Background:
Rib fractures are a common thoracic injury that is encountered in 20% to 39% of patients with blunt chest trauma and is associated with substantial morbidity and mortality1,2. Traditionally, the majority of patient with rib fractures have been managed nonoperatively. Recently, the utilization of surgical stabilization of rib fractures has increased considerably because the procedure has shown improved outcomes3-5.
Description:
Surgical stabilization should be considered in cases of multiple bicortically displaced rib fractures, especially in those with a flail chest and/or a concomitant ipsilateral displaced midshaft clavicular fracture or sternal fracture, as such cases may result in thoracic wall instability. For surgical stabilization of rib fractures, we classify rib fractures by location, type of fracture, and degree of displacement after obtaining thin-sliced chest computed tomography (CT) scans. The incision is selected depending on the fracture location, and the surgical technique is chosen relevant to the type of fracture. Single-lung intubation is preferred if there is no severe contralateral pulmonary contusion. We favor performing video-assisted thoracoscopy if possible to control bleeding, evacuate hematomas, repair a lung, and perform cryoablation of the intercostal nerves. A lateral approach is considered to be the main surgical approach because it allows access to the majority of rib fractures. A curvilinear skin incision is made overlying the fractured ribs. Posterior rib fractures are exposed through a vertical incision within the triangle of auscultation, and anterior fractures, through a transverse inframammary incision. The muscle-sparing technique, splitting alongside fibers without transection, should be utilized if possible and supplemented by muscle retraction. For surgical stabilization of rib fractures, we currently prefer precontoured side and rib-specific plates with threaded holes and self-tapping locking screws. Polymer cable cerclage is used to enhance plating of longitudinal fractures, rib fractures near the spine, osteoporotic ribs, and injuries of rib cartilage. The third to eighth ribs are plated most often. Intercostal muscle deficit, if present, is repaired with a xenograft patch. In comminuted rib fractures, the bone gap is bridged with bone graft. Surgical stabilization of rib fractures is recommended within the first 7 days after trauma, preferably within the first 3 days6-8.
Alternatives:
Nonoperative treatment alternatives include (1) epidural analgesia when not contraindicated because of anticoagulant venous thromboembolism prophylaxis9,10; (2) thoracic paravertebral blockage, e.g., serratus anterior or erector spinae plane nerve block11,12; (3) intercostal nerve block; (4) intravenous or enteral analgesics, e.g., opioids, acetaminophen, and nonsteroidal anti-inflammatory drugs (NSAIDs); (5) intrapleural analgesia, e.g., bupivacaine infusion; and (6) multimodal analgesia that incorporates regional techniques, systemic analgesics, and analgesic adjuncts9.
Rationale:
Surgical stabilization of rib fractures is a safe and effective method to treat displaced rib fractures. The procedure provides definitive stabilization of fractures, improves pulmonary function, lessens pain medication requirements, prevents deformity formation, and results in reduced morbidity and mortality.
Introductory Statement
This article provides practicing surgeons with detailed surgical techniques for SSRF in frequently encountered clinical scenarios1-12.
Key Steps
Imaging: chest computed tomography (CT) scan.
Determination of indications and the order for surgical stabilization of rib fractures (SSRF) based on fracture characteristics and patient’s co-injuries.
Selection of the surgical approach based on fracture location, type, and displacement.
Intubation options (single or double-lung ventilation).
Cryoablation of the intercostal nerves.
Surgical stabilization of the rib fractures.
Immediate postoperative wound care and chest tube placement.
Indications & Contraindications1,13-17
Indications
Flail chest, defined radiographically as displaced segmental rib fractures with ≥3 consecutive ribs fractured in ≥2 places or clinically by visible paradoxical chest-wall movement.
Multiple rib fractures with bicortical displacement.
Fractured ribs acting as penetrating objects.
Displaced rib fractures combined with sternal fractures and/or ipsilateral displaced midshaft clavicle fractures.
Uncontrolled pain with failure of nonoperative treatment.
Chest-wall deformity, especially with reduction of thoracic volume (Figs. 1-A and 1-B).
Acute respiratory distress syndrome in patients with thoracic-cage instability.
Displaced rib fractures found during thoracotomy for other reasons.
Chronic pain in cases of symptomatic rib nonunion.
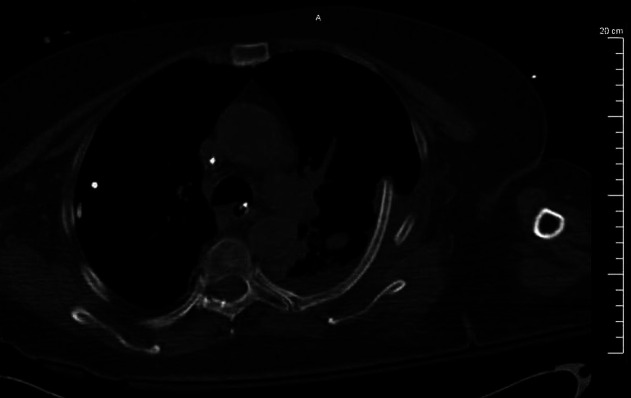
Figs. 1-A and 1-B Coronal (Fig. 1-A) and axial (Fig. 1-B) CT scans showing multiple left-sided displaced rib fractures with severe reduction of thoracic volume and chest-wall deformity.
Fig. 1-A.
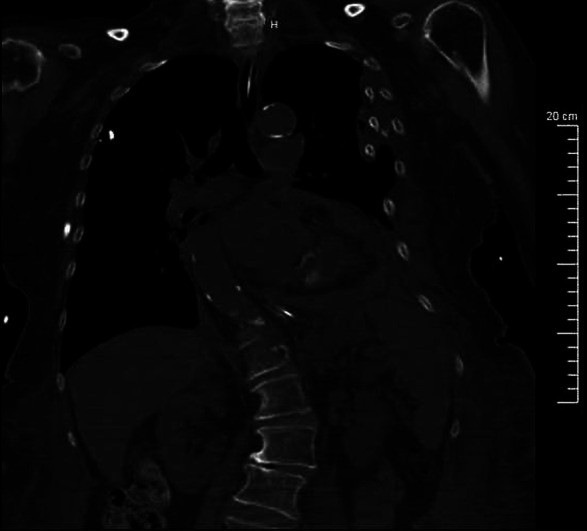
Fig. 1-B.
Contraindications
Hemodynamic instability.
Traumatic brain injury (Glasgow Coma Scale, ≤10).
Infection: pleural empyema, mediastinitis, severe pneumonia.
Need for long-term mechanical ventilation for other reasons.
Unstable spinal or pelvic fractures, because these fractures must be stabilized prior to SSRF.
Relative Contraindications
Severe pulmonary contusion of the contralateral lung.
Contaminated surgical field.
Local infection of the anterior chest wall outside of the surgical field.
Fungal colonization of the mediastinum17.
Step-by-Step Description of Procedure
Step 1: General Considerations for SSRF
After characterization of rib fractures and selection of ribs for fixation, timing of the surgical procedure and sequence of plating are determined.
-
Classification.
-
○
For the purpose of surgical stabilization, we classify rib fractures by location, type of fracture, and degree of displacement (see Appendix). This classification works as an algorithm of action to help surgeons with the decision-making process. The decision to perform SSRF is made on the basis of the degree of displacement. The incision is then selected depending on the fracture location, and surgical technique is chosen relevant to the type of fracture.
-
○
-
Timing of the surgical procedure.
-
○
For acute rib fractures, we perform the surgical procedure as soon as possible after the decision is made and tend to perform SSRF within the first 7 days after the trauma. Performing the surgical procedure within the first 3 days after trauma is recommended because inflammation and callus formation have yet to begin and, therefore, fracture reduction is less difficult, leading to a technically easier procedure6.
-
○
-
Selection of ribs for SSRF.
-
○
We plate displaced ribs from the second to tenth; however, we usually stabilize ribs from the third to the eighth. Ribs 4 to 7 are plated most often because they are fractured more frequently and also contribute more to the chest-wall movement. SSRF of the second rib is rarely performed because it requires extra exposure and is more technically challenging, and therefore is justified when additional indications are present (e.g., a displaced ipsilateral midshaft clavicle fracture). In cases of fractured and severely displaced eleventh and/or twelfth ribs, these ribs are excised.
-
○
-
Sequence of plating.
-
○
When several ribs are fractured and require stabilization, we prefer to start from the epicenter of the chest wall trauma (usually the most displaced fractures).
-
○
The sequence of plating may also depend on the need to reposition the patient and to change the exposure and dressing; therefore, all ribs accessible from the main surgical approach are stabilized first.
-
○
-
Selective stabilization versus all-ribs stabilization.
-
○
Stabilization of all displaced ribs that are accessible through the main incision is preferred. The reason for plating the maximum possible number of ribs is to avoid the risk of subsequent displacement, which may occur rapidly and cause cardiopulmonary injuries18. The other reasons include the prospect of deformity formation and recalcitrant pain in cases of nonunion.
-
○
Selective plating can be utilized if some fractures have moderate displacement and if the number of fractured ribs is limited (≤3), therefore not requiring stabilization. Selective plating can also be implemented if the condition of the patient deteriorates and, as a result, the surgical procedure must be abbreviated or aborted.
-
○
-
Bilateral rib plating.
