Abstract
Objectives
To investigate the correlation between the four dimensions of Oral Health-Related Quality of Life (OHRQoL) and Health-Related Quality of Life (HRQoL) constructs in a dental patient population.
Methods
A cross-sectional study carried out at HealthPartners, Minnesota, USA. This study is a secondary data analysis of available adult dental patients’ data. The instruments used to assess the OHRQoL and HRQoL constructs were the Oral Health Impact Profile–version with 49 items (OHIP-49) and Patient-Reported Outcome Measures Information System (PROMIS) measures v.1.1 Global Health instruments Patient Reported Outcome Measures (PROMs), respectively. We used Structural Equation Modeling to determine the correlation between OHRQoL and HRQoL.
Results
Two thousand and seventy-six dental patients participated in the study. OHRQoL and HRQoL scores correlated with 0.56 (95%CI:0.52–0.60). The OHRQoL and Physical Health dimension of HRQoL correlated with 0.55 (95%CI:0.51–0.59). The OHRQoL and Mental Health dimension of HRQoL correlated with 0.51 (95%CI:0.47–0.55). When adjusted for age, gender, and depression, the correlation coefficients changed only slightly and resulted in 0.52 between OHRQoL and HRQoL Physical Health, and 0.47 between OHRQoL and HRQoL Mental Health. Model fit statistics for all analyses were adequate and indicated a good fit.
Conclusions
OHRQoL and HRQoL overlap greatly. For dental practitioners, the OHRQoL score is informative for their patients’ general health status and vice versa. Study results indicate that effective therapeutic interventions by dentists improve patients’ OHRQoL as well as HRQoL.
Keywords: oral health, health, quality of life, self report, surveys and questionnaires, depressive disorder, public health, structural equation modeling, correlation of data, evidence-based dentistry
IZVLEČEK
Namen
Določiti korelacijo med štirimi dimenzijami konstrukta z oralnim zdravjem povezana kakovost življenja (ang. Oral Health-Related Quality of Life ali krajše OHRQoL) in konstruktom z zdravjem povezana kakovost življenja (ang. Health-Related Quality of Life ali krajše HRQoL) pri zobozdravstvenih pacientih.
Metode
Podatki zobozdravstvenih pacientov so bili v tej presečni raziskavi pridobljeni s klinike HealthPartners, Minnesota, ZDA. Ta študija je sekundarna analiza podatkov o razpoložljivih podatkih o zobozdravnikih za odrasle. Za oceno konstruktov OHRQoL in HRQoL sta bila uporabljena instrumenta Oral Health Impact Profile, ki sestoji iz 49 vprašanj (OHIP-49) in Patient-Reported Outcome Measures Information System (PROMIS) v.1.1 Global Health. Korelacija med konstruktoma je bila izračunana na podlagi modeliranja strukturnih enačb.
Rezultati
V raziskavo je bilo vključenih 2.076 zobozdravstvenih pacientov. Korelacijski koeficient med konstruktoma OHRQoL in HRQoL je znašal 0,56 (95 % CI:0,51–0,59). Korelacijski koeficient med oceno telesnega zdravja po OHRQoL in HRQoL (ang. HRQoL Physical Health) je znašal 0,55 (95 % CI:0,51–0,59). Korelacijski koeficient med oceno duševnega zdravja OHRQoL in HRQoL (ang. HRQoL Mental Health) je znašal 0,51 (95 % CI:0,47–0,55). Ob upoštevanju motečih dejavnikov, kot so starost, spol in depresija, je korelacijski koeficient med OHRQoL in telesnim zdravjem znašal 0,52 ter med OHRQoL in duševnim zdravjem 0,47. Pokazatelji stopnje prileganja modelov so bili ustrezni in so pokazali dobro prileganje.
Zaključek
Konstrukta OHRQoL in HRQoL se zelo prekrivata. Zobozdravstveni delavci lahko na osnovi pacientove ocene OHRQoL pridobijo tudi koristne informacije o njihovem sistemskem zdravju, drugi zdravstveni delavci pa informacije o njihovem oralnem zdravju. Rezultati raziskave dokazujejo, da učinkovito zobozdravniško zdravljenje ne izboljša samo pacientove z oralnim zdravjem povezane kakovosti življenja, ampak tudi s sistemskim zdravjem povezano kakovost življenja.
Ključne besede: oralno zdravje, zdravje, kakovost življenja, samoocena, ankete in vprašalniki, depresivna motnja, javno zdravje, modeliranje strukturnih enačb, korelacija podatkov, z dokazi podprto zobozdravstvo
1. Introduction
Environmental, behavioral, and personal factors influence both oral and general health, and oral health is also considered a “window” to overall health (1, 2). The overlap between oral health and general health can be assessed with the constructs Oral Health-Related Quality of Life (OHRQoL) (3,4) and Health-Related Quality of Life (HRQoL) (5,6), respectively, that is, how much OHRQoL data could explain HRQoL, and vice versa (1, 2, 7). Knowing the magnitude of the OHRQOL-HRQOL relationship would enable a more patient-centered treatment approach for patients in general and dental patients, specifically.
