Abstract
Nasal high flow (NHF) has gained popularity among intensivists to manage patients with acute respiratory failure. An important literature has accompanied this evolution. In this review, an international panel of experts assessed potential benefits of NHF in different areas of acute respiratory failure management. Analyses of the physiological effects of NHF indicate flow-dependent improvement in various respiratory function parameters. These beneficial effects allow some patients with severe acute hypoxemic respiratory failure to avoid intubation and improve their outcome. They require close monitoring to not delay intubation. Such a delay may worsen outcome. The ROX index may help clinicians decide when to intubate. In immunocompromised patients, NHF reduces the need for intubation but does not impact mortality. Beneficial physiological effects of NHF have also been reported in patients with chronic respiratory failure, suggesting a possible indication in acute hypercapnic respiratory failure. When intubation is required, NHF can be used to pre-oxygenate patients either alone or in combination with non-invasive ventilation (NIV). Similarly, NHF reduces reintubation alone in low-risk patients and in combination with NIV in high-risk patients. NHF may be used in the emergency department in patients who would not be offered intubation and can be better tolerated than NIV.
Electronic supplementary material
The online version of this article (10.1007/s00134-020-06228-7) contains supplementary material, which is available to authorized users.
Keywords: Acute respiratory failure, ARDS, Intubation, High flow oxygen, Nasal canula, Palliative care
Take-home message
| In every segment of acute hypoxemic respiratory failure management (first-line ventilatory support, preoxygenation, post-extubation, palliative care), evidence suggests that nasal high flow has the potential to benefit the patient. Beneficial effects also seem to be seen in patients with chronic respiratory disease. |
Introduction
In the past years, nasal high flow has gained an important popularity among intensivists to manage patients with acute respiratory failure, filling a gap in the ventilatory support escalation between facemask oxygen and noninvasive or invasive mechanical ventilation. Interestingly, use of NHF was widely and rapidly adopted in ICUs before in-depth knowledge of its physiological effects and evidence of its efficacy were published. Since, a great amount of literature has been published and indications other than acute respiratory failure have emerged. In this narrative review, we have aimed to summarize the available data and address the different clinical scenarios in which NHF can be used, highlighting areas where further research is required to confirm or not the potential for NHF to improve patient outcome.
Nasal High Flow (NHF) in acute hypoxemic respiratory failure (AHRF)
Physiological effects of NHF
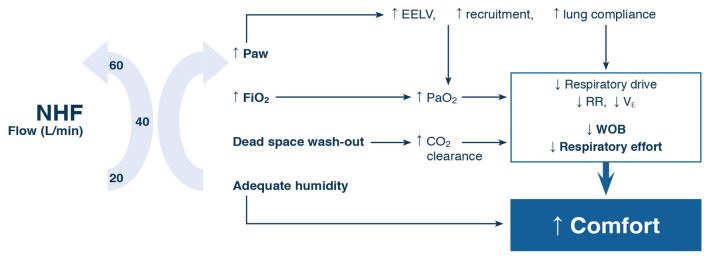
A unique feature of NHF is its ability to comfortably deliver high flows of warmed humidified gas, 20–70 L/min, with a FiO2 range of 0.21–1.0. Physiological responses to NHF therapy include increases in airway pressure, end-expiratory lung volume (EELV), and oxygenation which are probably optimal with higher flows (60–70 L/min), while the effects on dead-space washout, work of breathing, and respiratory rate may be obtained with intermediate flows (20–45 L/min) [1–3] (Fig. 1). Most of this evidence relates to patients with hypoxemic respiratory failure and, to date, few physiological data have been obtained in hypercapnic populations [4].
Fig. 1.
Schematic representation of the physiologic effects of Nasal High Flow (NHF) and possible impact of the flow. Increase in airway pressure and FiO2 improve oxygenation by different mechanisms and may be optimal at higher flows. Most of dead-space wash-out-related effects (increased CO2 clearance, decrease respiratory drive, respiratory rate and effort to breathe) may be obtained for lower flows. All these physiological effects probably explain the improved comfort in patients with respiratory failure and possibly the outcomes. NHF nasal high flow, Paw airway pressure; FiO2 fraction of inspired oxygen, EELV end-expiratory lung volume, RR respiratory rate, VE minute volume, WOB work of breathing
As NHF rate increases, so does EELV [2] (ESM Fig. 1). This relationship is linear with each litre of increased flow resulting in 0.7% increase in EELV [5]. A strong correlation exists between increases in airway pressure and EELV (r = 0.7) [5], suggesting that this mechanism is responsible for the improvements in oxygenation seen with NHF, particularly at higher flows [2], through alveolar recruitment (ESM Fig. 2).
