Abstract
The Onduo Virtual Diabetes Clinic (VDC) telehealth technology/care model for adults with type 2 diabetes (T2D) combines connected devices, remote lifestyle coaching, and clinical support with a mobile App. Key differentiating program features are the availability of live video consultations with board-certified endocrinologists for medication management and real-time continuous glucose monitor use for higher-risk participants. Preliminary data (n = 740) suggest that participation was associated with a significant improvement in HbA1c with up to 6 months follow-up in those not meeting treatment targets. HbA1c decreased by 2.3% ± 1.9%, 0.7% ± 1.0%, and 0.2% ± 0.8% across baseline categories of >9.0%, 8.0%-9.0% and 7.0% to <8.0%, respectively (all P < .001). These findings suggest that the VDC has potential to support individuals with T2D and their clinicians in diabetes management between office visits.
Keywords: A1c, connected care, digital health, mobile health, telemedicine, type 2 diabetes
Introduction
Despite increases in the number of effective drugs, the availability of advanced treatment technologies and evidence-based prevention and lifestyle modification programs, diabetes outcomes have not improved over time.1,2 New approaches to diabetes care and delivery are needed given the expected increase in the prevalence of type 2 diabetes (T2D) to 49 million people by the year 2030, most of whom will not have access to care from diabetes specialists.3-7
Telemedicine is a growing area of healthcare for people with diabetes and has the potential to increase access to care, positively impact self-management behaviors, and improve health outcomes.8-14 However, current programs vary in the use of technologies employed, models for interactions, and access to diabetes professionals. This report describes the Onduo Virtual Diabetes Clinic (VDC) telehealth technology and the associated care model, and presents preliminary HbA1c outcomes data.
Methods
The VDC Program
Overview
The VDC is a telehealth program for people with T2D designed to support diabetes management in the primary care setting between office visits. The program combines mobile App technology, remote personalized lifestyle coaching from certified diabetes educators (CDEs) and health coaches, and connected tools and medical devices, including blood glucose (BG) meters and continuous glucose monitor (CGM) devices. Key differentiating features are the availability of live video consultations with board-certified endocrinologists for medication management (diabetes-related, antihypertensives) and/or to prescribe real-time (rt)CGM devices as clinically appropriate for higher-risk participants. The program is managed through an innovative software platform, which includes a central dashboard for care team management of participant profiles, data, and program engagement and the VDC mobile App, a communication and education tool that allows for messaging between care leads, clinicians, and participants.
The VDC App
The VDC App connects wirelessly to commercially available medical devices and allows for logging and tracking of data relevant to participant’s diabetes care. These include the display of glucose readings from BG meters or CGM, medication tracking, logging of physical activity such as step counting, nutritional support from meal logging (including meal photos and location of meal consumption), educational materials about lifestyle modification, and notifications and reminders. Participants interact with their care team primarily through messaging in the VDC App, and with occasional phone calls. Participant demographic and clinical profiles, management goals, and uploaded and logged program data are managed by the care team through the dashboard, which also serves as an analytic tool for program outcomes data. The VDC technology provides channels for communication and transfer of medical record data with participant’s primary care providers (PCP). The VDC endocrinologists manage participant clinical visit data in a commercially available electronic health record system (athenahealth, Watertown, MA, USA).
Enrollment and engagement
The VDC is available to eligible adults with T2D who are members of health plans and employers who sponsor the program throughout the United States. Those who elect to enroll then download the VDC App to their smartphone and complete baseline surveys. Participants are subsequently mailed a self-management kit that includes a cellular-connected BG meter (Telcare, Malvern, PA, USA), test strips, and a home HbA1c testing kit (DTI Laboratories Inc., Thomasville, GA, USA).
As first level of support, health coaches actively engage with participants and send educational microlearning modules and videos via the App to support lifestyle change goals. BG data, from the connected meter or program-prescribed rtCGM (Dexcom G5/G6, Dexcom, San Diego, CA, USA), are a cornerstone of the VDC. Glucose data are used by the care team for review and coaching as an educational feedback loop that allows participants to associate their glucose levels with their diet, lifestyle, and other factors to reinforce and optimize self-management. The lifestyle and clinical guidance follow the best practices of the American Association of Diabetes Educators Diabetes Education Curriculum and the American Diabetes Association (ADA) Standards of Care.15-17
An escalation protocol based upon ADA standards16 triggers higher-risk case review and a second level of education with a CDE. These participants typically have an HbA1c ≥8.0%, use insulin or a sulfonylurea, or have repeated hypo- or hyperglycemic episodes as identified by the connected BG meter. Participants may also have further escalation to a third-level clinical consultation with an endocrinologist for specialist evaluation.