Studies have shown different magnitudes of the association between OHRQoL and HRQoL. In one cohort of first-year students, it was found that OHRQoL and HRQoL have various determinants suggesting that these two constructs are unrelated in this healthy population (8). In contrast, two studies using two patient-reported outcome measures (PROMs), specifically Oral Health Impact Profile (OHIP) and Short Form Survey (SF) in German dental patients, identified a high correlation between OHRQoL and HRQoL (9, 10). Zimmer et al. derived a correlation between OHIP-14 and SF-12 scores of 0.31–0.32 (9), while Reissmann et al. reported a slightly higher correlation of 0.40 between OHIP-49 and SF-36 scores (10). Ranfl and Zeletel-Kragelj assessed the association between self-rated dentate status and self-rated general health and concluded that poor self-rated health was associated with a higher number of self-reported missing teeth (11).
Single-item or multi-item PROMs can theoretically measure both constructs, but the number of items also influences the reliability, validity, and overall precision of measurement. HRQoL PROMs designed for medical conditions, e.g. dyspnea (12), are used for evaluation of how disease impacts patients HRQoL (13, 14). The Patient-Reported Outcomes Measurement Information System (PROMIS) provides such PROMs (15). With more than 300 individual PROMIS PROMs, it is possible to comprehensively evaluate physical, mental, and social health components in general and patient populations (15).
Several theoretical models exist that aim to explain the OHRQoL construct (16). A new four-dimensional OHRQoL structure was proposed in 2014 (17, 18), providing dentists and researchers with a solid theoretical background for the development of measures for OHRQoL assessment (17,18,19,20,21). It was also demonstrated that this four-dimensional OHRQoL structure could be measured with the most extensively applied dental PROMs (22,23), i.e. longer and shorter OHIP versions (24,25,26,27,28), which assess the patient’s self-perception of oral health. Investigation of the measurement precision of different OHIP versions has provided evidence that even the ultra-short OHIP version, i.e. OHIP-5 (28), precisely measures all four dimensions (29).
The aim of this study was to identify the magnitude of overlap between oral health and general health. Thus the objective of this study was to investigate the correlation between the four-dimensional OHRQoL and HRQoL constructs in a dental patient population.
2. Methods
2.1. Study Subjects and Data Collection
Adult dental patients’ data came from a cross-sectional study carried out at HealthPartners (HP), Minnesota, USA. Our study is a secondary data analysis of available data. A consecutive sample of English and Spanish-speaking dental patients was targeted to recruit 2,000 patients. Study participants were patients attending HP dental clinics for dental interventions or follow-ups and having 40% or less missing information (N=2,076, response rate 55%) about their OHRQoL or HRQoL as measured with the 49-item OHIP and the PROMIS v.1.1 Adult Global Health, respectively. Patients were asked to complete a printed battery of self-administered PROMs and informed consent at home. Data were collected from July 2014 to April 2016. The study was reviewed and approved by the Institutional Review Board of the HealthPartners Institute (Study Number A11–136).
2.2. Patient Reported Outcome Measures and Items Included in Structural Equation Modeling
A battery of PROMs about broad self-perceived oral and general health indicators, more specifically, Oral Health Impact Profile version with 49 items (OHIP-49) (24) and PROMIS v.1.1 Adult Global Health (30), were administered to each participant. Both instruments were developed in English and thoroughly psychometrically tested in English (15, 24) and Spanish language versions (31, 32).
2.2.1. Oral Health Impact Profile Questionnaire
The OHIP-49 questionnaire is based on five response options, where “0” indicates the absence of any problem, while higher OHIP scores represent more impaired patients’ OHRQoL (24). OHIP-49 summary scores range from zero to 196. To give the construct OHRQoL the same direction in comparison to the construct HRQoL regarding their correlation estimation, we reversely coded OHIP items so that higher summary scores represented better OHRQoL. With reversely coded OHIP items, a positive correlation between OHRQoL and HRQoL scales indicated that better OHRQoL is associated with better HRQoL.
We characterized the OHIP summary scores based on the four dimensions of OHRQoL (17, 18), i.e., Oral Function, Orofacial Pain, Orofacial Appearance, and Psychosocial Impact, which are composed of ten, seven, six, and 18 OHIP items, respectively, and derived from the 41 OHIP items that were identified in the previous exploratory (17) and confirmatory factor analyses (CFA) (18) when OHIP-49 structure was thoroughly investigated.
2.2.2. Patient Reported Outcome Measurement Information System v.1.1 - Global Health Questionnaire
PROMIS v.1.1 - Global Health questionnaire (12, 30) measures self-reported general health with ten items. The instrument is composed of two components or dimensions, namely Physical Health and Mental Health. Each component comprises four items. The remaining two items assess overall HRQoL. The values of the response to each question for a given respondent are summed. The PROMIS v.1.1 - Global Health PROM was recently addressed as “a retired” measure (30). For this reason, we converted the scores from PROMIS v.1.1 - Global Health PROM into the latest PROMIS v.1.2 Global Health.
2.2.3. Patient Reported Outcome Measurement Information System v.1.0 Emotional Distress - Depression Questionnaire
The PROMIS v.1.0 Emotional Distress - Depression questionnaire (33) measures the level of depression by evaluating self-reported negative mood, views of self, and social cognition. It consists of 28 items with five response options. In this study, a higher depression score indicated more severe depression. The score range is 28 to 140, and the higher score represents more severe depression.
2.3. Statistical Analysis
We performed all statistical analyses with Mplus Statistical Software, version 8 (Muthén & Muthén, Los Angeles, CA, USA). This software uses by default a Full Information Maximum Likelihood (FIML) (34) estimation approach to handle missing values. Study subjects who did not complete 40% or more of the 46 non-dental items of OHIP-49, PROMIS v.1.1 Global Health, and v.1.0 Emotional Distress - Depression were excluded from the study. Ninety-eight percent of patients in the analysis sample were missing less than 5% of 46 OHIP items, and 96% were missing less than 5% of the ten global health items. For the Depression score, the average item score from non-missing responses was imputed for these patients missing less than 40% of items; 93% of patients were not missing any Depression items, and 97% were missing less than 5% of 28 Depression items.