Inspiratory effort decreases with increasing flow rates, and Mauri et al. [2] suggest it is best supported by flows of 60 L/min. However these, and other authors, also recognised that important reductions in work of breathing can still be achieved with lower rates of 20–45 L/min [1, 2] (ESM Fig. 3). As flow increases, respiratory rate decreases [2, 4], along with minute ventilation [2, 4], without any resultant hypercapnia. In other words, alveolar ventilation (minute ventilation − dead-space ventilation) remains stable whereas minute ventilation decreases. The main mechanism to explain the stability in PaCO2 is the washout of physiological dead space.
Importantly, higher flows are well tolerated by hypoxemic patients, whose comfort was not adversely affected by higher gas flows [6].
As NHF is used for respiratory support in a wide range of conditions, clinicians should titrate flow to patient’s response to therapy. ESM Table 1 provides some guidance on achieving optimal flow rates for patients with hypoxemic respiratory failure. If tolerated, the highest flow as a starting point seems optimal in patients with hypoxemic respiratory failure, while lower flows may be efficient to reduce the respiratory rate and work of breathing, especially in hypercapnic patients (see dedicated section).
Avoidance of intubation
Since the introduction of NHF in the armamentarium of respiratory failure management, a number of observational studies have shown that respiratory status of patients with AHRF is significantly improved with NHF in comparison with standard oxygen [7–11]. Although they suggested that intubation may have been avoided in some patients, design of these studies precluded any formal demonstration of intubation rate reduction with NHF. The characteristics of NHF and the related physiological effects account for the superiority of NHF in terms of comfort, tolerance, alleviation of respiratory distress and improved oxygenation. The Florali study [12] showed in a post hoc subgroup (patients with a PaO2/FiO2 < 200) analysis that intubation rate was lower in patients treated with NHF compared to those treated with NIV or standard oxygen. This clinically relevant difference translated into a reduction in hospital and 90-day mortality rate in favour of patients that received NHF as first-line therapy. Several meta-analysis [13], but not all [14], also found that use of NHF was associated with a reduction in intubation rate. A concern with some is the inclusion of studies assessing patients with very different intubation risks and required information size was not reached [14]. Intubation rates in patients with AHRF admitted to the ICU range between 30 and 40%. These figures are only 1–2% in the ED as those needing immediate intubation or NIV for AHRF were excluded. Thus, the choice of primary outcome selected in certain settings may not have been the most relevant. In the ED, three of five RCT of NHF compared to conventional oxygen therapy reported intubation rates, with no studies finding a difference between the groups [15–17]. A meta-analysis of the studies with either undifferentiated respiratory distress [15, 17, 18] or cardiogenic pulmonary oedema [16] found only 7/571 patients required intubation (1.2%), with no difference in intubation rates: RR 0.69 (0.12, 4.12), p = 0.68 [19]. A single RCT comparing NHF to NIV for undifferentiated respiratory failure found that NHF was non-inferior to NIV for intubation rates [20]. It, therefore, appears that contrary to the ICU, delayed intubation is a rare event in the ED, so much larger studies would be required to demonstrate any benefit with respect to avoiding intubation.
Severe AHRF
In patients with AHRF, NHF is usually initiated in case of persistence of hypoxemia and/or respiratory distress despite conventional oxygen therapy. Hence, levels of hypoxemia of these patients vary considerably, from mild- to-moderate to severe hypoxemia (PaO2/FiO2 < 200). Although a noticeable proportion of them is successfully treated with NHF, the lower boundary in terms of PaO2/FiO2 has not been established.
In the Florali study [12], among the 80% of patients with a PaO2/FiO2 below 200, this ratio was in the range of 120 and many had bilateral chest X-ray involvement. They would have probably qualified as ARDS patients. They clearly presented the clinical, radiographical and biological features of ARDS. It has indeed been convincingly shown by Garcia-de-Acilu et al. that hypoxemic patients with bilateral infiltrates treated with NHF present the same levels of plasma biomarkers of epithelial and endothelial injury and biomarkers of inflammation as ARDS patients who undergo mechanical ventilation [21]. Importantly, half of these patients treated with NHF did not require intubation. Similar findings were reported by Messika et al. In their cohort of 45 patients treated with NHF, all of whom met all the Berlin criteria other than PEEP, success rate was 60%. Of note, worst recorded PaO2/FiO2 for the cohort was 108.6 and number of quadrants involved in the chest X-ray was 3 [7].
