Abstract
This retrospective study explored the efficacy and safety of dexmedetomidine in treating early postoperative cognitive dysfunction (EPPNCD) after video-assisted thoracoscopic lobectomy (VATL) in elderly male patients with lung cancer (LC).
This study included a total of 80 elderly male patients with LC who received VATL. All of them were equally assigned to a treatment group and a control group, with 40 patients each group. The primary outcome included cognitive dysfunction, as evaluated by mini-mental state examination scale. The secondary outcomes consisted of incidence of EPPNCD, lung function (as measured by forced vital capacity, forced expiratory volume in 1 second, peak expiratory flow, and maximal voluntary ventilation), and adverse events. All outcome data were analyzed before and 3 days after surgery.
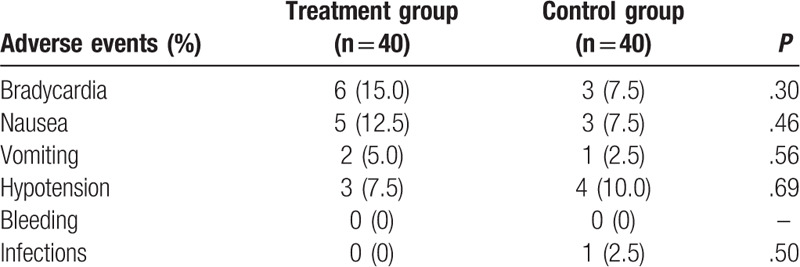
After surgery, all patients in the treatment group exerted better efficacy in mini-mental state examination scale (P < .01) and incidence of EPPNCD (P = .03), than patients in the control group. However, no significant differences were detected in forced vital capacity (P = .65), forced expiratory volume in 1 second (P = .50), peak expiratory flow (P = .73), and maximal voluntary ventilation (P = .27) between 2 groups. In addition, there is similar safety profile between 2 groups.
The findings of this study showed that dexmedetomidine may benefit EPPNCD after VATL in elderly male patients with LC. Future studies are needed to warrant the present conclusions.
Keywords: cognitive dysfunction, efficacy, lobectomy, safety
1. Introduction
Lung cancer (LC) is one of the most common cancers; and it is also the leading cause of cancer deaths worldwide.[1–4] Lobectomy, such as video-assisted thoracoscopic lobectomy (VATL), is considered as the gold standard intervention,[5–6] and it has become the preferred approach for patients with LC.[7–10] During the period of VATL, all patients received analgesia. However, most patients experience a variety of complications, such as bleeding, infections, postoperative pain and early postoperative cognitive dysfunction (EPPNCD).[11–14] Thus, it is very important to choose an effective analgesia with fewer complications, especially for EPPNCD.
Dexmedetomidine is a highly selective α2-adrenergic receptor agonist,[15,16] which is utilized as a short-term sedation and analgesia in several preoperative settings.[17–21] Studies suggested that it can benefit EPPNCD after VATL.[22–24] However, there is still limited data available regarding the efficacy and safety of dexmedetomidine on EPPNCD after VATL in elderly male patients with LC. Thus, this retrospective study investigated the efficacy and safety of dexmedetomidine on EPPNCD after VATL in elderly male patients with LC.
2. Patients and methods
2.1. Ethical approval
This study was approved by the ethics medical committee of The Affiliated Hospital of Inner Mongolia Medical University. All eligible patients provided written informed consent.
2.2. Design
This retrospective study included 80 elderly male patients with LC who received VATL from The Affiliated Hospital of Inner Mongolia Medical University between May 2017 and August 2019. All 80 eligible patients were assigned to a treatment group (n = 40) and a control group (n = 40), according to the different treatment schedules they received. All patients received same baseline anesthesia. In addition, all patients in the treatment group received dexmedetomidine, while the patients in the control group underwent 0.9% NaCl. No randomization procedure was applied to this study because it was conducted based on the completed patient records. In addition, no blind was placed to the outcome assessors. However, data analyst was blind in this study.