Endocrinologist consultations are live video medical appointments held via a commercially available telemedicine App (Amwell, American Well Corp., Boston, MA, USA). VDC endocrinologists are licensed in 49 states and may initiate and/or change medication prescriptions and prescribe an rtCGM if the participant elects, and all these information are communicated with the PCP. Participants may transition between levels of care over time based upon their clinical profile, with the VDC goal of providing higher levels of clinical support only when needed and allowing individuals to choose their level of engagement with the program and care team.
Outcomes
This preliminary analysis characterized VDC participants who enrolled from February 2018 through December 2018 and had initial and follow-up HbA1c measurements. Demographic characteristics and clinical data were obtained by self-report from the onboarding survey and/or verified with medical records or health insurance claims records. HbA1c testing was requested but was not a requirement for program participation. Available HbA1c data were either provided by the participant and verified by the health coach with the PCP or obtained directly from the provider or medical record, or obtained from a central laboratory analyzing the participant home-test samples. Change in HbA1c was calculated as the difference between the initial measurement, obtained within 30 days prior to or post enrollment, and the follow-up measurement, obtained between 90 and 180 days from the initial measurement. The analysis was approved by the Western Institutional Review Board for waiver of consent.
Results
Participants (n = 740) residing in 21 states throughout the United States are described in Table 1. The mean follow-up time period was 4.2 months (125.6 ± 22.4 days) and 191 (25.8%) participants had a telemedicine appointment with an endocrinologist. Change in HbA1c is reported in Figure 1. HbA1c decreased significantly by −2.3% ± 1.9%, −0.7% ± 1.0%, and −0.2% ± 0.8% across the baseline categories of >9.0%, 8.0%-9.0%, and 7.0% to <8.0%, respectively (all P < .001). Within these categories, HbA1c improved in 91.9%, 77.3%, and 63.5% of participants, respectively. Participants with an initial HbA1c <7.0% who were meeting the ADA treatment target, HbA1c 6.3% ± 0.4%, continued to maintain this level of glycemic control at follow-up, HbA1c 6.4% ± 0.6% (ns).
Table 1.
Demographic and Baseline Clinical Characteristics.
| Parameter | HbA1c evaluation cohort (n = 740) |
|---|---|
| Age, y | 53.8 ± 8.8 |
| Female, # (%) | 468 (63) |
| Body mass index | 35.6 ± 8.5a |
| Baseline HbA1c, % | 7.7 ± 1.7 |
| Medication use, # (%) | |
| Sulfonylurea | 192 (25.9) |
| Insulin | 230 (31.1) |
| CGM delivered, # (%) | 340 (45.9) |
| Geography, # (%)18 | |
| Urban | 512b (70.0) |
| Rural | 222b (30.0) |
Data are mean ± SD unless otherwise indicated.
CGM, continuous glucose monitor.
n = 663, bn = 734.
Figure 1.
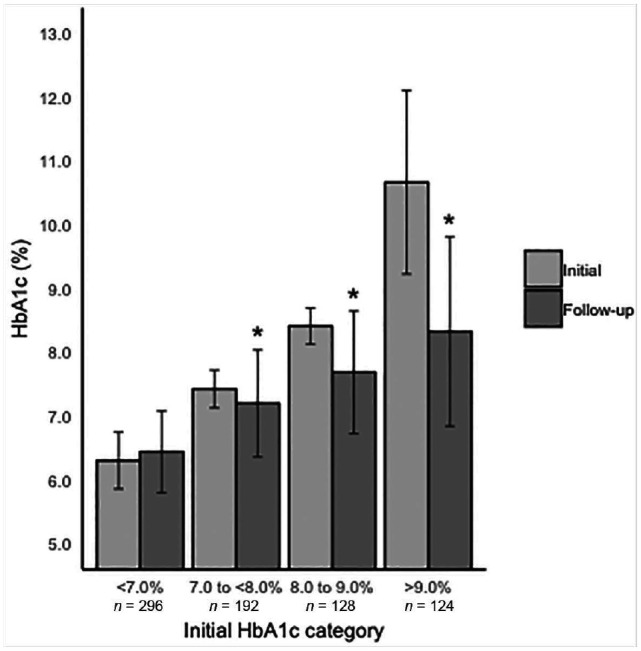
Change in HbA1c from initial measurement to follow-up stratified by initial HbA1c range.