Hence, in the absence of criteria for immediate intubation, patients presenting with ARDS can be offered a NHF trial. Those with a low PaO2/FiO2 (< 100) will be at greater risk of intubation. Hence, a close monitoring will be required to anticipate when intubation needs to be performed in a timely fashion. (see below for the preoxygenation strategy in such patients).
Anticipating outcome with NHF
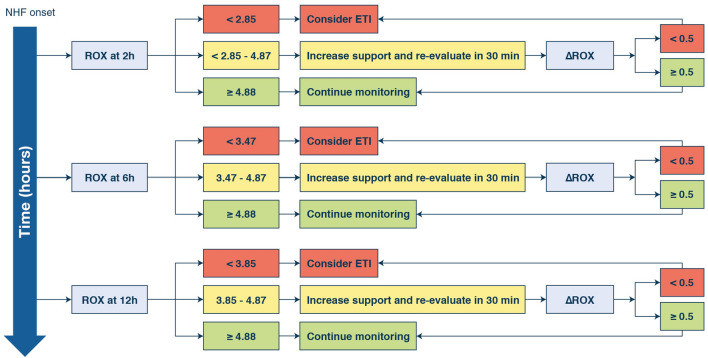
This close monitoring mentioned above should include several variables (oxygenation, thoracoabdominal asynchrony, need for vasopressors, SOFA score or disease severity) that have been shown to be associated with NHF failure [7, 9–11]. This association is not, however, directly predictive of the outcome of NHF. More recently, the ROX index, defined as the ratio of SpO2/FiO2 over RR, has been described and prospectively validated to predict success and failure of NHF in pneumonia patients with AHRF [22, 23]. The rationale behind this index is that it combines in a single value, the best describers of patients’ respiratory status. Patients with a ROX index greater than or equal to 4.88 after 2, 6 and 12 h of NHF therapy were less likely to be intubated. In contrast, patients with a ROX index below 2.85, 3.47 and 3.85 after 2, 6 and 12 h of HFNC therapy, respectively, were more likely to fail. In addition, patients who failed presented a smaller increase in the ROX index between 2 and 12 h and 6 and 12 h, which highlights the fact that dynamic assessment of the ROX index may also be helpful to identify those patients who are more likely to fail. This dynamic assessment could be especially useful in classifying those patients who have ROX index values between the boundaries of failure and success facilitating the day-to-day clinical decision process of NHF patients and minimizing the risk of delaying a needed intubation (see Fig. 2 and ESM for detail). Of note however, the ROX was validated in patients with pneumonia-related AHRF. Although severe pneumonia is the most frequent cause of AHRF, to what extent the same cut-offs values for the ROX will have the same performances in other etiologies of AHRF remains to be shown.
Fig. 2.
Suggested algorithm using the ROX index to help with intubation decision. Because the index includes in a single value three relevant respiratory parameters, the overall philosophy of the index is that if its value is increasing, the patient’s respiratory status is improving. For each time-point, there are three possibilities: (1) the patient’s ROX index is below the cut-off value, we suggest considering intubation of the patient; (2) the index is between the lower and the higher cut-off value, we suggest increasing the level of NHF (increase flow to its maximum and FiO2 to 1) and re-evaluate after 30 min; (3) finally, if the index is above the upper boundary, we suggest pursuing NHF and close monitoring of the patient. Of note, this algorithm will require a formal validation by a RCT comparing standard of care and application of the algorithm in terms of safety and efficacy (timing of intubation)
Hazards associated with NHF
As mentioned earlier, between 30 and 40% of patients with AHRF initially treated with NHF will require invasive mechanical ventilation finally. Hence, the principal hazard associated with NHF is the delay in intubating these patients in which NHF is insufficient. One study has shown that delayed intubation is associated with increased mortality in patients with community-acquired pneumonia. This observation was initially made in patients with AHRF receiving NIV [24] and has been shown to occur also in patients treated with NHF. Rello et al. found that patients who failed NHF in H1N1 pneumonia-related ARDS had a 27% mortality rate whereas this figure was 20% in those immediately intubated, suggesting that in some instances at least, a delay in intubation might be detrimental [10]. Kang et al. further explored this hazard. They found very different mortality rates in patients treated with NHF between those intubated within 48 h of therapy and those intubated after. This landmark study clearly illustrated the risk of a delayed intubation [25]. Several reasons may explain these findings. Leaving a patient breathe spontaneously for too long may worsen the nature and the extent of the initial injury, a concept termed patient self-inflicted lung injury. In addition, oxygen supplementation through NHF may rapidly normalize oxygen saturation leading to the misjudgment that the patient is improving whereas in fact, the underlying disturbances (such as ventilation perfusion mismatch or alveolar hypoventilation requiring inspiratory pressure support and positive-end expiratory pressure) are insufficiently corrected [26]. Patients may hence gradually and “silently” deteriorate to the point of respiratory muscle fatigue, cardiac dysfunction, and organ failure, thus contributing to a worse prognosis. Hence, close monitoring as described above of patients under NHF is mandatory to enable early detection of clinical deterioration, and thereby prevent evitable delay in intubation.
