Objective:
This analysis examined the relationship between Gulf War (GW) exposures and health symptoms reported in three time periods over 20 years in Ft. Devens Cohort veterans.
Methods:
Repeated logistic regression models examined the association of exposures and health symptoms over time. Models included baseline age, active duty status, post-traumatic stress disorder status, sex, and time since deployment as covariates.
Results:
Exposure to tent heaters was associated with increased odds of crying easily and muscle twitching. Exposure to pyridostigmine bromide (PB) pills was associated with increased odds of depression and fatigue. Exposure to the Khamisiyah sarin plume was associated with increased odds of trouble concentrating and crying easily.
Conclusion:
This longitudinal analysis demonstrated an association between neurotoxicant exposures and increased odds of cognitive/mood, fatigue, and neurological symptoms. In addition, most symptoms increased over time since deployment regardless of exposure.
Keywords: gulf war, gulf war illness, health symptoms, longitudinal analysis, neurotoxicants exposures, veterans
Learning Objectives
Summarize previous findings on the environmental hazards and symptoms reported by Gulf War veterans, including previous follow-up studies.
Discuss the new 20-year follow-up findings in the Ft. Devens Cohort of Gulf War veterans, including specific symptoms associated with specific exposures.
Discuss the study implications for ongoing care and monitoring of Gulf War veterans.
Military personnel deployed during the 1990 to 1991 Gulf War (GW) were exposed to unique environmental hazards in theatre, including pesticides, petrochemicals, debris from SCUD missiles, smoke from oil well fires, depleted uranium, prophylactic medications such as pyridostigmine bromide (PB) pills, and the chemical warfare agents sarin/cyclosarin.1–4 Previous findings from cross-sectional data suggest that GW veterans self-reporting exposure to smoke from oil well fires, pesticides, debris from SCUD missiles, hearing chemical weapon alerts, and using PB anti-nerve gas pills, were more likely to report cognitive dysfunction (eg, changes in memory), depressive symptoms, and neurological complaints (eg, headaches).1,2,5–9 In addition, pulmonary symptoms such as asthma, chronic bronchitis, cough, and shortness of breath, were more likely to be reported among GW veterans with exposure to combustion by-products from oil well fires, propane fuel emissions from tent heaters, and chemical weapons.7,10–12 Several studies have now found that these symptoms may stem from chronic neuroinflammatory or neuroimmune responses following neurotoxicant exposures.13–18
Follow-up studies among deployed GW veterans found that the number and severity of health symptoms remained stable or slightly worsened over follow-up periods of varying lengths (4–18 years), indicating neither improvement nor significant progression of symptoms.19–25 However, few longitudinal studies have examined the relationship over time between GW exposures and health symptoms in the same group. As GW veterans age, it is becoming increasingly important to evaluate these symptoms over time to study how neurotoxicants may influence patterns of aging.
The Ft. Devens cohort (FDC) is a population of former US Army Active, Reserve, and National Guard GW veterans followed prospectively through a series of surveys since their return from deployment in the Persian Gulf in 1991.7,9,26–30 These veterans were not recruited on the basis of symptom reporting but based on their military units. The findings from the FDC included early documentation of the most common health symptoms, cognitive decrements in environmentally exposed GW veterans, and differences in structural neuroimaging, including lower white matter volumes, as well as the effects of mild traumatic brain injury (mTBI) on GWI.7,9,26,30,31 To our knowledge, the present study is the first to utilize data from three surveys with the same veterans over a 20-year period to examine the relationship between self-reported GW deployment exposures and health symptoms over time.
METHODS
Participants and Surveys
In the Spring of 1991 (Baseline), Active Duty, Reserve, and National Guard Army personnel who returned from deployment to the Persian Gulf through Ft. Devens, Massachusetts, were recruited to participate in a survey to assess psychological health and combat exposure. Follow-up questionnaires were designed to assess long-term health, and psychological and functional well-being, as well as Gulf-specific environmental and combat exposures.7,28,29Figure 1 illustrates the overall timeline of the FDC study. The current study uses a subset of FDC participants who completed the Health Symptom Checklist at three follow-up time points (1992, 1997, 2013). All demographic variables were taken from the baseline survey (1991). All participants gave their informed consent for inclusion at each timepoint, before they participated in the surveys. Institutional review board approvals were obtained from VA Boston Healthcare System and Boston University before initiating the surveys.
FIGURE 1.