Data are presented as mean ± SD. The initial HbA1c measurement was obtained within 30 days prior to or post enrollment and the follow-up HbA1c was defined as the most recent measurement obtained within 90 to 180 days from initial measurement. The mean follow-up time period was 4.2 months (125.6 ± 22.4 days). *P < .001.
Discussion
The VDC is an innovative telehealth program for people with T2D. The clinic is enabled by a software platform that includes a smartphone App for communication with the care team and connected device data transfer. The program also includes a strong analytic framework to inform health coaching, stepped clinical care, and provide population outcomes data. The VDC care model allows participants to transition dynamically between levels of clinical support as needed. This may be particularly beneficial to increase access to specialist care for people with diabetes, the overwhelming majority who are treated in the primary care setting without access to endocrinologists or CDEs, or advanced technology including CGM. Increasing access to specialist care is also an important consideration for those living in rural areas, which included 30% of participants in this analysis.
There is a growing body of evidence supporting the use of CGM technology in T2D management to improve glycemic control and treatment adherence; however, utilization and access have been limited, particularly for primary care patients.19,20 The ability of VDC endocrinologists to prescribe rtCGM devices with remote CGM onboarding and use by higher-risk participants to improve self-management and clinical outcomes are currently being evaluated.
While recent data from a commercially available telehealth program suggest that connected BG meter use with responsive automated messaging and access to coaching for goal setting may reduce glucose excursions12 and improve mean BG,14 significantly greater decreases in mean BG were observed with a greater level/intensity of coaching. This highlights the potential benefits of highly accessible personalized, ongoing coaching to support lifestyle change, which is central to VDC diabetes management approach.
Preliminary data suggest that participation in the VDC was associated with a significant improvement in HbA1c in adults with T2D who were not meeting targets. The greatest improvement was seen in those with higher initial HbA1c levels, with HbA1c improving by more than 2% points in participants with an initial HbA1c >9.0%. Importantly, the majority of program participants who were not meeting treatment targets experienced an improvement in HbA1c. Supporting individuals with HbA1c <7.0% to maintain at target and to improve diabetes self-management through individualized coaching is also an important focus of the VDC.
Strengths of the VDC care model include real-time engagement with the care team, availability of remote live medical appointments for potential medication adjustments, the widespread use of CGM and use of measured HbA1c as an outcome. This preliminary analysis presents real-world data on a large number of participants with a wide range of treatment regimens, baseline levels of glycemic control, and geographies. However, this analysis has several limitations including lack of a control group and self-selection bias. In addition, the follow-up time period for HbA1c outcomes was relatively short (mean 4.2 months) with measurements ranging from 3 to 6 months due to the real-world nature of the data compared to a clinical trial protocol. There were also challenges in obtaining follow-up data as HbA1c testing, although requested, is not a requirement for program participation, and in some cases initial and follow-up data were not concordant for source. Longer-term data are being collected, which might or might not differ from the data collected to date, and these data will be reported subsequently.
Ongoing and future research initiatives, including randomized trials, will evaluate intermittent use of rtCGM, comorbidities (eg, hypertension and obesity), medication adherence and optimization, program engagement and lifestyle interventions, quality of life, and healthcare costs. The results of the studies will inform the VDC technology development, model of care, and processes to further optimize engagement and outcomes for participants.
Conclusion
The VDC, which combines mobile App technology, remote personalized lifestyle coaching, connected devices, and clinical support from board-certified endocrinologists, is a unique telehealth model to support individuals with T2D and their clinicians in diabetes management between office visits. Preliminary data suggest that participation in the VDC may be associated with improvement in HbA1c in participants with T2D who were not meeting treatment targets.
Acknowledgments
The authors thank the care leads, certified diabetes educators, and physicians of Onduo for their dedication to VDC member care, and Amy Armento Lee of Verily Life Sciences for her assistance with data analysis.
Footnotes
Authors’ Note: Data included in this manuscript will be presented in part at the 2019 Connected Health Conference in Boston, MA.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: RFD, JEL, NAB, DPMo, and JR are employees of Onduo LLC. Onduo is a joint venture of Verily and Sanofi; HZ and DPMi are employees of Verily Life Sciences. ARM has received consulting fees from Onduo LLC, and RAG has received consulting fees from Onduo LLC, Health Reveal, and Lark Health.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by Onduo, LLC.
