Abstract
To date, few programs that integrate traditional practices with evidence-based practices have been developed, implemented, and evaluated with urban American Indians/Alaska Natives (AI/ANs) using a strong research design. The current study recruited urban AI/AN teens across northern, central, and southern California during 2014–2017 to participate in a randomized controlled trial testing two cultural interventions that addressed alcohol and other drug (AOD) use. Adolescents were 14–18 years old (inclusive), and either verbally self-identified as AI/AN or were identified as AI/AN by a parent or community member. We tested the added benefit of MICUNAY (Motivational Interviewing and Culture for Urban Native American Youth) to a CWG (Community Wellness Gathering). MICUNAY was a group intervention with three workshops that integrated traditional practices with motivational interviewing. CWGs were cultural events held monthly in each city. AI/AN urban adolescents (N = 185) completed a baseline survey, were randomized to MICUNAY + CWG or CWG only, and then completed a three- and six-month follow-up. We compared outcomes on AOD use, spirituality, and cultural identification. Overall, AOD use remained stable over the course of the study, and we did not find significant differences between these two groups over time. It may be that connecting urban AI/AN adolescents to culturally centered activities and resources is protective, which has been shown in other work with this population. Given that little work has been conducted in this area, longer term studies of AOD interventions with urban AI/AN youth throughout the U.S. are suggested to test the potential benefits of culturally centered interventions.
Keywords: American Indian/Alaska Native, Adolescents, Intervention, Culture, Motivational interviewing, Traditional practices
1. Introduction
The American Indian/Alaska Native (AI/AN) population suffers from numerous health disparities, including high rates of substance use and poor mental and physical health (Grant et al., 2017; Mack, Jones, & Ballesteros, 2017; Trout, Kramer, & Fischer, 2018; Warne & Frizzell, 2014). These health disparities are historically rooted in European contact, forced relocation, and cultural genocide, leading to widespread traumatic experiences and unresolved grief across generations (Brave Heart & DeBruyn, 1998). In their seminal paper, Brave Heart and DeBruyn (1998) describe events and policies put in place over decades that have contributed to historical trauma among AI/ANs, including the boarding school era and federal policies focused on assimilation and destruction of AI/AN culture. The Relocation Act of 1956 (Burt, 1986) is one U.S. law that many believe contributed to numerous health disparities among urban AI/ANs. This Act financed the relocation of individual AIs and AI families to job training centers in designated U.S. cities. Instead of creating greater economic stability, large numbers of AIs who moved to urban areas became unemployed, homeless, and disconnected from their community-based support networks ( Myhra, 2011; Myhra & Wieling, 2014). Recent research has only just begun to document the deleterious effects of these events (Brockie, Heinzelmann, & Gill, 2013; Jernigan et al., 2015; Mullett, 2015; Paradies, 2016; Stoner et al., 2015).
According to the 2010 U.S. Census, approximately 70% of AI/ANs now live in urban areas (Norris, Vines, & Hoeffel, 2012). The urban environment poses many challenges for AI/ANs (Brown, Dickerson, & D’Amico, 2016; Brown et al., In press; Castor et al., 2006; Dickerson et al., 2019). Traditionally, AI/ANs lived in extended family and community networks, socially connected through common cultural practices. Although some urban AI/AN communities are closely connected, many urban areas are geographically and socially fragmented (Jones & Galliher, 2015; Kennedy et al., 2018). As a result, urban AI/ANs often feel ostracized, socially disconnected, confused about their identity, and victimized (Brodish et al., 2011; Tobler et al., 2013). Our work with urban AI/AN adolescents has shown that many AI/AN teens experience stress related to identity in the form of both subtle (e.g., being asked whether one is a “real” Indian) and overt (e.g., being called a racist name like Squaw or Red Skin) discrimination (D’Amico et al., 2019; Dickerson et al., 2019). Among urban AI/ANs, programming that incorporates traditional practices, promotes community involvement, and encourages healthy notions of AI/AN identity may increase well-being and healthy behaviors by ameliorating stress linked to cultural identity and stigma, as well as increasing community connections (Brown et al., 2016; Dickerson, Brown, Johnson, Schweigman, & D’Amico, 2015; Jernigan, D’Amico, & Kaholokula, 2018; Venner et al., 2018). However, few evidence-based programs that integrate these cultural elements have been developed, implemented, and evaluated with urban AI/ANs using a strong research design (Dickerson & Johnson, 2012; Dickerson, Baldwin, et al., 2018; Native American Health Center, 2012). This research gap is particularly evident for urban AI/AN adolescents (Jernigan, D’Amico, Duran, & Buchwald, 2018). The current study describes a randomized controlled trial that tested two culturally appropriate interventions for urban AI/AN adolescents addressing alcohol and other drug (AOD) use.
We are part of a group of investigators funded by the National Institutes of Health (NIH) to conduct Intervention Research to Improve Native American Health (IRINAH) (Crump, Etz, Arroyo, Hemberger, & Srinivasan, 2017). Our work and the work of other IRINAH investigators has highlighted the importance of utilizing a community based participatory research (CBPR) approach when developing and implementing interventions with AI/ANs, and intervening at multiple levels to address disparities (Crump et al., 2017; Dickerson, Baldwin et al., 2018; Gittelsohn et al., 2018; Ivanich, Mousseau, Walls, Whitbeck, & Whitesell, 2020; Jernigan, D’Amico, Duran, & Buchwald, 2018; Jernigan, D’Amico, & Kaholokula, 2018; Stanley et al., 2018; Walters et al., 2018). Work with AI/AN communities has also shown the value of traditional healing and practices, as well as ensuring that programming is culturally centered ( Dickerson & Johnson, 2011; Freeman et al., 2016; Jernigan, D’Amico, Duran, & Buchwald, 2018; Jernigan, D’Amico, & Kaholokula, 2018; Kaholokula, Ing, Look, Delafield, & Sinclair, 2018; Moghaddam, Momper, & Fong, 2015; National Center of Urban Indian Health, 2015; Novins et al., 2012; Raghupathy & Forth, 2012; Walters et al., 2018). Utilizing CBPR methodologies can also create sustainable interventions that can be more easily disseminated and ultimately help to decrease health disparities among urban AI/ANs (Gittelsohn et al., 2018; Jernigan, D’Amico, & Kaholokula, 2018).
To date, there are very few AOD prevention/intervention programs for urban AI/AN teens that have been rigorously designed, address culture, and also integrate evidence-based practices (EBP), such as Cognitive Behavior Therapy (CBT) or Motivational Interviewing (MI). A systematic review in 2015 found only six studies of mental health and substance use interventions for Indigenous youth. Only two of these studies utilized a randomized controlled trial (RCT) research design (Antonio & Chung-Do, 2015). Both studies had very small samples: one had a sample size of 19 (Listug-Lunde, Vogeltanz-Holm, & Collins, 2013), and the other had a sample size of 56 (however, final outcome data were only available for 24 youth) (Woods & Jose, 2011). Only one study occurred in an urban setting. Investigators addressed depression in Māori and Pasifika youth by adapting a CBT program for middle school youth by working with mental health professionals from local Māori and Pasifika groups. Despite the small sample of 24, they found that depression scores were lower one year later for youth who participated in the intervention compared to the control group (Woods & Jose, 2011).
A 2017 review of culturally informed interventions for Indigenous adolescents ages 9–18 examined programming from 1988 to 2016 (Liddell & Burnette, 2017). Out of 148 articles obtained, only 14 articles met inclusion criteria of evaluating an intervention targeting AOD use focused on Indigenous youth in the United States; however, only 2 studies were: (1) with urban AI/AN teens, (2) integrated culture with an EBP, and (3) tested effects of intervention programming using an RCT. The first study, Living in 2 Worlds (L2W) is a culturally adapted program of the Keepin’ it REAL (kiR) program, which addresses substance use through a “refuse, explain, avoidance and leave” approach (Kulis, Dustman, Brown, & Martinez, 2013). In the RCT study (Kulis, Ayers, & Harthun, 2017), the authors compared 107 middle school students who received the original kiR (n = 22) to middle school students who received the adapted L2W (n = 85). They conducted a pre-test and a one month follow up that occurred after the last lesson was taught. Overall, they found that during this time, both groups increased their substance use, positive attitudes about drugs, and exposure to drugs over time; however, the L2W group only reported increases in marijuana use frequency whereas the kiR group reported increases in alcohol, marijuana, and cigarette use frequency ( Kulis et al., 2017).
A second RCT with middle school adolescents compared a culturally appropriate school-based intervention, Intertribal Talking Circle (ITC), to Drug Abuse Resistance Education (DARE). They recruited 100 Keetoowah-Cherokee 6th grade students (Lowe, Liang, Henson, & Riggs, 2016). The ITC intervention was based upon the Native Self Reliance model and focused on three areas: being responsible, disciplined, and confident. They examined changes using the Global Assessment of Individual Needs-Quick Scale over a one year period, and found that adolescents in the ITC program decreased their scores on the general life problem index, the substance problem scale, and the total symptoms severity scale across all time points compared to teens in the DARE group (Lowe et al., 2016). Findings highlight the importance of culturally grounded programming for AI/AN.
There was one other large RCT (N = 1396) that provided an intervention to Native American youth in 27 tribal and public schools from 10 reservations in North and South Dakota, Idaho, Montana, and Oklahoma (Schinke, Tepavac, & Cole, 2000). It is important to describe this study even though youth were from reservations instead of urban areas, as it is one of the few RCT studies that culturally adapted an evidence based intervention, Life Skills Training (LST), focused on cognitive and behavioral skills for substance abuse prevention (Botvin, Baker, Dusenbury, Tortu, & Botvin, 1990), and examined outcomes in the long-term. The authors tailored LST for the Native American youth in the reservation settings, teaching them skills to resist pressures to use AOD within Native society and in the dominant American society. Over the 3.5 year time period of the study, all youth increased their tobacco, alcohol, and marijuana use; however, rates of smokeless tobacco, alcohol, and marijuana use increased less for youth who received LST than for youth in the control group (Schinke et al., 2000).
In our review of this literature, we found only one additional RCT with urban AI/AN youth that integrated culture with an EBP. Of note, this study is the only one to date comparing two interventions that both incorporated culturally based approaches. One-on-one interventions were conducted with 69 youth age 13–20 who lived on or near eight Southwest California reservations served by the health clinic (Gilder et al., 2017). Although this sample was not all urban, some youth in the sample were living in urban areas. One intervention utilized MI, and the other intervention focused on psychoeducation. Of note, both interventions focused on youths’ experience of their family, friends and tribal members with alcohol. The counselor also explained that alcohol was never used in the culture prior to European contact, and discussed the strong tribal belief that intoxication excludes individuals from participating in cultural events. Thus, both interventions included cultural elements; however, the MI intervention integrated these cultural components with an EBP. Overall, regardless of which intervention they received, youth reduced their quantity and frequency of drinking and reported fewer problem behaviors. The authors suggest that no differences were found because both interventions addressed culture in their sessions; that is, they focused on the history of alcohol in these communities and how alcohol was not part of tribal culture in the past (Gilder et al., 2017).