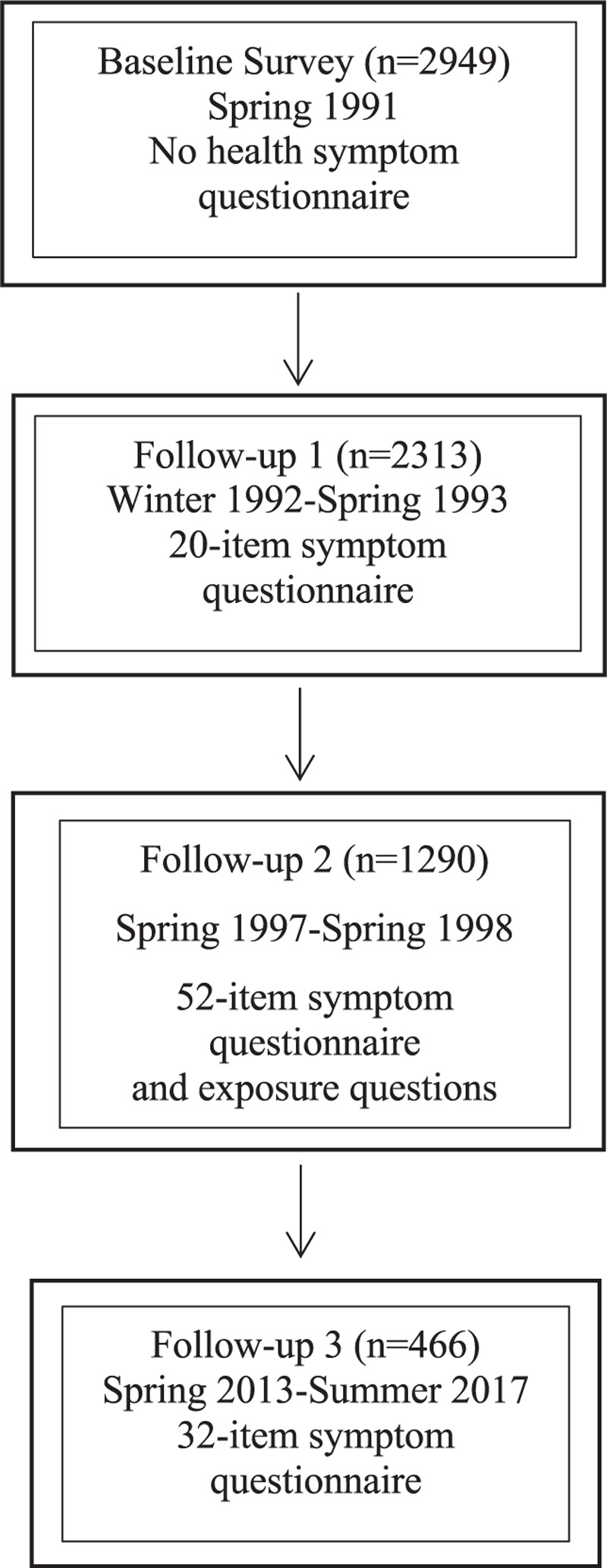
Overall timeline of the Ft. Devens Cohort (FDC) study.
The Health Symptom Checklist
The Health Symptom Checklist is a pre-set list of health symptoms originally adapted from Bartone et al.32 This measure asks participants to indicate whether they had experienced any of the specific health symptoms. At Follow-up 1, a 20-item Health Symptom Checklist asked veterans to indicate the frequency of 20 symptoms over the past 4 weeks using a Likert-scale rating (none, a little, often, very often).28 Follow-up 2 included a 52-item Expanded Health Checklist,7,29 which asked veterans to indicate whether they experienced each health symptom over the past 4 weeks (yes or no). If the veteran indicated yes, they were asked to indicate the frequency of the symptom as either sometimes, or a lot. Follow-up 3 included a 34-item Health Symptom Checklist, which asked veterans to endorse whether they experienced a symptom (yes or no) over the past 30 days. If veterans indicated yes, they were asked to indicate the frequency of the symptom [(rarely (once or twice in all), some (about once per week), often (several times per week), very often (almost every day)]. All responses were dichotomized as present or absent. If a veteran initially indicated not experiencing a symptom, but then endorsed a frequency, the response was recoded as being present.
On the basis of the epidemiological literature examining GW exposures and reported health symptoms,4 symptoms were chosen that could be characterized as belonging to one of the following categories: mood-cognition, fatigue, and neurological or physical symptoms. A total of 12 symptoms fit these categories and were included in all follow-up surveys: difficulty concentrating, feeling depressed, crying easily, feeling anxious, trouble sleeping, lack of energy, dizziness, headache, muscle twitching or trembling, rapid heart rate, skin rash, and shortness of breath.
Gulf War Exposure Characterization
At Follow-up 2 and Follow-up 3, FDC veterans were asked about environmental and combat exposures specific to GW deployment. Exposure to PB pills and chemical weapons were assessed at both Follow-up 2 and Follow-up 3. There was substantial agreement for PB pill exposure as assessed by the Kappa statistic [0.628 (95% confidence interval, 95% CI = 0.516 to 0.740)]. However, agreement was low for chemical weapon exposure [0.098 (95% CI = -0.005 to 0.201)]. This may be due to the differential wording for the assessment of chemical weapons at Follow-up 2 and Follow-up 3. Follow-up 2 assessed number of times a participant was on formal alert for a chemical attack, and Follow-up 3 assessed whether or not the participant was ever exposed to chemical/biological warfare. To minimize the length of time between deployment and recall, exposure data were taken from the Follow-up 2 survey, 6 years after deployment.
Veterans were asked to recall whether or not they had consumed PB pills and heard formal chemical weapons alerts in a dichotomous, yes or no response. They were also asked whether they had experienced exposure to smoke from tent heaters according to these categories: “not exposed,” “exposed but did not feel ill,” “exposed and felt ill.” Answers for these three GW-specific exposures were dichotomized into exposed and not exposed.
In addition, veterans were measured in regard to exposure to the Khamisiyah weapons demolition. In March of 1991, the Army Corp of engineers detonated underground munitions bunkers with thousands of Iraqi rockets, which they were unaware at the time had chemical weapons, sarin/cyclosarin, in the tips of the rockets. When the explosions occurred, it was estimated that over 100,000 GW veterans were exposed to low-level sarin/cyclosarin due to their proximity to the air plumes from the explosions.33,34 The Department of Defense (DOD) eventually notified exposed veterans by letter and a registry was established. A list of FDC veterans who received notification letters of potential exposure to sarin based on their proximity to the Khamisiyah weapons depot detonations and presumed to be exposed to low levels of sarin/cyclosarin based on wind plume modeling in 2000 was obtained by the DoD. These exposures were categorized as a dichotomous variable, yes (received a notification letter from the 2000 DOD exposure model) or no (never received a notification letter) for Khamisiyah exposure status as a proxy for sarin chemical weapons exposure during their deployment.34
Data Analysis
Descriptive statistics were used to describe the demographics and characteristics of the full FDC and the current study sample. The frequencies and percentages of health symptoms at each follow-up time point are reported. A generalized estimating equation using a logit link and an unstructured correlation was built for each health symptom, which included the GW-specific exposures to tent heaters, PB pills, self-reported exposure to chemical warfare agents and notification of proximity to sarin/cyclosarin air plumes, as well as the additional covariates of baseline age, active duty status, post-traumatic stress disorder (PTSD) status, and sex.