2.3. Patients
All eligible elderly male patients (over 60 years old) with LC after VATL were included in this study. In addition, all included patients should meet the following criteria: tumor diameter <5 cm, peripheral LC, and not close to large blood vessels. Patients were excluded if they had distant metastasis, sublobar resection, or cognitive dysfunction before surgery. In addition, patients were excluded if the surgery could not be completed successfully or received radiotherapy, or other medications for cognitive dysfunction, that may affect EPPNCD 1-month before the surgery. Furthermore, patients were excluded if they had history of chest surgery, single lung ventilation, and extensive pleural adhesions.
2.4. Treatment schedule
All patients were strictly required to fast and water before surgery, and were closely monitored changes in vital signs (including heart rate, blood pressure, pulse and blood oxygen saturation). Before induction of anesthesia, all patients in the treatment group received dexmedetomidine (Yangzijiang Pharmaceutical Group Co, Ltd, National Medicine Permit No. H20183220) with loading amount of 0.5 μg/kg for continuous 20 minutes. Then, the dose was adjusted to 0.2 μg/(kg.h) until 30 minutes before surgery finished. All patients in the control group administered 0.9% NaCl with the same procedure as the intervention group.
After continuous pumping in both groups, all patients were induced with 1 mg/kg propofol (Xi’an Libang Pharmaceutical Co, Ltd, National Medicine Permit No. H20163040), 0.5 μg/kg sufentanil (Yichang Renfu Pharmaceutical Co, Ltd, National Medicine Permit No. H20054172), and 0.2 mg/kg atracurium (Shanghai Pharmaceutical Dongying (Jiangsu) Pharmaceutical Co, Ltd Secretary, National Medicine Permit No. H20133373).
2.5. Outcome measurements
The primary outcome was cognitive dysfunction, as assessed by mini-mental state examination scale (MMSES).[25] It ranges from 0 to 30, the lower score, the severer cognitive dysfunction. It exerts in details as followings: scores of 24 to 30 shows no cognitive dysfunction; scores of 18 to 23 means mild cognitive dysfunction; and scores of 0 to 17 suggests severe cognitive dysfunction.
