Abstract
Background
Coronary artery disease (CAD) and lower extremity artery disease (LEAD) often coexist. Ankle brachial index (ABI) has been shown to be an independent predictor of CAD. Studies have reported correlation of CAD and LEAD on the basis of ABI and also invasive angiography. But rigorous searching did not reveal any similar research where severity of LEAD was assessed by duplex ultrasound (DUS).
In this study, we assessed the association of severity and localisation of LEAD by DUS with SYNTAX score (SS).
Results
A total of 637 subjects above 45 years of age with coronary angiographic confirmation of CAD were studied in this single centre cross-sectional, descriptive and analytical research. High SS was significantly more common in subjects with LEAD (p = 0.04). In the femoro-popliteal segment, total occlusion of arteries was found in significantly more proportion of subjects with high SS. A progressive increase in mean SS was noted across the grades of arterial disease in the femoro-popliteal segment (p = 0.007). 85.2% of the LEAD was in the femoro-popliteal segment, while below-knee arterial disease was present in 98.5% of subjects with LEAD. Hypertension, smoking, history of CVE and presentation with ACS independently increased the risk of LEAD.
Conclusion
High prevalence of asymptomatic LEAD and association of high SS with LEAD as a whole as well as femoro-popliteal involvement suggests the need for a point of care DUS study (POCUS) since treatment varies with location and extent of disease which cannot be fathomed by ABI alone. Being the largest study on association of CAD and LEAD from Indian subcontinent till date and also the first study to use non-invasive tool as DUS for LEAD assessment while studying its association with CAD makes this a landmark experience.
Background
Approximately 40% patients have coexisting coronary artery disease (CAD) and lower extremity artery disease (LEAD) and both share the similar risk factors. When one vascular region is diseased, there has been a trend in clinical practice, to look for lesions in various vascular areas [1, 2]. Moreover, coexistence of peripheral arterial disease (PAD) in a patient of CAD increases the risk of mortality [3–6]. LEAD increases with age with a prevalence of 10–25% in the general population aged > 55 years [7]. Ankle brachial index (ABI) has been shown to be an independent predictor of CAD in several studies [8]. The guidelines recommend duplex ultrasound (DUS) as the first-line imaging for LEAD lesions in combination with ABI measurement due to its high sensitivity, specificity and higher effectiveness at a lower cost per quality-adjusted life-year (QALY) compared to other imaging techniques [9, 10]. SYNTAX score (SS) for coronary angiography has become popular as it can guide the appropriate treatment protocol for revascularization and provides prognostic information [11]. Multiple studies have reported association or correlation of CAD and PAD on the basis of ABI and also invasive peripheral angiography [12–15]. But rigorous searching did not reveal any research studying the association of CAD and LEAD where severity of PAD was assessed by DUS.
In this study, our objectives were to assess the association of severity of CAD and LEAD by SS and DUS respectively and to find any relation of localisation of LEAD by DUS and severity of CAD by SS.
Methods
Subjects
This research was conducted as a single centre cross-sectional, descriptive and analytical study. Subjects who were admitted to the cardiology department of a tertiary care centre of Eastern India were recruited consecutively over a period of 15 months from 1 May 2018 to 31 July 2019. Purposive sample size was calculated to be ≥ 385 to have confidence level of 95% that the real values are within ± 5% of measured or surveyed value [https://www.calculator.net/sample-size-calculator.html]. Patients above 45 years of age with coronary angiographic confirmation of CAD were included. Exclusion criteria were creatinine clearance ≤ 30 mL/min, previous surgery or intervention for LEAD, history of percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG), past trauma, surgery in last 3 months, any malignancy, any other inflammatory condition and any anti-inflammatory drug intake apart from aspirin. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later revisions. Informed consent was obtained from all patients for being included in the study.
Clinical indices
Detailed history including age, smoking history, diabetes, hypertension, chronic kidney disease (CKD), cerebrovascular events (CVE), and claudication was taken. Claudication was defined as a pain, cramp or sense of fatigue in a muscle group of the lower limbs related to sustained exercise and relieved with a few minutes of rest while standing evenly on both feet [16]. It was assessed by the Edinburgh claudication questionnaire [17]. Medicine history was documented. Detailed physical examination including height, weight, body mass index (BMI) and cardiovascular system examination was carried out. These were recorded in a proforma sheet. Smokers included both current and past smokers. Hypertension was defined as systolic blood pressure > 140 mm Hg and/or diastolic blood pressure > 90 mm Hg or if the patient was on antihypertensive medications.
