Abstract
Despite the substantial burden of HIV in Africa, and the knowledge that depression causes worse HIV outcomes, the burden of depression in people living with HIV in Africa is unknown.
We searched Pubmed and four other databases using key terms: depression, Africa, HIV, and prevalence from 2008 to 2018. We summarized depression prevalence by country. We estimated the burden of depression using our prevalence data and 2018 UNAIDS HIV estimates.
Our search yielded 70 articles across 16 African countries. The overall prevalence of major depression in those HIV-infected using a diagnostic interview was 15.3% (95%CI, 12.5-17.1%). We estimate that 3.63 million (99.7% CI, 3.15-4.19 million) individuals with HIV in Sub-Saharan Africa have major depression and provide country-level estimates. We estimate that 1.57 million (99.7%CI, 1.37-1.82 million) DALYs are lost among people with depression and HIV in Sub-Saharan Africa.
There is a significant burden of depression in Africans with HIV. Further work to screen for and treat depression in Sub-Saharan Africa is needed to improve HIV outcomes and achieve the 90-90-90 UNAIDS goals.
Keywords: HIV, depression, Sub-Saharan Africa, prevalence, burden of disease
Resumen
A pesar del problema sustancial del VIH en África y el conocimiento de que la depresión causa peores resultados en pacienes con VIH, se desconoce el impacto especifico de la depresión en las personas que viven con el VIH en África.
Se realizaron búsquedas en Pubmed y otras cuatro bases de datos utilizando términos clave: depresión, África, VIH y prevalencia desde 2008 hasta 2018. Resumimos la prevalencia de depresión por país. Estimamos el impacto de la depresión utilizando nuestros datos de prevalencia y las estimaciones de VIH de ONUSIDA para 2018.
Nuestra búsqueda indetifico 70 artículos en 16 países africanos. La prevalencia general de depresión en las personas infectadas por el VIH durante entrevista de diagnóstico fue del 15,3% (IC del 95%, 12,5-17,1%). Estimamos que 3.63 millones (99.7% CI, 3.15-4.19 millones) de personas con VIH en África Subsahariana sufren de depresión y proporcionamos estimaciones a nivel país. Estimamos que se pierden 1,57 millones (IC del 99,7%, 1,37-1,82 millones) de AVAD entre las personas con depresión y VIH en el África subsahariana. La depresión tiene un impacto significativo en los africanos con VIH. Se necesitan más estudios para detectar y tratar la depresión en África subsahariana con el fin de mejorar los resultados del VIH y alcanzar los objetivos 90-90-90 de ONUSIDA.
Background
Depression is estimated to cause 2.2 million excess deaths globally in 2010 from suicide or worsening of comorbid diseases.1 Depression is significantly more common in people living with HIV, where the prevalence estimates range widely from 13% to 78% compared with 5% prevalence in the general population.2,3 Persons with HIV and depression are less likely to achieve good antiretroviral therapy (ART) adherence, more likely to have clinical progression regardless of adherence behavior,4 and more likely to develop virologic failure.2,5
Despite the known worse outcomes and quality of life, depression in HIV is often overlooked in clinical practice.6,7 One study in the USA showed that only half of those depressed carried the diagnosis.8 The diagnosis of depression is even less common in low-resource countries. A Nigerian studied showed that no patients with depression carried the diagnosis.9 There are many reasons for this including busy clinics, limited resources for mental health practitioners, and a difference in the expected versus actual presentation of depression in people living with HIV.6,10,11
To improve screening and diagnosis of depression, a better understand of the burden of depression is needed, particularly in sub-Saharan Africa which has the most substantial burden of HIV.12 The countries in sub-Saharan Africa are low and middle income, underscoring the need for quantifiable data to justify spending resources on mental health care.6 Given the dearth of mental health practitioners in sub-Saharan Africa, a long term commitment to training and retaining professionals or ways to task-shift would be required to improve the situation.13
While there have been some global estimates of depression in HIV,2,3 there are a paucity of data from Africa with just one multi-country survey done14 and several single-country, often single health center studies.15-22 To date, there has been one review on depression prevalence in people living with HIV in Arica.23 This analysis presented the prevalence of depression by the MINI international neuropsychiatric interview (MINI) or other diagnostic interview and presented depressive symptoms using depression screening tools by tool. However, through limiting the inclusion criteria by diagnostic tool, the number of studies and countries included is limited.
Additionally, this review prior review did not provide country or region level data nor provide the burden of depression. Given that the ministry of health in each country makes spending decisions on an individual basis, we wanted to provide depression prevalence and burden among those HIV-infected by country and region. We also present both the prevalence of major depression as well as depressive symptoms, as the diagnosis of major depression is more precise, but a depressive symptom screening tool is most likely to be the only metric used in HIV clinics. We hope this will better inform country-level resource allocation for mental health services.
Our objective was to perform a systematic review and meta-analysis of the prevalence of depression in those with HIV in Africa to estimate the burden of depression, using multiple metrics, among persons HIV-infected by country in Africa.
Methods
Systematic Search
The current systematic review and meta-analysis were conducted following the preferred reporting items of systematic reviews and meta-analyses (PRISMA) guidelines. Medline/Pubmed was searched using the terms HIV and Africa and Depression, and limited to articles in English involving human adults. This resulted in the following search string ((“depressive disorder”[MeSH Terms] OR (“depressive”[AII Fields] AND “disorder”[AII Fields]) OR “depressive disorder”[AII Fields] OR “depression”[AII Fields] OR “depression”[MeSH Terms]) AND (“hiv”[MeSH Terms] OR “hiv”[AII Fields]) AND (“africa”[MeSH Terms] OR “africa”[AII Fields])) AND “humans”[MeSH Terms] AND English24 AND “adult”[MeSH Terms].
Additionally, Scopus, Web of Science, Embase, and African Journals Online were searched using the same terms HIV, depression, and Africa. The dates of all searches were limited to 2008-2018. We compared the articles between searches and eliminated duplicates.
Inclusion/Exclusion Criteria
Included articles: 1) measured depression in humans using standardized and validated diagnostic interviews, screening tools, or psychological distress tools (there were no restrictions on severity of depression or treatment history), 2) included adult outpatients living with HIV, 3) were conducted in Africa, and 4) were valid cross-sectional or cohort studies, which presented numbers for depression prevalence (number depressed and total evaluated).
Articles were excluded if they were: 1) peripartum depression studies, 2) pediatric studies, 3) qualitative studies, 4) unpublished data, conference abstracts, or case reports, 5) multiple reports from the same data set (only the most recent study was included as it was felt to be the most up-to-date estimate of prevalence), 6) those with sub-populations such as HIV-TB co-infection, and 7) those at HIV testing it would be challenging to distinguish adjustment disorder from depression. These articles were excluded as there was a recent review on peripartum depression,25 and as depression presentation and screening is very different in children. Articles that were case-control studies or interventions, which do not give the number of those screened, were excluded. We excluded articles with the sub-population of just women as most studies over-represented women; however, we included articles with only older adults as they are generally under-represented in studies.
We allowed a wide range of depression tools to have broad applicability and cover many countries across the continent. We parsed the prevalence by the diagnostic method to standardized interviews that diagnosed major depressive disorder, screening tools specific for depressive symptoms, and tools measuring general psychological distress. All prevalence numbers are point prevalences.
Data Extraction and Statistical Analysis
The first author (SL) extracted data using a standardized data extraction spreadsheet from included studies to evaluate study characteristics and risk of bias systematically. When there were concerns about study generalizability (i.e., risk of bias of selected, non-generalizable populations), the first author discussed the concerns with other authors (DB and NN), and a consensus was reached.
From each selected article, we extracted data on each study population, country, year, and study design. Additionally, we assessed the prevalence data presented, the depression scale(s) utilized, sample size, inclusion criteria, CD4 counts, ART status, and any control groups used. Duplicate references were identified and removed. Descriptive comparisons were compiled using Microsoft Excel. We performed a quantitative analysis using Microsoft Excel and IBM SPSS. We generated maps via GunnMap.26
We calculated the weighted prevalence by summing the number of depressed participants and dividing by the total number of participants in each study or group of studies, using numerical counts from each article. The studies were organized by country and demographic factors. We examined the prevalence comparing a diagnostic interview and a depression screening tool in the countries that used both. Next, we evaluated the prevalence of depression by ART status. The ART status was recorded as a binary variable (i.e., on ART or not). We then calculated a weighted risk difference and relative risk, both with confidence intervals. The CD4 count mean or median versus prevalence were graphed for each study, and the Pearson r2 correlation coefficient calculated using Microsoft Excel 2016. Next, we looked at studies that compared those with HIV and controls. We also noted those studies with comparisons to HIV negative people at HIV testing, where data were available.