In addition, dates of survey completion were used to determine the amount of time in years since baseline survey completion to evaluate the effect of time on health symptom reporting. Interaction terms for years since deployment and each exposure were initially included in each model. Interaction terms that were not significant were removed from final models. Odds ratios (ORs) and 95% CIs were calculated from the logistic regression models. In interactions models, years since deployment were centered at 1.24 years, the mean time since deployment at Follow-up 1, so that ORs for exposure involved in interactions are describing associations at Follow-up 1. P values less than 0.05 were considered significant. Adjustments were not made for multiplicity. All analyses were performed using SAS 9.4 (SAS, Cary, North Carolina).
RESULTS
Demographics and Baseline Characteristics
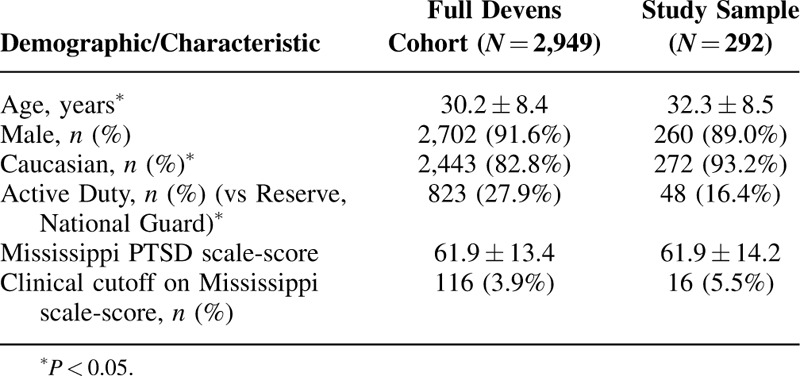
A total of 2949 FDC veterans completed the initial survey upon return from the GW in 1991. A total of 295 FDC veterans responded at all three time points, of whom 292 veterans had health symptom data at all three time points. In this subsample, the average age immediately after deployment was approximately 32.3 years, and veterans were more likely to be male and Caucasian. Only 16.4% were active duty and 5.5% met the clinical cut off for PTSD. The full FDC from the baseline survey did not differ from the subgroup with three time points compared in this study with regard to sex or PTSD status as measured by the Mississippi PTSD Scale. However, the study sample differed from the full FDC with regard to age, race, and active duty status (Table 1).
TABLE 1.
Demographics and Baseline (1991) Characteristics of Full Ft. Devens Cohort and Current Ft. Devens Cohort Sample
Reported Exposure and Health Symptoms
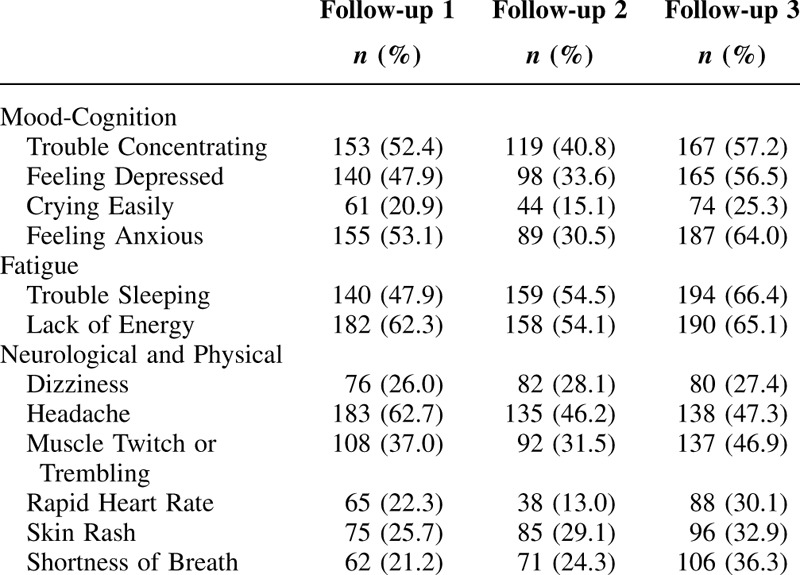
At Follow-up 2, approximately 85.6% of veterans reported exposure to chemical weapons, 68.5% reported exposure to PB pills, and 68.2% reported exposure to tent heaters. Approximately, 41.4% of veterans received notification of exposure to sarin gas from the Khamisiyah munitions demolition. On average, the number of years since deployment was 1.24 ± 0.28 years at Follow-up 1, 5.95 ± 0.18 years at Follow-up 2, and 23.91 ± 0.92 years at Follow-up 3. Frequencies and percentages of reported health symptoms at each Follow-up period are displayed in Table 2. Frequency of symptoms ranged from as low as 13.0% (rapid heart rate) to as high as 66.4% (trouble sleeping).
TABLE 2.