We analyzed the following three models with Structural Equation Modeling (SEM) methodology.
Model 1: We measured HRQoL with the two HRQoL factors, i.e., Physical Health and Mental Health. In this model, only the Physical and Mental Health of HRQoL were used because PROMIS documentation does not indicate a global HRQoL factor that combines the two HRQoL factors.
We measured OHRQoL with four first-order factors, i.e., the dimensions of OHRQoL. We introduced a second-order OHRQoL factor comprising the four first-order factors. We determined two correlation coefficients for the HRQoLOHRQoL association: one for HRQoL Physical Health - OHRQoL and one for HRQoL Mental Health - OHRQoL.
Model 2: Even if the PROMIS authors do not suggest forming a global factor for PROMIS v.1.1 Global Health PROM, we added a second-order global HRQoL factor in Model 2 because we wanted to derive a single correlation coefficient characterizing the association between OHRQoL and HRQoL constructs. Model 2 is otherwise identical to Model 1.
Model 3: To be comparable with previous analysis (10), three independent variables, i.e. age, gender, and level of depression, were included in Path Analysis (35). Age and gender were self-reported by the patients. This model allows us to compute the association between OHRQoL and HRQoL controlled for potential confounders. We first approached the path analysis model by adding the three independent variables to Model 2. However, we encountered problems fitting the second model, and have, therefore, added the three independents to Model 1 composed of one global OHRQoL factor and two HRQoL Physical and Mental Health factors, which we regressed upon patients’ age, gender, and depression score.
SEM-based second-order confirmatory factor analysis was used to test the model fit scale of OHIP and both PROMIS PROMs and to assess correlations between the global OHRQoL factor and its four dimensions with HRQoL Physical and Mental Health dimensions. In addition, correlation coefficients between OHRQoL dimensions were also estimated from the SEM second-order confirmatory factor analysis model.
Two model fit indices that account for model complexity are the Comparative Fit Index (CFI) and Tucker-Lewis Index (TLI). For both indices, an index value higher than 0.95 indicates a good fit of the model to the data. The Root Mean Square Error of Approximation (RMSEA) of less than 0.08 indicates a good fit (36). More recently, RMSEA (37) of less than 0.06 or a stringent upper limit of 0.07 is the current consensus for a good fit (38). The Weighted Root-Mean-Square Residual (WRMR) uses a variance-weighted approach (39). The WRMR statistic of less than 1.0 indicates a good fit. We judged the magnitude of correlation coefficients according to Cohen (40), where the effect size of 0.1 is considered small, 0.3 medium, and 0.5 large.
3. Results
3.1. Demographic and Clinical Characteristics
In total, 2,076 dental patients completed OHIP and PROMIS v.1.1 Global Health PROMs (Table 1). Patients had a mean age of 54.7 (16.2) years. The number of patients who also completed PROMIS v.1.0 Emotional Distress - Depression was 2,049 dental patients (mean age (SD): 54.8 (16.2)), of which 1,239 were females (59.7%).
Table 1.
Dental patients’ demographic and clinical characteristics.
| Dental patients (n=2,076) | mean (SD) or % |
|---|---|
| Demographics | |
| Gender (female) | 59.7 |
| Age (years) | 54.7 (16.2) |
| Language | |
| English | 84.5 |
| Spanish | 15.5 |
| Ethnicity | |
| Hispanic or Latino | 12.3 |
| Unknown | 87.7 |
| Self-reported oral health | |
| Excellent | 6.5 |
| Very good | 24.1 |
| Good | 35.2 |
| Moderate | 25.6 |
| Poor | 8.5 |
| Self-reported general health | |
| Excellent | 10.3 |
| Very good | 36.8 |
| Good | 38.4 |
| Moderate | 13.0 |
| Poor | 1.3 |
| OHIP summary scores | |
| OHIP-49 | 32.0 (32.3) |
| OHIP-14 | 7.7 (9.4) |
| OHIP-5 | 3.4 (3.7) |
| OHIP-49 dimensional scores | |
| Oral Function | 6.4 (7.6) |
| Orofacial Pain | 6.0 (5.7) |
| Orofacial Appearance | 6.9 (7.0) |
| Psychosocial Impact | 7.8 (12.0) |
| PROMIS v.1.1 Global Health dimensional scores | |
| Physical Health | 15.3 (2.9) |
| Mental Health | 15.1 (3.0) |
Legend: SD=standard deviation; OHIP=Oral Health Impact Profile; PROMIS=Patient-Reported Outcomes Information System
3.2. Model 1
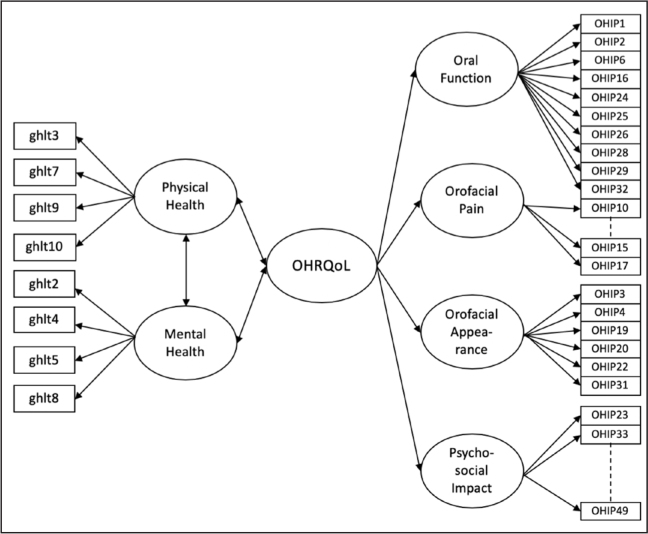
For this model, all correlation coefficients displayed in Table 4 were positive and significant (p<0.05). The correlation between the OHRQoL score and the two HRQoL scores was “large,” as reported by Cohen, i.e. 0.55 and 0.51 for Physical Health and Mental Health, respectively (Figure 1, Table 2).