Laboratory parameters
Lipid parameters and blood glucose were tested apart from routine pre angiographic investigations which included transthoracic echocardiography and creatinine clearance. Dyslipidaemia was diagnosed as per Lipid Association of India Expert Consensus Statement on Management of Dyslipidaemia in Indians or when the subject was on lipid-lowering medicines [18]. Subjects having fasting blood glucose (FBG) > 126 mg/dL or patients on anti-diabetic medicines were diagnosed as diabetes mellitus. Transthoracic echocardiography was done by Vivid S5 machine with a M3S matrix array probe with a frequency range from 1.7 to 3.2 MHz (GE Vingmed, Horten, Norway), and basic 2-dimensional and M-mode measurements were done with evaluation of left ventricular ejection fraction (LVEF). Each echocardiography study was associated with machine integrated ECG recording.
DUS
DUS was performed before doing coronary angiography and after the subject had rested for at least 5 min in supine position. It was carried out by three experienced radiologists who were blinded to clinical data and consensus was required between at least two of them. PHILIPS iu22 xMATRIX Ultrasound system using 1–3 MHz Broadband linear array transducer and 5–7 MHz curved array transducer with colour Doppler and power Doppler assessment was used. The wall, lumen and flow of the common femoral artery (CFA), superficial femoral artery (SFA), popliteal artery (PA), anterior tibial artery (ATA) and posterior tibial artery (PTA) were evaluated. Velocity criteria were based on the peak systolic velocity (PSV) and velocity ratio (VR). LEAD was classified into mild (1–49% stenosis), significant (50–99% stenosis) and total occlusion (100% stenosis) [19].
CAD and SS
Three experienced interventional cardiologists, who were blinded to clinical data, analysed the coronary angiogram performed using conventional techniques by radial artery access. Consensus was required between at least two of them. The lesions were described on the basis of location, number, extent of involvement, thrombus burden, extent of calcification, tortuosity of involved segments, bifurcation or trifurcation involvement and total occlusion. Scoring was done for each lesion. The SYNTAX Score Calculator software version 2.11 (SYNTAX Score Working Group, www.syntaxscore.com) was used to deduce the SS [11]. The SS was graded into low (0–22), intermediate (23–32) and high (> 32) risk.
Statistical analysis
SPSS version 25.0 (IBM Co, Armonk, NY, USA) was used for data analysis. The continuous variables were presented as the mean ± standard deviation (SD) or median with range, and the categorical variables were presented as percentages. Mann-Whitney test or independent t test was used to compare continuous variables among groups and the chi-square test for comparison of proportional data. Chi-square test was used to evaluate categorical parameters and estimation of risk. Analysis of correlations between categorical variables and risk factors was done by binary logistic regression analysis, and continuous variables were analysed by multivariate linear regression analysis. All statistical tests were two-tailed, and p < 0.05 was considered significant.
Results
Patient’s baseline characteristics
A total of 637 subjects above 45 years of age with coronary angiographic confirmation of CAD were studied. Patients’ baseline characteristics and comparison of characteristics among subjects with and without LEAD is shown in Table 1. Two hundred three subjects (31.9%) had LEAD while it was absent in 68.1%. 85.7% of the subjects with LEAD were male (p = 0.008). Hypertension (77.3%) and smoking (61.1%) were significantly more prevalent among subjects with LEAD. CVE occurred in significantly more number of subjects having LEAD (p = 0.003). 76.4% of patients with LEAD complained of claudication while the rest were asymptomatic. 56.4% of the study population had acute coronary syndrome (ACS) while the rest had stable ischemic heart disease (SIHD). ACS patients comprised 64.5% of subjects with LEAD (p = 0.005). Overall mean age, mean BMI and LVEF were 61.8 ± 8.4 years, 25.2 ± 2.5 kg/m2 and 44.9 ± 7.3% respectively with no significant difference between the two groups. 45.1% of all subjects were diabetic, with no significant difference of presence of diabetes between the groups. Nearly 97% of the subjects were having hypercholesterolemia with no significant difference between subjects with and without LEAD.
Table 1.