NHF in immunocompromised patients
In the past years, several studies have assessed non-invasive management of AHRF in immunocompromised patients (ESM Table 2). Most of them were retrospective. Comparators (NIV or standard oxygen or NIV + NHF), primary endpoint (intubation or mortality) as well as type of immunosuppression differed between studies, making direct comparisons difficult [9, 27–33]. Nonetheless, taken together, these studies suggested that NHF might reduce intubation rate, particularly when compared to NIV. They also showed that use of HNFC was possibly associated with a lower mortality rate and was not harmful.
Those results were confirmed in an international multicentre observational cohort study [34] in which patients admitted to ICU who received either NHF, NIV, standard oxygen or NHF + NIV were analysed. Intubation rate was similar for each oxygenation strategy. However, the multivariate analysis indicated a trend towards lower intubation rate with NHF.
These observational data required a prospective multicentre RCT to confirm the trends their results suggested. Such a trial was recently performed in 776 immunocompromised patients who either received standard oxygen or NHF [32]. Primary endpoint was D-28 mortality and secondary endpoints included intubation rate. NIV was not used according to the results of a previous study [32]. Patients were mostly admitted for pneumonia. Mortality rates did not differ between NHF (35, 6%) and standard oxygen (36, 1%) (p = 0, 94), as well as intubation rates (respectively, 38, 7% and 43.8%, p = 0, 17). The mortality rates for patients who required intubation did not differ either. In a predefined subgroup of patients (oxygen flow > 9 l/min, duration between ICU admission and randomization > 3 days or use of vasopressors), primary and secondary endpoints did not differ. In this study, greater PaO2/FiO2 obtained with NHF did not translate into better outcome.
More recently Dumas et al. analysed the daily probability of intubation according to the patient’s characteristics the day before [33]. Using a propensity score, authors did not find any impact of the oxygenation device on the probability of intubation the following day. In this post hoc joint analysis of three previously published studies, only a small proportion of patients received NHF.
How can data from non-immunocompromised patients indicating more positive effects of NHF be reconciled with the more neutral data coming from immunocompromised patients? One possible explanation is that patients’ underlying disease and/or the precipitating factor leading to AHRF in immunocompromised patients require more time for recovery. Consequently, these patients may have a longer duration of oxygen dependency and may require more invasive procedures. In addition, comfort was not improved in these patients. This may be related to other sources of discomfort (side effects of chemotherapy) than respiratory ones in those patients that were not relieved by NHF. For all those reasons, the nature of the ventilatory support may not have such impact in this particular setting.
Recent meta-analyses focusing on immunocompromised patients [35, 36] have included the studies presented here and all conclude that use of NHF is associated with a decreased intubation rate but with no impact on mortality.
NHF in hypercapnic respiratory failure
Physiological effects in stable COPD
As illustrated above, there is a strong rationale for the use of NHF in patients with chronic respiratory failure [37].
Comparable to patients with AHRF, NHF may reduce the entrainment of room air during high breathing efforts, such as during exercise [38]. Early physiological studies revealed an increase in mean airway pressure [39], and a decrease in dead-space ventilation [40]. These changes increase tidal volume, decrease respiratory rate and end-expiratory lung volume [4, 39, 41, 42] which result in a measurable reduction in work of breathing [23].
A direct comparison of respiratory parameters under three conditions (oxygen, NHF and NIV) was conducted by Longhini et al. [43]. Diaphragmatic sonography and ventilatory parameters rose during interruptions of NIV trials (30 min). PaCO2 remained stable irrespective of the modality of oxygen administration. However, respiratory rate and diaphragm contractile activation (inspiratory thickening fraction) increased with standard oxygen, but not with NHF. The latter was associated with improved comfort. This study, therefore, suggested that NHF might lead to a greater unload of the diaphragm than standard oxygen.