Evaluation for Bias
Next, we evaluated if our use of articles with different tools altered the prevalence of depression. We graphed a funnel plot to assess for publication bias of prevalence by the size of the study. We also generated scatter plots of the prevalence by year. Finally, we graphed the prevalence by the screening or diagnostic method.
The Burden of Depression in Absolute Numbers
Next, we estimated the burden of overall depressive symptoms among HIV-infected persons in sub-Saharan Africa. We used 2018 UNAIDS estimates for the number of HIV-infected adults 15 and older in sub-Saharan Africa, and by country.27 These were accessed on December 1, 2018, and are UNAIDS data for the calendar year 2017. We used standard β distributions for binomial data of estimate of depressive symptoms, and normal distribution for estimates of HIV prevalence with 95% confidence intervals for countries with data and 99.7% confidence intervals (3 standard deviations) for countries without published data using the depression prevalence from that region: Southern, East, and West/Central Africa. Using Microsoft Excel 2016, we randomly selected a value for each parameter within the appropriate distribution and used the combination of these values to estimate the number of HIV-infected persons with depression symptoms. Using 20,000 iterations, we obtained empirical distributions corresponding to posterior distributions calculated by Monte Carlo simulations for each country and region. These distributions were used to generate a point estimate (posterior mean) and Monte Carlo confidence intervals for the 99.7% confidence intervals. We used the estimated burdens to calculate the country-specific prevalence, the regional, and overall prevalence of depression in people with HIV in sub-Saharan Africa.
Review of Burden of Depression Measures
We next evaluated the general metrics of the burden of disease. We looked at which of the studies had follow-up data. We assessed what articles had measured disability-adjusted life years (DALY) or quality-adjusted life years (QALY), ART adherence, and viral suppression rates.
The Burden of Depression in Disability-Adjusted Life Years (DALYs)
Finally, we calculated the DALYs from our data. First, we found the studies which used PHQ-9 and presented the data by the severity of depression. We used this to calculate the prevalence of moderate and severe depression amongst those depressed. We then used the disability weights from those used in the Global Burden of Disease 2013 study to calculate DALYs associated with moderate to severe depression.28 Specifically, the disability weight for mild depression was 0.145 (95% CI, 0.099-0.209), for moderate depression was 0.396 (95%CI, 0.267-0.531), and severe depression was 0.658 (95%CI, 0.477-0.807).
Results
Search Outcomes
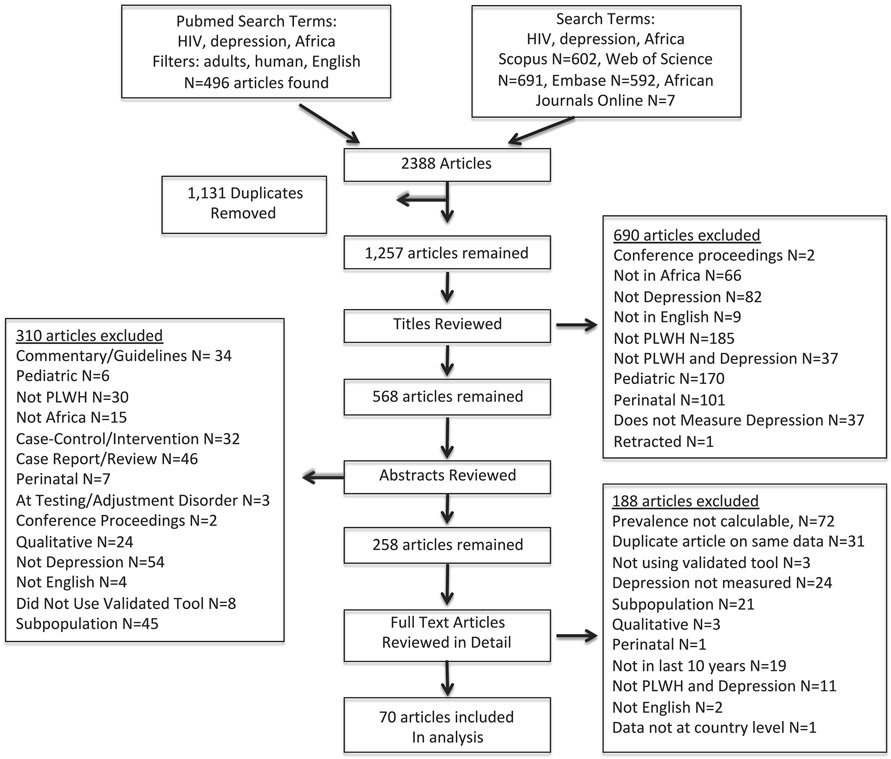
We completed our search on the prevalence of depression in HIV in Africa on August 4, 2018. Our PubMed search yielded 496 articles, our Scopus search yielded 602 articles, our Web of Science search yielded 691, Embase yielded 592 articles, and African Journals Online yielded 7 articles for a total of 2388 articles. In removing duplicates, we subjected each of the 1258 articles to each of the selection criteria with a title evaluation, of which 690 articles were excluded, leaving 568 articles. We reviewed the abstracts and removed 310 based on inclusion/exclusion criteria. Then, we reviewed the full texts of the remaining 258 and removed 189 more articles. Full search details are displayed in Figure 1.
Fig. 1.
Burden of Depression Search Strategy. Note: Search performed in August 2018
Our search to quantify the prevalence of depression in HIV-infected persons in Africa resulted in 70 articles, which we read and abstracted data per our criteria. The search revealed that the investigators used a variety of depression scales. We divided studies into those who measured depression using standardized, diagnostic interviews, studies using a depression-specific screening tool, and, finally, studies using a tool measuring generalized psychological distress. We provide full details of the articles in Supplemental Table 1 and the details on depression tools in Supplemental Table 2. We graphed depression prevalence by each article in Supplemental Figure 1.
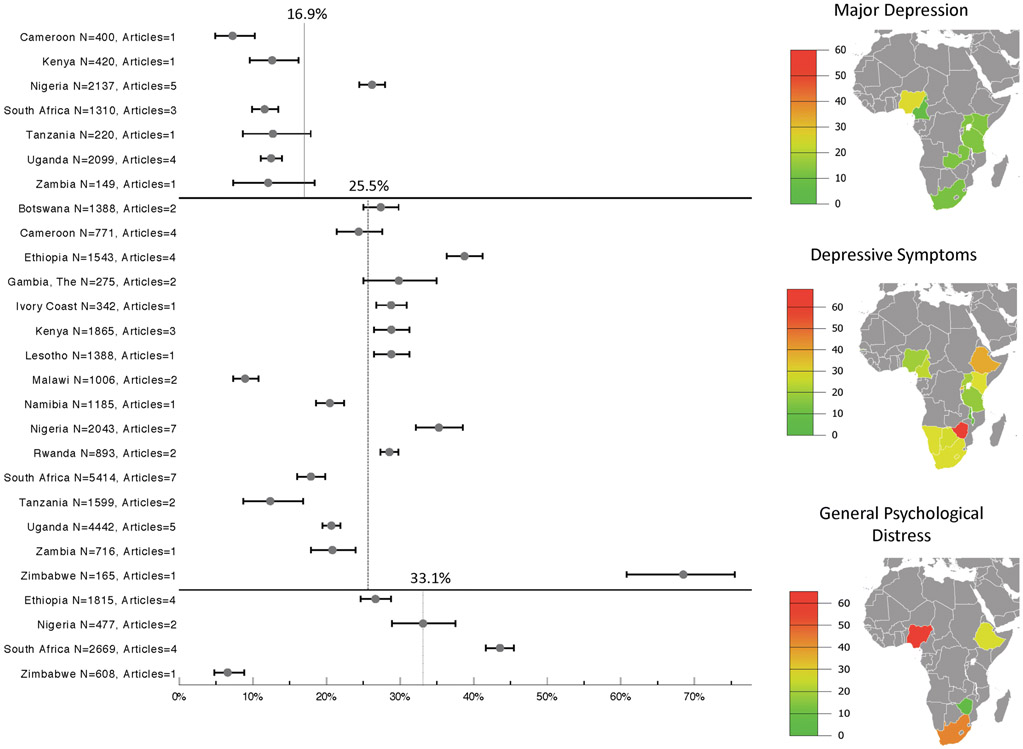
Prevalence of Depression
The prevalence of depression by country among HIV-infected persons was calculated using a diagnostic interview, a depression-specific screening tool, or general psychological distress (Supplemental Table 3-5). We found that the mean weighted prevalence of major depression was 16.8% (95%CI, 15.9-17.7%) using a diagnostic interview. The prevalence of depressive symptoms was 25.5% (95%CI, 24.9-26.0%) using a depression screening tool, and the prevalence of general psychological distress was 33.1% (95%CI, 31.9-34.4%). This data of weighted prevalence by country and diagnostic method is displayed via a map in Figure 2.