Patients’ baseline characteristics and comparison of characteristics among subjects with and without LEAD
| LEAD present n = 203 (%) |
LEAD absent n = 434 (%) |
Total n = 637(%) |
Difference/OR (95% CI) | p value | |
|---|---|---|---|---|---|
| Age in years | 61.4 ± 7.9 | 62.1 ± 8.6 | 61.8 ± 8.4 | − 0.7 (− 2.1–0.7) | 0.3 |
| Male gender | 174 (85.7) | 332 (76.5) | 506 (79.4) | 1.8 (1.2–2.9) | 0.008* |
| BMI | 24.9 ± 2.3 | 25.3 ± 2.6 | 25.2 ± 2.5 | − 0.4 (− 0.8–0.02) | 0.06 |
| Diabetic | 97 (47.8) | 190 (43.8) | 287 (45.1) | 1.2 (0.8–1.6) | 0.35 |
| Hypertensive | 157 (77.3) | 295 (68.0) | 452 (`71.0) | 1.6 (1.1–2.36) | 0.01* |
| Hypercholesterolemia | 197 (97.0) | 419 (96.5) | 616 (96.7) | 1.2 (0.5–3.1) | 0.82 |
| Smoker | 124 (61.1) | 217 (50.0) | 341 (53.5) | 1.6 (1.1–2.2) | 0.01* |
| CKD | 10 (4.9) | 51 (11.8) | 61 (9.6) | 0.4 (0.2–0.8) | 0.006* |
| CVE | 10 (4.9) | 4 (0.9) | 14 (2.2) | 5.6 (1.7–17.9) | 0.003* |
| Claudication | 155 (76.4) | 6 (1.4) | 161 (25.3) |
230.4 (96.7–548.9) Ln 5.4 (4.6–6.3) |
< 0.0001* |
| ACS | 131 (64.5) | 228 (52.5) | 359 (56.4) | 0.6 (0.4–0.8) | 0.005* |
| EF (%) | 44.3 ± 8.1 | 45.2 ± 6.8 | 44.9 ± 7.3 | 0.9 (− 2.1–0.3) | 0.1 |
| Antiplatelets | 167 (82.3) | 393 (90.5) | 568 (89.2) | 8.2 (2.2–15.2) | 0.006* |
| Statins | 156 (76.8) | 401 (92.4) | 557 (87.4) | 15.6 (8.94–23.2) | < 0.0001* |
| ACEI/ARB | 111 (54.7) | 215 (49.5) | 326 (51.2) | 5.2 (− 6.2–16.3) | 0.4 |
| Beta-blockers | 99 (48.8) | 216 (49.8) | 315 (49.5) | 1.0 (− 10.7–12.67) | 0.9 |
| CCB | 34 (16.7) | 74 (17.1) | 108 (17.0) | 0.4 (− 16.8–13.9) | 0.9 |
| Nitrates | 165 (81.2) | 366 (84.3) | 531 (83.3) | 3.1 (− 3.5–10.6) | 0.4 |
| Antidiabetics | 77/ 97(79.4) | 180/ 190 (94.7) | 257/ 287 (89.5) | 15.3 (6.6–25.9) | 0.0002* |
| SS | 23.2 ± 9.5 | 21.7 ± 8.6 | 22.2 ± 8.9 | 1.5 (− 0.03–3.0) | 0.06 |
Data given as mean ± SD or n (%)
ACEI/ARB angiotensin-converting enzyme inhibitor/angiotensin receptor blocker, ACS acute coronary syndrome, BMI body mass index, CCB calcium channel blockers, CI confidence interval, CKD chronic kidney disease, CVE cerebrovascular event, EF ejection fraction, LEAD lower extremity arterial disease, OR odds ratio, SD standard deviation, SS SYNTAX score, * significant
Baseline antiplatelet, statin and antidiabetic medication intake was significantly less among subjects with LEAD. There was no difference between the groups in usage of angiotensin-converting enzyme inhibitor/angiotensin receptor blocker (ACEI/ARB), beta-blockers, calcium channel blockers (CCB) and nitrates.
LEAD and SS
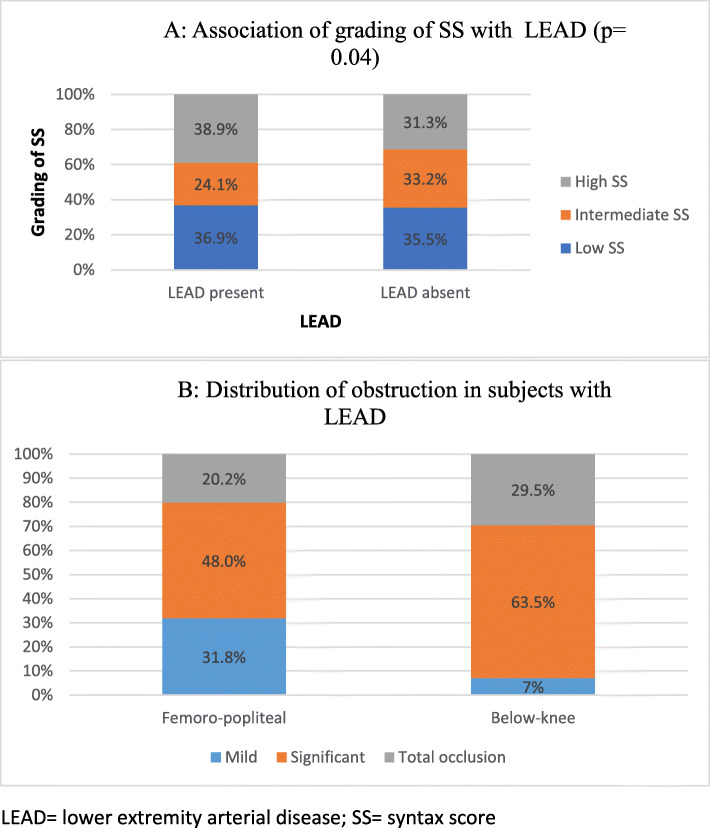
High SS was significantly more common in subjects with LEAD (p = 0.04) (Fig. 1a).