-
○
When bilateral rib plating is performed, the surgical procedure starts from the more severely injured side. The patient is placed in a semilateral position to reduce the load on the contralateral fractured ribs and with the healthier hemithorax down. Preoperatively, a chest tube must be placed into the contralateral hemithorax to prevent possible tension pneumothorax. We prefer to perform SSRF on the contralateral side 24 to 48 hours after the first surgical procedure. In a rare scenario in which multiple bilateral displaced rib fractures with concomitant sternal fracture result in an unstable thorax, a bilateral procedure is performed under the same anesthesia.
-
○
Step 2: Preoperative Preparation
CT imaging with rib-thickness measurements, endotracheal intubation (single-lung intubation preferred), and video-assisted thoracoscopy (VATS) are followed by cryoablation of intercostal nerves.
-
Imaging.
-
○
Chest CT scans without contrast (1 or 2-mm slices) are taken. Regular CT is enough to appreciate the number and location of the fractured ribs. On the initial CT scans with the patient in the supine position, posterior rib fractures may be partly reduced and, consequently, the degree of displacement may be underestimated. Therefore, we recommend CT scans be made on inspiration, which allows for more displacement to occur; this is easier to do if the patient is under anesthesia. On the CT scan, measurement of the ribs (coronal view) and sternal thickness (sagittal view) is made to estimate the screw length, assuming perpendicular screw positioning.
-
○
When the patient is positioned for the surgical procedure, intraoperative CT scans with 3-dimensional reconstruction are useful to help estimate the extent and location of the skin incision, especially in morbidly obese patients and particularly with posterior fractures (Fig. 2). In such cases, the patient is placed on a beanbag in a lateral or semilateral decubitus position.
-
○
-
Antimicrobial and venous thromboembolism prophylaxis.
-
○
For prophylaxis against infection and thromboembolism, we follow the previously published guidelines6. Weight-based antimicrobial therapy is administered within 30 to 60 minutes of the incision (e.g., 30 minutes for cefazolin). For patients with a penicillin allergy, vancomycin or clindamycin is administered 120 minutes prior to incision. Appropriate intraoperative redosing should be timed from the initial antibiotic administration, not from the incision time.
-
○
Venous thromboembolism pharmacoprophylaxis is performed with subcutaneous injections of 30-mg low-molecular-weight heparin twice daily, with the first injection given 4 hours prior to the surgical procedure and the next within 12 hours after the procedure (if not contraindicated for intracranial hemorrhage, epidural placement, heparin-induced thrombocytopenia, etc.) and, in higher-risk patients, continued with subcutaneous intraoperative administration of 5,000 units of heparin as well as pneumatic compression of the lower extremities. Postoperatively, we continue prophylaxis with 30-mg low-molecular-weight heparin subcutaneous injections twice daily.
-
○
-
Operating table.
-
○
A standard operating table that has the ability to flex in order to help open the intercostal space can be used if no additional imaging will be required. We utilize a Jackson or a diving-board table when the patient must be in the prone position and/or when intraoperative CT scans are planned (e.g., to improve visualization in morbidly obese patients or in cases of posterior fractures).
-
○
-
Intubation.
-
○
Prior to positioning the patient for the selected surgical approach, the patient is placed in the supine position and intubated with a standard single lumen endotracheal tube with the largest possible diameter (preferred size, 8 Shiley or larger).
-
○
Although single-lung intubation is not mandatory for SSRF, it is useful to improve exposure and avoid injury to the lung parenchyma during the surgical procedure and aids in performing VATS and cryoablation of the intercostal nerves. A severe contralateral pulmonary contusion may limit tolerance to single-lung intubation1.
-
○
-
VATS.
-
○
We often perform VATS prior to SSRF. The purpose of VATS is to control the intercostal vessel bleeding, evacuate hematomas, wash out the chest cavity, perform lung repair/resection, repair the diaphragm, and appreciate the level of protrusion of bone fragments into the chest cavity and reduce them (Fig. 3). VATS also aids in visualization of the spine if intercostal nerve ablation is performed.
-
○
-
Cryoablation of the intercostal nerves.
-
○
We routinely perform a cryogenic nerve block of multiple intercostal nerves in order to reduce the amount of medication required for pain management, particularly opioid administration19. Cryoablation causes axonotmesis and provides extended pain relief compared with an intercostal anesthetic nerve block. This extended pain relief, with pain management throughout the entire postoperative period, is associated with better fracture-healing times. Following cryoablation, cutaneous sensation is gradually restored over 2 to 6 months as a result of nerve regeneration along the remaining perineural structures. The other reason to implement cryoablation is the fact that the patient is already undergoing a surgical procedure, so separate arrangements for the procedure would not be required. The effectiveness of cryoablation in pain management was confirmed by previously published studies and includes rapid pain relief, reduction of narcotic medication, and long-term chest-wall analgesia19,20. Depending on the extent of the fractures, we ablate from the third up to the ninth intercostal nerve (Fig. 4, Video 1). The cryoSPHERE or cryoICE probe (AtriCure) is used depending on the anatomy of the patient or fracture location. The probe is positioned 2 to 4 cm lateral to the spine in order to avoid iatrogenic injury to the sympathetic chain and is applied to the inferior edge of the rib. We prefer to perform cryogenic nerve block during VATS because it is easier to reach all necessary locations with the probe when the lung is deflated; however, cryogenic nerve block can also be performed during thoracotomy.
-
○
Fig. 2.
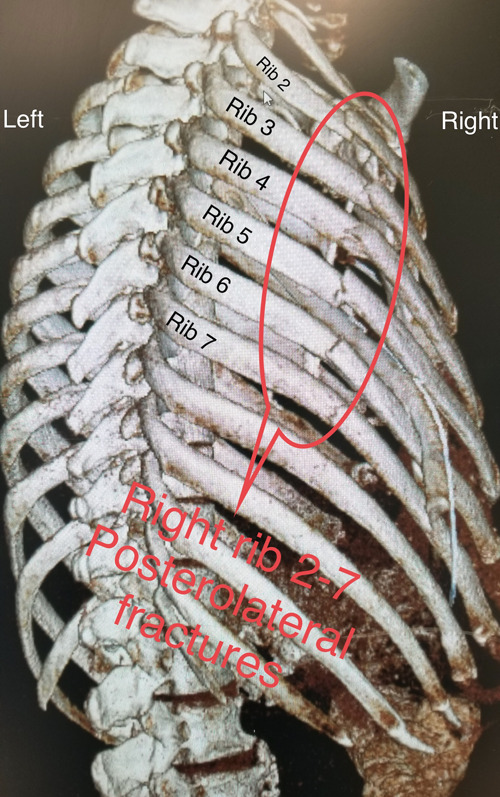
Three-dimensional CT scan reconstruction of multiple rib fractures. Shown are multiple severely displaced lateral rib fractures.
Fig. 3.
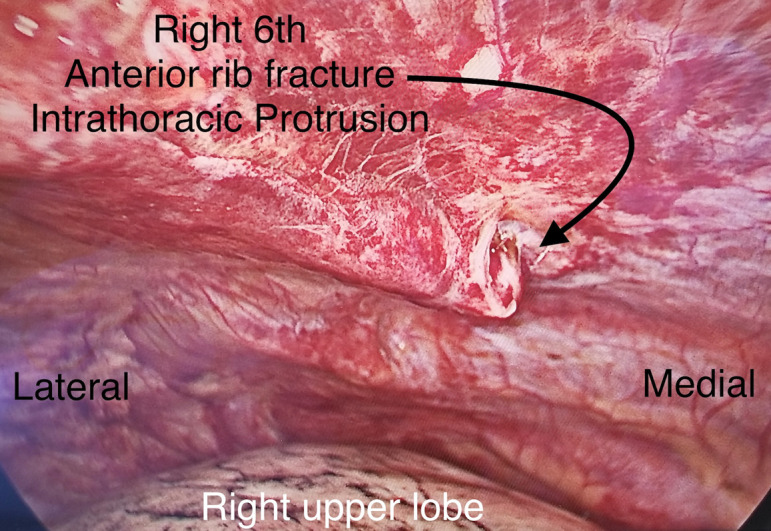
VATS. The patient is in the left lateral decubitus position. The black arrow indicates a severely displaced anterior fracture of the sixth rib protruding into the right hemothorax. The right lung is deflated and is seen at the bottom.
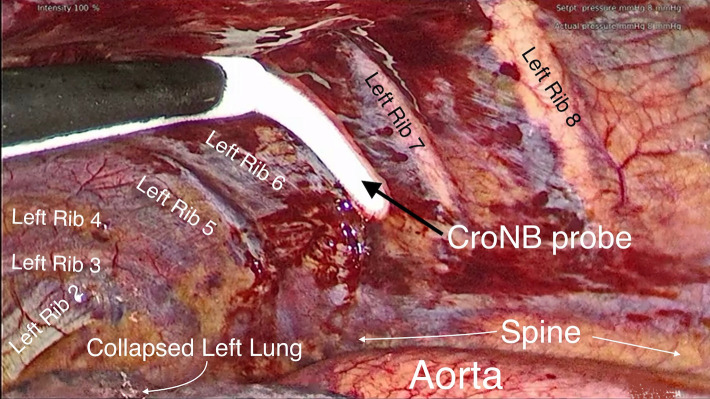
Fig. 4.
Cryoablation of the intercostal nerves utilizing an AtriCure probe. The patient is in the right lateral decubitus position. The black arrow points to the probe resting on the left sixth intercostal nerve during cryoablation. Ice condensate buildup can be seen on the tip of the probe.
Video 1.
Cryoablation of the intercostal nerves during VATS.
Step 3: Clinical Scenarios
The type and location of rib fractures encountered in different clinical scenarios will determine the selection of an appropriate incision and the optimal surgical stabilization technique.