Table 4.
Estimated correlation matrix for first and second-order factors from structural equation modeling confirmatory factor analysis for Model 2.
| Factors | HRQoL | Physical Health | Mental Health | OHRQoL | Oral Function | Orofacial Appearance | Orofacial Pain | Psychosocial Impact |
|---|---|---|---|---|---|---|---|---|
| HRQoL | 1.00 | |||||||
| Physical Health | 0.98 | 1.00 | ||||||
| Mental Health | 0.90 | 0.89 | 1.00 | |||||
| OHRQoL | 0.56 | 0.55 | 0.51 | 1.00 | ||||
| Oral Function | 0.46 | 0.45 | 0.41 | 0.81 | 1.00 | |||
| Orofacial Appearance | 0.50 | 0.49 | 0.45 | 0.88 | 0.72 | 1.00 | ||
| Orofacial Pain | 0.47 | 0.46 | 0.42 | 0.83 | 0.67 | 0.73 | 1.00 | |
| Psychosocial Impact | 0.55 | 0.54 | 0.50 | 0.98 | 0.79 | 0.86 | 0.81 | 1.00 |
Note: The highlighted correlations are the only correlations that are specified by Model 2. All other correlations between all latent variables and dimensions were generated but were not specified by the model.
Figure 1.
Structural equation modeling confirmatory factor analysis for correlations of one second-ordered global OHRQoL measure (OHIP-49) and two first-ordered HRQoL measures (PROMIS v.1.1 Global Health).
Note: Circles reflect latent constructs, and rectangles represent measured variables.
Table 2.
Model 1 estimated correlation matrix for first and second-order OHRQoL and HRQoL factors from structural equation modeling confirmatory factor analysis.
| Factors | Physical Health | Mental Health | OHRQoL | Oral Function | Orofacial Appearance | Orofacial Pain | Psychosocial Impact |
|---|---|---|---|---|---|---|---|
| Physical Health | 1.00 | ||||||
| Mental Health | 0.89 | 1.00 | |||||
| OHRQoL | 0.55 | 0.51 | 1.00 | ||||
| Oral Function | 0.45 | 0.41 | 0.81 | 1.00 | |||
| Orofacial Appearance | 0.49 | 0.45 | 0.88 | 0.72 | 1.00 | ||
| Orofacial Pain | 0.46 | 0.42 | 0.83 | 0.67 | 0.73 | 1.00 | |
| Psychosocial Impact | 0.54 | 0.50 | 0.98 | 0.79 | 0.86 | 0.81 | 1.00 |
Note: The highlighted correlations are the only correlations that are specified by Model 1. All other correlations between all latent variables and dimensions were generated but were not specified by the model.
The two HRQoL factors, i.e. Physical and Mental Health, correlated almost perfectly (r=0.98). All four first-order OHRQoL scores correlated very strongly to almost perfectly with the second-order OHRQoL score (r=0.81–0.98). The four first-order OHRQoL scores strongly correlated with each other (r=0.67–0.81).
The proportion of variance in the Physical and Mental Health of HRQoL explained by OHRQoL was R2 for Physical Health of HRQoL and equaled 0.30. The R2 for the Mental Health of HRQoL equaled 0.26. We present the Model Fit statistics for Model 1 in Table 3.
Table 3.
Model Fit Indices of Model 1, Model 2, and Model 3.
| Model Fit Indices | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Index value | |||
| Comparative Fit Index (CFI) | 0.96 | 0.96 | 0.94 |
| Tucker-Lewis Index (TLI) | 0.95 | 0.95 | 0.94 |
| Standardized Root Mean Square Residual (RMSEA) | 0.06 (95%CI:0.063–0.065) | 0.06 (95%CI:0.063–0.065) | 0.06 (95%CI:0.061–0.063) |
| Weighted Root Mean Square Residual (WRMR) | 3.14 | 3.14 | 3.16 |
Note: The highlighted correlations are the only correlations that are specified by Model 1. All other correlations between all latent variables and dimensions were generated but were not specified by the model.