Fig. 2.
Prevalence of Depression in Africans Living with HIV by Country. Note: Major depression as defined by a standardized, diagnostic interview; Depressive symptoms as defined by a depression-specific screening tool; Generalized psychological distress as defined by a psychological distress screening tool. Error bars are the 95% CI
We next compared the prevalence of major depression and depressive symptoms in HIV-infected individuals using different depression tools within the same population. Specifically, we wanted to compare the prevalence of depression in countries, which was found using both a screening tool and a diagnostic interview. We found two cohorts from Nigeria and South Africa, which used both methods.9,29,30 In Nigeria, the prevalence of major depression by diagnostic interview was 23.9% (110/460) versus 24.8% (114/460) prevalence of depressive symptoms by screening tool. In South Africa, the prevalence of major depression by diagnostic interview was 13.5% (63/465) versus 44.7% (208/465) prevalence of depressive symptoms by screening tool. The weighted average prevalence for those countries was 16.3% (151/925) by interview compared to 34.8% (322/925) by screening tool. Thus, there is an 18.5% (95%CI, 14.6-22.4%) higher prevalence of depressive symptoms compared to major depression diagnosis by diagnostic interview.
Next, we compared the prevalence of depressive symptoms by ART status and CD4 count. Those not on ART had a prevalence of 28.8% (846/2942),31-36 compared with those on ART of 26.5% (3475/13097) prevalence of depressive symptoms.9,14-16,18-21,29,30,37-58 The relative difference was 8.7%, weighted absolute difference was 2.3% (95%CI, 0.5-4.1%; p=0.011), more depression for those not on ART. We examined the relationship between the prevalence of depressive symptoms and CD4 count, which can be seen in Supplemental Figure 2. The overall correlation was very weak and nonsignificant (R2= 0.00075 for mean CD4 and R2= 0.026 for median CD4 count)14,18,30,33,34,36,38,40,42,47,49-51,59-63
We next characterized differences in prevalence of depression by biological sex among 17 studies providing distribution by sex. In those studies using diagnostic interviews, men had a 12.9% (145/1121) prevalence of major depression while 17.7% (450/2547) of women had major depression (relative difference 36.6%, absolute difference: 4.8% 95%CI, 2.3-7.2%; p<0.001).35,37,59,64,65 In the studies that used a depression screening tool men had a 23.5% (776/3296) prevalence of depressive symptoms while women had a prevalence of 31.1% (1606/5169) (relative difference 32.0%, absolute difference: 7.6%, 95%CI, 5.7-9.5%; p<0.001).9,14,18,34,45,52,54,60-62,66,67 Overall, in this HIV-infected African population, women had more major depression and depressive symptoms than men.
We then wanted to understand the prevalence of major depression and depressive symptoms in those with HIV compared to the background prevalence of depression in the HIV-negative general population. This extra depression in the HIV-infected population is termed “excess depression.” To this end, we evaluated seven studies with control groups to find excess depression in those with HIV compared to controls from the general population.21,29,43,44,54,68-70 There were studies that used diagnostic interviews from Nigeria29 and Uganda,44 and studies that used a depression screening tool from Malawi,71 South Africa,69 Zambia,70 Zimbabwe, 43 and Cameroon.54 Those studies utilizing diagnostic interviews showed the prevalence of major depression in those with HIV was 30.0% compared with 18.1% in HIV-negative controls for a relative increase of 65.7% and an absolute difference of 11.9% (95%CI, 7.3-16.6%). Those studies utilizing screening tools found a prevalence of depressive symptoms of 27.8% in those with HIV and 13.5% in HIV-negative controls for a relative increase of 206% and an absolute difference of 14.3% (95%CI, 11.8-16.9%). Thus, depressive symptoms are two-fold more common in HIV-infected African adults than in general African populations.
Next, we assessed whether there was a potential publication bias based on the size of the study. Thus, we graphed the prevalence data in funnel plots, which show a funnel pattern, consistent with minimal bias, seen in the Supplemental Figure 3a and 3b for diagnostic interview and depression screening tool. Next, we graphed the prevalence of depression by diagnostic method, by year of data collection, and by year of publication Supplemental Figure 4. Overall there does not seem to be a relationship between prevalence and method or date. As such, there seems again to be minimal bias.
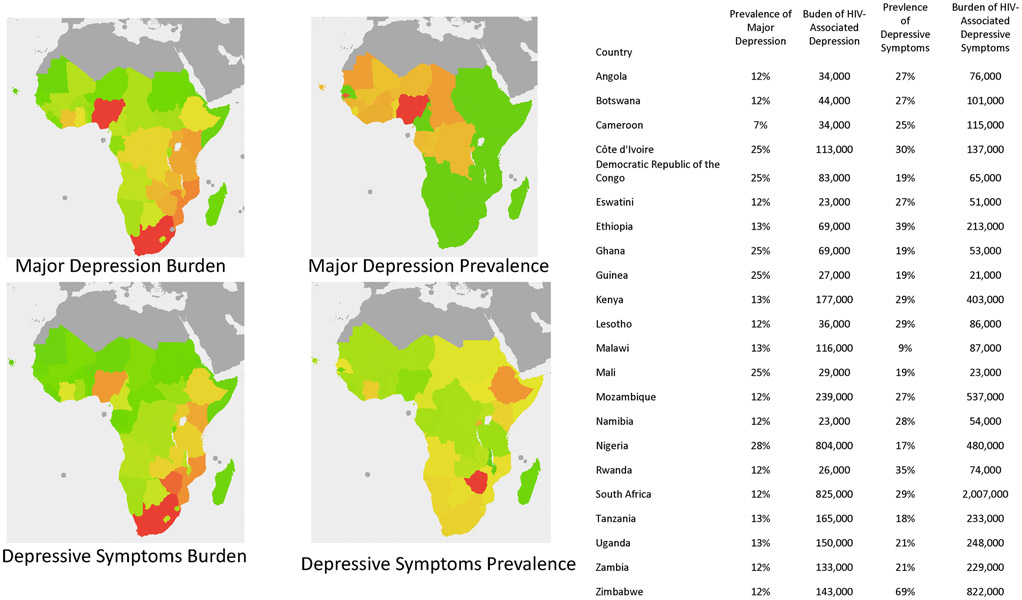
The Burden of HIV-associated Depression in Absolute Numbers
The burden of depression and depressive symptoms in absolute numbers was estimated using our prevalence data and found to be 3,626,000 (99.7% CI, 3,152,000-4,189,000) people living with HIV in Sub-Saharan Africa for major depression (Table 1) and 6,376,000 (99.7%CI, 5,565,000-7,386,000) individuals HIV-infected with depressive symptoms (Table 2). The calculated estimates are based on the prevalence by country. Where country-specific data was lacking, we estimated the burden using regional averages. From these estimates, we mapped the burden of major depression and depressive symptoms (Figure 3).
Table 1.