The secondary outcomes were incidence of EPPNCD, lung function (as measured by forced vital capacity (FVC, known as the volume of maximally forcefully exhaled air), forced expiratory volume in 1 second (FEV1, known as the best appraisal measurement of airway obstruction), peak expiratory flow [PEF, known as the maximum speed of expiration], and maximal voluntary ventilation [MVV, known as the maximum breathing capacity]),[26,27] and adverse events. All outcomes were measured before and 3 days after surgery.
2.6. Statistical analysis
All data were analyzed using SAS package (Version 9.1; SAS Institute Inc, Cary, NC). All continuous data was analyzed by t test or Wilcoxon test, and all discontinuous data was analyzed by Pearson chi-square test or Fisher exact test. We defined P < .05 as having statistical significance.
Although several studies have investigated the efficacy of dexmedetomidine for EPPNCD, no study has specifically appraised its efficacy and safety for EPPNCD after VATL in elderly male patients with LC. Thus, no closely relevant study was previously published that help to calculate sample size of this study. Taking into account the minimum number of patients necessary to assess the efficacy of dexmedetomidine for EPPNCD after VATL in elderly male patients with LC, this retrospective study included 80 patients (40 in each group) with an expected dropout rate of 20%.[28]
3. Results
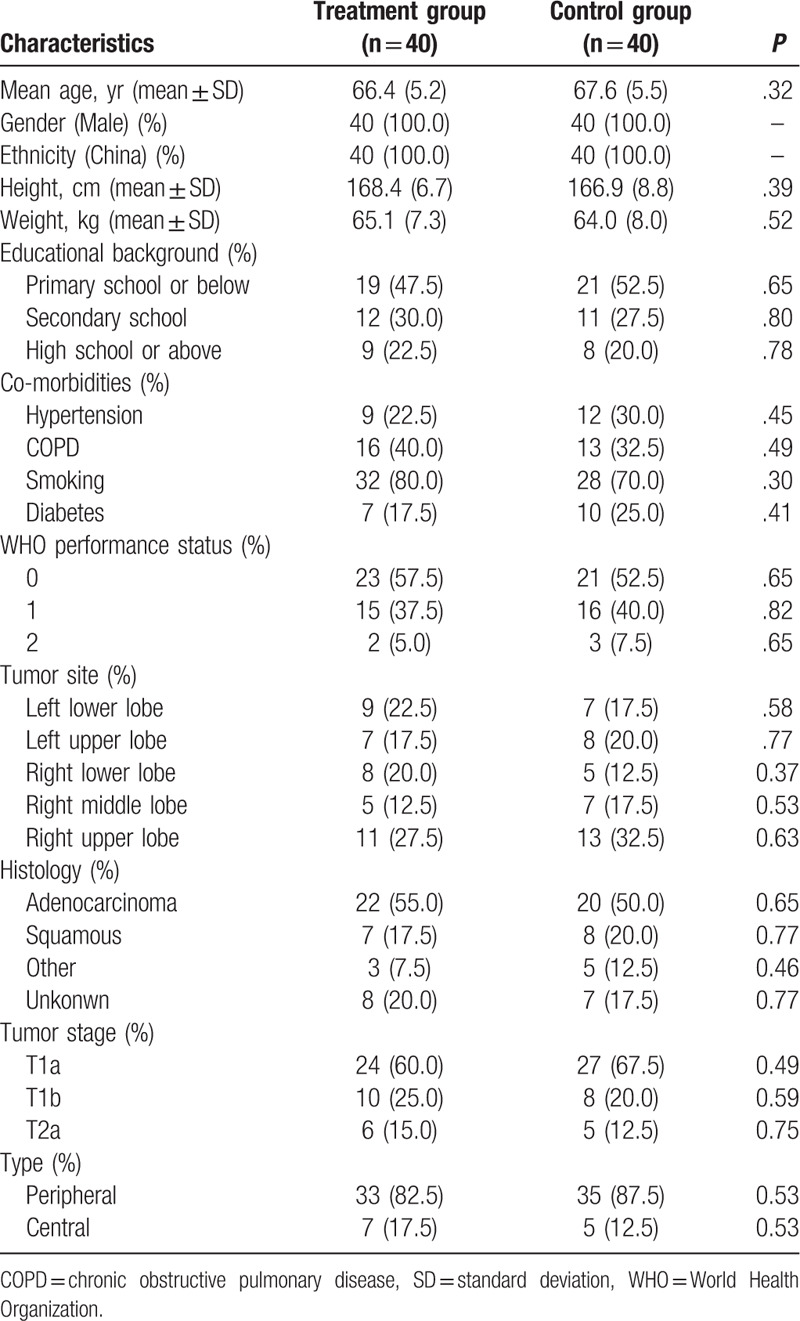
We summarized characteristic information of all included patients in both groups (Table 1). There were not significant differences regarding all baseline characteristic values between 2 groups.
Table 1.
Comparison of baseline characteristics between 2 groups.
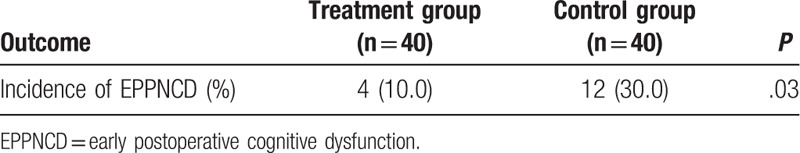
The results of this study demonstrated that patients in the treatment group showed better efficacy in cognitive dysfunction by MMSES (P < .01, Table 2), and incidence of EPPNCD (P = .03, Table 3), than those of patients in the control group.
Table 2.
Comparison of cognitive dysfunction before and 3 days after surgery between 2 groups.
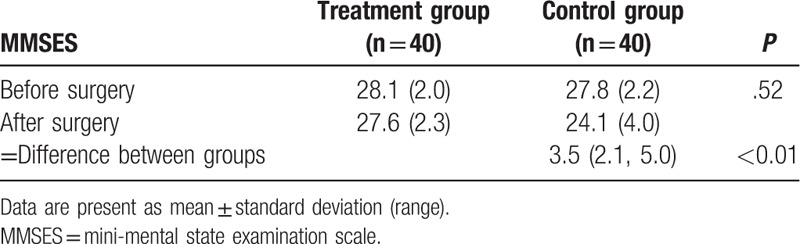
Table 3.
Comparison of incidence of EPPNCD 3 days after surgery between 2 groups.