In stable COPD patients, studies have consistently shown that NHF reduces hypercapnia despite a decreased respiratory rate [41, 42, 44]. This is related to a flow- and leakage-dependent clearance of upper airway gases that reduces CO2 rebreathing [44, 45]. These findings were confirmed by Bräunlich et al. in the clinical setting [46]. They found that after 6 weeks, reduction of hypercapnia and improvement in quality of life obtained with NHF were non-inferior to those obtained with NIV. These results may be, however, limited to patients without overlap syndrome (i.e. association of COPD and obstructive sleep apnea), as recently demonstrated [47]. A summary of these studies is detailed in ESM Table 3.
Strategies for NHF in hypercapnic respiratory failure
NIV is the ventilatory modality of first choice in hypercapnic ARF [48]. However poor tolerance often limits its success.
NHF has been suggested as complementary therapy during breaks off NIV [43, 49], or as an alternative to NIV [50] or controlled oxygen therapy [51] in mild respiratory acidosis.
By overcoming the drawbacks of standard oxygen during breaks off NIV [43], NHF could reduce the time spent on ventilator and improve work of breathing during breaks [50]. A single RCT assessed NHF in this scenario, on a mixed population with 22 out of 54 hypercapnic subjects [49], while not reducing the time spent on NIV, NHF improved comfort, control of dyspnea and respiratory rate compared to standard oxygen. The main limitations of this study, i.e. small sample size and possibility to override the criteria for NIV sessions, are expected to be overcome by the High-flow ACRF trial [52]. This ongoing large-scale RCT will assess ventilator-free days when comparing NHF to standard oxygen during breaks off NIV.
NHF has been proposed as an alternative to NIV in mild-to-moderate respiratory acidosis [51]. An ongoing non-inferiority multi-center trial will further explore this strategy by assessing short-term effects on gas exchange and treatment failure [53].
These and future studies will be needed to better assess the role of NHF in hypercapnic ARF, to understand which strategies are better to pursue.
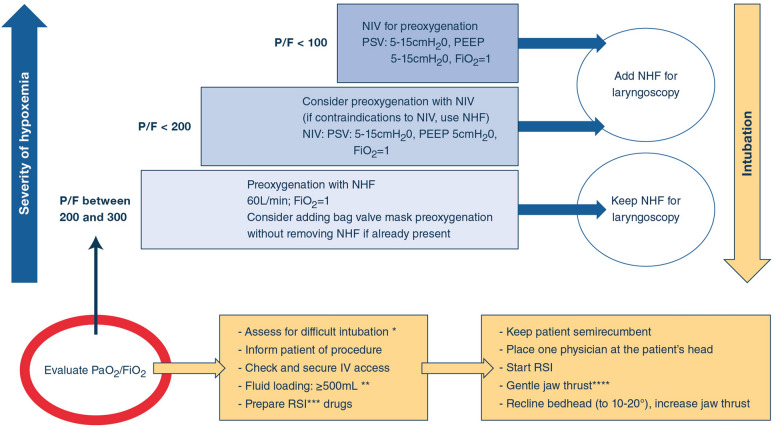
NHF and preoxygenation
A significant proportion of patients admitted to the ICU for AHRF will fail a noninvasive ventilatory strategy and, thus, require tracheal intubation [54]. In these patients, this procedure is at even greater risk of complications, mainly oxygen desaturation [55]. Studies have clearly shown that standard preoxygenation, even when properly performed, is insufficient to ensure satisfactory oxygenation levels in critically ill patients. This has led clinicians to investigate other modes of preoxygenation. NIV was convincingly shown to be superior to standard oxygen [56], although a confirmatory trial failed to confirm NIV’s superiority [57]. Because a growing number of patients with AHRF are treated with NHF as first-line ventilatory support [58], the device is often in place when the decision to intubate is taken. Hence, NHF has also been evaluated as a means to prevent desaturation during intubation [59]. Compared to standard oxygen, results of preoxygenation with NFH seem consistent in patients with mild-to-moderate hypoxemia [57, 60]. Paradoxically, in patients with more severe hypoxemia, NHF failed to prove superior than standard oxygen to prevent profound desaturation during intubation [61, 62]. Of note however, suboptimal preoxygenation procedures (absence of jaw thrust which is essential to promote apneic oxygenation) may explain these discrepancies [63]. This illustrates the importance of the two components of the “preoxygenation process”: preoxygenation and apneic oxygenation. Intuitively, because of the greater levels of positive pressure applied, NIV may be seen superior to NHF during the spontaneously breathing phase and NHF may prove more beneficial during apnea and laryngoscopy because it can be left in place. This hypothesis was tested in a recent RCT that compared NIV and NHF to ensure preoxygenation of patients with AHRF requiring tracheal intubation in the ICU [64]. Primary outcome measure was incidence of profound desaturation (SpO2 < 80%). There was no difference between the two strategies in this incidence (23% with NIV v. 27% with HFNC) in the overall study patients. In patients with moderate-to-severe hypoxemia (PaO2/FiO2 ≤ 200 mm Hg), desaturation < 80% occurred less frequently after preoxygenation with NIV than with nasal high-flow (24% v. 35% respectively, p = 0·046). Serious adverse events did not differ between the two groups. Finally, based on the above, the combination of both NIV and NHF to prevent desaturation during intubation was compared to NIV alone. Significantly less desaturations occurred with the combination [65]. Based on all these results, we can suggest an algorithm to guide clinicians in their choice of preoxygenation technique (see Fig. 3).