In the current study, we conducted a RCT throughout California with urban AI/AN teens to address AOD use. Conducting RCTs with AI/ANs is often challenging as communities are close-knit, which can lead to intervention cross-contamination and difficulty in recruiting sufficient numbers for each condition. Furthermore, AI/AN communities are often concerned that randomization to treatment in RCTs does not provide benefits to the entire community, and thus are often perceived as unacceptable and unfair (Dickerson, Baldwin, et al., 2018). The design of the study was therefore informed by CBPR ( Jernigan, D’Amico, Duran, & Buchwald, 2018); thus, every adolescent in the RCT was randomized to receive some form of culturally appropriate programming - as requested by the community ( Dickerson et al., 2015). The goal of the study was to compare six-month outcomes for urban AI/AN teens who only received a culturally appropriate community event to those who received this community event plus three AOD workshops that integrated the evidence-based practice of MI with traditional AI/AN practices.
2. Materials and methods
2.1. Procedure
From 2014 to 2017, we worked closely with our community partner, Sacred Path Indigenous Wellness Center (SPIWC), to recruit AI/AN adolescents from large cities in northern, central and southern California. SPIWC is led by Dr. Carrie Johnson (Wahpeton Dakota), and is a non-profit organization that provides AOD and mental health services for AI/ANs, and consultation to help ensure that research and services are provided in a culturally appropriate manner. All procedures were approved by the institution’s review board and by the communities with whom we collaborated on the project. We also had a community Elder Advisory Board and a Teen Advisory Board, and we collaborated with AI/AN community organizations in every city to determine how to best engage the community in our project and recruit AI/AN families and adolescents. For example, each recruitment flyer used images relevant to the particular community (e.g., in one community, we used a picture of a known landmark that community members recognized in a park where culturally-related events were often held), and we worked closely with leaders in each community to provide events tailored to the needs of that particular community ( Jernigan, D’Amico, & Kaholokula, 2018). We held information meetings, attended Pow Wows and other community events, posted information on AI/AN email listservs and on Facebook, and hired AI/AN recruiters in each community to discuss the project with AI/AN families. Interested parents and adolescents could call our 1–800 project number or provide contact information to one of our recruiters at these events and be called by our staff. Eligibility criteria required that adolescents be 14–18 years old (inclusive), and either verbally self-identify as AI/AN or be identified as AI/AN by a parent or community member. Eligible adolescents were then scheduled to complete a baseline survey at a time and place that was convenient to them. They were paid $25. At that time, teens were randomly assigned by block randomization to either Community Wellness Gathering (CWG) only or MICUNAY + CWG. Teens had a three-month period to complete all three MICUNAY workshops, which rotated weekly, and to complete one CWG, which occurred once per month. After completion of MICUNAY and/or the CWG, teens then completed a three and six month follow up interview, for which they were paid $50 and $75, respectively. We also reimbursed for transportation to the MICUNAY workshops, and adolescents were provided a $5 gift card or free movie pass at each workshop.
Over the course of the project, 334 adolescents provided consent to contact. Forty-one of these youth were not eligible, 9 declined participation, and 69 were not able to be contacted within the field period. Thus, 215 adolescents screened in as eligible to be in the project (see Fig. 1). Of these adolescents, 30 did not complete their baseline assessment within the field period or hand unreliable contact information. This yielded a final enrolled sample of 185 adolescents who completed a baseline survey.
Fig. 1.
Consort diagram.
2.2. Intervention overview
We worked closely with communities and our Elder Advisory Board over the first year of the project to design the two interventions, and determine how to best implement the RCT in these urban communities. Intervening at the community level, we offered monthly CWGs for all adolescents at each study site, with a focus on traditional practices and living a healthy life, which included making healthy choices around AOD use. Half of the youth were also randomized to attend three 2-h group workshops that addressed traditional practices, including beading, prayer, and Native cooking. Upon completion of the six-month follow up, every adolescent in the CWG only group was offered an opportunity to participate in the three MICUNAY workshops.
2.2.1. Community wellness gatherings
Every youth that participated in the study was assigned to attend a CWG. These two-hour events were held monthly in each community, typically in the evening. Many communities often had these types of gatherings already scheduled. When this occurred, we would provide the food, and compensate the people who conducted the gathering (e.g., the Elder who conducted the beading workshop). When a gathering was not already scheduled, we worked with each community to have someone from the community conduct the CWG. Some examples of CWGs included beading workshops, hoop dancing, drumming and singing, and storytelling. Each CWG began with a prayer and discussion of the importance of making healthy choices. CWGs also focused on the importance of traditional practices and discussed ways that youth could connect with their culture.
2.2.2. MICUNAY
We developed MICUNAY (Motivational Interviewing and Culture for Urban Native American Youth) to address the gap in culturally-appropriate evidence-based interventions targeting AOD use among urban AI/AN teens (Dickerson et al., 2015). Our team was one of the first groups funded as part of the IRINAH initiative, and we are the only research group to date to conduct culturally centered prevention intervention work with AI/AN adolescents in urban settings (Dickerson, Moore, et al., 2018). To help design MICUNAY, we conducted qualitative research with AI/AN adolescents, parents, providers, and Elders in two large urban cities in California (Dickerson et al., 2015). Findings highlighted that urban AI/AN adolescents struggle with cultural disconnection, mixed identity, and racial-ethnic discrimination. We also found that cultural identity and participation in traditional practices is protective for AI/AN youth (Brown et al., 2016; Brown et al., In press; Dickerson et al., 2015). In addition to utilizing traditional practices, our work ( Dickerson et al., 2015; Dickerson, Moore, et al., 2018) and the work of others has emphasized the usefulness of MI with AI/ANs (Tomlin, Walker, Grover, Arquette, & Stewart, 2014; Venner et al., 2007). MI is one of the most widely-used EBPs for AOD use in the U.S (SAMHSA National Registry of Evidence-based Programs and Practices (NREPP), 2014). Many studies have shown the acceptability (Feldstein Ewing, Wray, Mead, & Adams, 2012; Gilder et al., 2011; Venner et al., 2007) and efficacy of MI with non-white youth ( D’Amico et al., 2018; Gil, Wagner, & Tubman, 2004; Gilder et al., 2011; Naar-King et al., 2010; Schmiege, Broaddus, Levin, & Bryan, 2009).
Half of the teens in the study were randomized to three 2-h MICUNAY workshops in addition to the CWG to test the added benefit of the workshops. One hour of the workshop focused on AOD use and making healthy choices using MI, and 1 h focused on a traditional Native American practice. MICUNAY workshop content was developed with extensive input from the community ( Dickerson et al., 2015), and the AOD information was taken, in part, from previous MI intervention development and evaluation work with adolescents ( D’Amico et al., 2015; D’Amico, Hunter, Miles, Ewing, & Osilla, 2013; D’Amico et al., 2018). One of the unique elements of the MICUNAY workshops was to ensure that the MI component and traditional practice component connected to ensure cohesiveness, deliverability and cultural relevance (Dickerson et al., 2015). For each traditional component, we provided guidelines for the facilitators on the overarching topic, but encouraged them to discuss the traditional practice in a way that fit best for their community. Based on our focus groups ( Brown et al., 2016), and given that these urban AI/AN adolescents came from over 60 tribes (Brown et al., In press), the focus of the cultural component of the workshop was on “pan-Indian” identity (being AI/AN in general) while empowering youth to learn about their own tribal-specific roots (Dickerson et al., 2015). Workshops were tailored to each participant’s experience and cultural background so that all felt welcome (Jernigan, D’Amico, Duran, & Buchwald, 2018).
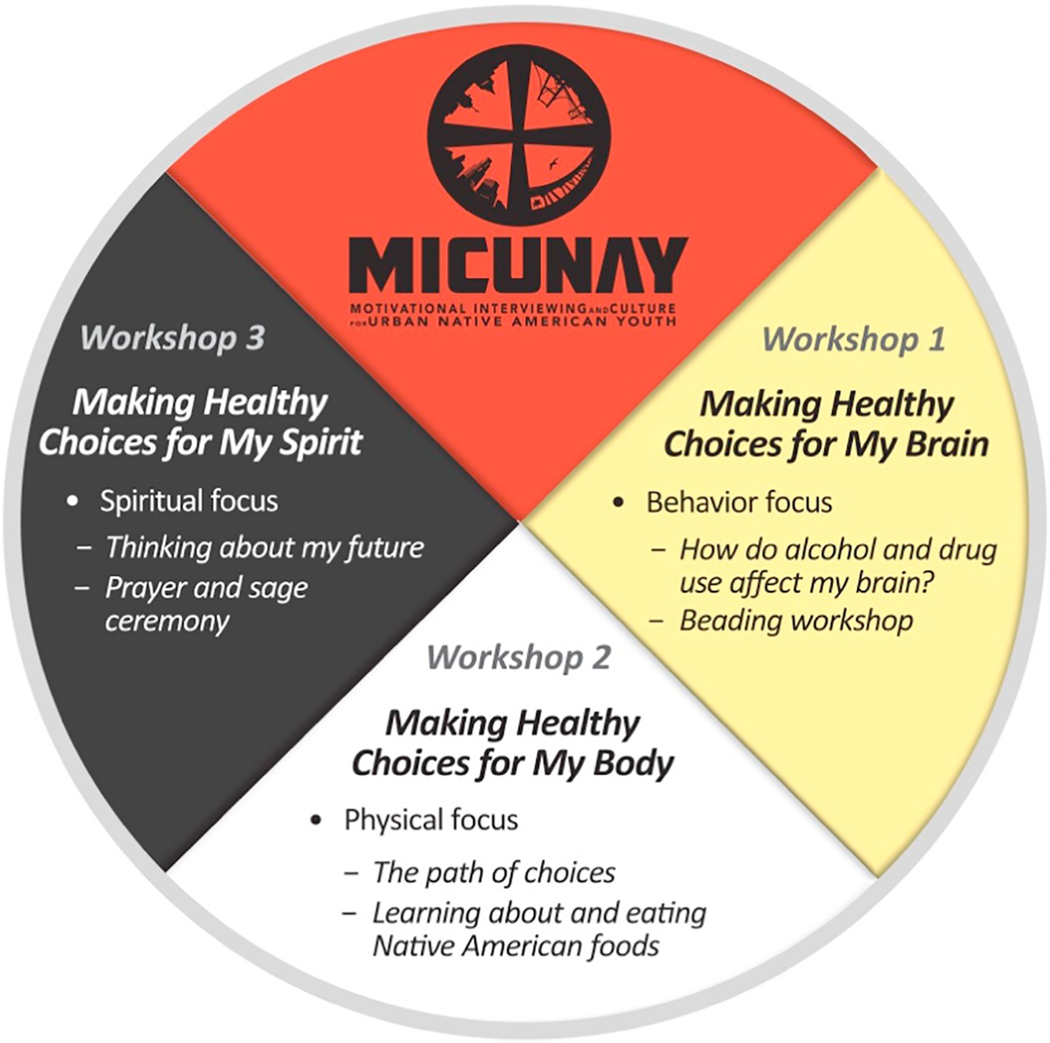
The cultural component of every session began with a discussion of the Medicine Wheel. As there are many versions of the Medicine Wheel, facilitators were encouraged to discuss the Medicine Wheel in ways that were most locally appropriate. Each workshop addressed a different aspect of the Medicine Wheel (Fig. 2). Every workshop was interactive and delivered using MI strategies, such as open-ended questions and reflections throughout both the cultural and MI portions of the session (see Table 1 for components in each session). Session 1 addressed “Making Healthy Choices for My Brain,” and started with a beading workshop for 1 h, after which youth could continue beading during the discussion of how AOD use can affect the brain. This interactive discussion encouraged teens to think about how AOD use may affect their brain and behavior, how and whether the brain recovers from AOD use, and how thinking about this information could affect their own personal use of substances. Session 2 addressed “Making Healthy Choices for my Body” which focused first on discussing the pros and cons of AOD use, how AOD use can affect one’s life, and alternative life paths to AOD use. The facilitator also used willingness and confidence rulers to discuss with teens where they were at in terms of potentially changing their AOD use, and how confident they were in making a change if they were ready. The second part of Session 2 addressed healthy food choices, focusing on Native American foods and traditions. Facilitators were instructed to discuss topics that were locally appropriate and interesting to youth. Some example topics were discussions of hunting and fishing, watching portions of the documentary, Good Meat, origins of the bow and arrow, and utilizing local tools and ingredients to make recipes, such as Three Sister Stew (https://en.wikibooks.org/wiki/Cookbook:Three_Sisters_Stew). Teens then had an opportunity to taste different foods, such as buffalo stew, grilled salmon, acorn squash, and Three Sister Stew. Session 3 addressed “Making Healthy Choices for My Spirit,” which first focused on different risky situations that may occur because of AOD use, as well as ways to make healthy life choices to avoid these risks. Teens were encouraged to discuss the pros and cons of substance use with two specific examples: impaired driving and having sex without a condom. Discussion revolved around how to make a healthy choice in these situations by planning ahead. Based on the strategies discussed, the facilitator then used the willingness and confidence rulers to help teens evaluate whether they felt that they could use these strategies to make a change if they were ready. The second part of Session 3 addressed spiritual life and ways of praying. Facilitators could use a video called, “Picking sage and great advice from an Elder” (www.youtube.com/watch?v=zzysDb4pVco) to generate discussion, or discuss local traditions for praying.