On the other hand, patients in the treatment group did not exert greater improvement in lung function by FVC (P = .65, Table 4), FEV1 (P = .50, Table 5), PEF (P = .73, Table 6), and MVV (P = .27, Table 7), than those of patients in the control group. Moreover, although several adverse events were documented in both groups, no significant differences of them were detected between 2 groups (Table 8).
Table 4.
Comparison of FVC before and 3 days after surgery between 2 groups.
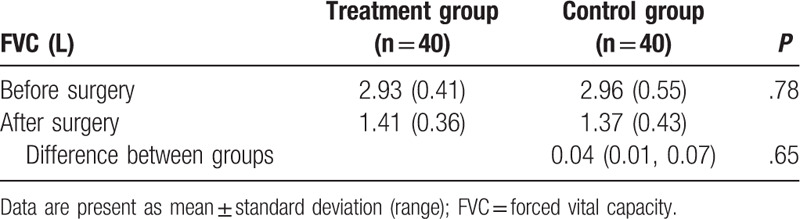
Table 5.
Comparison of FEV1 before and 3 days after surgery between 2 groups.
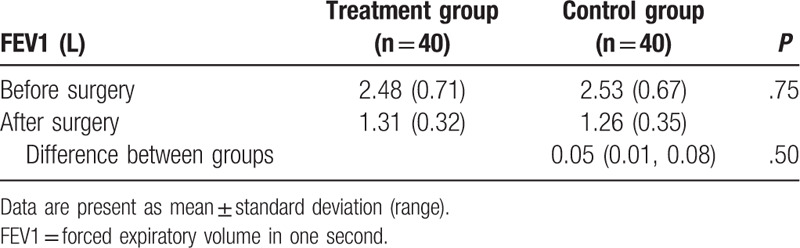
Table 6.
Comparison of PEF before and 3 days after surgery between 2 groups.
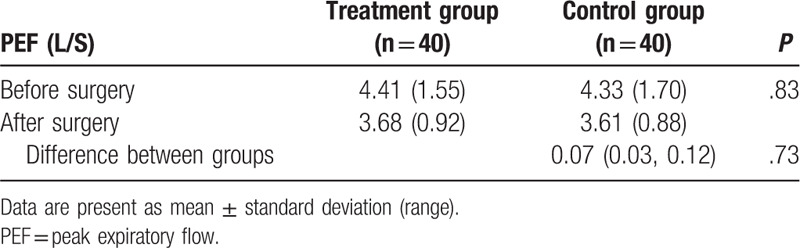
Table 7.
Comparison of MVV PEF before and 3 days after surgery between 2 groups.

Table 8.
Comparison of adverse events between 2 groups.
4. Discussion
LC is a very common cancer among the general population.[1,2] Although a variety of treatments are available to treat LC, their efficacy is still not satisfied. Surgery is considered as a common and effective approach for LC, especially for VATL.[7–10] Dexmedetomidine is commonly used as analgesia during the procedures of VATL. However, a lot of patients with LC who underwent VATL and dexmedetomidine experienced many complications, such as EPPNCD.[17–24] In addition, few data are available regarding the dexmedetomidine on EPPNCD after VATL in elderly male patients with LC.
This retrospective study investigated the efficacy and safety of dexmedetomidine on EPPNCD after VATL in elderly male patients with LC. In the present study, our findings found that patients in the treatment group showed more promising efficacy in EPPNCD, as measured by MMSES and incidence of EPPNCD, than patients in the control group. It indicates that dexmedetomidine may benefit EPPNCD after VATL in elderly male patients with LC.
On the other hand, patients in the treatment group did not show exciting outcome results in lung function, as assessed by FVC, FEV1, PEF, and MVV, when compared with patients in the control group. It suggests that dexmedetomidine is not superior to other analgesic drugs in lung function improvement. In addition, both groups showed similar safety profile.
Several limitations existed in this study. First, limited sample size of this study may affect our findings. Second, no randomization procedure was utilized to assign patients in this study, because we only analyzed data from existed patient records. Third, all patients, researchers and outcome assessors were not blind in this study. Fourth, all case records were collected from The Affiliated Hospital of Inner Mongolia Medical University, which may affect its generalization to other hospitals. Fifth, this study only assessed outcomes before and 3 days after surgery. Thus, data and following up assessment at other time points still need to be explored in the future.