Fig. 3.
Suggested algorithm for deciding how to preoxygenate a patient with AHRF who requires tracheal intubation. NIV: non-invasive ventilation; NHF: nasal high flow; PEEP: positive-end expiratory pressure; PSV: pressure support ventilation. *The MACOCHA score can be used; **low dose vasopressor may be also started in unstable patients; ***RSI: rapid sequence induction; ****jaw thrust is essential to ensure patent upper airway and efficient apneic oxygenation
NHF in the postextubation
Preventing reintubation is the cornerstone of patient management after extubation because of the complications associated with reintubation (prolonged mechanical ventilation and ICU stay, ventilator-associated pneumonia…). It has been suggested that NIV should not be used in patients with established post-extubation respiratory failure [48], after a safety concern was raised secondary to the risk of delaying reintubation. However, NIV has a preventive role in patients at high-risk for failure [48, 66].
Estimation of risk for failure generates controversy, as no score predicting failure in a general population of intubated patients has been validated and risks depend largely on patient population. ESM Table 4 displays these different risk factors. In surgical patients, expected reintubation rate is low because of the short duration of mechanical ventilation, and reasons for failing extubation are specific (e.g. anaesthetic factors, airway patency, surgical complications) [67]. Thus, studies in these patients are usually powered for primary outcomes different from the reintubation rate, and include composite end-points or have a non-inferiority design [68, 69]. In medical patients, many risk factors have been described, but most of them with a low level of evidence [70]. In addition, subjective definitions for these risks (those related to cough and secretions management for example) limit their reproducibility in clinical trials. Traditional definition of patients at high-risk required at least one risk factor, but recent trials including a large number of those risk factors, suggest that the risk for failing extubation should be better defined [71, 72]. This is supported by results of multivariable models, reporting more than one independently associated high-risk factor to reintubation [70], with a potential summation effect, and previous data reporting a synergistic interaction between high-risk factors for reintubation [73]. These issues are worth considering when analyzing the data.
Several studies have compared NHF to standard oxygen to prevent reintubation according to a given risk for failure. In a large heterogeneous population of patients at low risk [74], including complicated surgical patients with more than 12 h of mechanical ventilation, NHF significantly reduce post-extubation respiratory failure and reintubation rate after 24 h in comparison with standard oxygen. No such difference was found in another study in uncomplicated patients after abdominal surgery [69]. A probably lower risk for respiratory complications in the OPERA trial explains this discrepancy [69]. Recent meta-analyses confirm the superiority of NHF over conventional oxygen therapy in terms of post-extubation respiratory failure and reintubation rate [75].
In high-risk patients, two large studies found that NHF was non-inferior to NIV [68, 72]: one in a general population [72], the other cardiothoracic surgery patients [68]. Discomfort limited the effective time under NIV in these studies to 14 and 6.6 h, respectively, during the first 24 h. This was particularly the case after cardiothoracic surgery, where discomfort was significantly more frequent with NIV than with NHF.