ORCID iD: Jennifer E. Layne  https://orcid.org/0000-0001-7144-7051
https://orcid.org/0000-0001-7144-7051
References
- 1. Kazemian P, Shebl FM, McCann N, Walensky RP, Wexler DJ. Evaluation of the cascade of diabetes care in the United States, 2005-2016. JAMA Intern Med. 2019;179(10):1376-1385.doi: 10.1001/jamainternmed.2019.2396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Foster NV, Beck RW, Miller KM, et al. State of type 1 diabetes management and outcomes from the T1D exchange in 2016-2018. Diabetes Technol Ther. 2019;21(2):66-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention. 2017 National Diabetes Statistics Report. Atlanta, GA: US Department of Health and Human Services; 2019. [Google Scholar]
- 4. Bullard KM, Cowie CC, Lessem SE. Prevalence of diagnosed diabetes in adults by diabetes type — United States, 2016. Morb Mortal Wkly Rep. 2018;67(12):359-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Meyers JL, Parasuraman S, Bell KF, Graham JP, Candrilli SD. The high-cost, type 2 diabetes mellitus patient: an analysis of managed care administrative data. Arch Public Health. 2014;72(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. American Diabetes Association. Economic costs of diabetes in the US 2017. Diabetes Care. 2018;41(5):917-928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rowley WR, Bezold C, Arikan Y, Byrne E, Krohe S. Diabetes 2030: insights from yesterday, today, and future trends. Popul Health Manag. 2017;20(1):6-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hou C, Carter B, Hewitt J, Francisa T, Mayor S. Do mobile phone applications improve glycemic control (HbA1c) in the self-management of diabetes? A systematic review, meta-analysis, and GRADE of 14 randomized trials. Diabetes Care. 2016;39(11):2089-2095. [DOI] [PubMed] [Google Scholar]
- 9. Hou C, Xu Q, Diao S, Hewitt J, Li J, Carter B. Mobile phone applications and self-management of diabetes: a systematic review with meta-analysis, meta-regression of 21 randomized trials and GRADE. Diabetes Obes Metab. 2018;20(8):2009-2013. [DOI] [PubMed] [Google Scholar]
- 10. Garg SK, Parkin CG. The emerging role of telemedicine and mobile health technologies in improving diabetes care. Diabetes Technol Ther. 2019;21(S2):S21-S23. [DOI] [PubMed] [Google Scholar]
- 11. Debong F, Mayer H, Kober J. Real-world assessments of mySugr mobile health app. Diabetes Technol Ther. 2019;21(S2):S235-S240. [DOI] [PubMed] [Google Scholar]
- 12. Downing J, Bollyky J, Schneider J. Use of a connected glucose meter and certified diabetes educator coaching to decrease the likelihood of abnormal blood glucose excursions: the Livongo for diabetes program. J Med Internet Res. 2017;19(7):e234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Offringa R, Sheng T, Parks L, Clements M, Kerr D, Greenfield MS. Digital diabetes management application improves glycemic outcomes in people with Type 1 and Type 2 diabetes. J Diabetes Sci Technol. 2018;12(3):701-708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bollyky JB, Bravata D, Yang J, Williamson M, Schneider J. Remote lifestyle coaching plus a connected glucose meter with certified diabetes educator support improves glucose and weight loss for people with type 2 diabetes. J Diabetes Res. 2018;3961730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Beck J, Greenwood DA, Blanton L, et al. 2017 National standards for diabetes self-management education and support. Diabetes Educ. 2018;44(1):35-50. [DOI] [PubMed] [Google Scholar]
- 16. American Diabetes Association. Standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Supplement 1):S1.30559224 [Google Scholar]
- 17. American Association of Diabetes Educators. AADE7 self-care behaviors. Diabetes Educ. 2008;34(3):445-449. [DOI] [PubMed] [Google Scholar]
- 18. Health Resources & Services Administration. Defining rural population–2018. https://www.hrsa.gov/rural-health/about-us/definition. Accessed June 28, 2019.
- 19. Beck RW, Riddlesworth TD, Ruedy K, et al. Continuous glucose monitoring versus usual care in patients with type 2 diabetes receiving multiple daily insulin injections: a randomized trial. Ann Intern Med. 2017;167(6):365-374. [DOI] [PubMed] [Google Scholar]
- 20. Vigersky RA, Fonda SJ, Chellappa M, Walker MS, Ehrhardt NM. Short- and long-term effects of real-time continuous glucose monitoring in patients with type 2 diabetes. Diabetes Care. 2012;35(1):35-38. [DOI] [PMC free article] [PubMed] [Google Scholar]