-
Flail chest and segmental rib fractures.
-
○
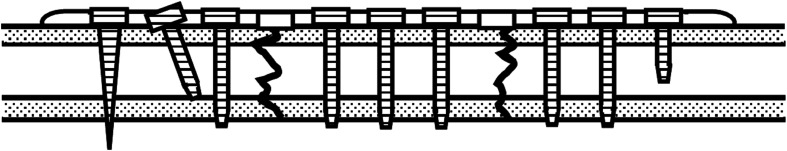
In cases of flail chest or displaced segmental fractures, we recommend stabilization o f all fractures of each rib involved with use of long plates and locking screws. The advantage of using 1 long plate instead of 2 short plates is improved fixation through reduced stiffness of the implant. The long plate must cover 2 fracture lines of the segmental fracture, have 3 holes over the displaced segment, and have at least 3 holes on each side (lateral and medial) of the segment. The long plate has a minimum of 11 holes, with 9 holes designated for screws and 2 holes left empty above the fracture lines (Fig. 5).
-
○
-
Rib fractures combined with clavicular fracture.
-
○
In cases of upper rib fractures combined with an ipsilateral displaced clavicular fracture, we tend to plate ribs as high as possible (e.g., stabilizing the second rib), and we also recommend clavicular plating. It has been reported that displacement rates of midshaft clavicular fractures increased significantly in the presence of ipsilateral upper rib fractures21. It has also been reported that one-third of patients with a first-rib fracture (isolated or combined with other rib fractures) had a clavicular fracture22. Solberg et al. described the nonunion of clavicular fractures when SSRF was not accompanied by surgical repair of clavicular fractures23.
-
○
-
Rib fractures near the spine.
-
○
When a posterior rib fracture is located close to the spine in the tubercle region, we perform plating only if at least 2 plate holes can be positioned on the neck of the rib, which requires approximately 20 to 25 mm of space between the head and tubercle (Fig. 6). Careful contouring of the plate to match the curved neck segment is required. We do not perform SSRF if the fracture is located closer to the spine. We also reinforce the stabilization by adding a ZIPFIX polymer cable cerclage (DePuy Synthes) on the top of the plate (Fig. 7), which is a polyetheretherketone (PEEK) biocompatible cable tie system with a self-locking ratchet for fast fixation of the sternum. We use this stabilization system as reinforcement of plating in certain clinical scenarios, including sternal fractures combined with long longitudinal rib fractures, in cases of osteoporotic bone, rib cartilage fractures, and fracture locations that do not allow the placement of at least 3 screws on each side of a fracture for plate attachment to the rib.
-
○
-
Rib fractures combined with spine fractures.
-
○
When a surgical procedure in the spine is required in patients with rib fractures, the sequence of procedures is determined by collaborative efforts with a spine surgeon. In general, spine surgery should be done first.
-
○
In patients with an unstable spine fracture and flail chest who may experience cardiopulmonary collapse because of prone positioning while undergoing spinal instrumentation and fusion, chest support from the anterior portion of a rigid thoracolumbosacral orthosis brace (with extra padding at the shoulders and iliac crest) may be utilized along with standard hip and chest bolsters24. If this is not possible, in the rare situation in which an additional sternal fracture is present, stabilization of the sternum is performed first with the patient in a supine position, followed by the spinal procedure in a prone position, and then by SSRF. The latter can be delayed if needed (patient condition, anesthesia time too long, etc.).
-
○
-
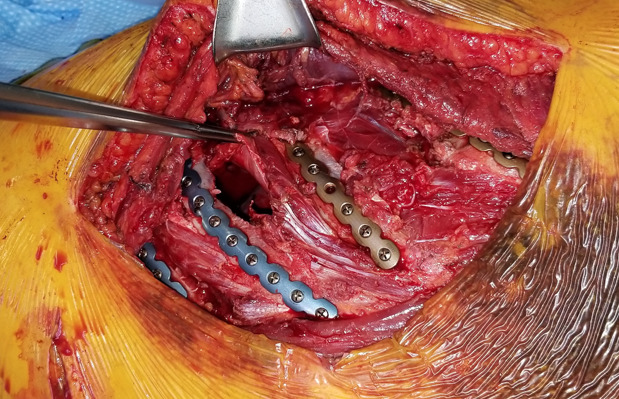
Rib fractures with concomitant sternal fractures.
-
Rib fractures with intercostal muscle deficit.
-
○
When rib fractures are combined with defects of the intercostal muscles, in order to prevent lung herniation, we repair the defect with a xenograft or a synthetic mesh (Fig. 9). To prevent shifting of the patch, we anchor it by several sutures to the surrounding tissues of the anterior chest wall and also circumferentially encompass the ribs. Xenograft can also be positioned on the surface of the ribs, just on top of the plates, or in an underlay configuration (Fig. 10).
-
○
-
Fractures of the rib cartilage.
-
○
In cases of chondral fracture, we use a long plate to span the lesion and secure the plate medially to the sternum and laterally to the osseous part of the rib, thereby avoiding putting screws through the cartilage (Fig. 11).
-
○
-
Rib fractures with bone deficit (gap fractures).
-
○
Free rib fragments in cases of comminuted fractures should be removed. Definitive apposition without tension should be achieved after reduction and prior to fracture plating. It is possible to accomplish this only when the gap between the edges of the fractured ribs is <10 mm. If tension or a gap is present, an autologous bone graft from the iliac crest or an allogenic rib graft should be used to bridge the gap. Even a small gap should not be left or spanned by a plate without the use of a graft. The plate goes on the top of the bridged fracture with at least 1 screw directed through the bone graft (more screws can be used depending on the length of the graft), complemented by a polymer cerclage cable tie and at least 3 screws positioned on each side of the fracture (Figs. 12 and 13). First, on a tray table outside of the wound, the bone graft is predrilled and attached to the plate by bicortical self-tapping locking screw(s) (Figs. 14 and 15). The plate-bone assembly is then attached to the dorsal end of the fractured rib, followed by definitive apposition and final fixation to the ventral end of the fractured rib.
-
○
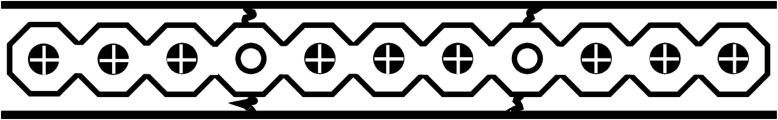
Fig. 5.
Diagram of a long plate stabilizing a reduced segmental rib fracture. The long plate must cover the 2 fracture lines of the segmental fracture. It is preferred to have 3 holes over the displaced segment with at least 3 holes on each side (lateral and medial) of the segment. Two plate holes are left empty above the fracture lines.
Fig. 6.
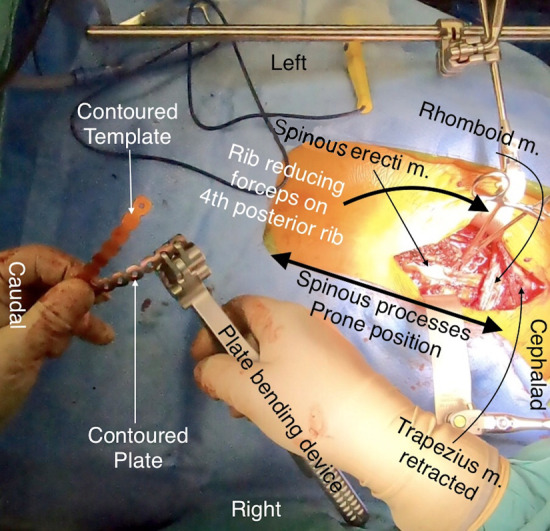
Intraoperative photograph showing the repair of a severely displaced left posterior paraspinous rib fracture. The patient is in the prone position. A Thompson retractor is seen at the top. Black arrows point to the left-sided spinal erector muscle, trapezius muscle, and rhomboid muscle. A curved thick black arrow points to the left posterior fracture of the fourth rib, which was reduced and held in place with rib reducing forceps. A plate-bending device is shown, which was used to further bend the precontoured left-sided fourth rib plate against a bent/shaped contoured template.
Fig. 7.
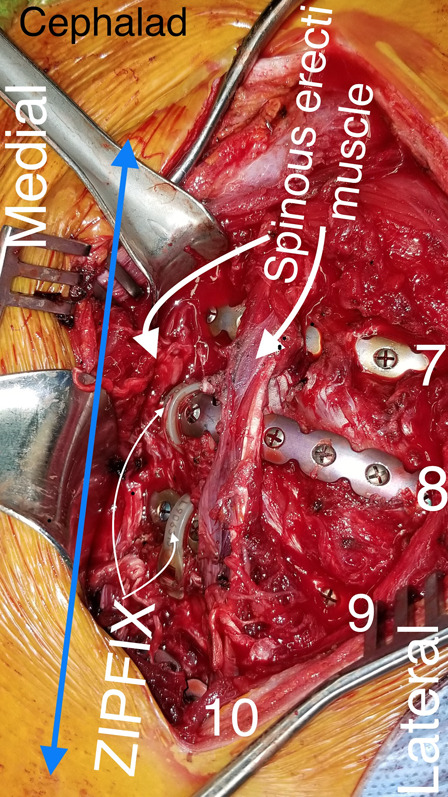
Intraoperative photograph showing posterior fractures of right ribs 7 to 10. The patient is in the prone position. A blue double arrow denotes the spine. Ribs 7 to 10 are numbered. Thin white arrows show ZIPFIX bands placed in a paraspinous fashion on the right eighth and ninth ribs. The erector spinae muscles are noted with thick white arrows.