A recent trial compared NHF to the combination of NHF and NIV in high-risk patients [76]. Patients received preventive therapy for a minimum of 48 h. Very similar to previous results [72], time spent under NIV was 13 h during the first 24 h highlighting the fact that NIV tolerance may be a limitation to this strategy in this subset of patients. Nonetheless, authors found that the combination of NHF and NIV led to less reintubation that NHF alone. Interestingly, reintubation rate at day 7 was significantly lower with NIV than with NHF alone in patients with PaCO2 > 45 mmHg before extubation, but no such difference was found in patients with PaCO2 < 45 mmHg.
In high-risk patients, the combination of NIV and NHF therefore seems to benefit more patients with pre-extubation hypercapnia. Duration of preventive therapy and date of assessment of reintubation are important variables to take into account.
NHF in the ED and palliative care
Several RCTs compare NHF to standard oxygen via low-flow nasal prongs or facemask in ED for adults with moderate-to-severe respiratory distress in different conditions [15–18]. A systematic review of these RCTs [15–18] found no difference in mortality (RR 1.20; 95% CI 0.58, 2.48, p = 0.62) or treatment failure (RR 1.49; 95% CI 0.33, 6.82, p = 0.60) compared to standard oxygen. However, more patients did not tolerate NHF than standard oxygen (RR 6.81; 95% CI 1.18, 39.19, p = 0.03) [19]. These data are limited as rates of intubation (1.2%) and NIV (3.1%) were low, despite enrolment of patients with AHRF in the included studies. This is because patients needing immediate NIV or intubation were excluded from the studies. Standard care in ED is usually effective in avoiding mechanical ventilation in the remaining patients and studies may have included patients with ceilings of care. So, any differences between NHF and standard oxygen for these outcomes are likely to be small. Compared to NIV for undifferentiated respiratory failure, there was no difference between NHF for any outcome in a single RCT [20]. In contrast, a small RCT in palliative patients with limitations on invasive ventilation found dyspnea was reduced with NHF compared to NIV [77]. NHF may have a role in some ED patients who would not be offered intubation or when NIV is not well tolerated. More studies are required to confirm this.
NIV is recommended in palliative care [48]. However, patient discomfort and inability to eat or communicate may limit its use. NHF may be an alternative method for providing oxygen and respiratory support in this setting. Many studies have reported the benefit of NHF by alleviating dyspnea in patients with advanced cancer and do-not-intubate patients with hypoxemic respiratory failure [78–81]. Furthermore, NHF might not be inferior to NIV in palliation of dyspnea in patients with terminal cancer [82]. However, further studies are needed to evaluate the benefits of NHF in terms of patient comfort and quality of life in palliative care.
Concluding remarks
In a small 10-year span, NHF has found its place in the armamentarium of AHRF treatment. In every segment of AHRF management (first-line ventilatory support, preoxygenation, post-extubation, palliative care), evidence suggests benefits to the patient. Interestingly, there are still aspects that further need investigation. These include improving comfort, exploring the potential for even higher flows, and addressing the issue of weaning.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank Camille Le Breton for her support in drawing Figure n.3.
Compliance with ethical standards
Conflicts of interest
JDR received travel expenses and accommodation coverage from Fisher&Paykel Healthcare to attend scientific meetings. Fisher&Paykel Healthcare provided support for the ongoing High Flow ACRF trial (NCT03406572) but took no part in design or conduct of the study. OR received speaker fees from Air Liquide. His institution received consultancy fees from Hamilton Medical. VL has no conflict of interest to declare concerning this topic. JB received travel expenses, lecture fees and accommodation coverage from TNI medical AG and Fisher & Paykel Healthcare. TNI medical AG provided support for several NHF trials. AC’s employer, on her behalf, has received travel expenses, lecture fees and accommodation from Fisher & Paykel Healthcare to attend scientific meetings. Fisher & Paykel Healthcare has also provided an unrestricted grant to support investigator driven research, but has had no part in study design, conduct, analysis or reporting of the studies. PJ received competitive grant funding from the A + Trust (4926) and Greenlane Research and Education Fund (12/15/4086) for the HOTER RCT (ACTRN12610000960411) on HFNO in the ED. F&P Healthcare