3.3. Model 2
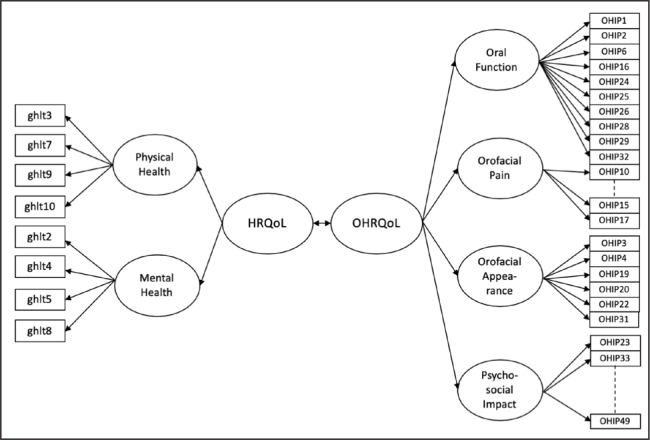
Compared to Model 1, Model 2 contains an overall HRQoL factor (Figure 2).
Figure 2.
Structural Equation Modeling Path Analysis for correlations of one second-ordered global OHRQoL measure (OHIP-49) and two first-ordered HRQoL measures (PROMIS v.1.1 Global Health).
Note: Circles reflect latent constructs, and rectangles represent measured variables.
In this model, HRQoL and OHRQoL are represented by their two or four dimensions, respectively. We present the model fit statistics for Model 2 in Table 3. The added level of complexity with a second-order global HRQoL factor did not alter the exactness of the model fit. In line with Cohen’s r guidelines, the correlation of 0.56 between OHRQoL and HRQoL scores was “large.” All correlation coefficients for Model 2 are displayed in Table 4.
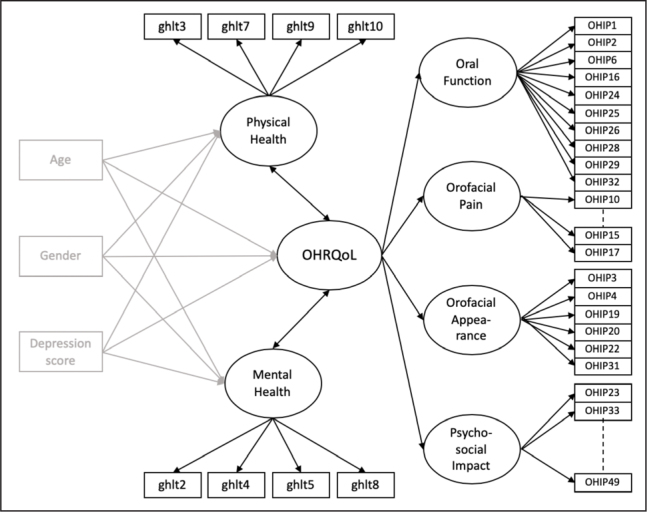
3.4. Model 3
The SEM path model was specified for Model 2 with the global HRQoL and OHRQoL second-order factors regressed on the patients’ age, gender, and depression score. The strong correlation between Physical Health and global HRQoL (0.98 in Model 2) resulted in linear dependency between these two factors when we included additional variables in the model. Therefore, we used the model conceptualizing HRQoL with two factors and OHRQoL with four factors, and an overall OHRQoL factor (Figure 3).
Figure 3.
Structural Equation Modeling Path Analysis for correlations of one second-ordered global OHRQoL measure (OHIP-49) and two first-ordered HRQoL measures (PROMIS v.1.1 Global Health). Note: Circles reflect latent constructs, and rectangles represent measured variables.
Note: Circles reflect latent constructs, and rectangles represent measured variables.
We presented the Model Fit statistics in Table 3. Patients’ older age was significantly (p<0.001) associated with increased OHRQoL and decreased Physical Health factor scores and was not significantly associated with Mental Health. Female gender was associated with significantly lower Physical and Mental health scores but was not significantly associated with the OHRQoL score. Increased depression score (more depression) was significantly associated with decreased OHRQoL, Physical, and Mental Health factor scores (Table 5).
Table 5.
The structural equation modeling path analysis model estimated standardized regression coefficients (SE). Standardized estimates are for the mean change in factor score for one standard deviation increase in the independent variable.
| Independent variables | Factors | |||||
|---|---|---|---|---|---|---|
| OHRQoL | Physical Health | Mental Health | ||||
| Estimate (SE) | p-value | Estimate (SE) | p-value | Estimate (SE) | p-value | |
| Age | 0.052 (0.023) | 0.024 | −0.167 (0.022) | <0.001 | 0.007 (0.018) | 0.704 |
| Female | −0.029 (0.023) | 0.195 | −0.101 (0.022) | <0.001 | −0.055 (0.018) | 0.003 |
| Depression score | −0.410 (0.019) | <0.001 | −0.520 (0.018) | <0.001 | −0.663 (0.012) | <0.001 |
Legend: SE=standard error; OHRQoL=Oral Health-Related Quality of Life.
The magnitude of correlations between the factors in this model was significant (p<0.05) and similar to those of Model 1. According to Cohen’s r, the association between the two HRQoL scores (Physical and Mental Health) of 0.87 was “large,” as well as correlations of all four first-order OHRQoL scores with the second-order global OHRQoL score which ranged from 0.83 to 0.97, and with each other ranging from 0.68 to 0.86. The correlation between the global OHRQoL score and the two HRQoL scores was “large,” i.e., 0.52 and 0.47 for Physical Health and Mental Health, respectively (Table 6).
Table 6.