Estimated Burden of Major Depression in those with HIV in Sub-Saharan Africa Using Data from Systematic Review and UNAIDS 2008-2018.
| Country | Estimated Prevalence |
Mean Estimate of Major Depression |
Confidence Interval of Estimate |
Disability Adjusted Life- Years (DALY)s |
|---|---|---|---|---|
| Eastern and Southern Africa | ||||
| Angola | 12.1% | 34,000 | (21,000-49,000) | 15,000 |
| Botswana | 12.2% | 44,000 | (28,000-65,000) | 19,000 |
| Ethiopia | 12.5% | 69,000 | (45,000-98,000) | 30,000 |
| Kenya* | 12.6% | 177,000 | (130,000-232,000) | 77,000 |
| Lesotho | 12.0% | 36,000 | (22,000-52,000) | 16,000 |
| Malawi | 12.6% | 116,000 | (72,000-169,000) | 50,000 |
| Mozambique | 12.1% | 239,000 | (142,000-361,000) | 104,000 |
| Rwanda | 12.4% | 26,000 | (18,000-36,000) | 11,000 |
| South Africa* | 12.0% | 825,000 | (699,000-961,000) | 360,000 |
| Tanzania* | 12.7% | 165,000 | (112,000-229,000) | 72,000 |
| Uganda* | 12.5% | 150,000 | (130,000-172,000) | 65,000 |
| Zambia* | 12.1% | 133,000 | (80,000-196,000) | 58,000 |
| Zimbabwe | 12.1% | 143,000 | (89,000-210,000) | 62,000 |
| Regional Sub-Total | 12.4% | 2,243,000 | (2,045,000-2,521,000) | 972,000 |
| Western and Central Africa | ||||
| Cameroon* | 7.3% | 34,000 | (22,000-49,000) | 15,000 |
| Côte d'Ivoire | 24.5% | 113,000 | (71,000-160,000) | 49,000 |
| Dem. Republic Congo | 24.5% | 83,000 | (60,000-110,000) | 36,000 |
| Ghana | 24.5% | 69,000 | (52,000-88,000) | 30,000 |
| Guinea | 24.5% | 27,000 | (20,000-35,000) | 12,000 |
| Mali | 24.5% | 29,000 | (21,000-39,000) | 13,000 |
| Nigeria* | 27.8% | 804,000 | (527,000-1,095,000) | 348,000 |
| Regional Sub-Total | 24.7% | 1,383,000 | (1,019,000-1,754,000) | 599,000 |
| Sub-Saharan Africa Total | 15.3% | 3,626,000 | (3,152,000-4,189,000) | 1,572,000 |
Country burden calculated from prevalence data identified from systematic review. Other countries’ burdens were calculated using regional mean for major depression and 99.7% confidence interval (i.e. 3 standard deviations). ** Only the 20 countries with the highest prevalence of depression are listed. A full listing of all countries is provided in Supplemental Table 6.
Table 2.
Burden of Depressive Symptoms in those with HIV in Sub-Saharan Africa Using Data from Systematic Review 2008-2018.
| Country | Estimated Prevalence |
Mean Estimate of Depressive Symptoms |
Confidence Interval of Estimate |
|---|---|---|---|
| Eastern and Southern Africa | |||
| Eswatini | 26.8% | 51,000 | (46,000-57,000) |
| Tanzania* | 17.9% | 232,000 | (203,000-264,000) |
| Uganda* | 20.7% | 248,000 | (223,000-274,000) |
| Ethiopia* | 38.7% | 213,000 | (165,000-262,000) |
| Kenya* | 28.8% | 403,000 | (340,000-469,000) |
| Rwanda* | 35.2% | 74,000 | (65,000-84,000) |
| Zambia* | 20.8% | 229,000 | (191,000-271,000) |
| Botswana* | 27.3% | 101,000 | (88,000-116,000) |
| Lesotho* | 28.7% | 86,000 | (77,000-96,000) |
| Malawi* | 9.0% | 87,000 | (70,000-105,000) |
| Angola | 27.1% | 76,000 | (47,000-106,000) |
| Namibia* | 28.4% | 54,000 | (47,000-62,000) |
| Mozambique | 26.9% | 538,000 | (421,000-660,000) |
| South Africa* | 29.1% | 2,007,000 | (1,814,000-2,205,000) |
| Zimbabwe* | 68.5% | 822,000 | (713,000-932,000) |
| Regional Sub-Total | 29.4% | 5,304,000 | (4,851,000-5,955,000) |
| Western and Central Africa | |||
| Cameroon* | 24.5% | 115,000 | (93,000-138,000) |
| Ghana | 18.9% | 53,000 | (41,000-68,000) |
| Dem. Republic Congo | 19.1% | 65,000 | (47,000-85,000) |
| Nigeria* | 16.6% | 480,000 | (312,000-654,000) |
| Ivory Coast* | 29.8% | 137,000 | (89,000-190,000) |
| Regional Sub-Total | 19.1% | 1,072,000 | (785,000-1,358,000) |
| Sub-Saharan Africa Total: | 27.0% | 6,376,000 | (5,565,000-7,386,000) |
Country burden calculated from prevalence data identified from systematic review. Other countries’ burdens were calculated using regional mean for major depression and 99.7% confidence interval (i.e. 3 standard deviations).
Only the 20 countries with the highest prevalence of depression are listed. A full listing of all countries is provided in Supplemental Table 6.
Fig. 3.
Prevalence of Depression in Africans Living with HIV by Country in Absolute Numbers. Note: Major depression as defined by a standardized, diagnostic interview; Depressive symptoms as defined by a depression-specific screening tool
Descriptive Assessment of the Effects of HIV-associated Depression
We characterized other measures of the effects of depression, including DALYs, ART adherence, or viral suppression, and found the data to be scarce. None of the 70 articles presented DALYs or QALYs. Eight articles addressed baseline ART adherence with two finding no association between depression and adherence,33,72 while six found depression was negatively associated with adherence.20,22,39,50,73,74 Only, two of the 70 articles evaluated the relationship between depression and HIV viral load with neither finding a statistically significant relationship between more depressive symptoms and more virologic failure on ART.47,50
Disability-adjusted Life Years (DALYs) lost due to Major Depression
Finally, to better understand the burden of disability from depression in Africans with HIV, we calculated DALYs. We found five papers from Nigeria,56,75,76 Cameroon,77 and Uganda, 48 which used PHQ-9 to estimate the severity of depression. We estimated 18.5% of individuals had mild depression (95%CI, 16.6-20.6%), 8.4% had moderate depression (95%CI, 7.1%-9.9%), and 1.4% had severe depression (95%CI, 0.8- 2.1%). Since our data used the cutoff of major depression, we only calculated DALYs for moderate to severe depression. We estimated that the DALYs lost from major depression were 1.57 million (95% CI, 1.37-1.82 million) across Sub-Saharan Africa among people living with HIV (Supplemental Table 6).
Discussion
We estimated the prevalence of major depression in people living with HIV in Sub-Saharan Africa to be 17%, the prevalence of depressive symptoms to be 26%, and the prevalence of psychological distress to be 33%. This prevalence of depression is substantial, given the limited mental health resources and the large number of those with HIV in Africa. These prevalence rates are up to 2-fold higher than in non-HIV populations in Africa.29,43,44,54,69-71 Above and beyond improving the quality of life of people with HIV, treatment of depression is vital given depression in HIV is known to cause worse HIV outcomes.4,5
There are significant differences in the prevalence of depression in HIV-infected individuals between different African countries. The prevalence of major depression ranged from 7% in Cameroon78 to 28% in Nigeria.15,29,37,65,79 Reasons for this difference could be social and political, or highlight differences in specific diagnostic methods. It is also possible that those sampled as controls in these studies had been impacted by HIV more than the general sub-Saharan African population and thus had higher rates of depression.
We found that the absolute prevalence of depressive symptoms was similar between those participants on ART and those not on ART. This consistency is likely because of changing guidelines for the CD4 cut-offs to start ART. Given that the studies were mostly cross-sectional, the longitudinal changes over time were not assessed. However, two studies did longitudinal assessments. Specifically, Kinyanda showed that depression decreased as individuals initiated ART, and Chan showed that population-level rates of depression over time declined as people initiated ART earlier.34,35
Depression appeared to affect women more than men, with women having one-third higher prevalence of both major depression and depressive symptoms compared to men. This difference in prevalence has been shown in other settings.80 There is some thought that hormones may be involved in this difference.81 Our data show a smaller disparity between men and women than in different contexts, although most of the other data originated in western countries.82 Further work is needed to know if this difference is related to HIV or social factors.
We looked at several metrics of the burden of depression, including markers related to disability, adherence, and viral suppression. Our search found a paucity of data. DALYs were not reported in the articles we found, so we calculated them and found 1.57 million DALYs lost among people living with HIV in sub-Saharan Africa. Our calculation is likely a conservative estimate as the DALY estimate does not include those with sub-clinical or mild depression. We could not find a clear link between depression and viral suppression; however, virologic testing has only been available in Africa for a limited time.83 The relationship between viral suppression and depression is an area of needed further study. A study from the USA has found this link between depression and more virologic failure.84
We compiled as many articles as possible, but some countries have no data or a paucity of data. Many different depression tools were used. While these tools have been validated, the cutoff for depression is not identical between different diagnostic methods.85-88 We evaluated the validity of combining the prevalence using various tools by generating a scatter plot; the prevalence was not significantly altered by the tool used. The lack of significance suggests that combining prevalences using different methods was reasonable. We also completed a funnel plot for both major depression and depressive symptoms, which did not show significant publication bias despite using various tools. We estimated the burden of depression in those with HIV using regional averages. However, more accurate data would require more research to survey the prevalence of depression in many more countries.