Fig. 1.
a Association of grading of SS with LEAD (p = 0.04). b Distribution of obstruction in subjects with LEAD. LEAD, lower extremity arterial disease; SS, SYNTAX score
In the femoro-popliteal segment, total occlusion of arteries were found in significantly more proportion of subjects with high SS (9.3%) than low and intermediate SS separately. Significant occlusion in the femoro-popliteal segment was also more prevalent in the subjects with high SS whereas in the below-knee arterial segment no such association was noted (p = 0.08). Mean SS was 22.2 ± 8.9 with no significant difference between the two groups (Table 1). A progressive increase in mean SS was noted across the grades of arterial disease in the femoro-popliteal segment (p = 0.007). Though mean SS was more in subjects with significant occlusion and total occlusion in the below-knee arterial segment than those with normal arteries, no significant association was noted in this segment between mean SS and grades of LEAD (p = 0.06).
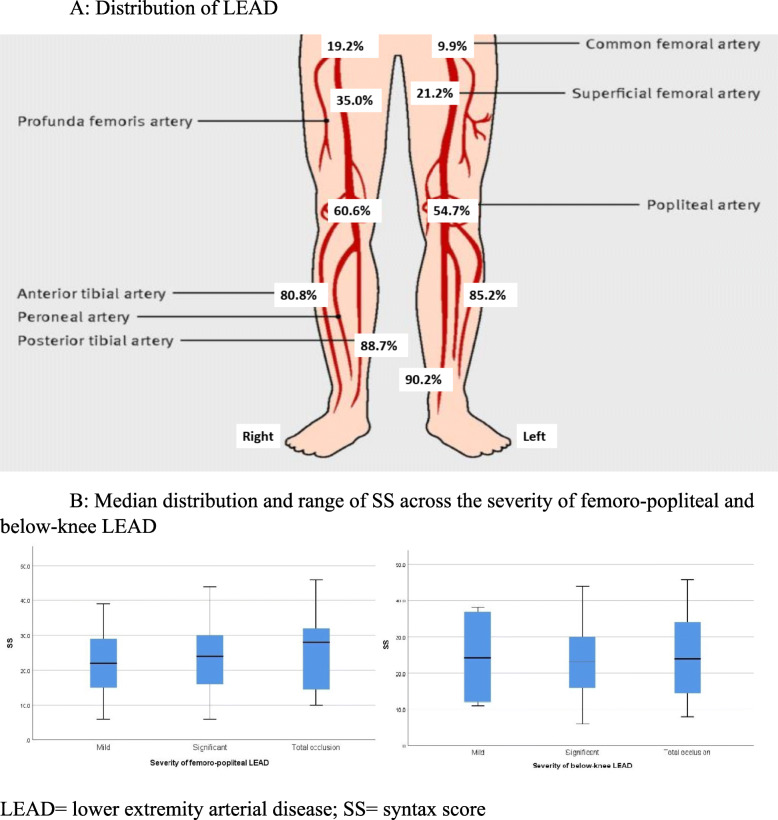
Distribution of LEAD
Figure 1b shows the distribution of obstruction in subjects with LEAD. Figure 2a shows the overall distribution of LEAD. Above 80% of the LEAD were in below-knee arteries (ATA and PTA) whereas only 10–20% of the disease were in the CFA. Figure 2b shows the median distribution and range of SS across the severity of femoro-popliteal and below-knee disease.