Frequencies and Percentages of Reported Health Symptoms at Each Follow-Up
Longitudinal Associations Between Gulf War Exposure and Health
The relation between GW-specific exposures and health symptoms are displayed in Table 3. Overall, years since deployment was significantly associated with an increase in reporting of 9 of the 12 symptoms and a decrease in one symptom (headache) over time (Table 3). The increase odds of reporting of these symptoms ranged from 2% to 6% per year since deployment. Self-reported exposure to chemical weapons was not significantly associated with health symptoms. However, self-reported exposure to tent heaters was associated with increased odds of crying easily (OR = 1.77, 95% CI = 1.03 to 3.04, P = 0.038) and muscle twitch or trembling (OR = 1.50, 95% CI = 1.00 to 2.23, P = 0.048) compared with veterans not reporting exposure to tent heaters. Significant interactions between tent heaters and years since deployment were noted for lack of energy (P = 0.036) and shortness of breath (P = 0.009), with differing patterns. Those reporting exposure to tent heaters initially reported lower frequency of shortness of breath (at Follow-up 1 OR = 0.59, 95% CI = 0.33 to 1.04, P = 0.068), but eventually reported a higher frequency (at Follow-up 3 OR = 1.33, 95% CI = 0.75 to 2.37, P = 0.331), than those unexposed. Those reporting exposure to tent heaters reported higher frequency of fatigue initially (at Follow-up 1 OR = 1.60, 85% CI = 0.92 to 2.76, p = 0.09), but eventually reported lower frequencies (at Follow-up 3 OR = 0.84, 95% CI = 0.50 to 1.43, P = 0.52), than those unexposed.
TABLE 3.
Longitudinal Associations Between GW-Specific Exposures and Reported Health Symptoms
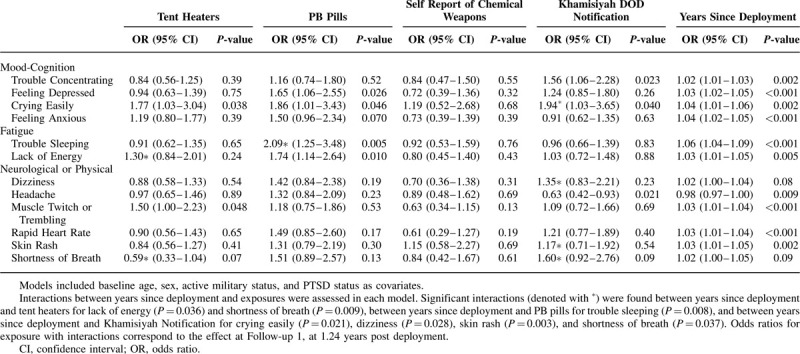
Self-reported exposure to PB pills was associated with increased odds of feeling depressed (OR = 1.65, 95% CI = 1.06 to 2.55, P = 0.026), crying easily (OR = 1.86, 95% CI = 1.01 to 3.43, P = 0.046), and lack of energy (OR = 1.74, 95% CI = 1.14 to 2.64, P = 0.010) compared with veterans not reporting PB pill usage. In addition, a significant interaction was noted between PB pill exposure and years since deployment for trouble sleeping (P = 0.008), where those reporting exposure initially reported higher frequency of trouble sleeping (at Follow-up 1 OR = 2.09, 95% CI = 1.25 to 3.48, P = 0.005), but eventually endorsed trouble sleeping at the same frequency as those unexposed (at Follow-up 3 OR = 0.83, 95% CI = 0.47 to 1.48, P = 0.053).
Exposure to the sarin plume from the Khamisiyah demolition operation was associated with increased odds of trouble concentrating (OR = 1.56, 95% CI = 1.06 to 2.28, P = 0.023) and decreased odds of headaches (OR = 0.63, 95% CI = 0.42to 0.93, P = 0.021) compared with FDC veterans who did not receive Khamisiyah notification letters. A significant interaction was noted between exposure to sarin and years since deployment for crying easily (P = 0.021), where those exposed initially reported higher frequency of crying easily (at Follow-up 1 OR = 1.94, 95% CI = 1.03 to 3.65, P = 0.040). Additional significant interactions between notification of exposure to the sarin plume from Khamisiyah and years since deployment were seen for dizziness (P = 0.028), skin rash (P = 0.003), and shortness of breath (P = 0.037). For each of these four symptoms, the exposed group reported initially reported higher frequency of symptoms than the unexposed group, but eventually reported either similar or lower rates than the unexposed group.