Fig. 2.
MICUNAY medicine wheel1.
Note: 1Originally published in Dickerson, D. L., Brown, R. A., Johnson, C. L., Schweigman, K., & D’Amico, E. J. (2015). Integrating motivational interviewing and traditional practices to address alcohol and drug use among urban American Indian/Alaska Native youth. Journal of Substance Abuse Treatment, 65, 26–35. PMCID: PMC4732924.
Table 1.
Overarching components of each MICUNAY workshop.
| Workshop 1 | Workshop 2 | Workshop 3 | |
|---|---|---|---|
| Introduction, opening prayer, and purpose of group | x | x | x |
| Discussion of medicine wheel | x | x | x |
| Beading | x | ||
| Native cooking | x | ||
| Prayer | x | ||
| Discussion of how AOD affects the brain and whether our brain recovers | x | ||
| Memory game | x | ||
| Discussion of personal AOD use and potential changes | x | ||
| Pros and cons of AOD use | x | x | |
| The path of choices for AOD use versus healthy behavior | x | ||
| Willingness and confidence rulers | x | x | |
| Discussion of how AOD use might affect choices using two examples: Driving under the influence and risky sexual behavior | x | ||
| Discussion of ways to think ahead and plan for risky situations | x | ||
Note: Each workshop was interactive and delivered using motivational interviewing. Facilitators focused on asking open ended questions, providing reflections, and summarizing throughout the session. Some of the alcohol and other drug curricula is available on www.groupmiforteens.org.
2.3. Measures
2.3.1. Demographics
Initially, adolescents had to either verbally self-identify as AI/AN or be identified as AI/AN by a parent or community member to participate in the project ( D’Amico et al., 2019). In a subsequent self-report survey using categories established by NIH, participants checked “all that apply” for the following categories: AI/AN, Hispanic or Latino/Latina, Asian or Asian American, Native Hawaiian or Pacific Islander, black or African American, white or Caucasian, and other. Adolescents reported their age, gender, and level of education for each parent or guardian.
2.3.2. AOD use
We assessed substance use with the well-established Monitoring the Future items (Miech, Johnston, O’Malley, Bachman, & Schulenberg, 2016). Adolescents reported past 3-month use for cigarettes, alcohol, and marijuana. For this study, we created a dichotomous indicator of whether adolescents reported any use of these substances. This is because AOD use rates are typically lower in younger adolescents, leading to highly skewed distributions in continuous variables (D’Amico et al., 2016).
2.3.3. Consequences of alcohol and marijuana use
Adolescents reported on the consequences they had experienced in past three months. Consequences are based on DSM-IV criteria with 7 items for alcohol (e.g., missed school or work) and 5 for marijuana (e.g., had difficulty concentrating) ( D’Amico et al., 2016). Both scales have been used extensively with adolescents and were reliable with teens in this study (α = 0.77 for marijuana and α = 0.94 for alcohol). For this analysis we created dichotomous indicators of whether adolescents reported any consequences from alcohol or any consequences from marijuana.
2.3.4. Intentions to use AOD
Three separate items assessed whether adolescents believed they would drink any alcohol, use any marijuana, or smoke a cigarette in the next six months (1=“definitely yes” to 4=“definitely no”) (Ellickson, McCaffrey, Ghosh-Dastidar, & Longshore, 2003).
Resistance self-efficacy (RSE)
( D’Amico et al., 2012) for alcohol was defined as the average of four items rated from “I would definitely use” to “I would definitely not use” based on different situations (e.g., if my best friend were using; you were bored at party; your friend gives you a drink). RSE ranged from 1 to 4; higher scores indicated greater RSE (α = 0.94).
2.3.5. Peer influence
Three separate items assessed how often adolescents spend time around teens who drink, use marijuana, or smoke cigarettes (1 = “never” to 4 = “often”) ( D’Amico, Miles, Stern, & Meredith, 2008).
2.3.6. Intentions to participate in traditional practices
Adolescents reported how likely they were to participate in >20 different traditional practices (e.g., going to Pow Wows, prayer, playing Native hand or stick games) in the next six months (1=“definitely yes” to 4=“definitely no”). Items were based upon extensive research conducted with AI/AN adolescents, parents, and community partners (α = 0.97) (Kaufman et al., 2014).
2.3.7. Cultural pride and belonging
We assessed adolescents’ AI/AN cultural pride and sense of belonging with the Multigroup Ethnic Identity Measure (MEIM), which has twelve items (α = 0.94). Respondents are asked the degree to which they agree with statements such as, “I have a clear sense of my ethnic background and what it means to me” on a scale from 1 = “strongly disagree” to 5 = “strongly agree” (Phinney & Ong, 2007; Ponterotto, Gretchen, Utsey, Stracuzzi, & Saya, 2003). Given that our prior focus group work (Brown et al., 2016) indicated that many adolescents were of mixed ethnicity, and our focus was on AI/AN identity, we modified these items to focus on AI/AN heritage (e.g., “I have clear sense of my AI/AN identity and what it means to me”).
2.3.8. Spirituality/happiness
Spirituality and happiness were measured using a subset of ten items from the 12-item Functional Assessment of Chronic Illness Therapy-Fatigue-Spiritual Questions instrument, or FACIT-SP 12 (Peterman, Fitchet, Brady, Hernandez, & Cella, 2002). Adolescents reported agreement with statements such as “I find comfort in my faith or spiritual beliefs” and “I feel a sense of harmony within myself.” Two items that referred specifically to chronic illness were removed from the scale as they were not relevant for this study. Response options, which ranged from 1=“not at all” to 5=“very much,” were averaged (α = 0.83), with negative statements reversed such that higher scores indicated greater spirituality and happiness.
3. Primary analysis
We first tested whether teens in the MICUNAY + CWG and CWG only groups differed at baseline with Fisher’s exact tests for categorical characteristics and t-tests for continuous characteristics. We used intention-to-treat analyses to assess all intervention effects. Intervention efficacy was estimated with a series of longitudinal linear and logistic regression models. The models included an indicator for being randomized to the intervention group and the following covariates: baseline value of the outcome and demographics (age, gender, and race/ethnicity [self-identification as Hispanic, multi-racial, or other vs. AI/AN]). Because follow-up surveys were administered over a somewhat wide timespan from the intended 3-month and 6-month time points (the interquartile range was 80–158 days for administration of the 3-month survey and 170–243 days for the 6-month survey), models additionally adjust for the number of days between the end of the treatment period and the follow-up survey date, as well as which follow-up survey the response is from. Because each adolescent contributed two records (3- and 6-month follow up) to this analysis, standard errors were adjusted for clustering on individuals with SAS Proc SURVEYREG and SURVEYLOGISTIC. Among the intervention group only, a similar set of regressions was fit to estimate the effect of each intervention session.
3.1. Missing data
All analyses of responses to follow-up surveys were based on imputed data. SAS Proc MI was used to generate 40 imputed datasets for all variables used in the analysis at all time points, including for completely missing follow-up surveys. Imputed values were truncated to their original minima and maxima. SAS Proc MIANALYZE was used post-analysis to compile results across the 40 imputed datasets.
3.2. Descriptive statistics
Means at follow-up were calculated as the mean of the means from each of the 40 imputed data sets. Standard deviations were calculated using standard rules for multiple imputation (Rubin, 2004), which estimates the overall variance as the average within-imputation variance plus the product of the between-imputation variance and 1 + (1/m) where m = the number of imputations (40).
3.3. Loss to follow-up
Although we imputed data for those lost to follow-up, we also assessed the degree to which those lost to follow-up were different from those for whom we had complete data. Differential loss to follow-up was assessed by comparing adolescents who responded to either the 3- or 6-month follow-up survey to adolescents who did not respond to either survey on a variety of baseline characteristics. Statistical significance was assessed with t-tests for continuous characteristics or Fisher’s exact tests for binary characteristics. t-Tests and Fisher’s exact tests were similarly used to compare means and percentages reported for the control (CWG only) group versus the intervention (MICUNAY + CWG) group at baseline.