5. Conclusion
The findings of this study showed that dexmedetomidine may benefit EPPNCD after VATL in elderly male patients with LC. However, further studies are still needed to warrant the current conclusion.
Author contributions
Conceptualization: Hai-Xia Shi, Fan Wu, Ya-Juan Hu, Wei-Dong Mi.
Data curation: Hai-Xia Shi, Xue-Jiang Du, Fan Wu.
Formal analysis: Hai-Xia Shi, Xue-Jiang Du, Ya-Juan Hu, Wei-Dong Mi.
Investigation: Wei-Dong Mi.
Methodology: Hai-Xia Shi, Xue-Jiang Du, Fan Wu, Ya-Juan Hu.
Project administration: Wei-Dong Mi.
Resources: Hai-Xia Shi, Xue-Jiang Du, Fan Wu, Ya-Juan Hu.
Software: Hai-Xia Shi, Xue-Jiang Du, Fan Wu, Ya-Juan Hu.
Supervision: Wei-Dong Mi.
Validation: Hai-Xia Shi, Xue-Jiang Du, Fan Wu, Ya-Juan Hu, Wei-Dong Mi.
Visualization: Hai-Xia Shi, Xue-Jiang Du, Wei-Dong Mi.
Writing – original draft: Hai-Xia Shi, Xue-Jiang Du, Fan Wu, Ya-Juan Hu, Wei-Dong Mi.
Writing – review & editing: Hai-Xia Shi, Fan Wu, Wei-Dong Mi.
Footnotes
Abbreviations: EPPNCD = early postoperative neurocognitive dysfunction, FEV1 = forced expiratory volume in one second, FVC = forced vital capacity, LC = lung cancer, MMSES = mini-mental state examination scale, MVV = maximal voluntary ventilation, PEF = peak expiratory flow, VATL = video-assisted thoracoscopic lobectomy.
How to cite this article: Shi HX, Du XJ, Wu F, Hu YJ, Mi WD. Dexmedetomidine for early postoperative cognitive dysfunction after video-assisted thoracoscopic lobectomy in elderly male patients with lung cancer. Medicine. 2020;99:36(e21691).
The authors report no conflicts of interest.
The datasets generated during and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Funded by Inner Mongolia Natural Science Foundation (No. 2017MS08107) and Inner Mongolia Health and Family Planning Research Project (No. 201703096). Applicant: Hai-xia Shi.
References
- [1].Nasim F, Sabath BF, Eapen GA. Lung cancer. Med Clin North Am 2019;103:463–73.. [DOI] [PubMed] [Google Scholar]
- [2].Dlamini SB, Sartorius B, Ginindza T. Mapping the evidence on interventions to raise awareness on lung cancer in resource poor settings: a scoping review protocol. Syst Rev 2019;8:217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Lewis R, Hendry M, Din N, et al. Pragmatic methods for reviewing exceptionally large bodies of evidence: systematic mapping review and overview of systematic reviews using lung cancer survival as an exemplar. Syst Rev 2019;8:171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Cao M, Chen W. Epidemiology of lung cancer in China. Thorac Cancer 2019;10:3–7.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Demmy TL, Yendamuri S, D’Amico TA, et al. Oncologic equivalence of minimally invasive lobectomy: the scientific and practical arguments. Ann Thorac Surg 2018;106:609–17.. [DOI] [PubMed] [Google Scholar]
- [6].Liu B, Flores RM, Taioli E. Patterns of elective lobectomy for lung cancer. J Surg Res 2017;220:59–67.. [DOI] [PubMed] [Google Scholar]
- [7].Berfield KS, Farjah F, Mulligan MS. Video-assisted thoracoscopic lobectomy for lung cancer. Ann Thorac Surg 2019;107:603–9.. [DOI] [PubMed] [Google Scholar]
- [8].Lex JR, Naidu B. In patients with resectable non-small-cell lung cancer, is video-assisted thoracoscopic segmentectomy an appropriate alternative to video-assisted thoracoscopic lobectomy? Interact Cardiovasc Thorac Surg 2016;23:826–31.. [DOI] [PubMed] [Google Scholar]
- [9].Harris CG, James RS, Tian DH, et al. Systematic review and meta-analysis of uniportal versus multiportal video-assisted thoracoscopic lobectomy for lung cancer. Ann Cardiothorac Surg 2016;5:76–84.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Gonzalez-Rivas D, Delgado M, Fieira E, et al. Double sleeve uniportal video-assisted thoracoscopic lobectomy for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Okyere S, Attia R, Toufektzian L, et al. Is the learning curve for video-assisted thoracoscopic lobectomy affected by prior experience in open lobectomy? Interact Cardiovasc Thorac Surg 2015;21:108–12.. [DOI] [PubMed] [Google Scholar]