DISCUSSION
In a longitudinal analysis controlling for baseline age, active duty status, PTSD status, and sex, exposure to tent heaters was associated with higher endorsement of crying easily and muscle twitching/trembling. Our findings are similar to other studies that have shown tent heater exposure to be related to increased reporting of cardiac, neurological, and pulmonary symptoms,7 as well as chronic multisymptom illness (CMI), involving fatigue, cognitive/mood, and musculoskeletal symptoms.29
Self-reported exposure to PB pills was significantly associated with higher endorsement of feeling depressed, crying easily, trouble sleeping, and lack of energy. These results are consistent with previous reports of nearly 250,000 GW veterans, which suggested consumption of PB pills is a causal factor of GW Illness (GWI), a disorder that affects approximately 30% of GW veterans and is characterized by a combination of symptoms that include fatigue, cognitive and mood dysfunction, musculoskeletal pain, gastrointestinal complaints, respiratory symptoms, and skin rashes.1–4,35–37 Similarly, other studies demonstrated that veterans who consumed PB pills had significantly higher odds of CMI, which is a commonly used definition for GWI.29,35 In addition, self-reported PB exposure has recently been associated with medical conditions, including myocardial infarction, diabetes, and chronic fatigue syndrome.12
PB reversibly binds to the same cholinergic receptors as nerve agents such as sarin and soman causing the receptors to be unavailable for these nerve agents. Thus, a Food and Drug Administration waiver was obtained by the DoD for PB pills to be administered as a prophylactic medication during the GW. Safety was assumed, as PB pills were commonly used to treat a chronic autoimmune neuromuscular disorder, myasthenia gravis.38 However, PB is an acetylcholinesterase inhibitor (AChEi), which reversibly inactivates the AChE enzyme preventing the breakdown of acetylcholine (ACh).39,40 Subsequent accumulation of ACh in the synapse overstimulates muscarinic and nicotinic cholinergic receptors and has been shown to be associated with later cognitive, muscle, and sleep dysfunction.41,42 Further, oligodendrocytes have now been shown to have functional cholinergic receptors that are affected by GW-relevant AChE inhibitors, suggesting brain myelination may also be affected.43,44
Exposure to ACHEis, such as PB pills and sarin nerve gas, may also trigger brain-immune responses due to activation of microglia and astrocytes, the brain's immune sentinels. These sentinels enhance cytokine and chemokine signaling leading to chronic neuroinflammation.14,15,45–49 In addition, neuroendocrine and autonomic nervous system disruptions can occur, as well as alteration of innate immune function as cholinergic receptors also exist outside the central nervous system (CNS).4,42,50
In the current analysis, consumption of PB pills was associated with mood-cognition and fatigue symptoms, but significant associations were not observed among other neurological or physical symptoms. However, it is interesting to note that the ORs consistently indicated that PB pill consumption was associated with a 16% to 51% increase in symptoms even when the association was not statistically significant. The current sample size is relatively small, so it is possible that the current analysis lacks statistical power to detect associations that may be seen with a larger sample size.
Self-reported exposure to chemical weapons was not associated with any of the 12 symptoms despite several studies examining cross-sectional symptoms, medical conditions, and cognitive outcomes reporting differences .7,9,12,51,52 However, comparison of an objective notification from the DOD of Khamisiyah-related sarin exposure was associated with increased odds of trouble concentrating and crying easily and decreased odds of headaches. These symptoms of altered mood and cognitive functioning after nerve agent exposure are consistent with those reported in the literature for other known exposed groups, including those poisoned from the Tokyo subway terrorist attacks in 1995.53 The DoD notified approximately 100,000 veterans who may have been exposed to sarin following the demolition plume, based on where their unit was located.33,34 Although we recognize that the Khamisiyah notified groups may not be the only GW veterans exposed to chemical weapons during the war,54,55 the Khamisiyah incident remains at least one verified and sensitive measure of sarin exposure during the deployment. Our results add to the evidence that the Khamisiyah notification letter is a sensitive surrogate measure of sarin exposure, particularly for those who were at close proximity to the demolition plume. Our group was the first to report a dose--response association of brain imaging outcomes with the Khamisiyah plume estimated exposure levels obtained by DOD26 and this finding has since been partially replicated.56,57 Therefore, these results suggest that self-reported exposure to chemical weapons may not be as sensitive as the Khamisiyah notification letter for longitudinal analyses.
Previous research indicates that symptom reporting remains relatively stable or has increased slightly in GW veterans over time.23 In this sample, significant associations between time since deployment and symptom reporting were observed in 10 of 12 symptoms. Generally, these symptoms significantly increased over time, with the exception of headaches, which decreased. Although speculative, this may be due to veterans seeking effective treatments early after return from deployment for this symptom. The changes in symptom trajectories could indicate emerging or worsening symptoms with age or could reflect normative aging. Porter et al58 found that rates of CMI significantly increased over time in all groups assessed, with GW veterans having the highest prevalence rate compared with era and non-era personnel at each timepoint. It is particularly striking that the symptoms involved in the criteria for CMI are increasing over time in veteran comparison groups (era and non-era personnel) and thus may be related to normal aging symptomatology. However, it was recently demonstrated that GW deployment is associated with accelerated aging such that the average 50-year-old GW deployed veteran exhibits rates of medical conditions that are similar to those seen in 70-year-old non-veterans.12 Thus, symptom trajectories may be altered in this aging population and GW veterans should be carefully monitored for age-related chronic illnesses and treated to prevent further health complications.
Limitations and Strengths
The current analysis was limited to subjects that had data at all three time points, which may limit the generalizability of our results to the greater Ft. Devens cohort and the population of GW veterans as a whole. Indeed, compared with the greater Ft. Devens cohort, the current sample appeared to be more likely to meet the clinical cut off for PTSD and more likely to be Caucasian. Selection bias is also a concern for a variety of reasons. First, selection bias is inherent in surveys, as it is possible that veterans who respond may be different than veterans that do not respond. Concern for selection bias is higher in longitudinal studies, as individuals with more health problems may be more likely to remain in the study than healthy individuals. Alternatively, longitudinal studies also exclude the sickest veterans, who are either too ill to participate, or may have died during the course of the study. However, it is important to note that the FDC is unlike other veteran samples, as they were not recruited from patients at the Department of Veteran Affairs hospitals but rather were recruited and interviewed as a cohort study days after their return from the war.
Another important challenge to studying the effects of GW exposures on veteran health is a lack of records or measurements quantifying chemical exposures during deployment. It may also be the case that other exposures that were not assessed in this cohort may be contributing to chronic health symptoms in this cohort including depleted uranium or other heavy metals that may be better suited to biomarker studies for assessment. However, although three of the four exposures analyzed were self-reported, recall bias was minimized by using exposure data from Follow-up 2, which was less than 5 years after return from the GW and before many exposure-outcome reports had been made public. It is also important to note that the first round of DOD Khamisiyah notification letters were sent out in 1997. The first two surveys included in this study were conducted before the Khamisiyah letters were sent. Therefore, the subjective reporting of symptoms may be less biased, as veterans may not have known that they were exposed to sarin and thus would not attribute their symptoms as such.