4. Results
4.1. Fidelity and quality of MICUNAY sessions
Across the study, we had five different Native American facilitators deliver MICUNAY. One facilitator had a high school degree, one had an Associate degree in sociology and was a certified addictions counselor, two had a Bachelor’s degree, and one had a Master’s degree. The first author, a member of the Motivational Interviewing Network of Trainers (MINT), trained all facilitators in MI, and the second author, a leader in utilizing traditional healing practices to address substance use, conducted the training on traditional practices. Each facilitator was trained on the MICUNAY protocol through role playing with other project staff who pretended to be teens involved in the program. Facilitators needed to pass a final skills review before they could deliver MICUNAY in the field.
We digitally recorded all MICUNAY sessions. The first and second author listened to all MICUNAY sessions and provided weekly supervision; 20% of sessions were coded by a rater from the RAND/UCLA team for fidelity to MI and to the protocol using an adherence checklist (D’Amico et al., 2013), and most sessions (60%) were coded by two raters who were part of the RAND/UCLA team. We coded fidelity to MI using the Motivational Interviewing Treatment Integrity scale (MITI) 3.1.1 ()(Moyers, Martin, Miller, & Ernst, 2010).
Fidelity to the MICUNAY workshop protocol was high across workshops with facilitators addressing the main topics in each workshop (e.g., confidentiality, pros and cons of use, how AOD use affects the brain). Average global scores on the MITI for the workshops (evocation, collaboration, autonomy/support, direction, and empathy) ranged from 3.2 to 4.8, with an overall average of 3.5 (3.5 is beginning proficiency and 4 is competent), and the percent of complex reflections was 42% (40% is beginning proficiency; 50% is competent).
At the three month follow-up, adolescents reported their satisfaction and perceived quality (Larsen, Atkinson, Hargreaves, & Nguyen, 1979) of the MICUNAY workshops. Adolescents also reported on therapeutic alliance (e.g., We worked together to set goals) (Hatcher & Gillaspy, 2006), and on session style (e.g., The group leader valued my opinion) ( D’Amico et al., 2013). The quality item ranged from 1 (poor) to 4 (excellent); all other items were rated on a 1 to 5 scale from strongly disagree (1) to strongly agree (5). Table 2 shows that 80% of adolescents were satisfied with the MICUNAY workshops, and 85% thought the quality of the workshops was good or excellent. Eighty-four percent of adolescents felt that the group leader was helpful, 80% said the group leader helped them believe they could change and improve their life, and 86% agreed that the facilitator valued their opinion. Regarding activities, 75% thought they were helpful, 77% said they learned more about their culture, and 73% felt that the cultural activities in MICUNAY could help them lead a healthier life.
Table 2.
Adolescent quality and satisfaction ratings for the MICUNAY intervention.
| % of adolescents | |
|---|---|
| Quality | |
| How would rate the quality of the groups? | 85% |
| Satisfaction | |
| Generally, I am satisfied with the groups I attended. | 80% |
| Therapeutic alliance | |
| The group leader and I respected each other. | 80% |
| The group leader respected my background. | 86% |
| We worked together to set goals. | 62% |
| I feel that the things I did in the group will help me to make the changes that I want. | 73% |
| The group leader helped me believe that I could change and improve my life. | 80% |
| The group leader was helpful. | 84% |
| Session style | |
| The group leader respected where I was at with my AOD use and that any change was up to me. | 76% |
| The group leader valued my opinion. | 86% |
| I feel that the things I did in the group will help me to make the changers that I want. | 72% |
| I learned more about AI/AN culture. | 77% |
| The different activities that we did in group were helpful. | 75% |
| Participating in the MICUNAY cultural activities can help me lead a healthier life. | 73% |
Note:
For quality, percent reflects adolescents who reported “excellent” or “good”; for satisfaction, therapeutic alliance and session style, percent reflects those who reported “strongly agree” or “agree”.
Overall, MITI scores and adolescents’ ratings indicate that the MICUNAY workshops were delivered with fidelity to MI and the protocol. Adolescents felt respected and listened to during the workshops, and agreed that facilitators valued their opinions and background.
4.2. Baseline differences and attrition
We provide demographic characteristics and baseline outcomes by group in Table 3. There were 115 adolescents in the MICUNAY + CWG group and 70 adolescents in the CWG-only group. As noted, to be part of the project, all teens had to either verbally self-identify as AI/AN or be identified as AI/AN by a parent or community member. Adolescents also self-reported race/ethnicity on baseline surveys, marking “all that apply.” Based on this self-report, 81% of the overall sample identified as AI/AN (35 youth did not mark AI/AN on the survey (D’Amico et al., 2019)), 45% as Hispanic/Latino, and 17% White/Caucasian. Female participants made up 51% of the sample; 14- and 15-year-olds comprised 49% of the sample. In the 3 months prior to baseline, 15% of participants reported tobacco use, 23% reported drinking alcohol, 28% used marijuana, and 13% had 5 or more drinks in a row. Sixteen percent of the sample reported experiencing consequences from drinking alcohol in the past 3 months, and 15% reported experiencing consequences from marijuana use.
Table 3.
Baseline characteristics stratified by group.
| CWG (n = 70) | MICUNAY + CWG (n = 115) | ||
|---|---|---|---|
| Demographics | N (%) | N (%) | P-valuea |
| Age | 0.07 | ||
| 14 | 19 (27%) | 33(29%) | |
| 15 | 13 (19%) | 25 (22%) | |
| 16 | 24 (34%) | 21 (18%) | |
| 17 | 11 (16%) | 20 (17%) | |
| 18 | 3 (4%) | 16 (14%) | |
| Female | 48 (69%) | 47 (41%) | <0.001 |
| Race/ethnicityb | |||
| Hispanic/Latino | 28 (40%) | 55 (48%) | 0.36 |
| AI/AN | 59 (84%) | 91 (79%) | 0.44 |
| Asian/Asian American/Pacific Islander | 3 (4%) | 5 (4%) | 1.00 |
| Black/African American | 11 (16%) | 10 (9%) | 0.16 |
| White/Caucasian | 14 (20%) | 18 (16%) | 0.55 |
| Other | 1 (1%) | 7 (6%) | 0.26 |
| Mother’s education ≥ high school graduate | 49 (84%) | 71 (77%) | 0.30 |
| Father’s education ≥ high school graduate | 39 (80%) | 55 (70%) | 0.30 |
| Outcomes measured at baseline | Mean (SD) or N (%) | Mean (SD) or N (%) | P-valuea |
| Intentions | |||
| Intentions to drink any alcohol in next 6 months | 1.88 (0.82) | 1.66 (0.93) | 0.11 |
| Intentions to use any marijuana in next 6 months | 1.81 (1.05) | 1.71 (1.03) | 0.54 |
| Intentions to smoke a cigarette in next 6 months | 1.35 (0.75) | 1.26 (0.68) | 0.41 |
| Alcohol resistance self-efficacy1 | 3.18 (0.93) | 3.43 (0.81) | 0.06 |
| Peer influence1 | |||
| How often around teens smoking cigarettes | 1.71 (0.98) | 1.53 (0.93) | 0.21 |
| How often around teens drinking alcohol | 2.06 (1.02) | 1.83 (1.06) | 0.16 |
| How often around teens using marijuana | 2.43 (1.20) | 2.25 (1.18) | 0.31 |
| Cultural activities and cultural identity | |||
| Intentions to participate in cultural activities in next 6 months1 | 2.68 (0.83) | 2.63 (0.73) | 0.69 |
| Multigroup Ethnic Identity Measure (MEIM)2, c | 3.23 (0.95) | 3.39 (0.81) | 0.22 |
| Spirituality/happiness2 | 3.51 (0.78) | 3.71 (0.74) | 0.08 |
| Consequences of using alcohol and marijuana | |||
| Any consequences from drinking alcohol past 3 months | 14 (20%) | 15 (13%) | 0.22 |
| Any consequences from using marijuana past 3 months | 13 (19%) | 15 (13%) | 0.40 |
| Alcohol and marijuana use | |||
| Used tobacco in the past 3 months | 13 (19%) | 15 (13%) | 0.40 |
| Drank alcohol in the past 3 months | 19 (27%) | 24 (21%) | 0.37 |
| Had 5 or more drinks in a row in past 3 months | 11 (16%) | 13 (11%) | 0.50 |
| Used marijuana in the past 3 months | 22 (31%) | 30 (27%) | 0.50 |
This table reflects observed data without imputation. Percentages are calculated among non-missing values.
Scale is from 1 to 4.
Scale is from 1 to 5.
Fisher’s exact test for dichotomous or categorical characteristics; t-test for continuous characteristics.
All youth had to either verbally self-identify as AI/AN or be identified as AI/AN by a parent or community elder to be part of the project. They then completed a survey asking them to label their race/ethnicity. These numbers and percentages reflect what youth reported on the survey and can overlap if they identified more than one race/ethnicity. Thirty-five youth did not check AI/AN on the survey, although they identified as Native American to be in the study.
This scale measures ethnic identity and acculturation.
The only statistically significant difference between the two intervention groups at baseline was in terms of gender, where females made up 69% of the CWG only group and 41% of the MICUNAY + CWG group (p < 0.001). The MICUNAY + CWG group reported marginally more alcohol resistance self-efficacy (average score of 3.43) than the CWG group (average 3.18, p = 0.06), and also had a marginally higher score for the spirituality and happiness scale (3.71 vs. 3.51, p = 0.08).
Among the 185 adolescents who were included in the study, we were able to reach 76% for follow-up surveys at 3 months, and 82% at 6 months. Adolescents who completed at least one of the two follow-up surveys (89% of the 185) differed from those who did not on several baseline characteristics. On demographics, they were more likely to be female (54% vs. 29%, p = 0.04), younger (p = 0.01), and have mothers who were more likely to have a high school degree (84% vs. 40%, p < 0.001). For substance use outcomes, those who completed follow up were less likely to report tobacco use (12% vs. 43%, p = 0.001) or heavy drinking (11% vs. 29%, p = 0.04) at baseline. Those who completed a follow-up survey also had lower intentions to smoke marijuana (scale mean 1.67 vs. 2.29, p = 0.01), were with other teens smoking cigarettes less often (1.53 vs 2.14, p = 0.05), and scored lower on the spirituality/happiness scale (3.58 vs. 4.08, p = 0.004) at baseline. There was not a significant difference in follow-up rates between the intervention groups at 3 months (75.7% for MICUNAY +CWG vs. 75.7% for CWG only, p = 1.00 per Fisher’s exact test) or 6 months (82.6% MICUNAY +CWG vs. 80.0% CWG only, p = 0.70).