Fig. 8-A.
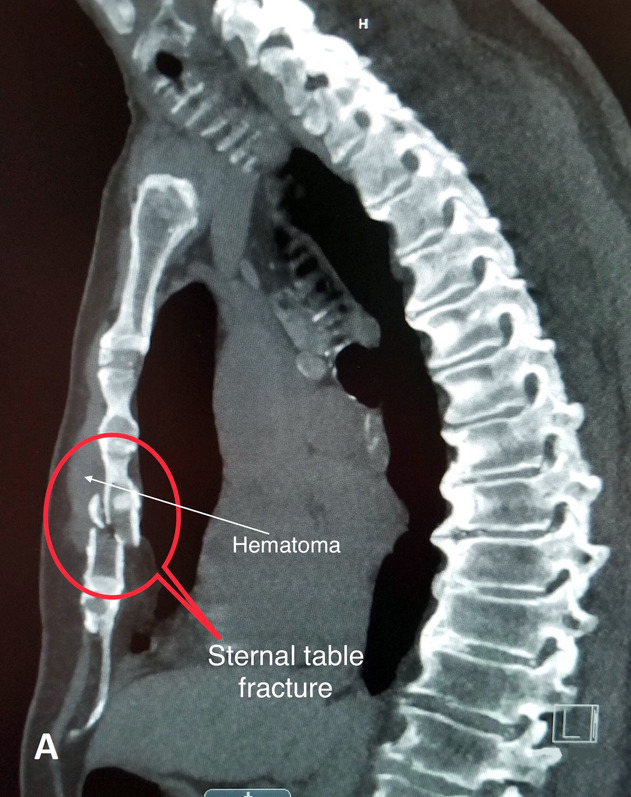
Lateral CT scan showing a displaced sternal fracture.
Fig. 8-B.
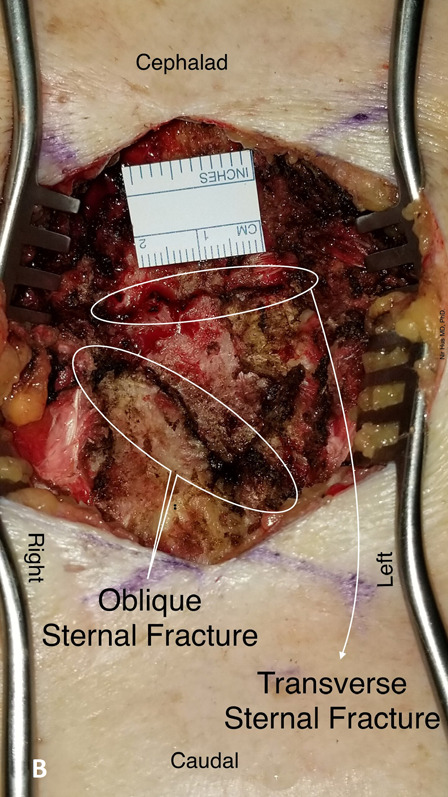
Intraoperative photograph showing transverse and oblique sternal fractures.
Fig. 8-C.
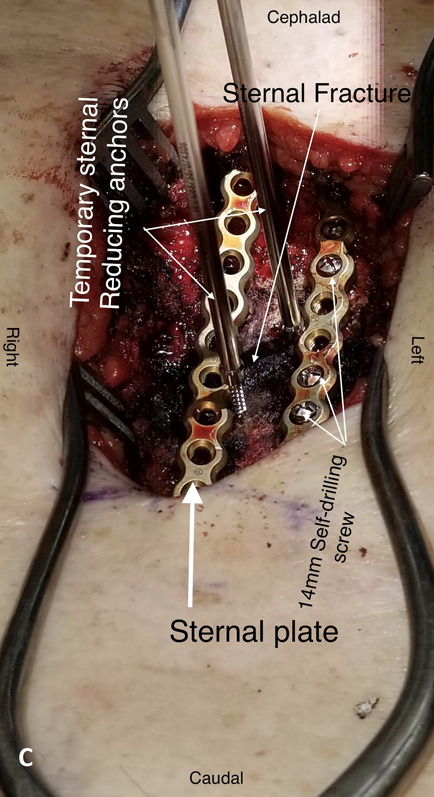
Intraoperative photograph showing sternal fractures stabilized by 2 parallel threaded sternal plates (contoured to conform to the shape of the sternum) with self-drilling screws.
Fig. 8-D.
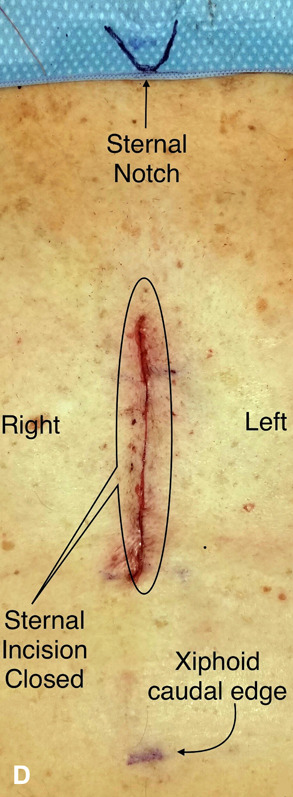
Photograph showing the skin incision closed with a cosmetic suture.
Fig. 9.
Intraoperative photograph showing multiple rib fractures with intercostal muscle defect. Reduced rib fractures are stabilized with precontoured titanium alloy plates with threaded holes.
Fig. 10.
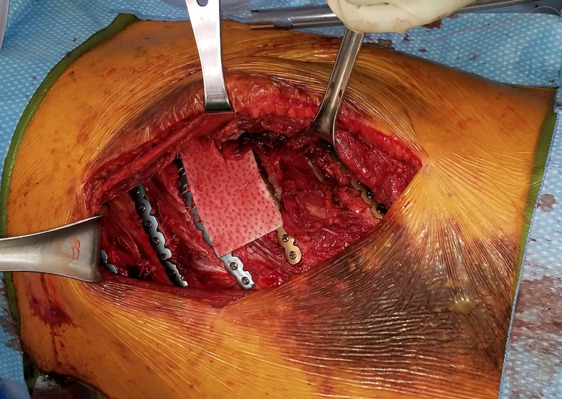
Intraoperative photograph made after plating 5 fractured ribs, showing the muscle defect covered with a xenograft positioned directly above the plates and secured with sutures to the surrounding tissues and ribs.
Fig. 11.
Intraoperative photograph showing multiple left-sided fractures of rib cartilage (ribs 3 to 6) stabilized by long threaded plates and cerclage fixation. Empty plate holes are seen above the fractured cartilage. The left pectoralis major muscle is retracted laterally. The plates are attached by screws medially to the sternum and laterally to the osseous part of the rib, with no screws through the cartilage. The manubrium fracture is stabilized by an H-shaped sternal plate (white arrow).
Fig. 12.
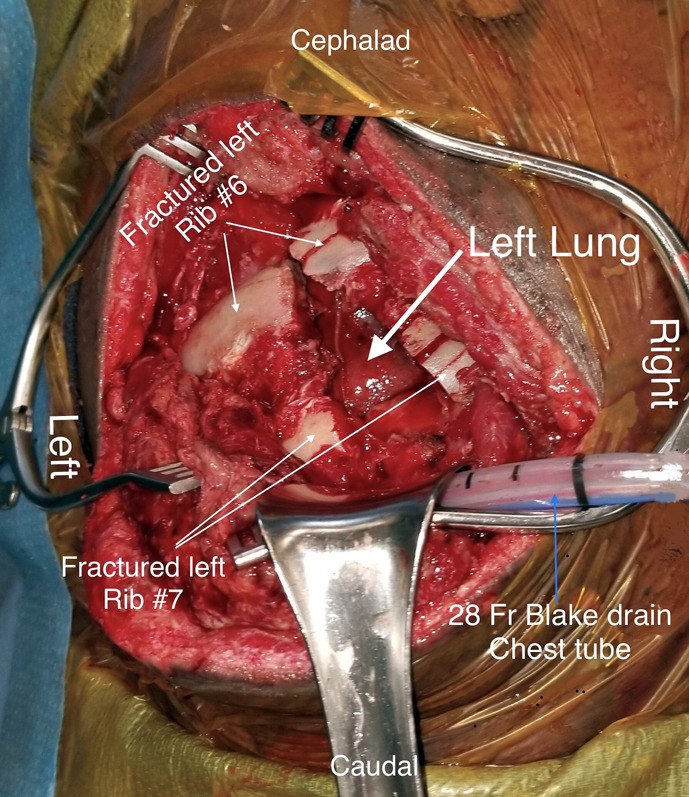
Intraoperative photograph made with the patient in the lateral decubitus position showing a traumatic lung herniation through injured intercostal muscle between left ribs 5/6, 6/7, and 7/8. Gap fractures of the left sixth and seventh ribs with bone deficits are shown. A thick arrow points to the left lung. Thin white arrows point to left sixth and seventh ribs. A thin blue arrow points to a 28 French gauge Blake drain chest tube.