Overall, this work reveals a substantial burden of depression in those with HIV in Africa. As governments, non-profits, and international commissions work to reach the 90-90-90 goals,89 interventions for depression and mental illness broadly are needed. Those with depression are known to have a higher risk of acquiring HIV,90 and a lower rate of linkage to HIV care that those without depression.69 Those with HIV-associated depression are also less likely to achieve good ART adherence,2 more likely to develop virologic failure,5 and are more likely to have HIV progression, independent of ART adherence, than those without depression.4
While this review highlights the need for more screening to diagnose depression, screening alone is insufficient to improve depression care in resource-limited settings without more work on how best to treat depression in this setting. Our prior systematic review on depression interventions in sub-Saharan Africa showed many pilot and feasibility studies had been done. However, limited efficacy studies.91 High-quality clinical trials are needed to evaluate the effectiveness of antidepressant medications in these settings, given the paucity of data.92 While psychotherapy has been shown to improve symptomatology in those with depression and HIV,93 further work adapting psychotherapy to local settings is needed. Finally, implementation studies will be required to fully integrate depression care in HIV primary care if we hope to end the epidemic of HIV in sub-Saharan Africa.94-97
Limitations
A variety of validated depression tools have been used to quantify the prevalence of depression and depressive symptoms, and some inter-scale variation is likely. More agreement in depression scales would have made comparing data simpler. The prevalence by study and country varied significantly. The studies with a cross-sectional design using populations of convenience may not be fully representative of a country’s general population. Also, many favored urban areas, given the ease in sampling. ART status was measured as a binary state (on or off ART by study), but virologic outcomes were generally unknown. Among studies included, all but one used depression tools validated in Africa.
Conclusion
Depression in those with HIV in Africa is more prevalent than those uninfected with HIV, and this work better characterizes the prevalence by country and region. We found a prevalence of major depression of 15% in HIV-infected Africans. The overall burden of major depression in those with HIV in Sub-Saharan Africa was 3.6 million. More attention to interventions for mental illness will be needed to achieve control of HIV in Sub-Saharan Africa.
Supplementary Material
Acknowledgements
This research was supported by the National Institute of Neurologic Diseases and Stroke (NINDS), Fogarty International Center (R01NS086312, R25TW009345), the National Institute of Allergy and Infectious Diseases (T32AI055433), and the National Institute of Mental Health (K23 MH121220). We thank Jose Debes for his kind help in translating our abstract into Spanish.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Patel V, Chisholm D, Parikh R, et al. Addressing the burden of mental, neurological, and substance use disorders: key messages from Disease Control Priorities, 3rd edition. Lancet. April 16 2016;387(10028):1672–1685. [DOI] [PubMed] [Google Scholar]
- 2.Uthman OA, Magidson JF, Safren SA, Nachega JB. Depression and adherence to antiretroviral therapy in low-, middle- and high-income countries: a systematic review and meta-analysis. Curr HIV/AIDS Rep. September 2014;11(3):291–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ferrari AJ, Somerville AJ, Baxter AJ, et al. Global variation in the prevalence and incidence of major depressive disorder: a systematic review of the epidemiological literature. Psychol Med. March 2013;43(3):471–481. [DOI] [PubMed] [Google Scholar]
- 4.Bouhnik AD, Preau M, Vincent E, et al. Depression and clinical progression in HIV-infected drug users treated with highly active antiretroviral therapy. Antivir Ther. 2005;10(1):53–61. [PubMed] [Google Scholar]
- 5.Marconi VC, Wu B, Hampton J, et al. Early warning indicators for first-line virologic failure independent of adherence measures in a South African urban clinic. AIDS Patient Care STDS. December 2013;27(12):657–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abas M, Ali GC, Nakimuli-Mpungu E, Chibanda D. Depression in people living with HIV in sub-Saharan Africa: time to act. Trop Med Int Health. December 2014;19(12):1392–1396. [DOI] [PubMed] [Google Scholar]
- 7.Choi JY. Mental health of HIV-infected patients: A severe, but Overlooked Problem. Infect Chemother. June 2013;45(2):239–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asch SM, Kilbourne AM, Gifford AL, et al. Underdiagnosis of depression in HIV: who are we missing? J Gen Intern Med. June 2003;18(6):450–460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Olisah VO, Baiyewu O, Sheikh TL. Depression underdiagnosis and the effects on quality of life in outpatients with HIV at a Nigerian university teaching hospital. Afr J AIDS Res. September 2011;10(3):247–254. [DOI] [PubMed] [Google Scholar]
- 10.Marando F, Gualberti G, Costanzo AM, et al. Discrepancies between physician's perception of depression in HIV patients and self-reported CES-D-20 assessment: the DHIVA study. AIDS Care. 2016;28(2):147–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rodkjaer L, Laursen T, Balle N, Sodemann M. Depression in patients with HIV is under-diagnosed: a cross-sectional study in Denmark. HIV Med. January 2010;11(1):46–53. [DOI] [PubMed] [Google Scholar]
- 12.UNAIDS. AIDSinfo: Data Sheet HIV Prevalence 2017; http://aidsinfo.unaids.org/.
- 13.Nakimuli-Mpungu E. Depression and HIV: the search for solutions in sub-Saharan Africa. The Conversation. 2016. https://theconversation.com/depression-and-hiv-the-search-for-solutions-in-sub-saharan-africa-56514. Accessed 26 June 2019.
- 14.Seth P, Kidder D, Pals S, et al. Psychosocial functioning and depressive symptoms among HIV-positive persons receiving care and treatment in Kenya, Namibia, and Tanzania. Prev Sci. June 2014;15(3):318–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adewuya AO, Afolabi MO, Ola BA, et al. Relationship between depression and quality of life in persons with HIV infection in Nigeria. Int J Psychiatry Med. 2008;38(1):43–51. [DOI] [PubMed] [Google Scholar]
- 16.Gaynes BN, Pence BW, Atashili J, O'Donnell J, Kats D, Ndumbe PM. Prevalence and predictors of major depression in HIV-infected patients on antiretroviral therapy in Bamenda, a semi-urban center in Cameroon. PLoS One. 2012;7(7):e41699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kinyanda E, Hoskins S, Nakku J, Nawaz S, Patel V. Prevalence and risk factors of major depressive disorder in HIV/AIDS as seen in semi-urban Entebbe district, Uganda. BMC Psychiatry. December 30 2011;11:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.L'Akoa R M, Noubiap JJ, Fang Y, Ntone FE, Kuaban C. Prevalence and correlates of depressive symptoms in HIV-positive patients: a cross-sectional study among newly diagnosed patients in Yaounde, Cameroon. BMC Psychiatry. September 22 2013;13:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marwick KF, Kaaya SF. Prevalence of depression and anxiety disorders in HIV-positive outpatients in rural Tanzania. AIDS Care. April 2010;22(4):415–419. [DOI] [PubMed] [Google Scholar]
- 20.Nakimuli-Mpungu E, Musisi S, Katabira E, Nachega J, Bass J. Prevalence and factors associated with depressive disorders in an HIV+ rural patient population in southern Uganda. J Affect Disord. December 2011;135(1-3):160–167. [DOI] [PubMed] [Google Scholar]
- 21.Nyirenda M, Chatterji S, Rochat T, Mutevedzi P, Newell ML. Prevalence and correlates of depression among HIV-infected and -affected older people in rural South Africa. J Affect Disord. October 2013;151(1):31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tesfaw G, Ayano G, Awoke T, et al. Prevalence and correlates of depression and anxiety among patients with HIV on-follow up at Alert Hospital, Addis Ababa, Ethiopia. BMC Psychiatry. November 02 2016;16(1):368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bernard C, Dabis F, de Rekeneire N. Prevalence and factors associated with depression in people living with HIV in sub-Saharan Africa: A systematic review and meta-analysis. PLoS One. 2017;12(8):e0181960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Uicker WC, Doyle HA, McCracken JP, Langlois M, Buchanan KL. Cytokine and chemokine expression in the central nervous system associated with protective cell-mediated immunity against Cryptococcus neoformans. Med Mycol. February 2005;43(1):27–38. [DOI] [PubMed] [Google Scholar]
- 25.Sowa nA, Cholera R, Pence BW, Gaynes BN. Perinatal depression in HIV-infected African women: a systematic review. J Clin Psychiatry. October 2015;76(10):1385–1396. [DOI] [PubMed] [Google Scholar]
- 26.Gunn A Gunn Map 2. 2017.