Estimated correlation matrix for first and second-order factors adjusted for age, gender, and depression score for Model 3.
| Factors | Physical Health | Mental Health | OHRQoL | Oral Function | Orofacial Appearance | Orofacial Pain | Psychosocial Impact |
|---|---|---|---|---|---|---|---|
| Physical Health | 1.00 | ||||||
| Mental Health | 0.87 | 1.00 | |||||
| OHRQoL | 0.52 | 0.47 | 1.00 | ||||
| Oral Function | 0.43 | 0.39 | 0.83 | 1.00 | |||
| Orofacial Appearance | 0.46 | 0.42 | 0.88 | 0.73 | 1.00 | ||
| Orofacial Pain | 0.43 | 0.39 | 0.83 | 0.68 | 0.73 | 1.00 | |
| Psychosocial Impact | 0.50 | 0.46 | 0.97 | 0.80 | 0.86 | 0.80 | 1.00 |
Note: The highlighted correlations are the only correlations that are specified by Model 3. All other correlations estimates were generated but were not specified by the model.
The proportion of variance in Physical and Mental Health explained by OHRQoL, adjusted for effect of age, gender, and depression were R2 for the Physical Health of HRQoL and equaled 0.27. The R2 for Mental Health of HRQoL equaled 0.22.
4. Discussion
The magnitude of the correlation between the four-dimensional OHRQoL and HRQoL constructs was large in our dental patient population. This is the first study in which PROMIS PROMs for HRQoL evaluation was used to assess self-reported general health in a dental patient population. The included dental patients are representative of the full range of patients attending dental practices. OHIP-49 and PROMIS v.1.1 Global Health are psychometrically sound and valid PROMs.
Zimmer and co-authors explained that about 10% of the OHRQoL information is incorporated into HRQoL (9). Nevertheless, they did not take into account that measurement error can weaken a correlation evaluated with short PROMs. Reissmann and co-authors found a higher correlation coefficient compared to the previous study (10), explaining 29% of the information contained in HRQoL. While our dental patient population is similar to the subjects Reissmann and co-authors investigated, our measurement tools capturing OHRQoL and HRQoL constructs differ from their study. Reissmann et al. used OHIP-49 and SF-36 PROMs, while we used OHIP-49 and PROMIS v.1.1 Global Health PROMs. Similarly, the study by Ranfl and Zaletel-Kragelj used single items for the evaluation of the connection between dentate status and self-assessed general health on a large sample of general population subjects (11). Like us, they also considered the possibility of variation in data when adjusted for confounders such as age, gender, educational level, type of work, and self-classified social class (11).
Because the stomatognathic system is an essential component of the body, from a biological point of view, OHRQoL is embedded in the HRQoL construct. From a conceptual perspective, the HRQoL construct is broad, general, and not linked to body elements or organs. Also, the high correlation between Mental Health and Physical Health in our study indicates that in typical dental patients, the two scores measure the same underlying construct, i.e. the HRQoL construct. Oral disorders may have different outcomes. When patients perceive “physical” impacts in the OHRQoL area, their functional and psychosocial oral health deteriorate. This also worsens their HRQoL, but to a minor degree. This is of importance in clinical dentistry as well as in oral public health studies. For example, temporomandibular disorders (41) impact a patient’s oral health and may also influence overall health substantially. In other instances, oral disorders may also present as part of systemic disease. Dementia can affect patients’ oral health (42). A patient with oral cancer and resected mandible certainly has oral health-related psychosocial impacts, but mental health is also affected (43). Thus OHRQoL and HRQoL PROMs should be able to represent such information. A substantial overlap between OHRQoL and HRQoL should be detected if dental patients’ present both oral impairments and systemic effects, oral impairments with systemic effects, or a more general element, e.g. health behavior, that can influence oral and systemic diseases (44,45,46). On the contrary, the correlation should be small in a dental patient population with a localized oral disease not associated with systemic disease.
A limitation of the study could be the oversampling of Spanish-speakers, and we have not provided separate analyses for the two language groups. However, we did not see a reason why the OHRQoL-HRQoL relationship in those patients would differ. In contrast to modeling HRQoL or OHRQoL with its indicators, i.e. items, we used the depression instrument’s items and derived a summary score to be included in the SEM. While Mplus can handle missing data for the HRQoL and OHRQoL in the analysis, we imputed missing depression items to include patients with sufficient depression information. Overall, the amount of missing data was low, generating a limited potential to change the observed results. Especially for the two quality of life latent variables, we had sufficient information to characterize them. Adjustment by age, gender, and depression did not change the HRQoL-OHRQoL relationship substantially. Therefore, it seems unlikely that the small amount of missing depression information would alter the observed results substantially. We conceptualized OHRQoL as consisting of four dimensions. Consequently, we excluded three OHIP items related to denture wearers and five to the symptom status. While this concept should provide improved OHRQoL structural validity, it can limit comparability with other studies using 49 OHIP items.
The major strength of this study is that we used a highly precise statistical technique that allows modeling the variables directly by eliminating measurement errors that occur during data analysis (34, 43). Even though we provided valuable insights into the magnitude of overlap between OHRQoL and HRQoL constructs, further research of the magnitude between the two constructs’ dimensions can be explored, e.g. OHRQoL dimensions-HRQoL and HRQoL dimensions-OHRQoL. A future research synthesis that would summarize and analyze the correlations of available and future studies would provide a thorough understanding of the association between the two constructs of interest.
5. Conclusions
Our study provides good evidence that OHRQoL and HRQoL constructs overlap substantially, which is informative for public health because in the OHRQoL assessment, valuable medical information is embedded and vice versa; low HRQoL can be indicative also of impaired oral health.
Acknowledgment
The authors wish to thank Ms. Kathleen M. Patka, Executive Office and Administrative Specialist, Division of Oral Medicine, School of Dentistry, University of Minnesota, for proofreading the manuscript.
