive adenocarcinoma. Am J Surg Pathol. 2016;40:262–269. doi: 10.1097/PAS.0000000000000543. [DOI] [PubMed] [Google Scholar]
- 2.Lax SF, Horn LC, Löning T. Categorization of uterine cervix tumors: what’s new in the 2014 WHO classification. Pathologe. 2016;37:573–584. doi: 10.1007/s00292-016-0247-8. [DOI] [PubMed] [Google Scholar]
- 3.Xu H, Wang YM, Zhang J. Clinicopathological features of stratified mucin-producing neoplastic lesions of the cervix. Zhonghua Bing Li Xue Za Zhi. 2020;49:28–33. doi: 10.3760/cma.j.issn.0529-5807.2020.01.006. [DOI] [PubMed] [Google Scholar]
- 4.Backhouse A, Stewart CJ, Koay MH, Hunter A, Tran H, Farrell L, Ruba S. Cytologic findings in stratified mucin-producing intraepithelial lesion of the cervix: a report of 34 cases. Diagn Cytopathol. 2016;44:20–25. doi: 10.1002/dc.23381. [DOI] [PubMed] [Google Scholar]
- 5.Horn L, Handzel R, Borte G, Siebolts U, Haak A, Brambs CE. Invasive stratified mucin-producing carcinoma (i-SMILE) of the uterine cervix: report of a case series and review of the literature indicating poor prognostic subtype of cervical adenocarcinoma. J Cancer Res Clin Oncol. 2019;145:2573–2582. doi: 10.1007/s00432-019-02991-3. [DOI] [PubMed] [Google Scholar]
- 6.Lastra RR, Park KJ, Schoolmeester JK. Invasive stratified mucin-producing carcinoma (i-SMILE) of the uterine cervix: report of a case series and review of the literature indicating poor prognostic subtype of cervical adenocarcinoma. Am J Surg Pathol. 2016;40:262–269. doi: 10.1097/PAS.0000000000000543. [DOI] [PubMed] [Google Scholar]
- 7.Onishi J, Sato Y, Sawaguchi A, Yamashita A, Maekawa K, Sameshima H, Asada Y. Stratified mucin-producing intraepithelial lesion with invasive carcinoma: 12 cases with immunohistochemical and ultrastructural findings. Hum Pathol. 2016;55:174–181. doi: 10.1016/j.humpath.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 8.Yorita K, Kuroda N, Naroda T, Tamura M, Ohe C, Divatia M, Amin MB, Cubilla AL, Kazakov DV, Hes O, Michal M, Michal M. Penile warty mucoepidermoid carcinoma with features of stratified mucin-producing intra-epithelial lesion and invasive stratified mucin-producing carcinoma. Histopathology. 2018;72:867–873. doi: 10.1111/his.13438. [DOI] [PubMed] [Google Scholar]
- 9.Lei RX. Invasive stratified mucin-producing carcinoma: a clinicopathological analysis of three cases. Cancer Biol Ther. 2019;20:1403–1407. doi: 10.1080/15384047.2019.1647054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hodgson A, Olkhov-Mitsel E, Howitt BE, Nucci MR, Parra-Herran C. International endocervical adenocarcinoma criteria and classification (IECC): correlation with adverse clinicopathological features and patient outcome. J Clin Pathol. 2019;72:347–353. doi: 10.1136/jclinpath-2018-205632. [DOI] [PubMed] [Google Scholar]
- 11.Boyle DP, McCluggage WG. Stratified mucin-producing intraepithelial lesion (SMILE): report of a case series with associated pathological findings. Histopathology. 2015;66:658–663. doi: 10.1111/his.12498. [DOI] [PubMed] [Google Scholar]
- 12.Goyal A, Yang B. Cytologic features of stratified mucin producing intraepithelial lesion of the cervix-a case report. Diagn Cytopathol. 2014;42:792–797. doi: 10.1002/dc.23066. [DOI] [PubMed] [Google Scholar]
- 13.Sano T, Nakamura C, Yoshida T, Oyama T. Stratified mucin-producing intraepithelial lesions (SMILEs) of the uterine cervix are associated with HPV integration. Pathol Int. 2014;64:628–630. doi: 10.1111/pin.12217. [DOI] [PubMed] [Google Scholar]