- 27.UNAIDS data 2018. 2018 Accessed December 1, 2018. [Google Scholar]
- 28.Salomon JA HJ, Davis A, Maertens de Noordhout C, Polinder S, Havelaar AH, Cassini A,, Devleesschauwer B KM, Speybroeck N, Murray CJL, Vos T. Disability weights for the Global Burden of Disease 2013 study. Lancet Global Health. 2015;3(11):PE712–E723. [DOI] [PubMed] [Google Scholar]
- 29.Chikezie UE, Otakpor AN, Kuteyi OB, James BO. Depression among people living with human immunodeficiency virus infection/acquired immunodeficiency syndrome in Benin City, Nigeria: a comparative study. Niger J Clin Pract. Apr-Jun 2013;16(2):238–242. [DOI] [PubMed] [Google Scholar]
- 30.Myer L, Seedat S, Stein DJ, Moomal H, Williams DR. The mental health impact of AIDS-related mortality in South Africa: a national study. J Epidemiol Community Health. April 2009;63(4):293–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kingori C, Haile ZT, Ngatia P. Depression symptoms, social support and overall health among HIV-positive individuals in Kenya. Int J STD AIDS. March 2015;26(3):165–172. [DOI] [PubMed] [Google Scholar]
- 32.Klis S, Velding K, Gidron Y, Peterson K. Posttraumatic stress and depressive symptoms among people living with HIV in the Gambia. AIDS Care. April 2011;23(4):426–434. [DOI] [PubMed] [Google Scholar]
- 33.Krumme AA, Kaigamba F, Binagwaho A, Murray MB, Rich ML, Franke MF. Depression, adherence and attrition from care in HIV-infected adults receiving antiretroviral therapy. J Epidemiol Community Health. March 2015;69(3):284–289. [DOI] [PubMed] [Google Scholar]
- 34.Chan BT, Weiser SD, Boum Y, et al. Declining prevalence of probable depression among patients presenting for antiretroviral therapy in rural Uganda: the role of early treatment initiation. AIDS Behav. January 2015;19(1):19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kinyanda E, Weiss HA, Levin J, et al. Incidence and Persistence of Major Depressive Disorder Among People Living with HIV in Uganda. AIDS Behav. June 2017;21(6):1641–1654. [DOI] [PubMed] [Google Scholar]
- 36.Peltzer K Social grants for people living with HIV and on antiretroviral therapy in KwaZulu-Natal, South Africa: a longitudinal study. SAHARA J. 2012;9(1):6–14. [DOI] [PubMed] [Google Scholar]
- 37.Ibrahim AW, Jidda MS, Wakil MA, et al. Prevalence, Correlates and Under-Diagnosis of Clinical Depression among Adults on Highly Active Antiretroviral Therapy in a Tertiary Health Institution in Northeastern Nigeria. J Public Health Afr. June 29 2014;5(2):342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Endeshaw M, Walson J, Rawlins S, et al. Stigma in Ethiopia: association with depressive symptoms in people with HIV. AIDS Care. 2014;26(8):935–939. [DOI] [PubMed] [Google Scholar]
- 39.Nel A, Kagee A. The relationship between depression, anxiety and medication adherence among patients receiving antiretroviral treatment in South Africa. AIDS Care. August 2013;25(8):948–955. [DOI] [PubMed] [Google Scholar]
- 40.Lawler K, Mosepele M, Seloilwe E, et al. Depression among HIV-positive individuals in Botswana: a behavioral surveillance. AIDS Behav. January 2011;15(1):204–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.van den Heuvel L, Chishinga N, Kinyanda E, et al. Frequency and correlates of anxiety and mood disorders among TB- and HIV-infected Zambians. AIDS Care. 2013;25(12):1527–1535. [DOI] [PubMed] [Google Scholar]
- 42.Martinez P, Andia I, Emenyonu N, et al. Alcohol use, depressive symptoms and the receipt of antiretroviral therapy in southwest Uganda. AIDS Behav. July 2008;12(4):605–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chibanda D, Cowan F, Gibson L, Weiss HA, Lund C. Prevalence and correlates of probable common mental disorders in a population with high prevalence of HIV in Zimbabwe. BMC Psychiatry. February 29 2016; 16:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kinyanda E, Kuteesa M, Scholten F, Mugisha J, Baisley K, Seeley J. Risk of major depressive disorder among older persons living in HIV-endemic central and southwestern Uganda. AIDS Care. December 2016;28(12):1516–1521. [DOI] [PubMed] [Google Scholar]
- 45.Asangbeh SL SJ, Ekali GL, Eyoum C, Msellati P. Predictors of depression among patients on art in a rural health district in North West Cameroon. AIDS Care. 2015;28(2):205–208. [DOI] [PubMed] [Google Scholar]
- 46.Farley J, Miller E, Zamani A, et al. Screening for hazardous alcohol use and depressive symptomatology among HIV-infected patients in Nigeria: prevalence, predictors, and association with adherence. J Int Assoc Physicians AIDS Care (Chic). Jul-Aug 2010;9(4):218–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Peterson K, Togun T, Klis S, Menten J, Colebunders R. Depression and posttraumatic stress disorder among HIV-infected Gambians on antiretroviral therapy. AIDS Patient Care STDS. October 2012;26(10):589–596. [DOI] [PubMed] [Google Scholar]
- 48.Okeke EN, Wagner GJ. AIDS treatment and mental health: evidence from Uganda. Soc Sci Med. September 2013;92:27–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Marcellin F, Moh R, Carrieri MP, et al. Depressive symptoms and exposure to efavirenz in West African HIV-infected adults. HIV Clin Trials. Nov-Dec 2008;9(6):445–447. [DOI] [PubMed] [Google Scholar]
- 50.Belenky NM, Cole SR, Pence BW, Itemba D, Maro V, Whetten K. Depressive symptoms, HIV medication adherence, and HIV clinical outcomes in Tanzania: a prospective, observational study. PLoS One. 2014;9(5):e95469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wagner GJ, Ghosh-Dastidar B, Slaughter M, et al. The role of depression in work-related outcomes of HIV treatment in Uganda. Int J Behav Med. December 2014;21(6):946–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cerutti B, Broers B, Masetsibi M, et al. Alcohol use and depression: link with adherence and viral suppression in adult patients on antiretroviral therapy in rural Lesotho, Southern Africa: a cross-sectional study. BMC Public Health. September 08 2016;16:947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kagee A, Martin L. Symptoms of depression and anxiety among a sample of South African patients living with HIV. AIDS Care. February 2010;22(2):159–165. [DOI] [PubMed] [Google Scholar]
- 54.Kanmogne GD, Qiu F, Ntone FE, et al. Depressive symptoms in HIV-infected and seronegative control subjects in Cameroon: Effect of age, education and gender. PloS one. 2017-1-1 2017;12(2):e0171956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Letta S, Demissie A, Oljira L, Dessie Y. Factors associated with adherence to Antiretroviral Therapy (ART) among adult people living with HIV and attending their clinical care, Eastern Ethiopia. BMC Int Health Hum Rights. December 28 2015;15:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Onyebuchi-Iwudibia O, Brown A. HIV and depression in Eastern Nigeria: the role of HIV-related stigma. AIDS Care. 2014;26(5):653–657. [DOI] [PubMed] [Google Scholar]
- 57.Mutabazi-Mwesigire D, Katamba A, Martin F, Seeley J, Wu AW. Factors That Affect Quality of Life among People Living with HIV Attending an Urban Clinic in Uganda: A Cohort Study. PLoS One. 2015;10(6):e0126810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wroe EB, Hedt-Gauthier BL, Franke MF, Nsanzimana S, Turinimana JB, Drobac P. Depression and patterns of self-reported adherence to antiretroviral therapy in Rwanda. Int J STD AIDS. March 2015;26(4):257–261. [DOI] [PubMed] [Google Scholar]