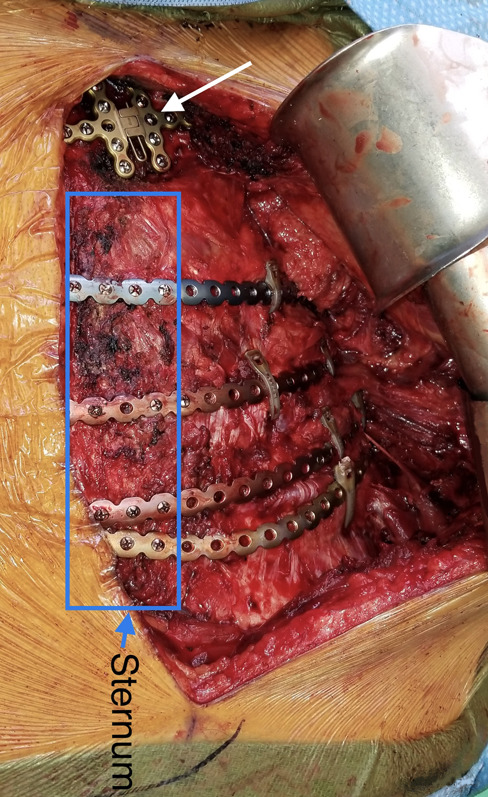
Fig. 13.
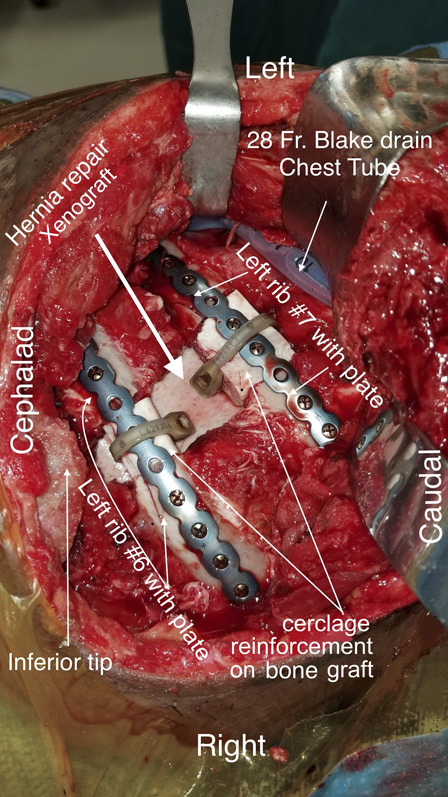
Intraoperative photograph showing repair of a traumatic hernia with destruction of a portion of the intercostal muscles between ribs 5/6, 6/7, and 7/8. Bone deficit is seen in the left sixth and seventh ribs. A thick white arrow shows a xenograft underlay repair of the traumatic hernia. Ribs 6 and 7 are repaired with precontoured rib-specific plates and a cadaveric bone graft to bridge the gaps. Polymer cerclage bands are utilized to further secure the bone graft to the plates when there is an insufficient number of anchoring screws (≤3). The inferior tip of the scapula is shown and labeled. A 28 French gauge Blake drain is used as a chest tube.
Fig. 14.
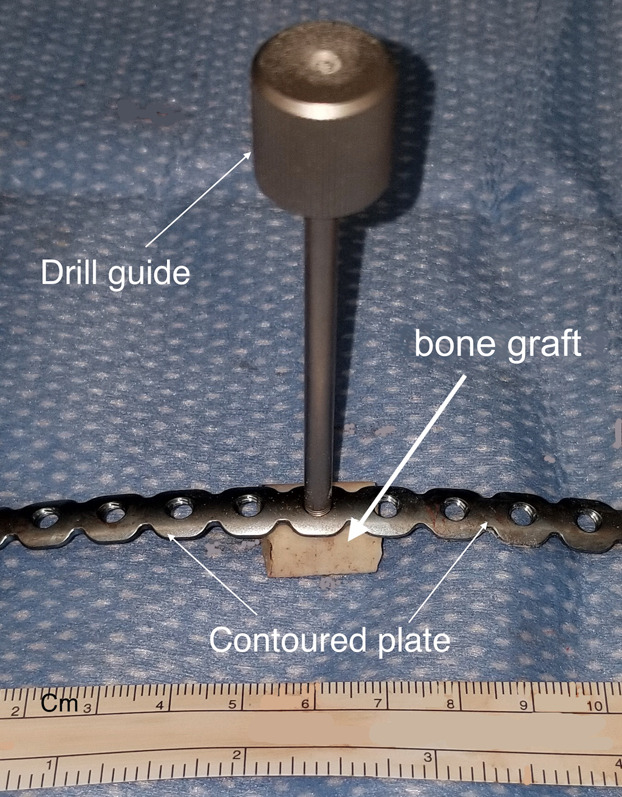
Photograph showing a bone graft (17 mm long) for gap fracture repair with a threaded plate and drill guide.
Fig. 15.
Photograph showing a plate-bone graft assembly before attachment to the rib.
Step 4: General Guidelines
General guidelines are applicable to all of the surgical approaches used in SSRF.
-
Patient positioning.
-
○
Patient positioning depends on the selected surgical approach, which in turn is determined by the location of the fracture.
-
○
-
Incision.
-
○
The optimal incision is marked on the skin over the epicenter of the fractured ribs. Anatomical landmarks such as the sternum, suprasternal notch, xiphoid, spinous processes, mid-clavicular or axillary lines, and inferior scapular angle (dependent on arm position) are also marked to help with the orientation and length of the incision. Dermatome-based skin incisions with muscle-sparing and muscle-splitting techniques are implemented.
-
○
-
Muscle-sparing technique.
-
○
The important first step of this technique is to create subcutaneous flaps superficial to the fascia and subsequently identify the edges of the muscle group prior to blunt dissection.
-
○
When possible, a muscle-splitting technique alongside and between the muscle fibers, without fibers transection, must be utilized and complemented by muscle retraction.
-
○
This technique may be combined with percutaneous screw placement with temporary bone reduction/holding, utilizing right-angled instrumentation.
-
○
If VATS is performed, subcutaneous insufflation of CO2 may help to expose muscles, partly substituting for a sharp dissection.
-
○
Step 5: Surgical Technique
The particular technique of a surgical approach varies and is guided by the location of the fracture. The general steps for surgical fixation listed under the lateral approach (outside of patient positioning, incision, and access to fractured ribs) are applicable to all other approaches.
-
Lateral approach.
-
○
The lateral incision is considered as the main approach because it allows access to the majority of rib fractures (i.e., anterolateral, lateral, and posterolateral) located from the mid-clavicular line to the vertebral border of the scapula.
-
○
The patient is positioned in a lateral decubitus position on a beanbag. If there are no lumbar or thoracic spine injuries, the operating room table is flexed to approximately 10° to 15°. The ipsilateral arm is draped and placed on a padded overhead arm-board at 90° of abduction and toward the head. We routinely include the ipsilateral arm in the sterilized surgical field. During the procedure, moving the ipsilateral arm helps to increase exposure by changing the scapular position. The contralateral arm is positioned on a padded horizontal arm-board with an axillary roll. It is important to leave enough space between the arm rest attachments in order to position the table-mounted retractor (Thompson, Omni-Flex [INTEGRA], etc.), which allows unobstructed and versatile tissue retraction and also obviates the need for an assistant.
-
○
Anatomical landmarks (e.g., inferior scapular angle, spinous processes) and the incision line are marked on the skin.
-
○
A lateral curvilinear skin incision is made overlying the fractured ribs. If needed, a “reversed lazy-S” extension of the incision will allow additional exposure of the posterior upper ribs and/or lower anterior ribs (Fig. 16, Video 2).
-
○
Dissection is carried through the subcutaneous tissue and subcutaneous flaps are developed so that the fascia continues encompassing the muscles, thus preserving the integrity as much as possible.
-
○
After a blunt dissection between muscles, the serratus anterior is retracted cephalad, the latissimus dorsi caudally, and the pectoralis major superiorly.
-
○
An iatrogenic injury of the long thoracic nerve (a pure motor nerve), which lies superficially on the serratus anterior muscle and descends alongside its outer border (in the projection of the mid-axillary line), should be avoided in order to prevent scapular winging25. Damage to the nerve may also be caused by the initial, direct thoracic trauma and by rib fractures. Neurological deficit must be documented prior to SSRF, but such damage may be difficult to detect because of the severity of trauma and the recumbency of the patient26. Posttraumatic winging of the scapula can also be a result of any disruption of the chain between the axial and appendicular skeleton, such as a sternoclavicular or acromioclavicular dislocation and clavicular or scapular fracture, which can be aggravated by ipsilateral upper rib fractures27.
-
○
Excisional debridement of all devitalized tissue, including subcutaneous fat, muscle, hematoma, and bone fragments, is performed and hemostasis is achieved. The wound is irrigated with warm saline solution.
-
○
Rib fractures are reduced with elevators, bone reduction graspers, a right-angled clamp, or a finger. The reduction of the most displaced rib fracture may help to reduce the adjacent rib fractures.
-
○
The periosteum must be preserved as much as possible to minimize the devascularization of the bone14. Plates can go on top of the periosteum and should be positioned over the thickest part of the rib, alongside the longitudinal axis.
-
○
The thickness of the ribs varies (most often 8 to 12 mm) and, in addition to the preoperative CT measurements, rib thickness is again verified by intraoperative measurement with a caliper on both sides of the fracture in order to choose the appropriate length of the screws. The selection of an appropriate screw length must take into account the thickness of the plate (approximately 1.5 to 2 mm). Rib thickness measurements on the CT scan are crucial near the spine and high under the scapula because these locations are not accessible by calipers. In cases in which the rib thickness is <8 mm, we add a polymer cable cerclage fixation.
-
○
-
Implant selection.