4.3. Outcomes
For outcomes, we found that the estimated added benefit of MICUNAY + CWG compared to CWG-only was small on the 16 outcomes we measured, with most effect sizes estimated to be <0.1 in magnitude (Table 4), and confidence intervals including both positive and negative values. The largest estimated effect size was −0.18 for consequences from using marijuana in the past 3 months, corresponding to an odds ratio of 0.72; however, the 95% confidence interval includes strong odds ratios in both directions (0.35–1.48, p = 0.37).
Table 4.
Effect of MICUNAY on 3-month and 6-month outcomesa.
| MICUNAY + CWG at 3 months | CWG at 3 months | MICUNAY + CWG at 6 months | CWG at 6 months | MICUNAY effectb | |||
|---|---|---|---|---|---|---|---|
| Continuous outcomes | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Coefficient (SE) | p-Value | Effect sizea |
| Intentions to drink any alcohol in next 6 months | 2.26 (1.27) | 2.22 (1.19) | 1.65 (0.96) | 1.84 (1.04) | 0.00 (0.12) | 0.99 | 0.00 |
| Intentions to use any marijuana in next 6 months | 1.97 (1.21) | 2.02 (1.15) | 1.92 (1.15) | 2.03 (1.14) | −0.05 (0.13) | 0.71 | −0.04 |
| Intentions to smoke a cigarette in next 6 months | 1.30 (0.71) | 1.30 (0.81) | 1.66 (1.14) | 1.77 (1.23) | −0.06 (0.11) | 0.59 | −0.06 |
| Alcohol resistance self-efficacy | 2.82 (1.21) | 2.78 (1.15) | 2.95 (1.09) | 3.00 (1.06) | −0.01 (0.13) | 0.93 | −0.01 |
| How often around teens smoking cigarettes | 1.52 (0.84) | 1.49 (0.96) | 1.54 (0.83) | 1.53 (0.93) | 0.07 (0.11) | 0.53 | 0.08 |
| How often around teens drinking alcohol | 1.78 (0.95) | 1.77 (1.05) | 1.76 (0.99) | 1.76 (0.94) | 0.11 (0.12) | 0.36 | 0.11 |
| How often around teens using marijuana | 2.42 (1.20) | 2.45 (1.29) | 2.04 (1.18) | 2.14 (1.18) | 0.09 (0.14) | 0.51 | 0.07 |
| Intentions to participate in cultural activities in next 6 months | 2.14 (0.94) | 2.29 (1.00) | 2.68 (0.89) | 2.71 (0.96) | 0.03 (0.11) | 0.80 | 0.03 |
| Multigroup Ethnic Identity Measure (MEIM) | 3.38 (1.08) | 3.36 (1.04) | 3.39 (1.14) | 3.11 (1.13) | 0.16 (0.13) | 0.21 | 0.15 |
| Spirituality/happiness | 3.41 (1.17) | 3.24 (1.18) | 3.29 (1.29) | 3.12 (1.24) | 0.13 (0.16) | 0.42 | 0.11 |
| Dichotomous outcomes | % | % | % | % | Odds ratio (CI) | p-Value | Effect sizec |
| Any consequences from drinking alcohol past 3 months | 35 | 31 | 32 | 33 | 1.15 (0.61–2.18) | 0.66 | 0.08 |
| Any consequences from using marijuana past 3 months | 11 | 16 | 30 | 33 | 0.72 (0.35–1.48) | 0.37 | −0.18 |
| Used tobacco in the past 3 months | 19 | 18 | 33 | 33 | 1.24 (0.57–2.70) | 0.59 | 0.12 |
| Drank alcohol in the past 3 months | 46 | 44 | 29 | 31 | 1.17 (0.63–2.19) | 0.61 | 0.09 |
| Had 5 or more drinks in a row in past 3 months | 32 | 29 | 24 | 25 | 1.01 (0.48–2.12) | 0.97 | 0.01 |
| Used marijuana in the past 3 months | 36 | 40 | 28 | 31 | 1.02 (0.50–2.10) | 0.96 | 0.01 |
All results in table account for missing data using multiple imputation methods.
Follow-up outcomes at 3- and 6-months were analyzed together. Regression models include records for each of the two follow-ups per participant. Models account for clustering of responses within individual and adjust for baseline values of the outcome, race/ethnicity, age, gender, which survey (3-month or 6-month) the response came from, and time elapsed between the end of treatment and the follow-up survey response.
For continuous outcomes, effect size is the coefficient divided by the standard deviation of the outcome for combined follow-up data. For dichotomous outcomes, the effect size is the log of the odds ratio divided by 1.81.
Rates of use for the overall sample remained fairly stable over time, with 23% of the sample reporting alcohol use in the past 3 months at baseline, and 30% of the sample reporting use at 6 months (Table 5). Similarly, for marijuana, 28% of the sample reported use in the past three months at baseline, and 29% reported use in the past three months at the six month follow up. Intentions to drink and use marijuana were also stable for the overall sample over the course of the study, as was the time that teens spent with peers who used alcohol, tobacco, and marijuana. Of note, tobacco use for the overall sample appeared to increase over time, as did the number of teens reporting consequences from drinking or marijuana (Table 5).
Table 5.
Means and standard deviations for outcomes for the whole sample.
| Baseline | 3 months | 6 months | |
|---|---|---|---|
| Continuous outcomes | Mean (SD) | Mean (SD) | Mean (SD) |
| Intentions to drink any alcohol in next 6 months | 1.75 (0.89) | 2.25 (1.24) | 1.72 (0.99) |
| Intentions to use any marijuana in next 6 months | 1.74 (1.04) | 1.99 (1.18) | 1.96 (1.15) |
| Intentions to smoke a cigarette in next 6 months | 1.30 (0.70) | 1.30 (0.75) | 1.70 (1.17) |
| Alcohol resistance self-efficacy | 3.33 (0.86) | 2.81 (1.18) | 2.97 (1.08) |
| How often around teens smoking cigarettes | 1.60 (0.95) | 1.51 (0.89) | 1.54 (0.86) |
| How often around teens drinking alcohol | 1.92 (1.05) | 1.77 (0.98) | 1.76 (0.97) |
| How often around teens using marijuana | 2.32 (1.19) | 2.43 (1.23) | 2.08 (1.18) |
| Intentions to participate in cultural activities in next 6 months | 2.65 (0.77) | 2.19 (0.96) | 2.69 (0.91) |
| Multigroup Ethnic Identity Measure (MEIM) | 3.33 (0.87) | 3.37 (1.07) | 3.28 (1.14) |
| Spirituality/happiness | 3.64 (0.76) | 3.34 (1.18) | 3.23 (1.27) |
| Dichotomous outcomes | N (%) | N (%) | N (%) |
| Any consequences from drinking alcohol past 3 months | 29(16) | 63 (34) | 59 (32) |
| Any consequences from using marijuana past 3 months | 28 (15) | 24 (13) | 57 (31) |
| Used tobacco in the past 3 months | 28 (15) | 33 (18) | 61 (33) |
| Drank alcohol in the past 3 months | 43 (23) | 83 (45) | 56 (30) |
| Had 5 or more drinks in a row in past 3 months | 24 (13) | 57 (31) | 44 (24) |
| Used marijuana in the past 3 months | 52 (28) | 70 (38) | 54 (29) |
Note: Ns are approximate, based on average of 40 imputed datasets.
Among those who were randomized to the MICUNAY + CWG group, 21 (18%) attended no workshops, 17 (15%) attended one workshop, 11 (10%) attended two workshops, and 66 (57%) attended all three MICUNAY workshops. The effect of each additional session of MICUNAY attended in this group was small, with an estimated effect size of about 0.15 or less in magnitude for each outcome (Table 6). Three outcomes had moderately sized associations and marginal p- values: intentions to drink alcohol, alcohol resistance self-efficacy, and intentions to participate in cultural activities. For example, for each MICUNAY session attended, the average alcohol resistance self-efficacy response was estimated to be 0.19 higher, with an effect size of 0.17 and a p-value of 0.04. However, the confidence interval for this effect is large, and after adjusting for performing tests on all 16 outcomes, the Bonferroni-adjusted p-value was 0.64. Although the Bonferroni adjustment is likely conservative, we conclude that there is not strong evidence in favor of a treatment effect for MICUNAY + CWG on these outcomes.
Table 6.
Effect of the Number of MICUNAY sessions attended on 3-month and 6-month outcomes, among youth randomized to the interventiona.
| Effect per sessionb | |||
|---|---|---|---|
| Continuous outcomes | Coefficient (SE) | p-Value | Effect sizec |
| Intentions to drink any alcohol in next 6 months | −0.18 (0.09) | 0.05 | −0.15 |
| Intentions to use any marijuana in next 6 months | −0.08 (0.13) | 0.54 | −0.07 |
| Intentions to smoke a cigarette in next 6 months | −0.04 (0.12) | 0.77 | −0.04 |
| Alcohol resistance self-efficacy | 0.19 (0.09) | 0.04 | 0.17 |
| How often around teens smoking cigarettes | 0.02 (0.08) | 0.81 | 0.02 |
| How often around teens drinking alcohol | 0.12 (0.09) | 0.21 | 0.13 |
| How often around teens using marijuana | −0.03 (0.12) | 0.84 | −0.03 |
| Intentions to participate in cultural activities in next 6 months | 0.15 (0.07) | 0.04 | 0.16 |
| Multigroup Ethnic Identity Measure (MEIM) | −0.04 (0.13) | 0.75 | −0.04 |
| Spirituality/happiness | 0.11 (0.20) | 0.58 | 0.09 |
| Dichotomous outcomes | Odds ratio (CI) | p-Value | Effect sizec |
| Any consequences from drinking alcohol past 3 months | 0.66 (0.34–1.29) | 0.23 | −0.23 |
| Any consequences from using marijuana past 3 months | 1.10 (0.64–1.90) | 0.72 | 0.05 |
| Used tobacco in the past 3 months | 0.90 (0.49–1.65) | 0.73 | −0.06 |
| Drank alcohol in the past 3 months | 0.72 (0.45–1.14) | 0.16 | −0.18 |
| Had 5 or more drinks in a row in past 3 months | 0.75 (0.38–1.47) | 0.40 | −0.16 |
| Used marijuana in the past 3 months | 0.64 (0.32–1.30) | 0.22 | −0.25 |
All results in table account for missing data using multiple imputation methods.
Follow-up outcomes at 3- and 6-months were analyzed together. Regression models include records for each of the two follow-ups per participant. Models account for clustering of responses within individual and adjust for baseline values of the outcome, race/ethnicity, age, gender, which survey (3-month or 6-month) the response came from, and time elapsed between the end of treatment and the follow-up survey response.
For continuous outcomes, effect size is the coefficient divided by the standard deviation of the outcome for combined follow-up data. For dichotomous outcomes, the effect size is the log of the odds ratio divided by 1.81.