- 59.Akena D, Musisi S, Joska J, Stein DJ. The association between aids related stigma and major depressive disorder among HIV-positive individuals in Uganda. PLoS One. 2012;7(11):e48671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gupta R, Dandu M, Packel L, et al. Depression and HIV in Botswana: a population-based study on gender-specific socioeconomic and behavioral correlates. PLoS One. December 08 2010;5(12):e14252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kitshoff C, Campbell L, Naidoo SS. The association between depression and adherence to antiretroviral therapy in HIV-positive patients, KwaZulu-Natal, South Africa. South African Family Practice. 2012-1-1 2012;54(2):145–150. [Google Scholar]
- 62.Shacham E, Estlund AL, Tanner AE, Presti R. Challenges to HIV management among youth engaged in HIV care. AIDS Care. February 2017;29(2):189–196. [DOI] [PubMed] [Google Scholar]
- 63.Redman KN, Karstaedt AS, Scheuermaier K. Increased CD4 counts, pain and depression are correlates of lower sleep quality in treated HIV positive patients with low baseline CD4 counts. Brain, Behavior, and Immunity. 2018-1-1 2018;69:548–555. [DOI] [PubMed] [Google Scholar]
- 64.Freeman MN N; Kafaar Z; Kelly K Mental disorder in people living with HIV/AIDS in South Africa. South African Journal of Psychology. 2008;38(3):489–500. [Google Scholar]
- 65.Egbe CO DP, Ekong E, Kohrt BA, Minto JG, Ticao CJ. Depression, suicidality, and alcohol use disorder among people living with HIV/AIDS in Nigeria. BMC Public Health. 2017;17(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ofovwe CE, Ofovwe C. Psychological disorders among human immunodeficiency virus-infected adults in southern Nigeria. Afr J Reprod Health. December 2013;17(4 Spec No):177–182. [PubMed] [Google Scholar]
- 67.Olley BO, Adebayo KO, Ogunde MJ, Ishola A, Ogar AP. Psychosocial factors predicting severity of depression among treatment-seeking HIV/AIDS patients: A multi-site Nigerian study. Niger J Clin Pract. March 2017;20(3):296–302. [DOI] [PubMed] [Google Scholar]
- 68.Kelly CM, van Oosterhout JJ, Ngwalo C, et al. HIV associated neurocognitive disorders (HAND) in Malawian adults and effect on adherence to combination anti-retroviral therapy: a cross sectional study. PLoS One. 2014;9(6):e98962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cholera R, Pence BW, Gaynes BN, et al. Depression and Engagement in Care Among Newly Diagnosed HIV-Infected Adults in Johannesburg, South Africa. AIDS Behav. June 2017;21(6):1632–1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chipimo PJ, Fylkesnes K. Mental distress in the general population in Zambia: impact of HIV and social factors. BMC Public Health. August 18 2009;9:298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kelly SG, Taiwo BO, Wu Y, et al. Early suppressive antiretroviral therapy in HIV infection is associated with measurable changes in the corpus callosum. J Neurovirol. October 2014;20(5):514–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kitshoff AM, de Rooster H, Ferreira SM, Steenkamp G. A retrospective study of 109 dogs with mandibular fractures. Vet Comp Orthop Traumatol. 2013;26(1):1–5. [DOI] [PubMed] [Google Scholar]
- 73.Adewuya AO, Afolabi MO, Ola BA, et al. The effect of psychological distress on medication adherence in persons with HIV infection in Nigeria. Psychosomatics. Jan-Feb 2010;51(1):68–73. [DOI] [PubMed] [Google Scholar]
- 74.Tlhajoane M, Eaton JW, Takaruza A, et al. Prevalence and Associations of Psychological Distress, HIV Infection and HIV Care Service Utilization in East Zimbabwe. AIDS Behav. May 2018;22(5):1485–1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Amoko A AB, Ajiboye PO, Olagunju OK, Sule AG. Family correlates of depression among hiv positive patients attending family medicine clinic at University of Ilorin Teaching Hospital, Ilorin, Nigeria." Nigerian Journal of Family Practice 7(4). Nigerian Journal of Family Practice. 2016;7(4). [Google Scholar]
- 76.Adiari O CP. Prevalence and Severity of Depression among People Living with HIV/AIDS in a Tertiary Hospital. Nigerian Hospital Practice. 2014;14(1-2):3–15. [Google Scholar]
- 77.Ngum PA, Fon PN, Ngu RC, Verla VS, Luma HN. Depression Among HIV/AIDS Patients on Highly Active Antiretroviral Therapy in the Southwest Regional Hospitals of Cameroon: A Cross-Sectional Study. Neurol Ther. June 2017;6(1):103–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gaynes Bn, Pence BW, Atashili J, O'Donnell J, Kats D, Ndumbe PM. Prevalence and predictors of major depression in HIV-infected patients on antiretroviral therapy in Bamenda, a semi-urban center in Cameroon. Vol 72012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Seb-Akahomen O, Lawani A, James B. Mood and anxiety disorders adversely influence medication adherence to antiretroviral therapy among people living with HIV/AIDS in Nigeria. Hiv Aids Rev. 2018;17(2):91–97. [Google Scholar]
- 80.Albert PR. Why is depression more prevalent in women? J Psychiatry Neurosci. July 2015;40(4):219–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Schule C, Nothdurfter C, Rupprecht R. The role of allopregnanolone in depression and anxiety. Prog Neurobiol. February 2014;113:79–87. [DOI] [PubMed] [Google Scholar]
- 82.Kessler RC, Bromet EJ The epidemiology of depression across cultures. Annu Rev Public Health. 2013;34:119–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.El-Sadr WM, Rabkin M, Nkengasong J, Birx DL. Realizing the potential of routine viral load testing in sub-Saharan Africa. J Int AIDS Soc. November 2017;20 Suppl 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pence BW, Mills JC, Bengtson AM, et al. Association of Increased Chronicity of Depression With HIV Appointment Attendance, Treatment Failure, and Mortality Among HIV-Infected Adults in the United States. JAMA Psychiatry. February 21 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Amorim P, Lecrubier Y, Weiller E, Hergueta T, Sheehan D. DSM-IH-R Psychotic Disorders: procedural validity of the Mini International Neuropsychiatric Interview (MINI). Concordance and causes for discordance with the CIDI. Eur Psychiatry. 1998;13(1):26–34. [DOI] [PubMed] [Google Scholar]
- 86.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. September 2001;16(9):606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Segopolo MT, Selemogwe MM, Plattner IE, Ketlogetswe N, Feinstein A. A screening instrument for psychological distress in botswana: validation of the Setswana version of the 28-item general health questionnaire. Int J Soc Psychiatry. March 2009;55(2):149–156. [DOI] [PubMed] [Google Scholar]
- 88.Tsai AC. Reliability and validity of depression assessment among persons with HIV in sub-Saharan Africa: systematic review and meta-analysis. J Acquir Immune Defic Syndr. August 15 2014;66(5):503–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.UNAIDS. 90-90-90 An ambitious treatment target to help end the AIDS epidemic: Joint United Nations Programme on HIV/AIDS (UNAIDS). 2014.