Fig 2.
a Distribution of LEAD. b Median distribution and range of SS across the severity of femoro-popliteal and below-knee LEAD. LEAD, lower extremity arterial disease; SS, SYNTAX score
Taking segmental distribution into account, 85.2% of the LEAD was in the femoro-popliteal segment, while below-knee arterial disease was present in 98.5% of subjects with LEAD (95% CI 8.2–18.9, p < 0.0001).
Multinomial logistic regression
Table 2 shows multinomial logistic regression for detection of independent contribution of the baseline factors in LEAD. Keeping other baseline parameters fixed, hypertension, smoking, history of CVE and presentation with ACS independently increased the risk of LEAD. Presence of CKD was found to have independent negative association with LEAD.
Table 2.
Predictors of LEAD in patients with CAD
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | |
| Male gender | 1.8 (1.2–2.9) | 0.008 | 1.5 (0.9–2.5) | 0.1 |
| Hypertension | 1.6 (1.1–2.36) | 0.01 | 1.9 (1.3–2.9) | 0.002* |
| Smoker | 1.6 (1.1–2.2) | 0.01 | 1.5 (1.01–2.2) | 0.046* |
| CKD | 0.4 (0.2–0.8) | 0.006 | 0.4 (0.2–0.8) | 0.01* |
| CVE | 5.6 (1.7–17.9) | 0.003 | 3.8 (7.3–12.7) | 0.03* |
| ACS | 0.6 (0.4–0.8) | 0.005 | 0.7 (0.5–0.97) | 0.03* |
We adjusted the result for male gender, hypertension, smoker, CKD, CVE and ACS
ACS acute coronary syndrome, CAD coronary artery disease, CI confidence interval, CKD chronic kidney disease, CVE cerebrovascular event, LEAD lower extremity arterial disease, OR odd ratio, * significant
Discussion
Atherosclerosis affects various arterial territories simultaneously since it is a systemic pathological process. Thus, a person with atherosclerotic disease in one vascular territory has higher risk of disease in other territories as well [20–22].
Prevalence of LEAD in subjects with CAD
LEAD is prevalent in 7–16% of subjects with CAD as per the Western data [9]. An Indian study by Saran et al. reported the prevalence to be 7.7%, but this was based on only ABI measurement [23]. We found the prevalence of LEAD in subjects with CAD to be 31.9% which was much higher than this previous study by Saran et al. but corroborated with the Indian data by Sarangi et al. (33.3%) [12]. We attribute this higher prevalence to the use of better diagnostic modality in form of DUS. Higher sample size in our study (n = 637) than the study by Saran et al. (n = 207) may have also provided a better picture.
Baseline characteristics
A study has documented the association of complexity in peripheral arterial lesions with complex coronary lesions while another study showed the increased risk for adverse cardiovascular events in patients with LEAD [24, 25]. Baseline risk factors like age, gender, hypertension, diabetes and dyslipidaemia should be taken into account while analysing such associations. In the study by Petracco et al., the baseline demographics were similar in both the groups whereas Sarangi et al. reported the predominance of PAD in diabetics and smokers [12, 15]. Falcão et al. found a significantly higher number of female subjects and subjects with ACS in the PAD group while Saran et al. reported significantly higher mean age, prevalence of diabetes and hypertension in subjects with ABI < 0.9 [14, 23]. In our study, male gender, hypertension, smoking, CVE and ACS were significantly more prevalent in the LEAD group. Baseline intake of antiplatelet, statin and antidiabetic medications were significantly less in subjects with LEAD which may have contributed to the progression of atherosclerotic disease process.
United States Preventive Services Task Force (USPSTF) states that the benefit of screening for PAD and CAD risk in asymptomatic adults with ABI is not clear cut with current evidence [26]. In our study, 23.6% subjects with DUS diagnosed LEAD were asymptomatic which is quite a sizeable proportion and thus further research regarding benefit of screening and the screening tool to be used is warranted.
LEAD and SS
The study by Korkmaz et al. on 150 patients with ACS reported higher SS in subjects with ABI ≤ 0.9 (p < 0.001) [27]. Benyakorn et al. included a large proportion of subjects with valvular heart disease and they also demonstrated significant negative correlation between ABI and SS [28]. Falcão et al. found that correlation between ABI and SS was lost when analysis was done among patients of obstructive CAD (p = 0.148) [14]. Petracco et al. reported negative correlation between ABI and SS but it was statistically insignificant [15]. In our study, high SS (>32) was more frequently noted in subjects with LEAD (p = 0.04) but mean SS did not vary significantly between the two groups.