Footnotes
CONFLICTS OF INTEREST
The authors declare that no conflicts of interest exist.
FUNDING
The study data came from a research project (R01DE022331), supported by the National Institute of Dental and Craniofacial Research, USA.
ETHICAL APPROVAL
Reviewed and approved by the Institutional Review Board of the HealthPartners Institute, Minnesota, USA (Study Number A11–136).
References
- 1.Dental Health Foundation. Links between oral & general health. The Mouth-Body Connection. Accessed August 31, 2019 at: https://www.dentalhealth.ie/dentalhealth/causes/general.html .
- 2.Dental Health Services Victoria. Links between oral health and general health - the case for action. Accessed August 31, 2019 at: https://mail.google.com/mail/u/1/#inbox/FMfcgxwDrHnCVtfLHjxpTVwHlGGwcTTm?projector=1&messagePartId=0.1 .
- 3.Bennadi D, Reddy C. Oral health related qualtiy of life. J Int Soc Prev Community Dent. 2013;3:1–6. doi: 10.4103/2231-0762.115700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sischo L, Broder HL. Oral health-related quality of life: what, why, how, and future implications. J Dent Res. 2011;90:1264–70. doi: 10.1177/0022034511399918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen LK, Jago JD. Toward the formulation of sociodental indicators. Int J Heal Serv. 1976;6:681–98. doi: 10.2190/LE7A-UGBW-J3NR-Q992. [DOI] [PubMed] [Google Scholar]
- 6.Petek D, Petek-Ster M, Tusek-Bunc K. Health behavior and health-related quality of life in patients with a high risk of cardiovascular disease. Zdr Varst. 2018;57:39–46. doi: 10.2478/sjph-2018-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Petersen PE. The world oral health report 2003: continuous improvement of oral health in the 21st century - the approach of the WHO global oral health programme. Community Dent Oral Epidemiol. 2003;31(Suppl 1):3–23. doi: 10.1046/j..2003.com122.x. [DOI] [PubMed] [Google Scholar]
- 8.Kieffer JM, Hoogstraten J. Linking oral health, general health, and quality of life. Eur J Oral Sci. 2008;116:445–50. doi: 10.1111/j.1600-0722.2008.00564.x. [DOI] [PubMed] [Google Scholar]
- 9.Zimmer S, Bergmann N, Gabrun E, Barthel C, Raab W, Rüffer JU. Association between oral health-related and general health-related quality of life in subjects attending dental offices in Germany. J Public Health Dent. 2010;70:167–70. doi: 10.1111/j.1752-7325.2009.00158.x. [DOI] [PubMed] [Google Scholar]
- 10.Reissmann DR, John MT, Schierz O, Kriston L, Hinz A. Association between perceived oral and general health. J Dent. 2013;41:581–9. doi: 10.1016/j.jdent.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 11.Ranfl M, Zaletel-Kragelj L. Assessment of the association between dentate status and self-rated general health. Zdr Varst. 2017;56:131–9. doi: 10.1515/sjph-2017-0017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.PROMIS Cooperative Group. List of adult measures. Accessed August 31, 2019 at: http://www.healthmeasures.net/explore-measurement-systems/promis/intro-to-promis/list-of-adult-measures .
- 13.Paravlić A, Pišot S, Mitić P. Validation of the slovenian version of motor imagery questionnaire 3 (MIQ-3): promising tool in modern comprehensive rehabilitation practice. Zdr Varst. 2018;57:201–10. doi: 10.2478/sjph-2018-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stern B, Socan G, Rener-Sitar K, Kukec A, Zaletel-Kragelj L. Validation of the Slovenian version of short sense of coherence questionnaire (SOC-13) in multiple sclerosis patients. Zdr Varst. 2019;58:31–9. doi: 10.2478/sjph-2019-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.PROMIS Cooperative Group. Patient-reported outcomes measurement information system (PROMIS). PROMIS user manual (Version 1.1) Accessed August 31, 2019 at: www.nihpromis.org .