- 90.Ahaneku H, Ross MW, Nyoni JE, et al. Depression and HIV risk among men who have sex with men in Tanzania. AIDS Care. 2016;28 Suppl 1:140–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lofgren SM, Nakasujja N, Boulware DR. Systematic Review of Interventions for Depression for People Living with HIV in Africa. AIDS Behav. September 12 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Eshun-Wilson I, Siegfried N, Akena DH, Stein DJ, Obuku EA, Joska JA. Antidepressants for depression in adults with HIV infection. . Cochrane Database Syst Rev. January 22 2018;1:CD008525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Honagodu AR, Krishna M, Sundarachar R, Lepping P. Group psychotherapies for depression in persons with HIV: A systematic review. Indian J Psychiatry. October 2013;55(4):323–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kaaya S, Eustache E, Lapidos-Salaiz I, Musisi S, Psaros C, Wissow L. Grand challenges: Improving HIV treatment outcomes by integrating interventions for co-morbid mental illness. PLoS Med. 2013;10(5):e1001447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Mahomed OH, Asmall S. Development and implementation of an integrated chronic disease model in South Africa: lessons in the management of change through improving the quality of clinical practice. Int J Integr Care. Oct-Dec 2015;15:e038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Udedi M, Stockton MA, Kulisewa K, et al. Integrating depression management into HIV primary care in central Malawi: the implementation of a pilot capacity building program. BMC health services research. July 31 2018;18(1):593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chibanda D Depression and HIV: integrated care towards 90-90-90. Int Health. March 01 2017;9(2):77–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Amberbir A, Woldemichael K, Getachew S, Girma B, Deribe K. Predictors of adherence to antiretroviral therapy among HIV-infected persons: a prospective study in Southwest Ethiopia. BMC Public Health. July 30 2008;8:265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Belete T, Medfu G, Yemiyamrew E. Prevalence of HIV Associated Neurocognitive Deficit among HIV Positive People in Ethiopia: A Cross Sectional Study at Ayder Referral Hospital. Ethiop J Health Sci. January 2017;27(1):67–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Mekuria LA, Sprangers MA, Prins JM, Yalew AW, Nieuwkerk PT. Health-related quality of life of HIV-infected adults receiving combination antiretroviral therapy in Addis Ababa. AIDS Care. 2015;27(8):934–945. [DOI] [PubMed] [Google Scholar]
- 101.Tesfaye SH, Bune GT. Generalized psychological distress among HIV-infected patients enrolled in antiretroviral treatment in Dilla University Hospital, Gedeo zone, Ethiopia. Glob Health Action. 2014;7:23882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yakob B, Purity Ncama B. Client satisfaction: correlates and implications for improving HIV/AIDS treatment and care services in southern Ethiopia. Int Health. July 2016;8(4):292–298. [DOI] [PubMed] [Google Scholar]
- 103.Kwobah E, Epstein S, Mwangi A, Litzelman D, Atwoli L. Prevalence of psychiatric morbidity in a community sample in Western Kenya. BMC Psychiatry. January 18 2017;17(1):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Adiari O PC. Prevalence and Severity of Depression among People Living with HIV/AIDS in a Tertiary Hospital. Nigerian Hospital Practice. 2014;14(1–2). [Google Scholar]
- 105.Ibrahim AW, Jidda MS, Wakil MA, et al. Prevalence, correlates and under-diagnosis of clinical depression among adults on highly active antiretroviral therapy in a Tertiary Health Institution in northeastern Nigeria. Journal of Public Health in Africa. 2014-7-1 2014;5(2):93–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Olagunju AT, Ogundipe OA, Erinfolami AR, Akinbode AA, Adeyemi JD. Toward the integration of comprehensive mental health services in HIV care: an assessment of psychiatric morbidity among HIV-positive individuals in sub-Saharan Africa. AIDS Care. 2013;25(9):1193–1198. [DOI] [PubMed] [Google Scholar]
- 107.Bhana A, Rathod SD, Selohilwe O, Kathree T, Petersen I. The validity of the Patient Health Questionnaire for screening depression in chronic care patients in primary health care in South Africa. BMC Psychiatry. 2015–1-1 2015; 15(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Cichowitz C, Maraba N, Hamilton R, Charalambous S, Hoffmann CJ. Depression and alcohol use disorder at antiretroviral therapy initiation led to disengagement from care in South Africa. PLoS One. 2017;12(12):e0189820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kagee A, Nel A, Saal W. Factor structure of the Beck Depression Inventory-II among South Africans receiving antiretroviral therapy. AIDS Care. 2014-1-1 2014;26(2):257–262. [DOI] [PubMed] [Google Scholar]
- 110.Pappin M, Wouters E, Booysen FL. Anxiety and depression amongst patients enrolled in a public sector antiretroviral treatment programme in South Africa: a cross-sectional study. BMC Public Health. March 27 2012;12:244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ramirez-Avila L, Regan S, Giddy J, et al. Depressive symptoms and their impact on health-seeking behaviors in newly-diagnosed HIV-infected patients in Durban, South Africa. AIDS Behav. November 2012;16(8):2226–2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. June 1961;4:561–571. [DOI] [PubMed] [Google Scholar]
- 113.Abubakar A, Kalu RB, Katana K, et al. Adaptation and Latent Structure of the Swahili Version of Beck Depression Inventory-II in a Low Literacy Population in the Context of HIV. PLoS One. 2016;11(6):e0151030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Amberbir A, Woldemichael K, Getachew S, Girma B, Deribe K. Predictors of adherence to antiretroviral therapy among HIV-infected persons: A prospective study in Southwest Ethiopia. BMC Public Health. 2008-1-1 2008;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behav Sci. January 1974;19(1):1–15. [DOI] [PubMed] [Google Scholar]
- 116.Lee B, Kaaya SF, Mbwambo JK, Smith-Fawzi MC, Leshabari MT. Detecting depressive disorder with the Hopkins Symptom Checklist-25 in Tanzania. Int J Soc Psychiatry. January 2008;54(1):7–20. [DOI] [PubMed] [Google Scholar]
- 117.Sweetland AC, Belkin GS, Verdeli H. Measuring depression and anxiety in sub-saharan Africa. Depress Anxiety. March 2014;31(3):223–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Semler G, Wittchen HU, Joschke K, et al. Test-retest reliability of a standardized psychiatric interview (DIS/CIDI). Eur Arch Psychiatry Neurol Sci. 1987;236(4):214–222. [DOI] [PubMed] [Google Scholar]
- 119.Gelaye B, Williams MA, Lemma S, et al. Diagnostic validity of the composite international diagnostic interview (CIDI) depression module in an East African population. Int J Psychiatry Med. 2013;46(4):387–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Pence BW, Gaynes BN, Atashili J, et al. Validity of an interviewer-administered patient health questionnaire-9 to screen for depression in HIV-infected patients in Cameroon. J Affect Disord. December 20 2012;143(1-3):208–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Gelaye B, Williams MA, Lemma S, et al. Validity of the Patient Health Questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. December 15 2013;210(2):653–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Nakku JEM, Rathod SD, Kizza D, et al. Validity and diagnostic accuracy of the Luganda version of the 9-item and 2-item Patient Health Questionnaire for detecting major depressive disorder in rural Uganda. Glob Ment Health (Camb). 2016;3:e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chibanda D, Verhey R, Gibson LJ, et al. Validation of screening tools for depression and anxiety disorders in a primary care population with high HIV prevalence in Zimbabwe. J Affect Disord. July 01 2016;198:50–55. [DOI] [PubMed] [Google Scholar]
- 124.Barczak P, Kane N, Andrews S, Congdon AM, Clay JC, Betts T. Patterns of psychiatric morbidity in a genito-urinary clinic. A validation of the Hospital Anxiety Depression scale (HAd). Br J Psychiatry. May 1988;152:698–700. [DOI] [PubMed] [Google Scholar]
- 125.Cairney J, Veldhuizen S, Wade TJ, Kurdyak P, Streiner DL. Evaluation of 2 measures of psychological distress as screeners for depression in the general population. Can J Psychiatry. February 2007;52(2):111–120. [DOI] [PubMed] [Google Scholar]
- 126.Andersen LS, Grimsrud A, Myer L, Williams DR, Stein DJ, Seedat S. The psychometric properties of the K10 and K6 scales in screening for mood and anxiety disorders in the South African Stress and Health study. Int J Methods PsychiatrRes. December 2011. ;20(4):215–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. September 1977;106(3):203–214. [DOI] [PubMed] [Google Scholar]
- 128.Olisah VO, Adekeye O, Sheikh TL. Depression and CD4 cell count among patients with HIV in a Nigerian University Teaching Hospital. Int J Psychiatry Med. 2015;48(4):253–261. [DOI] [PubMed] [Google Scholar]
- 129.Poupard M, Ngom Gueye NF, Thiam D, et al. Quality of life and depression among HIV-infected patients receiving efavirenz- or protease inhibitor-based therapy in Senegal. HIV Med. March 2007;8(2):92–95. [DOI] [PubMed] [Google Scholar]
- 130.Goldberg DP, Cooper B, Eastwood MR, Kedward HB, Shepherd M. A standardized psychiatric interview for use in community surveys. Br J Prev Soc Med. February 1970;24(1):18–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Henderson S, Duncan-Jones P, Byrne DG, Scott R, Adcock S. Psychiatric disorder in Canberra. A standardised study of prevalence. Acta Psychiatr Scand. October 1979;60(4):355–374. [DOI] [PubMed] [Google Scholar]
- 132.Wing JK, Babor T, Brugha T, et al. SCAN. Schedules for Clinical Assessment in Neuropsychiatry. Arch Gen Psychiatry. June 1990;47(6):589–593. [DOI] [PubMed] [Google Scholar]
- 133.Spitzer RL WJBW, Gibbon M, First MB,. Structured Clinical Interview for DSM-III-R, Patient Edition/Non-patient Edition. Washington, D.C.: American Psychiatric Press, Inc.; 1990. [Google Scholar]
- 134.Chikezie UE, Otakpor AN, Kuteyi OB, James BO. Depression among people living with human immunodeficiency virus infection/acquired immunodeficiency syndrome in Benin City, Nigeria: a comparative study. Nigerian journal of clinical practice. 2013-1-1 2013;16(2):238–242. [DOI] [PubMed] [Google Scholar]
- 135.Derogatis LR, Lipman RS, Covi L. SCL-90: an outpatient psychiatric rating scale-preliminary report. Psychopharmacol Bull. January 1973;9(1):13–28. [PubMed] [Google Scholar]
- 136.Berwick DM, Murphy JM, Goldman PA, Ware JE Jr., Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. February 1991. ;29(2):169–176. [DOI] [PubMed] [Google Scholar]
- 137.Rockliff BW. A brief self-rating questionnaire for depression (SRQ-D). Psychosomatics. Jul-Aug 1969;10(4):236–243. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.