The current study was limited to using 12 health symptom variables that were reported at all three time points. Some of the health symptoms assessed differed slightly in wording across the three surveys, and thus may have contributed to the decrease in symptoms observed at follow-up 2. It would be of interest to explore other symptoms commonly reported among GW veterans, including gastrointestinal symptoms such as nausea and diarrhea, respiratory symptoms such as coughing and wheezing, and additional cognitive symptoms including difficulty remembering and trouble finding words. In addition, the analyses presented in this paper reflect grouped data. Therefore, individual variation of symptoms over time may have been masked. Future studies should investigate individual trajectories of symptoms and their associations with exposure. Similarly, results are from a limited sample of GW veterans, and may lack generalizability to a larger population. Finally, analyses were not adjusted for multiple comparisons which increases the chance of type I error.
CONCLUSION
The current longitudinal analysis demonstrated higher odds of symptom reporting associated with exposure to tent heaters, consumption of PB pills, and exposure to sarin/cyclosarin from the Khamisiyah demolitions plume, among a group of GW veterans while controlling for baseline age, active duty status, PTSD status, and sex. In addition, overall, time since deployment was significantly related to symptom reporting indicating that symptoms are increasing over time in this cohort of GW veterans. This increase in symptoms may be the result of normative aging or may be specific to neurotoxicant-induced accelerated aging patterns in certain instances that should be further studied. These results raise concerns about GW veterans’ health more than 25 years after the war. GW veterans should continue to be followed over time by their care providers to properly manage long-term health issues and treat new health issues that may arise.
Footnotes
Kimberly A. Sullivan and Maxine H. Krengel are equal contributors to this article.
Funds for this study came from the Congressionally Directed Medical Research Program (CDMRP), Gulf War Illness Research Program grant # W81XWH-11–1–0818 to Dr. Maxine Krengel.
Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the Department of Defense or the Department of Veteran Affairs. The U.S. Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702-5014 is the awarding and administering acquisition office for this work.
Results indicate that GW neurotoxicant exposures are associated with increased odds of fatigue, mood-cognition, and neurological symptoms. Most strikingly, these health symptoms are increasing over time. These results highlight the importance for the continued screening of symptoms among veterans in exposure subgroups and how typical aging patterns may be influenced.
Krengel, Yee, Zundel, Maule, Heeren, Proctor, and Sullivan have no relationships/conditions/circumstances that present potential conflict of interest.
The JOEM editorial board and planners have no financial interest related to this research.
REFERENCES
- 1.Sullivan KM, Proctor SP, Devin S, Heeren T, White RF. Cognitive functioning in treatment-seeking Gulf war veterans: pyridostigmine bromide use and PTSD. J Psychopathol Behav Assess 2003; 25:95–103.. [Google Scholar]
- 2.Sullivan K, Krengel M, Bradford W, et al. Neuropsychological functioning in military pesticide applicators from the Gulf War: effects on information processing speed, attention and visual memory. Neurotoxicol Teratol 2018; 65:1–13.. [DOI] [PubMed] [Google Scholar]
- 3.RACoGWVI R-G. Gulf War Illness and the Health of Gulf War Veterans Scientific Findings and Recommendation. Washington, DC:Government Printing Office; 2008. [Google Scholar]
- 4.White RF, Steele L, O’Callaghan JP, et al. Recent research on Gulf War illness and other health problems in veterans of the 1991 Gulf War: effects of toxicant exposures during deployment. Cortex 2016; 74:449–475.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Iowa Persian Gulf Study Group. Self-reported illness and health status among Gulf War Veterans. JAMA 1997; 277:238–245.. [PubMed] [Google Scholar]
- 6.Kelsall H, Macdonell R, Sim M, et al. Neurological status of Australian veterans of the 1991 Gulf War and the effect of medical and chemical exposures. Int J Epidemiol 2005; 34:810–819.. [DOI] [PubMed] [Google Scholar]
- 7.Proctor SP, Heeren T, White RF, et al. Health status of Persian Gulf War veterans: self-reported symptoms, environmental exposures and the effect of stress. Int J Epidemiol 1998; 27:1000–1010.. [DOI] [PubMed] [Google Scholar]
- 8.Steele L, Sastre A, Gerkovich MM, Cook MR. Complex factors in the etiology of Gulf War illness: wartime exposures and risk factors in veteran subgroups. Environ Health Perspect 2012; 120:112–118.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White RF, Proctor SP, Heeren T, et al. Neuropsychological function in Gulf War veterans: relationships to self-reported toxicant exposures. Am J Ind Med 2001; 40:42–54.. [DOI] [PubMed] [Google Scholar]
- 10.Petruccelli BP, Goldenbaum M, Scott B, et al. Health effects of the 1991 Kuwait oil fires: a survey of US army troops. J Occup Environ Med 1999; 41:433–439.. [DOI] [PubMed] [Google Scholar]