-
○
We currently prefer low-profile, precontoured rib and side-specific plates because they allow maximal apposition with a flush fit on the rib surface (MatrixRib; DePuy Synthes). The use of low-profile plates also helps to prevent tissue irritation and implant sensation, especially in skinny subjects. This is particularly important for the subscapular location in order to minimize pain from the contact between the scapula and the implant28. The length of rib plates varies because the plates can be cut to the desired span and medial/lateral orientation must be preserved.
-
○
Complex rib geometry with variable curvature (increased in the posterior rib segment) requires additional contouring of the plates to ensure plate apposition29. A flexible template is manually contoured over the reduced rib fractures at each respective rib. The contoured template is then imposed on precontoured titanium alloy plates and the plates are finally shaped to match the desired profile prior to attachment to the rib. Precontoured plates reduce bending attempts and preserve hole threads and plate integrity as a result of lessening metal fatigue. We also favor plates with threaded holes as they are more “forgiving” for appropriate screw placement, especially if a second attempt is needed, and also allow the use of locking screws. Locking screws have a separate thread under the screw head that matches the hole thread of the plate, thus allowing secure attachment of the screw to the plate, while the different thread on the screw stem provides purchase in the rib bone.
-
○
Care is taken to drill holes and place screws perpendicular to the rib surface. For perpendicular screw placements, the use of a drill guide is recommended. To position the screws perpendicularly in areas that are challenging to reach, a right-angled drill and screwdriver are used. A right-angled powered screwdriver and right-angled powered drill are preferred (DePuy Synthes) instead of manual ones (Fig. 17). To ensure robust fixation, the screws must lock to the plate and go through both cortical layers of the rib, as the inner rib cortex is thicker than the outer cortex29.
-
○
Principally, a minimum of 3 screws on each side of the reduced fracture are utilized to anchor the titanium plates, but >3 screws are preferred.
-
○
In addition to screw fixation of the plates onto the bone, in fragmented, osteoporotic bone and/or longitudinal or oblique rib fractures, polymer cable cerclage is utilized to enhance fixation of the plates to the ribs.
-
○
-
Posterior approach.
-
○
The posterior approach is recommended for posterior and subscapular rib fractures, and those occurring near the spine.
-
○
The patient is placed in a prone position with the ipsilateral arm lowered in abduction and toward the head.
-
○
For posterior and subscapular rib fractures, a vertical skin incision is performed within the triangle of auscultation. The triangle of auscultation is bounded medially and superiorly by the trapezius, laterally by the vertebral border of the scapula, and inferiorly by the latissimus dorsi. The floor of the triangle is formed by the rhomboid major and sixth and seventh ribs. Excessive damage to the rhomboid muscle may result in scapular winging.
-
○
We further develop this plane in a blunt fashion with use of finger dissection, starting from underneath the inferior angle of the scapula and extending cephalad by dissecting the scapulothoracic bursa.
-
○
Once the plane is developed, we use a scapular retractor. The erector spinae is retracted medially and elevated to expose the neck of the rib. With muscle retraction, exposure of the second to eighth ribs can be achieved (Figs. 6 and 18). Elevation of the erector spinae is important to allow enough space for the positioning of instrumentation and to place the contoured plate over the curved neck of the rib.
-
○
-
Anterior approach.
-
○
The anterior approach is recommended for anterior rib fractures (i.e., costochondral, sternocostal, and sternal).
-
○
Anterior rib fractures can be exposed with an oblique incision along the inframammary fold with the patient in the supine position30. A subpectoral plane is developed with minimal muscle division.
-
○
To reach high anterior fractures, right-angled tools are utilized, such as a right-angled powered drill and right-angled powered screwdriver.
-
○
Displaced fractures of the rib cartilage require sternal exposure to place screws through the sternal bone and costal part of the rib (Fig. 11).
-
○
For low anterior rib fractures, when intercostal cartilage is injured, we extend the incision to expose the sternum and the osseous part of the ribs and use long sternal plates to perform stabilization from the sternum over the cartilage to the rib bone (Fig. 19).
-
○
In addition to plates, we also add a cerclage fixation over a chondral injury in cases of cartilage repair. We always reduce the rib and sternal fracture first and the cartilage fracture last, and prefer to avoid placing screws through the cartilage.
-
○
Fracture of the second rib often requires a plate to be anchored medially to the sternum. For SSRF of the second rib, we use a separate, transverse incision just above the rib and extend it to the sternum in order to preserve the pectoralis major muscle by elevating the muscle from the sternal side, instead of dissecting through the pectoralis muscle.
-
○
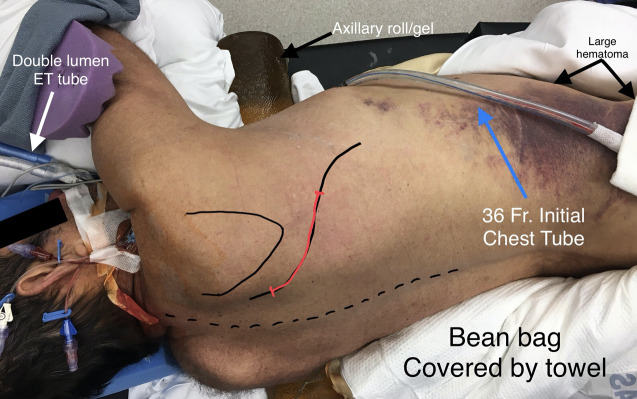
Fig. 16.
Photograph showing the patient positioned for the surgical procedure in a left decubitus position on a beanbag and axillary roll with the right arm in abduction. A double lumen endotracheal (ET) tube is seen. A lateral approach is marked as a curvilinear skin incision (red). If required, “lazy-S” extensions (black) may be added for access to the high-posterior and low-anterior rib fractures. Anatomical landmarks are noted (scapula and spinous processes). The operating table is flexed to 15°. An initial 36 French gauge chest tube (placed in the trauma bay) is to be removed before the incision and replaced with a new chest tube (in a new location) at the end of the procedure. The lateral abdominal hematoma does not indicate the epicenter of the rib fractures. The large hematoma includes the iliac crest area.
Fig. 17.
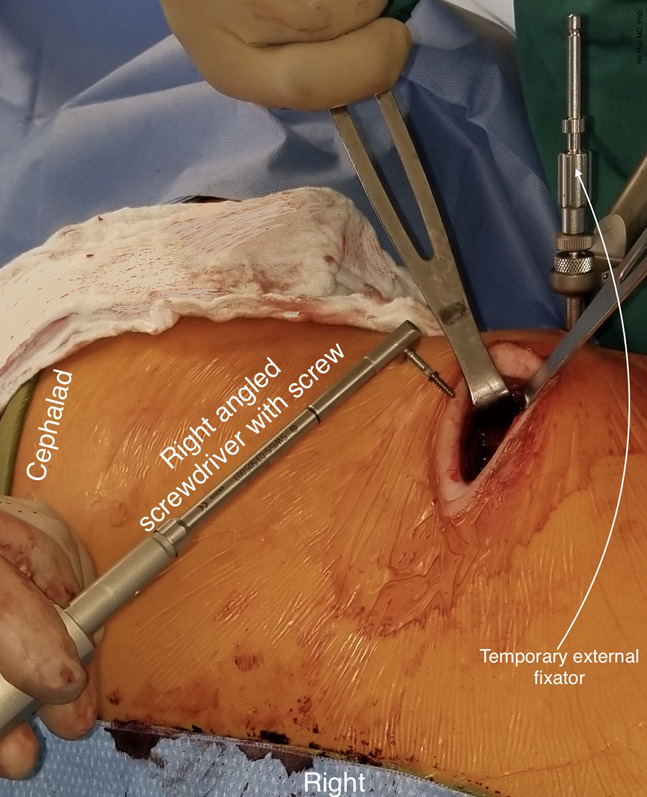
Intraoperative photograph made with the patient in a supine position showing external fixation temporarily holding the plate to the fractured rib. A locked screw is used with a right-angled screwdriver.
Fig. 18.
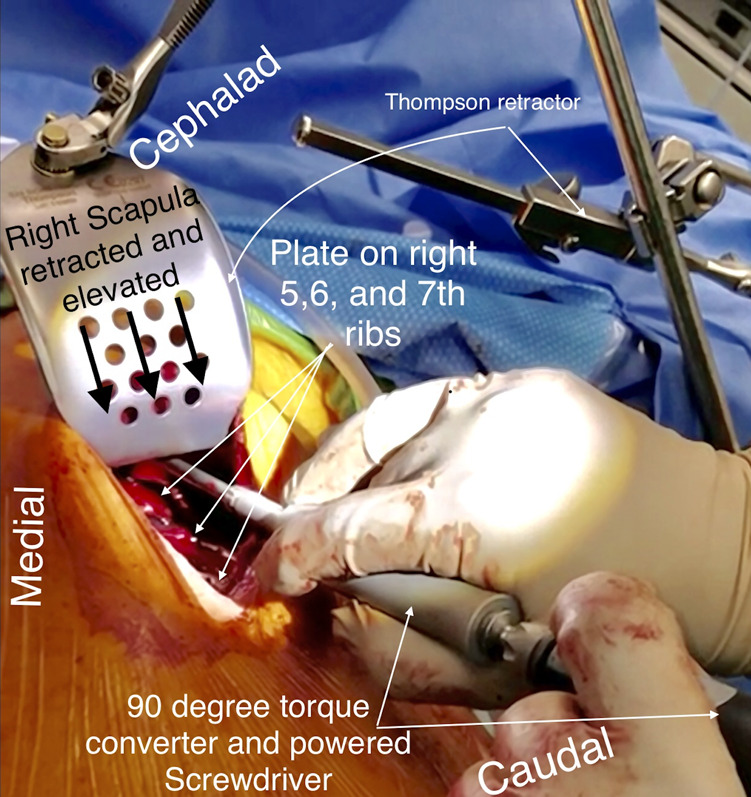
Intraoperative photograph showing the posterior subscapular approach. The right scapula is retracted and elevated, thus allowing placement of the screws on a plate stabilizing the third rib fracture using right-angled tools.