- [12].Perna V, Carvajal AF, Torrecilla JA, et al. Uniportal video-assisted thoracoscopic lobectomy versus other video-assisted thoracoscopic lobectomy techniques: a randomized study. Eur J Cardiothorac Surg 2016;50:411–5.. [DOI] [PubMed] [Google Scholar]
- [13].Wu CF, Paradela M, Wu CY, et al. Novice training: the time course for developing competence in single port video-assisted thoracoscopic lobectomy. Medicine (Baltimore) 2020;99:e19459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Agostini P, Lugg ST, Adams K, et al. Video-assisted thoracoscopic lobectomy: which patients require postoperative physiotherapy? Physiotherapy 2020;106:87–93.. [DOI] [PubMed] [Google Scholar]
- [15].Kulikov AS, Lubnin AY. Dexmedetomidine: new opportunities in anesthesiology. Anesteziol Reanimatol 2013;1:37–41.. [PubMed] [Google Scholar]
- [16].Gerresheim G, Schwemmer U. Dexmedetomidine. Anaesthesist 2013;62:661–74.. [DOI] [PubMed] [Google Scholar]
- [17].Keating GM. Dexmedetomidine: a review of its use for sedation in the intensive care setting. Drugs 2015;75:1119–30.. [DOI] [PubMed] [Google Scholar]
- [18].Sottas CE, Anderson BJ. Dexmedetomidine: the new all-in-one drug in paediatric anaesthesia? Curr Opin Anaesthesiol 2017;30:441–51.. [DOI] [PubMed] [Google Scholar]
- [19].Castillo RL, Ibacache M, Cortínez I, et al. Dexmedetomidine improves cardiovascular and ventilatory outcomes in critically Ill patients: basic and clinical approaches. Front Pharmacol 2020;10:1641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wang K, Wang LJ, Yang TJ, et al. Dexmedetomidine combined with local anesthetics in thoracic paravertebral block: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 2018;97:e13164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Lin N, Vutskits L, Bebawy JF, et al. Perspectives on dexmedetomidine use for neurosurgical patients. J Neurosurg Anesthesiol 2019;31:366–77.. [DOI] [PubMed] [Google Scholar]
- [22].Carr ZJ, Cios TJ, Potter KF, et al. Does dexmedetomidine ameliorate postoperative cognitive dysfunction? A brief review of the recent literature. Curr Neurol Neurosci Rep 2018;18:64. [DOI] [PubMed] [Google Scholar]
- [23].Du X, Song F, Zhang X, et al. Protective efficacy of combined use of parecoxib and dexmedetomidine on postoperative hyperalgesia and early cognitive dysfunction after laparoscopic cholecystectomy for elderly patients. Acta Cir Bras 2019;34:e201900905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Li WX, Luo RY, Chen C, et al. Effects of propofol, dexmedetomidine, and midazolam on postoperative cognitive dysfunction in elderly patients: a randomized controlled preliminary trial. Chin Med J (Engl) 2019;132:437–45.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Li H, Jia J, Yang Z. Mini-mental state examination in elderly Chinese: a population-based normative study. J Alzheimers Dis 2016;53:487–96.. [DOI] [PubMed] [Google Scholar]
- [26].Gao CL, Zhang X, Wang D, et al. Reference values for lung function screening in 10- To 81-year-old, healthy, never-smoking residents of Southeast China. Medicine (Baltimore) 2018;97:e11904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Zhang Y, Gao Y. Effects of VATS lobectomy, VATS anatomic segmentectomy, and open thoracotomy on pulmonary function of patients with non-small cell lung cancer. Zhongguo Fei Ai Za Zhi 2016;19:700–4.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Johanson GA, Brooks GP. Initial scale development: sample size for pilot studies. Educ Psychol Meas 2010;70:394–400.. [Google Scholar]