- 16.Sekulic S, Theis-Mahon N, Rener-Sitar K. A systematic scoping review of oral health models. Qual Life Res. 2019;28:2651–68. doi: 10.1007/s11136-019-02206-9. [DOI] [PubMed] [Google Scholar]
- 17.John MT, Reissmann DR, Feuerstahler L, Waller N, Baba K, Larsson P. et al. Exploratory factor analysis of the oral health impact profile. J Oral Rehabil. 2014;41:635–43. doi: 10.1111/joor.12192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.John MT, Feuerstahler L, Waller N, Baba K, Larsson P, Čelebić A. et al. Confirmatory factor analysis of the oral health impact profile. J Oral Rehabil. 2014;41:644–52. doi: 10.1111/joor.12191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.John MT, Reissmann DR, Čelebić A, Baba K, Kende D, Larsson P. et al. Integration of oral health-related quality of life instruments. J Dent. 2016;53:38–43. doi: 10.1016/j.jdent.2016.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.John MT, Rener-Sitar K, Baba K, Čelebić A, Larsson P, Szabo G. et al. Patterns of impaired oral health-related quality of life dimensions. J Oral Rehabil. 2016;43:519–27. doi: 10.1111/joor.12396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.John MT, Reissmann DR, Feuerstahler L, Waller N, Baba K, Larsson P. et al. Factor analyses of the oral health impact profile - overview and studied population. J Prosthodont Res. 2014;58:26–34. doi: 10.1016/j.jpor.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.John MT. Health outcomes reported by dental patients. J Evid Based Dent Pract. 2018;18:332–5. doi: 10.1016/j.jebdp.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 23.Mittal H, John MT, Sekulić S, Theis-Mahon N, Rener-Sitar K. Patient-reported outcome measures for adult dental patients: a systematic review. J Evid Based Dent Pract. 2019;19:53–70. doi: 10.1016/j.jebdp.2018.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Slade GD, Spencer AJ. Development and evaluation of the oral health impact profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 25.Allen PF, O’Sullivan M, Locker D. Determining the minimally important difference for the oral health impact profile-20. Eur J Oral Sci. 2009;117:129–34. doi: 10.1111/j.1600-0722.2009.00610.x. [DOI] [PubMed] [Google Scholar]
- 26.Allen F, Locker D. A modified short version of the oral health impact profile for assessing health-related quality of life in edentulous adults. Int J Prosthodont. 2002;15:446–50. [PubMed] [Google Scholar]
- 27.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–90. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 28.Naik A, John MT, Kohli NM, Self K, Flynn P. Validation of the English-language version of 5-item oral health impact profile. J Prosthodont Res. 2016;60:85–91. doi: 10.1016/j.jpor.2015.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.John MT, Baba K, Bekes K, Bondemark L, Fueki K, Häggman-Henrikson B, Scoring recommendations for the oral health impact profile. J Evid Based Dent Pract. 2019. In press. [DOI] [PMC free article] [PubMed]
- 30.PROMIS Cooperative Group. Global health. Accessed August 31, 2019 at: http://www.healthmeasures.net/images/PROMIS/manuals/PROMIS_Global_Scoring_Manual.pdf .
- 31.Leõn S, Bravo-Cavicchioli D, Giacaman RA, Correa-Beltrán G, Albala C. Validation of the spanish version of the oral health impact profile to assess an association between quality of life and oral health of elderly chileans. Gerodontology. 2016;33:97–105. doi: 10.1111/ger.12124. [DOI] [PubMed] [Google Scholar]
- 32.PROMIS Cooperative Group. Available translations. Accessed August 31, 2019 at: http://www.healthmeasures.net/explore-measurement-systems/promis/intro-to-promis/available-translations#targetText=PROMIS®. measures are available, target language (linguistic validation).
- 33.Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D. et al. Item banks for measuring emotional distress from the patient-reported outcomes measurement information system (PROMIS®): depression, anxiety, and anger. Assessment. 2011;18:263–83. doi: 10.1177/1073191111411667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Baraldi AN, Enders CK. An introduction to modern missing data analyses. J Sch Psychol. 2010;48:5–37. doi: 10.1016/j.jsp.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 35.Kline RB. Principles and practice of structural equation modeling. New York: Guilford Press; 2011. [Google Scholar]
- 36.MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychol Methods. 1996;1:130–49. [Google Scholar]
- 37.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model A Multidiscip J. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 38.Steiger J. Understanding the limitations of global fit assessment in structural equation modeling. Pers Individ Dif. 2007;42:893–8. doi: 10.1016/j.paid.2006.09.017. [DOI] [Google Scholar]
- 39.Cook KF, Kallen MA, Amtmann D. Having a fit: impact of number of items and distribution of data on traditional criteria for assessing IRT’s unidimensionality assumption. Qual Life Res. 2009;18:447–60. doi: 10.1007/s11136-009-9464-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hemphill JF. Interpreting the magnitudes of correlation coefficients. Am Psychol. 2003;58:78–9. doi: 10.1037/0003-066x.58.1.78. [DOI] [PubMed] [Google Scholar]
- 41.Ciancaglini R, Radaelli G. The relationship between headache and symptoms of temporomandibular disorder in the general population. J Dent. 2001;29:93–8. doi: 10.1016/s0300-5712(00)00042-7. [DOI] [PubMed] [Google Scholar]
- 42.Adam H, Preston AJ. The oral health of individuals with dementia in nursing homes. Gerodontology. 2006;23:99–105. doi: 10.1111/j.1741-2358.2006.00118.x. [DOI] [PubMed] [Google Scholar]
- 43.Schwentner I, Obrist P, Thumfart W, Sprinzl G. Distant metastasis of parotid gland tumors. Acta Otolaryngol. 2006;126:340–5. doi: 10.1080/00016480500401035. [DOI] [PubMed] [Google Scholar]
- 44.Ahacic K, Trygged S, Kåreholt I. Income and education as predictors of stroke mortality after the survival of a first stroke. Stroke Res Treat. 2012;2012:1–6. doi: 10.1155/2012/983145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Conway DI, Petticrew M, Marlborough H, Berthiller J, Hashibe M, Macpherson LMD. Socioeconomic inequalities and oral cancer risk: a systematic review and meta-analysis of case-control studies. Int J Cancer. 2008;122:2811–9. doi: 10.1002/ijc.23430. [DOI] [PubMed] [Google Scholar]
- 46.Edelstein BL. Disparities in oral health and access to care: findings of national surveys. Ambul Pediatr. 2002;2(Suppl 2):141–7. doi: 10.1367/1539-4409(2002)002<0141:DIOHAA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 47.Hoyle RH, Isherwood JC. Reporting results from structural equation modeling analyses in archives of scientific psychology. Arch Sci Psychol. 2013;1:14–22. doi: 10.1037/arc0000004. [DOI] [PMC free article] [PubMed] [Google Scholar]