Fig. 19.
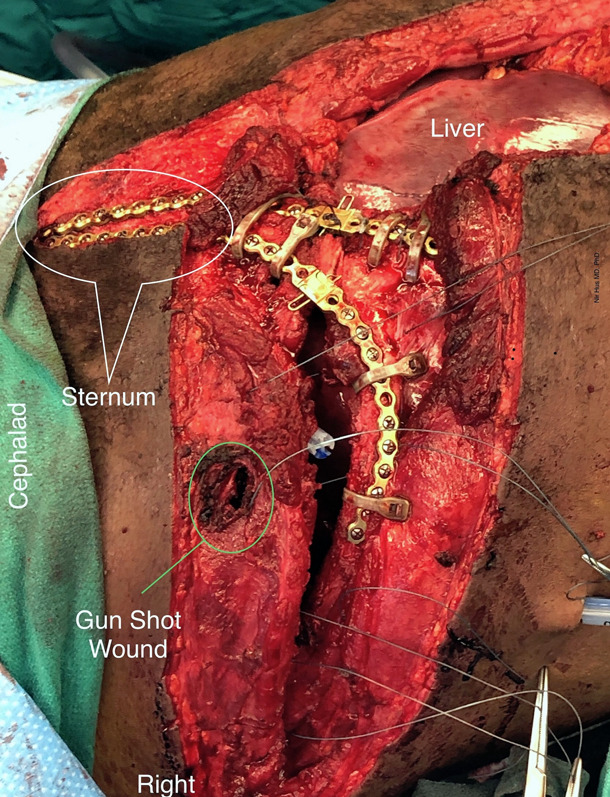
Intraoperative photograph of a patient with a right thoracoabdominal gunshot wound. Long sternal plates (30 holes) are contoured and anchored to the sternum and costal parts of the ribs spanning the fractured rib cartilage. Cerclage bands are enhancing rib fixation. The liver is exposed in the upper right corner.
Video 2.
Lateral approach and surgical stabilization of multiple rib fractures.
Step 6: Wound Closure and Postoperative Wound Care
Wound closure can be performed with use of staples or cosmetic sutures depending on the incision location, tissue condition, and cosmetic requirements.
If there was an initial chest tube, it is removed before an incision is made.
At the end of the procedure, a chest tube is placed outside of the incision and far from the implants. We prefer a single 28 French gauge (9.3-mm diameter) Blake drain for 48 to 72 hours.
We prefer to close the skin incision with staples.
We rarely place a vacuum drain between the muscle layers of the chest wall.
Results
Multiple rib fractures and unstable chest-wall injuries have high rates of morbidity and mortality.
Traditionally, the majority of these patients have been managed nonoperatively. With advances in the surgical technique and the growing utilization of SSRF, paralleled by improved outcomes, the indications for a surgical procedure are expanding from flail chest to multiple displaced rib fractures, and even include patients with pulmonary contusion15,16,31,32. It was reported that SSRF results in decreased length of hospital stay, increased critical care benefits, improved pulmonary function, and reduced rates of complications and mortality31,33. It was also suggested that the geriatric population (age ≥65 years) may benefit more from SSRF34. Previous studies have described different surgical approaches25,35,36; however, the availability of new technologies and advances in instrumentation present opportunities to improve surgical technique and expand SSRF to new patient populations.
In summary, the present article guides surgeons step by step through frequently encountered clinical scenarios. Key steps for SSRF include: CT imaging to choose the exact ribs for fixation, selection of optimal incision based on the fracture location, and selection of appropriate technique relevant to the type of fracture. The intended result of surgical fixation is to facilitate a complete recovery by reducing pain medication requirements and allowing the return to work and to preinjury quality of life.
Future directions for SSRF may include the following: (1) intrathoracic thoracoscopic minimally invasive plate osteosynthesis, (2) customization of plates using preoperative manufacturing of patient-specific contoured plates based on preoperative 3-dimensional printing37, (3) absorbable plates and screws, (4) low-profile, fatigue-free material plates (e.g., carbon fiber), and (5) fixation with a shape-memory alloy31.
Pitfalls & Challenges
Subcutaneous hematoma, especially in polytrauma patients, can be excessive and located outside of the epicenter of rib fractures, and therefore should not be relied on for the selection of the incision (Fig. 16).
Incorrect screw selection may result in the protrusion of screws that are too long beyond the inner cortex and consequently can cause lung parenchyma injury, especially when self-drilling screws are used (Fig. 20). Appropriate measurements during the surgical procedure and the selection of self-tapping screws will address this problem.
Plate breakage can occur, especially when complete apposition was not achieved during fracture reduction with the implant bridging the residual gap between segments. The major orthopaedic principle to reach the maximum apposition during fracture reduction must be upheld. Excessive contouring attempts, especially in the y axis (“smile”/“frown” face) and along the longitudinal axis (torqueing), should be avoided. Implant breakage and/or migration may require plate and/or screw removal and possible replacement in a symptomatic patient.
Detachment of the plate from the bone may occur as a result of stripping of the screw thread if the screw is not inserted perpendicular to the plate surface. That is why plates with threaded holes are preferred, as when using a nonthreaded plate and self-drilling screw, the surgeon has only 1 attempt to correctly place the screw (Fig. 21). Plate detachment may also happen when inadequate contouring of the plate occurs, which is why precontoured plates are preferred. This complication can be avoided by appropriate contouring of the plate before attachment, instead of forcing flush approximation just by screw insertion (Fig. 22).
Iatrogenic longitudinal rib fracture may occur when the bone is cracked during screw insertion. To avoid this, predrilling with the appropriate bit size and self-tapping screws must be used. A long plate supplemented with a polymer cerclage is recommended for treatment.f
Damage to the long thoracic nerve and excessive intraoperative trauma to rhomboid muscles may result in a winging scapula.
Excessive mobilization of the upper portions of the external oblique muscle during fixation of the lower ribs may result in hernia formation. Cryoablation of intercostal nerves below the tenth rib may also result in temporary bulging of the upper lateral abdominal wall.
Removal of the floating ribs or diaphragm plication may accidentally ensnare a branch of the phrenic nerve resulting in hiccups.
Nonunion of a plated fracture as a result of stabilization failure may also result in plate breakage.
Separation of the plate and/or screw from the rib may occur, especially in osteoporotic patients, in cases in which too-short plates were used and/or bicortical fixation was not achieved. If this complication occurs, a minimally invasive removal of the implant components in symptomatic patients can be performed under intraoperative CT imaging.
Fig. 20.
Diagram showing a long plate stabilizing a reduced segmental rib fracture (cross-sectional view). The plate is flush with the rib surface. The plate holes above the fracture lines are left empty. The first screw on the left is a self-drilling locking screw protruding too deep into the pleural cavity. The second screw from the left is a self-tapping locking screw that is inserted non-perpendicular to the rib surface with the screw head above the plate surface. The first screw on the right is too short and does not reach the inner cortex. The rest of the screws are flush with the plate surface and properly provide bicortical fixation.
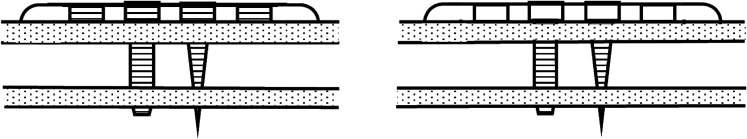
Fig. 21.
The left panel shows a threaded plate with a locking self-tapping screw (left), a locking self-drilling screw (right), and 2 empty plate holes on each side. The right panel shows a non-threaded plate with a self-tapping screw (left), a self-drilling screw (right), and 2 empty plate holes on each side.
Fig. 22.

Radiograph showing inappropriate plate shaping and inappropriate screw placement. The screw is not locked to the plate, resulting in plate migration and screw detachment.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJSEST/A293).
Published outcomes of this procedure can be found at: J Orthop Trauma. 2019 Jan;33(1):3-8.
Investigation performed at Delray Medical Center, Delray Beach, Florida
Disclosure: The authors indicated that no external funding was received for any aspect of this work. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJSEST/A292).