- 11.Cowan DN, Lange JL, Heller J, Kirkpatrick J, DeBakey S. A case-control study of asthma among U.S. Army Gulf War veterans and modeled exposure to oil well fire smoke. Mil Med 2002; 167:777–782.. [PubMed] [Google Scholar]
- 12.Zundel CG, Krengel MH, Heeren T, et al. Rates of chronic medical conditions in 1991 Gulf war veterans compared to the general population. Int J Environ Res Public Health 2019; 16:949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Michalovicz LT, Locker AR, Kelly KA, et al. Corticosterone and pyridostigmine/DEET exposure attenuate peripheral cytokine expression: Supporting a dominant role for neuroinflammation in a mouse model of Gulf War Illness. Neurotoxicology 2019; 70:26–32.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koo BB, Michalovicz LT, Calderazzo S, et al. Corticosterone potentiates DFP-induced neuroinflammation and affects high-order diffusion imaging in a rat model of Gulf War Illness. Brain Behav Immun 2018; 67:42–46.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abou-Donia MB, Conboy LA, Kokkotou E, et al. Screening for novel central nervous system biomarkers in veterans with Gulf War Illness. Neurotoxicol Teratol 2017; 61:36–46.. [DOI] [PubMed] [Google Scholar]
- 16.Georgopoulos AP, James LM, Carpenter AF, Engdahl BE, Leuthold AC, Lewis SM. Gulf War illness (GWI) as a neuroimmune disease. Exp Brain Res 2017; 235:3217–3225.. [DOI] [PubMed] [Google Scholar]
- 17.Coughlin SS. A neuroimmune model of Gulf war illness. J Environ Health Sci 2017; 3:1–11.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O’Callaghan J, Michalovicz L, Kelly K. Supporting a neuroimmune basis of Gulf War illness. EBioMedicine 2016; 13:5–6.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brewer NT, Hallman WK, Kipen HM. The symmetry rule: a seven-year study of symptoms and explanatory labels among Gulf War veterans. Risk Anal 2008; 28:1737–1748.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dursa EK, Barth SK, Schneiderman AI, Bossarte RM. Physical and mental health status of Gulf war and Gulf era veterans: results from a large population-based epidemiological study. J Occup Environ Med 2016; 58:41–46.. [DOI] [PubMed] [Google Scholar]
- 21.Gwini SM, Kelsall HL, Sim MR, Ikin JF, McFarlane AC, Forbes AB. Stability of symptom patterns in Australian Gulf War veterans: 10-year longitudinal study. Occup Environ Med 2016; 73:195–198.. [DOI] [PubMed] [Google Scholar]
- 22.Hotopf M, David AS, Hull L, Nikalaou V, Unwin C, Wessely S. Gulf war illness: better, worse, or just the same? A cohort study. BMJ 2003; 327:1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kang HK, Li B, Mahan CM, Eisen SA, Engel CC. Health of US veterans of 1991 Gulf War: a follow-up survey in 10 years. J Occup Environ Med 2009; 51:401–410.. [DOI] [PubMed] [Google Scholar]
- 24.Li B, Mahan CM, Kang HK, Eisen SA, Engel CC. Longitudinal health study of US 1991 Gulf War veterans: changes in health status at 10-year follow-up. Am J Epidemiol 2011; 174:761–768.. [DOI] [PubMed] [Google Scholar]
- 25.Ozakinci G, Hallman WK, Kipen HM. Persistence of symptoms in veterans of the First Gulf War: 5-year follow-up. Environ Health Perspect 2006; 114:1553–1557.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Heaton KJ, Palumbo CL, Proctor SP, Killiany RJ, Yurgelun-Todd DA, White RF. Quantitative magnetic resonance brain imaging in US army veterans of the 1991 Gulf War potentially exposed to sarin and cyclosarin. Neurotoxicology 2007; 28:761–769.. [DOI] [PubMed] [Google Scholar]
- 27.Proctor SP, Heaton KJ, Heeren T, White RF. Effects of sarin and cyclosarin exposure during the 1991 Gulf War on neurobehavioral functioning in US army veterans. Neurotoxicology 2006; 27:931–939.. [DOI] [PubMed] [Google Scholar]
- 28.Wolfe J. PS, Davis JD, Borgos MS, Friedman MJ. Health symptoms reported by Persian Gulf War veterans two years after return. Am J Ind Med 1998; 33:104–113.. [DOI] [PubMed] [Google Scholar]
- 29.Wolfe J.F PS, Erickson D, Hu H. Risk factors for multisymptom illness in US army veterans of the Gulf war. J Environ Med 2002; 44:271–281.. [DOI] [PubMed] [Google Scholar]
- 30.Yee MK, Seichepine DR, Janulewicz PA, Sullivan KA, Proctor SP, Krengel MH. Self-reported traumatic brain injury, health and rate of chronic multisymptom illness in veterans from the 1990-1991 Gulf war. J Head Trauma Rehabil 2016; 31:320–328.. [DOI] [PubMed] [Google Scholar]
- 31.Yee MK, Janulewicz PA, Seichepine DR, Sullivan KA, Proctor SP, Krengel MH. Multiple mild traumatic brain injuries are associated with increased rates of health symptoms and Gulf war illness in a cohort of 1990-1991 Gulf war veterans. Brain Sci 2017; 7:pii: E79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bartone PT, Ursano RJ, Wright KM, Ingraham LH. The impact of a military air disaster on the health of assistance workers. J Nerv Ment Dis 1989; 177:317–328.. [DOI] [PubMed] [Google Scholar]
- 33. Directorate for Deployment Health Support of the Special Assistant to the Under Secretary of Defense (Personnel and Readiness) for Gulf War Illness Medical Readiness and Military Deployment. Potential exposure to sarin from the demolitions at Khamisiyah, Iraq on March 10, 1991 Available at: http://www.gulflink.osd.mil; 1997. [Google Scholar]