Distribution of LEAD
Femoro-popliteal disease was more common than other distributions according to studies by Diehm et al. (51.2%), Hatmayer et al. (77%), Vogt et al. (47.3%) and Chen et al. (common femoral 57.6%) [29]. Contrary to the above data, our study revealed significantly more below-knee arterial disease than femoro-popliteal disease (p < 0.0001). This discrepancy may be attributed to the difference of baseline characteristics of the subjects.
Vuruskan et al. found that angiographic critical stenosis in femoro-popliteal segment was most reliable for the determination of subjects with high SS [30]. In the present study, significant and total occlusion of the femoro-popliteal segment arteries by DUS were found in significantly more proportion of subjects with high SS (p = 0.02). No such association was noted in the below-knee arterial segment (p = 0.08).
Predictors of peripheral artery disease in patients with CAD
Saleh et al. found independent association of age, hypertension, diabetes mellitus and smoking with PAD [31]. Another study found PAD was independent risk factor for CAD and CVE [13]. In the present study, hypertension, smoking, history of CVE and presentation with ACS independently increased the risk of LEAD. Strikingly, the presence of CKD was found to have independent negative association with LEAD which can be due to platelet and clotting factor dysfunction in CKD but needs further insight.
Limitations
The sample size was sizeable but larger population would give a better picture. This study does not provide outcome data due to lack of follow-up. Hospitalised patients with coronary angiographic confirmation of CAD were included thus automatically selecting a population with higher possibility of LEAD. Thus, these results should be treated with caution in general population. We studied only anatomical presentation of coronary and LEAD by angiographic calculation of SS and DUS respectively. Functional assessment of the lesions might find a more robust relationship between the diseases in two territories. Lower limb angiography was not performed hence extent and burden of underlying atherosclerosis may have not been accurately reflected. Exclusion of assessment of renal and aorto-iliac segments also remains a limitation. Randomised studies specifically designed for this purpose are needed to affirm the findings.
Conclusion
High prevalence of asymptomatic LEAD and association of high SS with LEAD as a whole as well as femoro-popliteal involvement suggests the need for a point of care DUS study (POCUS) which is being already used in multiple fields, since treatment varies with location and extent of disease which cannot be appreciated by ABI alone.
Acknowledgements
None
Abbreviations
- ABI
Ankle brachial index
- ACS
Acute coronary syndrome
- ATA
Anterior tibial artery
- BMI
Body mass index
- CABG
Coronary artery bypass grafting
- CAD
Coronary artery disease
- CFA
Common femoral artery
- CKD
Chronic kidney disease
- CVE
Cerebrovascular events
- DUS
Duplex ultrasound
- FBG
Fasting blood glucose
- LEAD
Lower extremity artery disease
- PA
Popliteal artery
- PAD
Peripheral arterial disease
- PCI
Percutaneous intervention
- PSV
Peak systolic velocity
- PTA
Posterior tibial artery
- SD
Standard deviation
- SFA
Superficial femoral artery
- SIHD
Stable ischemic heart disease
- SS
SYNTAX score
- USPSTF
United States Preventive Services Task Force
- VR
Velocity ratio
Authors’ contributions
AM and DK made substantial contributions to the conception and design of the work; SN, AM and KB to the acquisition, analysis and interpretation of data; AM and DK have drafted the work and substantively revised it, SN, AM, DK and KB have approved the submitted version and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Funding
None
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Ethical approval and consent was taken.
Institutional ethics committee of NRS Medical College, Kolkata, India, approved the study. Reference no. – No/NMC/959.
Informed written consent for participation was obtained from individual patients.
Consent for publication
N/A as anonymity was not compromised.
Competing interests
The authors declare that they have no competing interests.
Footnotes
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1186/s43044-020-00130-9
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
12/29/2020
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1186/s43044-020-00091-z.
Contributor Information
Saumen Nandi, Email: saumennandi@gmail.com.
Anindya Mukherjee, Email: anindya768@yahoo.co.in.
Dibbendhu Khanra, Email: ddk3987@gmail.com.
Kaushik Biswas, Email: b.drkaushik@gmail.com.