5. Discussion
This study contributes to the AOD prevention and intervention literature for urban AI/AN adolescents by conducting one of the largest RCTs to date of an AOD prevention intervention specifically tailored for this population. This project provides a rare opportunity to engage a highly under-served population in a large federally funded study. The study also demonstrates feasibility of conducting a randomized controlled trial in AI/AN communities outside of reservations. By utilizing CBPR principles and a well-established, multi-disciplinary research team including AI/AN researchers and community leaders, we obtained information to help move the field forward, providing some indicators of what might work (and not work) with urban AI/AN adolescents.
We compared two culturally based interventions for 185 urban AI/AN adolescents age 14–18 located in northern, central and southern California as part of the IRINAH initiative focused on improving Native American Health (Crump et al., 2017). Intervention content, materials and overall study design were developed with extensive community input to ensure cultural appropriateness, feasibility, and sustainability of the intervention, as well as a culturally acceptable control condition (Dickerson et al., 2015). We did not find significant differences between the CWG only group and the MICUNAY + CWG group on adolescents’ intentions to use AOD, time spent with peers who use AOD, personal use, consequences, or spirituality and identity. In fact, rates of alcohol and marijuana use remained relatively stable over the course of the study for teens in both groups. In addition, we found that adolescents’ intentions to use marijuana and cigarettes and drink alcohol remained relatively stable from the baseline assessment to the 6-month assessment for both groups, as well as the time that teens said that they spent with peers who used these substances. This contrasts with previous intervention work with AI/AN teens, where findings indicated that both groups increased their substance use, positive attitudes about drugs, and exposure to drugs over time in a one month period ( Kulis et al., 2017), and also with data showing that adolescents typically increase their AOD use during this developmental timeframe (Johnston et al., 2018; Pedersen et al., 2013).
It may be that connecting urban AI/AN adolescents to culturally centered activities and resources is protective, which has been shown in other work with this population (Dickerson et al., 2019; Schweigman, Soto, Wright, & Unger, 2011). Given that both interventions included cultural components, perhaps participants who had the opportunity to engage in either condition may have benefitted from exposure to activities emphasizing cultural education. That is, it may be that attending even one CWG offered an opportunity for the teens in our study to connect or reconnect with their AI/AN heritage. This is important to recognize since over the last decade, AI/AN traditional practices have gained increasing recognition as a crucial component in addressing health disparities among this population (Bassett, Tsosie, & Nannauck, 2012; Jernigan, D’Amico, Duran, & Buchwald, 2018; Kaholokula et al., 2018). In addition, the 2018 report released by the National Council of Urban Indian Health (NCUIH) emphasized the importance of connecting with AI/AN culture as way to promote resilience within urban areas (Shuman, 2018). The current study provides some preliminary information on the potential benefits of culturally centered interventions with a select sample of teens in California. However, longer term studies of AOD interventions throughout the U.S. are suggested to test the potential benefits of culturally centered interventions based on level of cultural education and traditional activity participation intensity with this population.
Another reason we may not have found differences between our two cultural interventions may be due to our recruitment approach for the study. For example, as part of our CBPR approach, we worked closely with each community by hiring AI/AN recruiters from the community who knew the AI/AN community well. We also recruited teens at community events, such as Pow Wows, and collaborated with AI/AN organizations in each community to spread the word about our project. Thus, the teens in our sample may have had stronger initial cultural connections to their community than other population based urban AI/AN adolescent samples. In fact, in our recently published reports generated from baseline data using this same sample, we found that this sample of urban AI/AN adolescents participated in numerous AI/AN traditional activities (D’Amico et al., 2019), and also demonstrated an ability to offset the potential negative consequences of experiencing overt discrimination and microaggressions (Dickerson et al., 2019). We also found that those who self-identified on their survey as AI/AN reported better mental health, less alcohol and marijuana use, lower rates of delinquency, and increased happiness and spiritual health (Brown et al., In press). Thus, adolescents’ strong connection with cultural resources and their added participation in CWG or CWG + MICUNAY may have contributed to this particular urban sample being more resilient, and perhaps supported them in making healthy choices.
There are several limitations to the current study. First, although the largest population of AI/ANs exists in California (Norris et al., 2012), conclusions may not be generalizable outside of California. In addition, as noted earlier, given our recruitment approach, the sample may have been biased towards adolescents who were more culturally connected at the outset. Furthermore, 18% of teens in the MICUNAY + CWG group and 37% of teens in the CWG only group did not receive any sessions and/or attend a gathering (Fig. 1). In our development work with these communities, transportation was noted as a significant barrier to obtaining services, which led us to change the scope of the original intervention from six 1-h workshops to three 2-h workshops ( Dickerson et al., 2015), and to ensure that we reimbursed for transportation to MICUNAY workshops. Despite this, results indicate that many teens were still not able to get to the MICUNAY workshops or the CWGs, even within the three-month timeframe. This is not unusual in these urban settings where many AI/ANs may find it difficult to get to the services offered in their community (Itty, Hodge, & Martinez, 2014). For example, many programs offered at one of our collaborating organizations provide home based services because of transportation issues experienced by their clients, which highlights the importance of finding ways to increase access to services for this population.
Given the difficulties teens had in getting to the workshops, our null findings could also be due to the fact that the “dose” of MICUNAY that many teens received was insufficient to lead to significant behavior change. In addition, the MI fidelity ratings for MICUNAY had a wide range, from 3.2 to 4.8. The average was 3.5, which indicates beginning proficiency in MI. Thus, the range of MI skill may have affected outcomes as well. Due to these observations and our experiences with this initial R01 study conducted within urban AI/AN communities throughout California, we recommend that future studies allow for provisions for transportation.
An additional challenge we faced during this study was the wide diversity of “starting points” for adolescents involved in the study with respect to cultural identity and knowledge, including mixed racial-ethnic ancestry and a range of experiences or attachments to specific tribal background (Whitesell, Mousseau, Parker, Rasmus, & Allen, 2018). Not only was this a challenge for intervention design and implementation (Brown et al., 2016; Dickerson et al., 2015), this diversity may also have affected the efficacy of our intervention for various teens and could have contributed to our null findings. Unfortunately, we are limited by our sample size to analyze the effects of such heterogeneity. Additionally, some of this heterogeneity may be linked to unmeasured variables in this study, such as adolescents’ connections (or lack of connections) to other AI/ANs in the community. Indeed, few studies have addressed this likely very important driver of urban AI/AN adolescent outcomes (Rees, Freng, & Winfree, 2014). Future work should assess the social networks of urban AI/AN adolescents, and also incorporate interventions to help bolster cultural support and social relationships that encourage healthy choices. To date, there are no social network studies of AOD use among urban AI/ANs, and no intervention studies for urban AI/AN youth informed by social network analysis (Shelton et al., 2018) despite the key role networks play in triggering AOD use (de la Haye, Green, Kennedy, Pollard, & Tucker, 2013; Rosenquist, Murabito, Fowler, & Christakis, 2010; Tucker, de la Haye, Kennedy, Green, & Pollard, 2014).
Finally, current measurement of cultural characteristics among AI/ANs is largely based on existing scales, many of which were designed for generic use or for other racial-ethnic groups. Our study was no different in this regard. Future work is needed to improve measurement of cultural characteristics among AI/AN adolescents, including systematic mixed methods approaches to assess cultural consensus around core beliefs (Matthews, Brown, & Kennedy, 2018).
6. Conclusions
This study is one of the first large scale AOD prevention RCTs to be conducted with urban AI/AN adolescents across the state of California. We were able to successfully conduct this RCT within these urban communities because of our research team’s unique set of expertise and community connections. We worked together with numerous urban communities in the state to deal with a challenging public health issue that has been noted for decades (Whitesell et al., 2018). We were able to effectively utilize CBPR principles, which resulted in successful partnerships with the communities, and provided us with the opportunity to educate participants and communities on how their involvement in this research study could help increase our understanding of what may enhance the health and well-being of urban AI/AN adolescents.
Overall, the data showed no differences between the CWG and MICUNAY + CWG groups. However, this simple result may not tell the full story. Given the importance to communities that every teen receive some culturally relevant intervention, our “control” group was not the standard control that is often seen in RCTs. In fact, our control group comprised a large cultural event designed to connect adolescents with their heritage and AI/AN resources in their community. The overall effort to conduct the work in a culturally appropriate manner was key to the success of the project – ensuring that Native American people were trained on MI and provided the workshops, working closely with community organizations to recruit the sample of teens across the state and following them up over time, and ensuring that every teen who was in the CWG only group had the opportunity after the six month follow up to participate in the MICUNAY workshops. This community effort may also have led to recruitment of more culturally connected teens, which could have affected findings.
This study is only the first step in understanding the effects of evidence-based prevention programming and traditional practices among urban AI/AN adolescents. There are many pieces that need to be better understood in order to put these findings in context. For example, our focus group work indicated that many urban AI/AN teens may not be in environments that encourage cultural learning (Brown et al., 2016), thus, it may be important to include measurement of adolescents’ social networks to understand the amount of support they receive to engage in traditional practices and make healthy choices around AOD use.
Given that few evidence based interventions are successfully implemented with Indigenous populations (Jernigan, D’Amico, & Kaholokula, 2018), it is crucial to continue to create programming collaboratively with communities to ensure both feasibility and sustainability. The overall response to MICUNAY was extremely positive, and several communities continue to implement the workshops as part of their programming for adolescents. By sharing these important lessons on conducting RCTs in Indian country, we hope to support the continued evolution of intervention work in Indigenous communities.
Acknowledgements
Work on this article was supported by a grant from the National Institute on Alcohol Abuse and Alcoholism R01AA022066 to Drs. D’Amico and Dickerson with co-funding from the National Institute on Drug Abuse. We would also to thank our Elder and youth advisory boards and the communities and organizations that helped us recruit adolescents for this study. Finally, we thank Jennifer Parker and the Survey Research Group for conducting all of the baseline and follow up surveys.
Footnotes
CRediT authorship contribution statement
Elizabeth J. D’Amico:Conceptualization, Methodology, Investigation, Writing - original draft, Writing - review & editing, Supervision, Project administration, Funding acquisition.Daniel L. Dickerson: Conceptualization,Investigation, Writing - review & editing, Supervision, Project administration, Funding acquisition.Ryan A. Brown:Conceptualization, Writing - review & editing.Carrie L. Johnson:Conceptualization, Writing - review & editing, Resources.David J. Klein:Data curation, Formal analysis, Methodology, Writing - review & editing.Denis Agniel:Formal analysis, Methodology, Writing - review & editing.