- 34. Directorate for Deployment Health Support of the Special Assistant to the Under Secretary of Defense (Personnel and R eadiness) for Gulf War Illness Medical Readiness and Military Deployments. US Demolition Operations at the Khamisiyah ammunition point (case narrative). Available at: http://www.gulflink.osd.mil/khamisiyahiii; 2002. Accessed September 19, 2019. [Google Scholar]
- 35.Fukuda K. NR, Stewart G, Thompson WW, et al. Chronic multisymptom illness affecting Air Force veterans of the Gulf War. JAMA 1998; 280:981–988.. [DOI] [PubMed] [Google Scholar]
- 36.(RAC-GWVI), RACoGWV.I.. Gulf War Illness and the Health of Gulf War Veterans: Research Update and Recommendations 2009-2013. Washington, DC:Government Printing Office; 2014. [Google Scholar]
- 37.Steele L. Prevalence and patterns of Gulf war illness in Kansas veterans: association of symptoms with characteristics of person, place, and time of military service. Am J Epidemiol 2000; 152:992–1002.. [DOI] [PubMed] [Google Scholar]
- 38.Golomb BA, Anthony CR. A Review of the Scientific Literature As It Pertains to Gulf War Illnesses: Pyridostigmine Bromide. Santa Monica, CA:RAND Corporation; 1999. [Google Scholar]
- 39.Grob D, Harvey JC. Effects in man of the anticholinesterase compound sarin (isopropyl methyl phosphonofluoridate). J Clin Invest 1958; 37:350–368.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McDonough JHST. Neuropharmacological mechanisms of nerve agent-induced seizure and neuropathology. Neurosci Biobehav Rev 1997; 21:559–579.. [DOI] [PubMed] [Google Scholar]
- 41.National Academies of Science, Engineering, and Medicine. Gulf War and Health: Volume 10: Update of Health Effects of Serving in the Gulf War 2016. Washington, DC:National Academy of Sciences; 2016. [Google Scholar]
- 42.Golomb BA. Acetylcholinesterase inhibitors and Gulf War illnesses. Proc Natl Acad Sci U S A 2008; 105:4295–4300.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fields DD, Belgrad J, Robnett M. Cholinergic signaling in myelination. Glia 2017; 65:687–698.. [DOI] [PubMed] [Google Scholar]
- 44.Belgrad J, Dutta DJ, Bromley-Coolidge S, et al. Oligodendrocyte involvement in Gulf war illness. Glia 2019; 67:2107–2124.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Banks CN, Lein PJ. A review of experimental evidence linking neurotoxic organophosphorus compounds and inflammation. Neurotoxicology 2012; 33:575–584.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Milligan ED, Watkins LR. Pathological and protective roles of glia in chronic pain. Nat Rev Neurosci 2009; 10:23–36.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morris G, Berk M, Walder K, Maes M. Central pathways causing fatigue in neuro-inflammatory and autoimmune illnesses. BMC Med 2015; 13:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.O’Callaghan JP, Kelly KA, Locker AR, Miller DB, Lasley SM. Corticosterone primes the neuroinflammatory response to DFP in mice: potential animal model of Gulf War Illness. J Neurochem 2015; 133:708–721.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Parihar VK, Hattiangady B, Shuai B, Shetty AK. Mood and memory deficits in a model of Gulf War illness are linked with reduced neurogenesis, partial neuron loss, and mild inflammation in the hippocampus. Neuropsychopharmacology 2013; 38:2348–2362.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Golier JA, Legge J, Yehuda R. The ACTH response to dexamethasone in Persian Gulf War veterans. Ann N Y Acad Sci 2006; 1071:448–453.. [DOI] [PubMed] [Google Scholar]
- 51.Chao LL. Associations between the self-reported frequency of hearing chemical alarms in theater and visuospatial function in Gulf war veterans. J Occup Environ Med 2016; 58:1014–1020.. [DOI] [PubMed] [Google Scholar]
- 52.Janulewicz P, Krengel M, Quinn E, et al. The multiple hit hypothesis for Gulf war illness: self-reported chemical/biological weapons exposure and mild traumatic brain injury. Brain Sci 2018; 8:pii: E198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yokoyama K. Our recent experiences with sarin poisoning cases in Japan and pesticide users with references to some selected chemicals. Neurotoxicology 2007; 28:364–373.. [DOI] [PubMed] [Google Scholar]
- 54.Haley RW, Tuite JJ. Epidemiologic evidence of health effects from long-distance transit of chemical weapons fallout from bombing early in the 1991 Persian Gulf War. Neuroepidemiology 2013; 40:178–189.. [DOI] [PubMed] [Google Scholar]
- 55.Tuite JJ, Haley RW. Meteorological and intelligence evidence of long-distance transit of chemical weapons fallout from bombing early in the 1991 Persian Gulf War. Neuroepidemiology 2013; 40:160–177.. [DOI] [PubMed] [Google Scholar]
- 56.Chao LL, Zhang Y, Buckley S. Effects of low-level sarin and cyclosarin exposure on white matter integrity in Gulf War Veterans. Neurotoxicology 2015; 48:239–248.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chao LL, Abadjian L, Hlavin J, Meyerhoff DJ, Weiner MW. Effects of low-level sarin and cyclosarin exposure and Gulf War Illness on brain structure and function: a study at 4T. Neurotoxicology 2011; 32:814–822.. [DOI] [PubMed] [Google Scholar]
- 58.Porter B, Long K, Rull RP, Dursa EK. Millennium Cohort Study. Prevalence of chronic multisymptom illness/Gulf war illness over time among millennium cohort participants, 2001 to 2016. J Occup Environ Med 2020; 62:4–10.. [DOI] [PubMed] [Google Scholar]