References
- 1.Pellegrino T, Storto G, Filardi PP, et al. Relationship betweenbrachial artery flow-mediated dilation and coronary flow reserve in patients with peripheral artery disease. J Nucl Med. 2005;46(12):1997–2002. [PubMed] [Google Scholar]
- 2.Ross AJ, Gao Z, Luck JC, et al. Coronary exercise hyperemia is impaired in patients with peripheral arterial disease. Ann Vasc Surg. 2017;38:260–267. doi: 10.1016/j.avsg.2016.05.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eagle KA, Rihal CS, Foster ED, Mickel MC, Gersh BJ. Long-termsurvival in patients with coronary artery disease: importance of peripheral vascular disease. The coronary artery surgery study (CASS)investigators. J Am CollCardiol. 1994;23:1091–1095. doi: 10.1016/0735-1097(94)90596-7. [DOI] [PubMed] [Google Scholar]
- 4.Krumholz HM, Chen J, Chen YT, Wang Y, Radford MJ. Predicting one-year mortality among elderly survivors of hospitalization for anacute myocardial infarction: results from the cooperative cardiovascular project. J Am CollCardiol. 2001;38:453–459. doi: 10.1016/S0735-1097(01)01395-X. [DOI] [PubMed] [Google Scholar]
- 5.Chiu JH, Topol EJ, Whitlow PL, Hsu AP, Tuzcu EM, Franco I, Moliterno DJ. Peripheral vascular disease and one-year mortality following percutaneous coronary revascularization. Am J Cardiol. 2003;92:582–583. doi: 10.1016/S0002-9149(03)00726-4. [DOI] [PubMed] [Google Scholar]
- 6.Narins CR, Zareba W, Moss AJ, Marder VJ, Ridker PM, Krone RJ, Lichstein E. Relationship between intermittent claudication, inflammation, thrombosis, and recurrent cardiac events among survivors ofmyocardial infarction. Arch Intern Med. 2004;164:440–446. doi: 10.1001/archinte.164.4.440. [DOI] [PubMed] [Google Scholar]
- 7.Cimminiello C. Peripheral arterial disease – epidemiology and pathophysiology. Thromb Res. 2002;106:295–301. doi: 10.1016/S0049-3848(01)00400-5. [DOI] [PubMed] [Google Scholar]
- 8.Leng GC, Fowkes FGR, Lee AJ. Use of the ankle brachial pressure index to predict cardiovascular events and death – a cohort study. BMJ. 1996;313:1440–1444. doi: 10.1136/bmj.313.7070.1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aboyans V, Ricco JB, Bartelink MEL, Björck M, Brodmann M, Cohnert T, Collet JP, Czerny M, De Carlo M, Debus S, Espinola-Klein C, Kahan T, Kownator S, Mazzolai L, Naylor AR, Roffi M, Röther J, Sprynger M, Tendera M, Tepe G, Venermo M, Vlachopoulos C, Desormais I, ESC Scientific Document Group 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries endorsed by: the European stroke organization (ESO) the Task Force for the diagnosis and treatment of peripheral arterial diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS) Eur Heart J. 2018;39(9):763–816. doi: 10.1093/eurheartj/ehx095. [DOI] [PubMed] [Google Scholar]
- 10.Collins R, Cranny G, Burch J, Aguiar-Ibanez R, Craig D, Wright K, Berry E, Gough M, Kleijnen J, Westwood M. A systematic review of duplex ultrasound, magnetic resonance angiography and computed tomography angiography for the diagnosis and assessment of symptomatic, lower limb peripheral arterial disease. Health Technol Assess. 2007;11:1–184. doi: 10.3310/hta11200. [DOI] [PubMed] [Google Scholar]
- 11.Serruys PW, Morice M-C, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. New Engl J Med. 2009;360(10):961–972. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 12.Sarangi S, Srikant B, Rao DV, Joshi L, Usha G. Correlation between peripheral arterial disease and coronary artery disease using ankle brachial index-a study in Indian population. Indian Heart J. 2012;64(1):2–6. doi: 10.1016/S0019-4832(12)60002-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pang XH, Han J, Ye WL, Sun X, Ding Y, Huang WJ, Zhao YM, Lou HY, Shan LZ, Kang YX, Song XX, Zhang SZ, Gu W, Shan PF. Lower extremity peripheral arterial disease is an independent predictor of coronary heart disease and stroke risks in patients with type 2 diabetes mellitus in China. Int J Endocrinol. 2017;2017:9620513. doi: 10.1155/2017/9620513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Falcão FJ, Rodrigues Alves CM, Caixeta A, de FreitasGuimarães L, de Sousa Filho JT, Soares JA, Helber I, Carvalho AC. Relation between the ankle-brachial index and the complexity of coronary artery disease in older patients. ClinInterv Aging. 2013;8:1611–1616. doi: 10.2147/CIA.S52778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Petracco AM, Carlos BL, Farias PG, Santos TG, de Oliveira PD, Claudio DL, et al. Assessment of the relationship of ankle-brachial index with coronary artery disease severity. Int J Cardiovasc Sci. 2018;31(1):47–55. [Google Scholar]
- 16.Smith RB III (1990) Claudication. In: Walker HK, Hall WD, Hurst JW, (ed) Clinical methods: the history, physical, and laboratory examinations, 3rd edn. Boston: Butterworths; Chapter 13. Available from: https://www.ncbi.nlm.nih.gov/books/NBK235/ [PubMed]
- 17.Edinburgh claudication questionnaire. (2002). Occasional paper (Royal College of General Practitioners), (82), 44.