References
- Antonio MCK, & Chung-Do JJ (2015). Systematic review of interventions focusing on indigenous adolescent mental health and substance use. American Indian and Alaska Native Mental Health Research, 22(3), 36–56. [DOI] [PubMed] [Google Scholar]
- Bassett D, Tsosie U, & Nannauck S. (2012). “Our culture is medicine”: Perspectives of Native healers on posttrauma recovery among American Indian and Alaska Native patients. The Permanente Journal, 16(1), 19–27 (PMC3327107). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botvin GJ, Baker E, Dusenbury L, Tortu S, & Botvin EM (1990). Preventing adolescent drug abuse through a multimodal cognitive-behavioral approach: Results of a three year study. Journal of Consulting and Clinical Psychology, 58, 437–446. [DOI] [PubMed] [Google Scholar]
- Brave Heart MYH, & DeBruyn LM (1998). The American Indian holocaust: Healing historical unresolved grief. American Indian and Alaska Native Mental Health Research, 8(2), 56–78. [PubMed] [Google Scholar]
- Brockie TN, Heinzelmann M, & Gill J. (2013). A framework to examine the role of epigenetics in health disparities among Native Americans. Nursing Research and Practice, 2013, 1–9. 10.1155/2013/410395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodish AB, Cogburn CD, Fuller-Rowell TE, Peck S, Malanchuk O, & Eccles JS (2011). Perceived racial discrimination as a predictor of health behaviors: The moderating role of gender. Race and Social Problems, 3(3), 160–169. 10.1007/s12552-011-9050-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Dickerson DL, & D’Amico EJ (2016). Cultural identity among urban American Indian/Alaska Native youth: Implications for intervention design. Prevention Science, 17(7), 852–861 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Dickerson DL, Klein DJ, Agniel D, Johnson C, D’Amico EJ (In press) Identifying as American Indian/Alaska Native: Implications for adolescent behavioral health and well-being. Youth and Society. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt LW (1986). Roots of the Native American urban experience: Relocation policy in the 1950s. American Indian Quarterly, 10(2), 85–99. 10.2307/1183982. [DOI] [Google Scholar]
- Castor ML, Smyser MS, Taualii MM, Park AN, Lawson SA, & Forquera RA (2006). A nationwide population-based study identifying health disparities between American Indians/Alaska Natives and the general populations living in select urban counties. American Journal of Public Health, 96(8), 1478–1484. 10.2105/AJPH.2004.053942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crump AD, Etz K, Arroyo JA, Hemberger N, & Srinivasan S. (2017). Accelerating and strengthening Native American health research through a collaborative NIH initiative. Prevention Science 10.1007/s11121-017-0854-5 November 16. (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Dickerson DL, Brown RA, Klein DJ, Agniel D, & Johnson C. (2019). Unveiling an “invisible” population: Health, substance use, sexual behavior, culture, and discrimination among urban American Indian/Alaska Native adolescents in California. Ethnicity & Health. 10.1080/13557858.2018.1562054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Houck JM, Hunter SB, Miles JNV, Osilla KC, & Ewing BA (2015). Group motivational interviewing for adolescents: Change talk and alcohol and marijuana outcomes. Journal of Consulting and Clinical Psychology, 83(1), 68–80 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Hunter SB, Miles JNV, Ewing BA, & Osilla KC (2013). A randomized controlled trial of a group motivational interviewing intervention for adolescents with a first time alcohol or drug offense. Journal of Substance Abuse Treatment, 45(5), 400–408 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Miles JNV, Stern SA, & Meredith LS (2008). Brief motivational interviewing for teens at risk of substance use consequences: A randomized pilot study in a primary care clinic. Journal of Substance Abuse Treatment, 35, 53–61. [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Parast L, Meredith LS, Ewing BA, Shadel WG, & Stein BS (2016). Screening in primary care: What is the best way to identify at-risk youth for substance use? Pediatrics, 138, 1–9 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Parast L, Shadel WG, Meredith LS, Seelam R, & Stein BD (2018). Brief motivational interviewing intervention to reduce alcohol and marijuana use for at-risk adolescents in primary care: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 86(9), 775–786 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JNV, Ewing BA, Shih RA, & Pedersen ER (2016). Alcohol and marijuana use trajectories in a diverse longitudinal sample of adolescents: Examining use patterns from age 11 to 17. Addiction, 111(10), 1825–1835 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JNV, Zhou AJ, Shih RA, & Green HD Jr. (2012). Preventing alcohol use with a voluntary after school program for middle school students: Results from a cluster randomized controlled trial of CHOICE. Prevention Science, 13(4), 415–425 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- de la Haye K, Green HD, Kennedy DP, Pollard MS, & Tucker JS (2013). Selection and influence mechanisms associated with marijuana initiation and use in adolescent friendship networks. Journal of Research on Adolescence, 23(3), 474–486 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, Baldwin J, Belcourt A, Belone L, Gittelsohn J, Kaholokula K, ... Wallerstein N. (2018). Encompassing cultural contexts within scientific research methodologies in the development of health promotion interventions. Prevention Science 10.1007/s11121-018-0926-1 (PMCID: doi: 10.1007/s11121-018-0926-1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, Brown RA, Johnson CL, Schweigman K, & D’Amico EJ (2015). Integrating motivational interviewing and traditional practices to address alcohol and drug use among urban American Indian/Alaska Native youth. Journal of Substance Abuse Treatment, 65, 26–35 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, Brown RA, Klein DJ, Agniel D, Johnson C, & D’Amico EJ (2019). Overt perceived discrimination and racial microaggressions and their association with health risk behaviors among a sample of urban American Indian/Alaska Native adolescents. Journal of Racial and Ethnic Health Disparities, 6, 733–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, Moore LA, Rieckmann T, Croy C, Venner K, Moghaddam J, ... Novins DK (2018). Correlates of motivational interviewing use among substance use treatment programs serving American Indians/Alaska Natives. The Journal of Behavioral Health Services & Research, 45(1), 31–45 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, & Johnson CL (2011). Design of a behavioral health program for urban American Indian/Alaska Native youths: A community informed approach. Journal of Psychoactive Drugs, 43(4), 337–342. [DOI] [PubMed] [Google Scholar]
- Dickerson DL, & Johnson CL (2012). Mental health and substance abuse characteristics among a clinical sample of urban American Indian/Alaska Native youths in a large California metropolitan area: A descriptive study. Community Mental Health Journal, 48(1), 56–62 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellickson PL, McCaffrey DF, Ghosh-Dastidar B, & Longshore DL (2003). New inroads in preventing adolescent drug use: Results from a large-scale trial of Project ALERT in middle schools. American Journal of Public Health, 93, 1830–1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldstein Ewing SW, Wray AM, Mead HK, & Adams SK (2012). Two approaches to tailoring treatment for cultural minority adolescents. Journal of Substance Abuse Treatment, 43, 190–213 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman BJ, Coll KM, Two Dogs R, Iron Cloud Two Dogs E, Iron Cloud E, & Robertson P. (2016). The value of Lakota traditional healing for youth resiliency and family functioning. Journal of Aggression, Maltreatment & Trauma, 25(5), 455–469. 10.1080/10926771.2015.1079282. [DOI] [Google Scholar]
- Gil AG, Wagner EF, & Tubman JG (2004). Culturally sensitive substance abuse intervention for Hispanic and African American adolescents: Empirical examples from the Alcohol Treatment Targeting Adolescents in Need (ATTAIN) project. Addiction, 99(Suppl. 2), 140–150. [DOI] [PubMed] [Google Scholar]
- Gilder DA, Geisler JR, Luna JA, Calac D, Monti PM, Spillane NS, ... Ehlers CL (2017). A pilot randomized trial of motivational interviewing compared to psycho-education for reducing and preventing underage drinking in American Indian adolescents. Journal of Substance Abuse Treatment, 82, 74–81. 10.1016/j.jsat.2017.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilder DA, Luna JA, Calac D, Moore RS, Monti PM, & Ehlers CL (2011). Acceptability of the use of motivational interviewing to reduce underage drinking in a Native American community. Substance Use & Misuse, 46(6), 836–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelsohn J, Belcourt A, Magarati M, Booth-LaForce C, Duran B, Mishra SI, ... Jernigan VBB (2018). Building capacity for productive indigenous community-university partnerships. Prevention Science 10.1007/s11121-0180949-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, ... Hasin DS (2017). Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry, 74(9), 911–923. 10.1001/jamapsychiatry.2017.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatcher RL, & Gillaspy JA (2006). Development and validation of a revised short version of the Working Alliance Inventory. Psychotherapy Research, 16(1), 12–25. [Google Scholar]
- Itty TL, Hodge FS, & Martinez F. (2014). Shared and unshared barriers to cancer symptom management among urban and rural American Indians. The Journal of Rural Health, 30(2), 206–213. 10.1111/jrh.12045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanich JD, Mousseau AC, Walls M, Whitbeck L, & Whitesell NR (2020). Pathways of adaptation: Two case studies with one evidence-based substance use prevention program tailored for indigenous youth. Prevention Science 10.1007/s11121-018-0914-5 (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jernigan VB, D’Amico EJ, Duran B, & Buchwald D. (2018). Multilevel and community-level interventions with Native Americans: Challenges and opportunities. Prevention Science 10.1007/s11121-018-0916-3 (Epub ahead of print).. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jernigan VB, D’Amico EJ, & Kaholokula JK (2018). Prevention research with indigenous communities to expedite dissemination and implementation efforts. Prevention Science 10.1007/s11121-018-0951-0 (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jernigan VB, Peercy M, Branam D, Saunkeah B, Wharton D, Winkleby M, ... Buchwald D. (2015). Beyond health equity: Achieving wellness within American Indian and Alaska Native communities. American Journal of Public Health, (Suppl. 3), S376–S379 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, & Patrick ME (2018). Monitoring the Future national survey results on drug use: 1975–2017: Overview, key findings on adolescent drug use. Ann Arbor, MI: Institute for Social Research, The University of Michigan. [Google Scholar]
- Jones ML, & Galliher RV (2015). Daily racial microaggressions and ethnic identification among Native American young adults. Cultural Diversity and Ethnic Minority Psychology, 21(1), 1–9. 10.1037/a0037537. [DOI] [PubMed] [Google Scholar]
- Kaholokula JK, Ing CT, Look MA, Delafield R, & Sinclair K. (2018). Culturally responsive approaches to health promotion for Native Hawaiians and Pacific Islanders. Annals of Human Biology, 45(3), 249–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman CE, Black K, Keane EM, Big Crow CK, Shangreau C, Arthur-Asmah R, ... Tuitt N. (2014). Planning for a group-randomized trial with American Indian youth. Journal of Adolescent Health Care, 54(3), S59–S63. [DOI] [PubMed] [Google Scholar]