References
- 1.Lafferty PM, Anavian J, Will RE, Cole PA. Operative treatment of chest wall injuries: indications, technique, and outcomes. J Bone Joint Surg Am. 2011. January 5;93(1):97-110. [DOI] [PubMed] [Google Scholar]
- 2.de Moya M, Nirula R, Biffl W. Rib fixation: who, what, when? Trauma Surg Acute Care Open. 2017. April 27;2(1):e000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kane ED, Jeremitsky E, Pieracci FM, Majercik S, Doben AR. Quantifying and exploring the recent national increase in surgical stabilization of rib fractures. J Trauma Acute Care Surg. 2017. December;83(6):1047-52. [DOI] [PubMed] [Google Scholar]
- 4.Dehghan N, de Mestral C, McKee MD, Schemitsch EH, Nathens A. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg. 2014. February;76(2):462-8. [DOI] [PubMed] [Google Scholar]
- 5.Dehghan N, Mah JM, Schemitsch EH, Nauth A, Vicente M, McKee MD. Operative stabilization of flail chest injuries reduces mortality to that of stable chest wall injuries. J Orthop Trauma. 2018. January;32(1):15-21. [DOI] [PubMed] [Google Scholar]
- 6.Pieracci FM, Majercik S, Ali-Osman F, Ang D, Doben A, Edwards JG, French B, Gasparri M, Marasco S, Minshall C, Sarani B, Tisol W, VanBoerum DH, White TW. Consensus statement: Surgical stabilization of rib fractures rib fracture colloquium clinical practice guidelines. Injury. 2017. February;48(2):307-21. Epub 2016 Nov 27. [DOI] [PubMed] [Google Scholar]
- 7.Pieracci FM, Coleman J, Ali-Osman F, Mangram A, Majercik S, White TW, Jeremitsky E, Doben AR. A multicenter evaluation of the optimal timing of surgical stabilization of rib fractures. J Trauma Acute Care Surg. 2018. January;84(1):1-10. [DOI] [PubMed] [Google Scholar]
- 8.Su YH, Yang SM, Huang CH, Ko HJ. Early versus late surgical stabilization of severe rib fractures in patients with respiratory failure: A retrospective study. PLoS One. 2019. April 25;14(4):e0216170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Galvagno SM, Jr, Smith CE, Varon AJ, Hasenboehler EA, Sultan S, Shaefer G, To KB, Fox AD, Alley DE, Ditillo M, Joseph BA, Robinson BR, Haut ER. Pain management for blunt thoracic trauma: A joint practice management guideline from the Eastern Association for the Surgery of Trauma and Trauma Anesthesiology Society. J Trauma Acute Care Surg. 2016. November;81(5):936-51. [DOI] [PubMed] [Google Scholar]
- 10.Peek J, Beks RB, Kingma BF, Marsman M, Ruurda JP, Houwert RM, Leenen LPH, Hietbrink F, de Jong MB. Epidural analgesia for severe chest trauma: an analysis of current practice on the efficacy and safety. Crit Care Res Pract. 2019. March 19;2019:4837591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adhikary SD, Liu WM, Fuller E, Cruz-Eng H, Chin KJ. The effect of erector spinae plane block on respiratory and analgesic outcomes in multiple rib fractures: a retrospective cohort study. Anaesthesia. 2019. May;74(5):585-93. Epub 2019 Feb 10. [DOI] [PubMed] [Google Scholar]
- 12.Rose P, Ramlogan R, Madden S, Lui A. Serratus anterior plane block home catheter for posterior rib fractures and flail chest. Can J Anaesth. 2019. August;66(8):997-8. Epub 2019 May 7. [DOI] [PubMed] [Google Scholar]
- 13.Fowler TT, Taylor BC, Bellino MJ, Althausen PL. Surgical treatment of flail chest and rib fractures. J Am Acad Orthop Surg. 2014. Dec;22(12):751-60. [DOI] [PubMed] [Google Scholar]
- 14.Sarani B, Schulte L, Diaz JJ. Pitfalls associated with open reduction and internal fixation of fractured ribs. Injury. 2015. December;46(12):2335-40. Epub 2015 Oct 21. [DOI] [PubMed] [Google Scholar]
- 15.Pieracci FM, Lin Y, Rodil M, Synder M, Herbert B, Tran DK, Stoval RT, Johnson JL, Biffl WL, Barnett CC, Cothren-Burlew C, Fox C, Jurkovich GJ, Moore EE. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. J Trauma Acute Care Surg. 2016. February;80(2):187-94. [DOI] [PubMed] [Google Scholar]
- 16.Gerakopoulos E, Walker L, Melling D, Scott S, Scott S. Surgical management of multiple rib fractures reduces the hospital length of stay and the mortality rate in major trauma patients: a comparative study in a UK major trauma center. J Orthop Trauma. 2019. January;33(1):9-14. [DOI] [PubMed] [Google Scholar]
- 17.Ju T, Rivas L, Sarani B. Successful surgical stabilization of rib fractures despite Candida colonization of the mediastinum. Ann Thorac Surg. 2018. September;106(3):e121-3. Epub 2018 Apr 6. [DOI] [PubMed] [Google Scholar]
- 18.Okamoto K, Ueda K, Ichinose M. Cardiac injury due to the rapid progress of the dislocation of rib fractures: A rare case that required urgent open reduction and internal rib fixation. Respir Med Case Rep. 2019. April 16;27:100840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Graves C, Idowu O, Lee S, Padilla B, Kim S. Intraoperative cryoanalgesia for managing pain after the Nuss procedure. J Pediatr Surg. 2017. June;52(6):920-4. Epub 2017 Mar 16. [DOI] [PubMed] [Google Scholar]
- 20.Vossler JD, Zhao FZ. Intercostal nerve cryoablation for control of traumatic rib fracture pain: A case report. Trauma Case Rep. 2019. July 31;23:100229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stahl D, Ellington M, Brennan K, Brennan M. Association of ipsilateral rib fractures with displacement of midshaft clavicle fractures. J Orthop Trauma. 2017. April;31(4):225-8. [DOI] [PubMed] [Google Scholar]
- 22.Fokin A, Wycech J, Picard E, Weisz R, Puente I. Is first rib fracture a culprit or a sign of injury severity? It is both. J Orthop Trauma. 2018. August;32(8):391-6. [DOI] [PubMed] [Google Scholar]
- 23.Solberg BD, Moon CN, Nissim AA, Wilson MT, Margulies DR. Treatment of chest wall implosion injuries without thoracotomy: technique and clinical outcomes. J Trauma. 2009. July;67(1):8-13, discussion :13. [DOI] [PubMed] [Google Scholar]
- 24.Pennington MW, Roche AM, Bransford RJ, Zhang F, Dagal A. A technique to allow prone positioning in the spine surgery patient with unstable spine fracture and flail segment rib fractures. A A Case Rep. 2016. July 1;7(1):2-4. [DOI] [PubMed] [Google Scholar]
- 25.Taylor BC, French BG, Fowler TT. Surgical approaches for rib fracture fixation. J Orthop Trauma. 2013. July;27(7):e168-73. [DOI] [PubMed] [Google Scholar]
- 26.Skedros JG, Mears CS, Langston TD, Van Boerum DH, White TW. Medial scapular winging associated with rib fractures and plating corrected with pectoralis major transfer. Int J Surg Case Rep. 2014;5(10):750-3. Epub 2014 Aug 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rasyid HN, Nakajima T, Hamada K, Fukuda H. Winging of the scapula caused by disruption of “sternoclaviculoscapular linkage”: report of 2 cases. J Shoulder Elbow Surg. 2000. Mar-Apr;9(2):144-7. [PubMed] [Google Scholar]
- 28.Marasco S, Saxena P. Surgical rib fixation - technical aspects. Injury. 2015. May;46(5):929-32. Epub 2015 Jan 10. [DOI] [PubMed] [Google Scholar]
- 29.Bottlang M, Walleser S, Noll M, Honold S, Madey SM, Fitzpatrick D, Long WB. Biomechanical rationale and evaluation of an implant system for rib fracture fixation. Eur J Trauma Emerg Surg. 2010. October;36(5):417-26. Epub 2010 Sep 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.de Campos JRM, White TW. Chest wall stabilization in trauma patients: why, when, and how? J Thorac Dis. 2018. April;10(Suppl 8):S951-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jiang Y, Wang X, Teng L, Liu Y, Wang J, Zheng Z. Comparison of the effectiveness of surgical versus nonsurgical treatment for multiple rib fractures accompanied with pulmonary contusion. Ann Thorac Cardiovasc Surg. 2019. August 20;25(4):185-91. Epub 2019 May 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fokin AA, Wycech J, Weisz R, Puente I. Outcome Analysis of Surgical Stabilization of Rib Fractures in Trauma Patients. J Orthop Trauma. 2019. January;33(1):3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shibahashi K, Sugiyama K, Okura Y, Hamabe Y. Effect of surgical rib fixation for rib fracture on mortality: A multicenter, propensity score matching analysis. J Trauma Acute Care Surg. 2019. September;87(3):599-605. [DOI] [PubMed] [Google Scholar]
- 34.Kane ED, Jeremitsky E, Bittner KR, Kartiko S, Doben AR. Surgical stabilization of rib fractures: a single institution experience. J Am Coll Surg. 2018. June;226(6):961-6. Epub 2017 Nov 26. [DOI] [PubMed] [Google Scholar]
- 35.Hasenboehler EA, Bernard AC, Bottiggi AJ, Moghadamian ES, Wright RD, Chang PK, Boulanger BR, Kearney PA. Treatment of traumatic flail chest with muscular sparing open reduction and internal fixation: description of a surgical technique. J Trauma. 2011. August;71(2):494-501. [DOI] [PubMed] [Google Scholar]
- 36.Pieracci FM, Rodil M, Stovall RT, Johnson JL, Biffl WL, Mauffrey C, Moore EE, Jurkovich GJ. Surgical stabilization of severe rib fractures. J Trauma Acute Care Surg. 2015. April;78(4):883-7. [DOI] [PubMed] [Google Scholar]
- 37.Zhou X, Zhang D, Xie Z, Chen M, Yang Y, Liang Z, Zhang G. 3D printing and thoracoscopy assisted MIPO in treatment of long-range comminuted rib fractures, a case report. J Cardiothorac Surg. 2019. April 29;14(1):83. [DOI] [PMC free article] [PubMed] [Google Scholar]