- 18.Iyengar SS, Puri R, Narasingan SN. Lipid Association of India Expert Consensus Statement on Management of Dyslipidemia in Indians 2016: part 1 - executive summary. J Clin Prev Cardiol. 2016;5:51–61. doi: 10.4103/2250-3528.186492. [DOI] [Google Scholar]
- 19.Eiberg JP, Grønvall Rasmussen JB, Hansen MA, Schroeder TV. Duplex ultrasound scanning of peripheral arterial disease of the lower limb. Eur J Vasc Endovasc Surg. 2010;40:507–512. doi: 10.1016/j.ejvs.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 20.Heras M, Chamorro A. Atherosclerosis: a systemic condition that requires a global approach. Eur Heart J. 2000;21(11):872–873. doi: 10.1053/euhj.1999.2071. [DOI] [PubMed] [Google Scholar]
- 21.Viles-Gonzalez JF, Fuster V, Badimon JJ. Atherothrombosis: a widespread disease with unpredictable and life-threatening consequences. Eur Heart J. 2004;25(14):1197–1207. doi: 10.1016/j.ehj.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 22.Saçar M, Önem G, Sarıoğlu Büke A, et al. The effect of distance based learning on the fifth stage medical students’ perception in peripheral vascular diseases course: a questionnaire survey. Anadolu Kardiyol Derg. 2013;13(3):275–277. doi: 10.5152/akd.2013.079. [DOI] [PubMed] [Google Scholar]
- 23.Saran R, Bhagat R, Narain V, et al. Prevalence of peripheral arterial diseases in patient with coronary artery diseases of Indian origin. Heart. 2012;98:E266. doi: 10.1136/heartjnl-2012-302920u.2. [DOI] [Google Scholar]
- 24.Aykan AÇ, Hatem E, Karabay CY, et al. Complexity of lower extremity peripheral artery disease reflects the complexity of coronary artery disease. Vascular. 2015;23(4):366–373. doi: 10.1177/1708538114550738. [DOI] [PubMed] [Google Scholar]
- 25.Subherwal S, Bhatt DL, Li S, et al. Polyvascular disease and long-term cardiovascular outcomes in older patients with nonST-segment-elevation myocardial infarction. Circ Cardiovasc Qual Outcomes. 2012;5(4):541–549. doi: 10.1161/CIRCOUTCOMES.111.964379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Preventive Services Task Force US, Curry SJ, Krist AH, et al. Screening for peripheral artery disease and cardiovascular disease risk assessment with the ankle-brachial index: US Preventive Services Task Force recommendation statement. JAMA. 2018;320(2):177–183. doi: 10.1001/jama.2018.8357. [DOI] [PubMed] [Google Scholar]
- 27.Korkmaz L, Adar A, Erkan H, et al. Ankle-brachial index and coronary artery lesion complexity in patients with acute coronary syndromes. Angiology. 2012;63(7):495–499. doi: 10.1177/0003319711429561. [DOI] [PubMed] [Google Scholar]
- 28.Benyakorn T, Kuanprasert S, Rerkasem K. A correlation study between ankle brachial pressure index and the severity of coronary artery disease. Int J Low Extrem Wounds. 2012;11(2):120–123. doi: 10.1177/1534734612446966. [DOI] [PubMed] [Google Scholar]
- 29.Chen Q, Shi Y, Wang Y, Li X. Patterns of disease distribution of lower extremity peripheral arterial disease. Angiology. 2015;66(3):211–218. doi: 10.1177/0003319714525831. [DOI] [PubMed] [Google Scholar]
- 30.Vuruskan E, Saracoglu E, Polat M, Duzen IV. Prediction of coronary artery disease severity in lower extremity artery disease patients: a correlation study of TASC II classification, Syntax and Syntax II scores. Cardiol J. 2017;24(5):495–501. doi: 10.5603/CJ.a2017.0033. [DOI] [PubMed] [Google Scholar]
- 31.Saleh A, Makhamreh H, Qoussoos T, et al. Prevalence of previously unrecognized peripheral arterial disease in patients undergoing coronary angiography. Medicine (Baltimore) 2018;97(29):e11519. doi: 10.1097/MD.0000000000011519. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.