- Kennedy DP, Osilla KC, Hunter SB, Golinelli D, Maksabedian Hernandez E, & Tucker JS (2018). A pilot test of a motivational interviewing social network intervention to reduce substance use among housing first residents. Journal of Substance Abuse Treatment, 86, 36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulis S, Dustman PA, Brown EF, & Martinez M. (2013). Expanding urban American Indian youths’ repertoire of drug resistance skills: Pilot results from a culturally adapted prevention program. American Indian and Alaska Native Mental Health Research, 20(1), 35–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulis SS, Ayers SL, & Harthun ML (2017). Substance use prevention for urban American Indian youth: A efficacy trial of the culturally adapted Living in 2 Worlds program. The Journal of Primary Prevention, 38(1–2), 137–158. 10.1007/s10935-016-0461-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen DL, Atkinson CC, Hargreaves WA, & Nguyen TD (1979). Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning, 2, 197–207. [DOI] [PubMed] [Google Scholar]
- Liddell J, & Burnette CE (2017). Culturally-informed interventions for substance abuse among indigenous youth in the United States: A review. Journal of Evidence-Informed Social Work, 14(5), 329–359. 10.1080/23761407.2017.1335631. [DOI] [PubMed] [Google Scholar]
- Listug-Lunde L, Vogeltanz-Holm N, & Collins J. (2013). A cognitive-behavioral treatment for depression in rural American Indian middle school students. American Indian and Alaska Native Mental Health Research, 20(1), 16–34. [DOI] [PubMed] [Google Scholar]
- Lowe J, Liang H, Henson J, & Riggs C. (2016). Preventing substance use among Native American early adolescents. Journal of Community Psychology, 44(8), 997–1010. 10.1002/jcop.21823. [DOI] [Google Scholar]
- Mack KA, Jones CM, & Ballesteros MF (2017). Illicit drug use, illicit drug use disorders, and drug overdose deaths in metropolitan and nonmetropolitan areas-United States. American Journal of Transplantation, 17(12), 3241–3252. [DOI] [PubMed] [Google Scholar]
- Matthews LJ, Brown RA, & Kennedy DP (2018). A manual for cultural analysis. Santa Monica, CA: RAND Corporation. [Google Scholar]
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, & Schulenberg JE (2016). Monitoring the Future national survey results on drug use, 1975–2015: Volume I, secondary school students. Ann Arbor: Institute for Social Research, The University of Michigan. [Google Scholar]
- Moghaddam J, Momper S, & Fong T. (2015). Crystalizing the role of traditional healing in an urban Native American health center. Community Mental Health Journal, 51(3), 305–314. 10.1007/s10597-014-9813-9. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin JK, Miller WR, & Ernst D. (2010). Revised Global Scales: Motivational Interviewing Treatment Integrity 3.1.1 (MITI 3.1.1). Center on Alcoholism, Substance Abuse and Addictions (CASAA). [Google Scholar]
- Mullett J. (2015). Issues of equity and empowerment in knowledge democracy: Three community based research examples. Action Research, 13(3), 248–261. [Google Scholar]
- Myhra LL (2011). “It runs in the family”: Intergenerational transmission of historical trauma among urban American Indians and Alaska Natives in culturally specific sobriety maintenance programs. American Indian and Alaska Native Mental Health Research, 18(2), 17–40. [DOI] [PubMed] [Google Scholar]
- Myhra LL, & Wieling E. (2014). Intergenerational patterns of substance abuse among urban American Indian families. Journal of Ethnicity in Substance Abuse, 13(1), 1–22. 10.1080/15332640.2013.847391. [DOI] [PubMed] [Google Scholar]
- Naar-King S, Parsons JT, Murphy D, Kolmodin K, Harris DR, & ATN 004 Protocol Team (2010). A multisite randomized trial of a motivational interviewing intervention targeting multiple risks in youth living with HIV: Initial effects on motivation, self-efficacy and depression. Journal of Adolescent Health, 46, 422–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center of Urban Indian Health (2015). The efficacy of American Indian and Alaska Native traditional healing methods: A literature review. As of April 15, 2019 https://www.ncuih.org/action/document/download?document_id=153. [Google Scholar]
- Native American Health Center (2012). Native vision: A focus on improving behavioral health wellness for California Native Americans - California Reducing Disparities Project (CRDP) Native American population report. Oakland, Calif: Native American Health Center. [Google Scholar]
- Norris T, Vines PL, & Hoeffel EM The American Indian and Alaska Native population: 2010. http://www.census.gov/prod/cen2010/briefs/c2010br-10.pdf. [Google Scholar]
- Novins DK, Boyd ML, Brotherton DT, Fickenscher A, Moore L, & Spicer P. (2012). Walking on: Celebrating the journeys of Native American adolescents with substance use problems on the winding road to healing. Journal of Psychoactive Drugs, 44(2), 153–159. [DOI] [PubMed] [Google Scholar]
- Paradies Y. (2016). Colonisation, racism and indigenous health. Journal of Population Research, 33(1), 83–96. 10.1007/s12546-016-9159-y. [DOI] [Google Scholar]
- Pedersen ER, Miles JNV, Ewing BA, Tucker JS, Shih RA, & D’Amico EJ (2013). A longitudinal examination of alcohol, marijuana, and cigarette perceived norms among middle school adolescents. Drug and Alcohol Dependence, 133(2), 647–653 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterman AH, Fitchet TG, Brady MJ, Hernandez L, & Cella D. (2002). Measuring spiritual well-being in people with cancer: The Functional Assessment of Chronic Illness Therapy–Spiritual Well-Being Scale (FACIT-Sp). Annals of Behavioral Medicine, 24, 49–58. [DOI] [PubMed] [Google Scholar]
- Phinney JS, & Ong AD (2007). Conceptualization and measurement of ethnic identity: Current status and future directions. Journal of Counseling Psychology, 54(3), 271–281. [Google Scholar]
- Ponterotto JG, Gretchen D, Utsey SO, Stracuzzi T, & Saya R. (2003). The multigroup ethnic identity measure (MEIM): Psychometric review and further validity testing. Educational and Psychological Measurement, 63(3), 502–515. 10.1177/0013164403063003010. [DOI] [Google Scholar]
- Raghupathy S, & Forth ALG (2012). The HAWK2 program: A computer-based drug prevention intervention for Native American youth. The American Journal of Drug and Alcohol Abuse, 38(5), 461–467. 10.3109/00952990.2012.694531. [DOI] [PubMed] [Google Scholar]
- Rees C, Freng A, & Winfree LT (2014). The Native American adolescent: Social network structure and perceptions of alcohol induced social problems. Journal of Youth and Adolescence, 43(3), 405–425. 10.1007/s10964-013-0018-2. [DOI] [PubMed] [Google Scholar]
- Rosenquist JN, Murabito J, Fowler JH, & Christakis NA (2010). The spread of alcohol consumption behavior in a large social network. Annals of Internal Medicine, 152(7), 426–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB (2004). Multiple imputation for nonresponse in surveys. Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- SAMHSA National Registry of Evidence-based Programs and Practices (NREPP) (2014). Motivational interviewing. Rockville, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Schinke SP, Tepavac L, & Cole KC (2000). Preventing substance use among Native American youth: Three-year results. Addictive Behaviors, 25(3), 387–397. 10.1016/S0306-4603(99)00071-4. [DOI] [PubMed] [Google Scholar]
- Schmiege SJ, Broaddus MR, Levin M, & Bryan AD (2009). Randomized trial of group interventions to reduce HIV/STD risk and change theoretical mediators among detained adolescents. Journal of Consulting and Clinical Psychology, 77(1), 38–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweigman K, Soto C, Wright S, & Unger J. (2011). The relevance of cultural activities in ethnic identity among California Native American youth. Journal of Psychoactive Drugs, 43(4), 343–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton RC, Lee M, Brotzman LE, Crookes DM, Jandorf L, Erwin D, & Gage-Bouchard E. (2018). Use of social network analysis in the development, dissemination, implementation, and sustainability of health behavior interventions for adults: A systematic review. Social Science & Medicine, 220, 81–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shuman N. (2018). The use of traditional healing practices to address AI/AN historical trauma and disparities in behavioral health. Washington D.C: National Council of Urban Indian Health. [Google Scholar]
- Stanley LR, Swaim RC, Kaholokula JK, Kelly KJ, Belcourt A, & Allen J. (2018). The imperative for research to promote health equity in indigenous communities. Prevention Science 10.1007/s11121-017-0850-9 November 6. (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoner L, Page R, Matheson A, Tarrant M, Stoner K, Rubin D, & Perry L. (2015). The indigenous health gap: Raising awareness and changing attitudes. Perspectives in Public Health, 135(2), 68–70. [DOI] [PubMed] [Google Scholar]
- Tobler AL, Maldonado-Molina MM, Staras SAS, O’Mara RJ, Livingston MD, & Komro KA (2013). Perceived racial/ethnic discrimination, problem behaviors, and mental health among minority urban youth. Ethnicity & Health, 18(4), 337–349. 10.1080/13557858.2012.730609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomlin K, Walker RD, Grover J, Arquette W, & Stewart P. (2014). Trainer’s guide to motivational interviewing: Enhancing motivation for change—A learner’s manual for the American Indian/Alaska Native counselor. Portland, OR: One Sky Center. [Google Scholar]
- Trout L, Kramer C, & Fischer L. (2018). Social medicine in practice: Realizing the American Indian and Alaska Native right to health. Health and Human Rights, 20(2), 19–30. [PMC free article] [PubMed] [Google Scholar]
- Tucker JS, de la Haye K, Kennedy DP, Green HD, & Pollard MS (2014). Peer influence on marijuana use in different types of friendships. Journal of Adolescent Health, 54, 67–73 (PMCID: ). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venner KL, Donovan DM, Campbell ANC, Wendt DC, Rieckmann T, Radin SM, ... Rosa CL (2018). Future directions for medication assisted treatment for opioid use disorder with American Indian/Alaska Natives. Addictive Behaviors, 86, 111–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venner KL, Feldstein SW, & Tafoya N. (2007). Helping clients feel welcome: Principles of adapting treatment cross-culturally. Alcoholism Treatment Quarterly, 25(4), 11–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters KL, Johnson-Jennings M, Stroud S, Rasmus S, Charles B, John S, ... Boulafentis J. (2018). Growing from our roots: Strategies for developing culturally grounded health promotion interventions in American Indian, Alaska Native, and Native Hawaiian communities. Prevention Science 10.1007/s11121018-0952-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warne D, & Frizzell LB (2014). American Indian health policy: Historical trends and contemporary issues. American Journal of Public Health, 104(Suppl. 3), S263–S267. 10.2105/AJPH.2013.301682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitesell NR, Mousseau A, Parker M, Rasmus S, & Allen J. (2018). Promising practices for promoting health equity through rigorous intervention science with indigenous communities. Prevention Science 10.1007/s11121-0180954-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods B, & Jose PE (2011). Effectiveness of a school-based indicated early intervention program for Māori and Pacific adolescents. Journal of Pacific Rim Psychology, 5(1), 40–50. 10.1375/prp.5.1.40. [DOI] [Google Scholar]