provided equipment for the HOTER RCT for which PJ was the principal investigator, but took no part in design, conduct, analysis or reporting of the study. PJ has no other personal financial or professional to declare. BJK: has no conflict of interest to declare. FL: Fisher&Paykel Healthcare provided support for the development of an application VentilO on optimization of protective mechanical ventilation. SN: Fisher&Paykel Healthcare provided support for the study # NCT03759457. NR received travel expenses and lecture fees from Fisher&Paykel Healthcare. GS: Fisher&Paykel Healthcare provided support for the study # NCT03965832 for which GS is the principal investigator. SJ received personal fees as consultant from Fisher-Paykel. GH received travel expenses coverage and lecture fees from Fisher&Paykel.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Delorme M, Bouchard P-A, Simon M, et al. Effects of high-flow nasal cannula on the work of breathing in patients recovering from acute respiratory failure. Crit Care Med. 2017;45:1981–1988. doi: 10.1097/CCM.0000000000002693. [DOI] [PubMed] [Google Scholar]
- 2.Mauri T, Alban L, Turrini C, et al. Optimum support by high-flow nasal cannula in acute hypoxemic respiratory failure: effects of increasing flow rates. Intensive Care Med. 2017;43:1453–1463. doi: 10.1007/s00134-017-4890-1. [DOI] [PubMed] [Google Scholar]
- 3.Mauri T, Turrini C, Eronia N, et al. Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195:1207–1215. doi: 10.1164/rccm.201605-0916OC. [DOI] [PubMed] [Google Scholar]
- 4.Bräunlich J, Köhler M, Wirtz H. Nasal highflow improves ventilation in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:1077–1085. doi: 10.2147/COPD.S104616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Corley A, Caruana LR, Barnett AG, et al. Oxygen delivery through high-flow nasal cannulae increase end-expiratory lung volume and reduce respiratory rate in post-cardiac surgical patients. Br J Anaesth. 2011;107:998–1004. doi: 10.1093/bja/aer265. [DOI] [PubMed] [Google Scholar]
- 6.Mauri T, Galazzi A, Binda F, et al. Impact of flow and temperature on patient comfort during respiratory support by high-flow nasal cannula. Crit Care. 2018;22:120. doi: 10.1186/s13054-018-2039-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Messika J, Ben Ahmed K, Gaudry S, et al. Use of high-flow nasal cannula oxygen therapy in subjects with ARDS: a 1-year observational study. Respir Care. 2015;60:162–169. doi: 10.4187/respcare.03423. [DOI] [PubMed] [Google Scholar]
- 8.Roca O, Pérez-Terán P, Masclans JR, et al. Patients with New York Heart Association class III heart failure may benefit with high flow nasal cannula supportive therapy: high flow nasal cannula in heart failure. J Crit Care. 2013;28:741–746. doi: 10.1016/j.jcrc.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 9.Roca O, de Acilu MG, Caralt B, et al. Humidified high flow nasal cannula supportive therapy improves outcomes in lung transplant recipients readmitted to the intensive care unit because of acute respiratory failure. Transplantation. 2015;99:1092–1098. doi: 10.1097/TP.0000000000000460. [DOI] [PubMed] [Google Scholar]
- 10.Rello J, Pérez M, Roca O, et al. High-flow nasal therapy in adults with severe acute respiratory infection: a cohort study in patients with 2009 influenza A/H1N1v. J Crit Care. 2012;27:434–439. doi: 10.1016/j.jcrc.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 11.Sztrymf B, Messika J, Bertrand F, et al. Beneficial effects of humidified high flow nasal oxygen in critical care patients: a prospective pilot study. Intensive Care Med. 2011;37:1780–1786. doi: 10.1007/s00134-011-2354-6. [DOI] [PubMed] [Google Scholar]
- 12.Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372(23):2185–2196. doi: 10.1056/NEJMoa1503326. [DOI] [PubMed] [Google Scholar]
- 13.Rochwerg B, Granton D, Wang DX, et al. High flow nasal cannula compared with conventional oxygen therapy for acute hypoxemic respiratory failure: a systematic review and meta-analysis. Intensive Care Med. 2019;45:563–572. doi: 10.1007/s00134-019-05590-5. [DOI] [PubMed] [Google Scholar]
- 14.Monro-Somerville T, Sim M, Ruddy J, et al. The effect of high-flow nasal cannula oxygen therapy on mortality and intubation rate in acute respiratory failure: a systematic review and meta-analysis. Crit Care Med. 2017;45:e449–e456. doi: 10.1097/CCM.0000000000002091. [DOI] [PubMed] [Google Scholar]
- 15.Jones PG, Kamona S, Doran O, et al. Randomized controlled trial of humidified high-flow nasal oxygen for acute respiratory distress in the emergency department: the HOT-ER study. Respir Care. 2016;61:291–299. doi: 10.4187/respcare.04252. [DOI] [PubMed] [Google Scholar]
- 16.Makdee O, Monsomboon A, Surabenjawong U, et al. High-flow nasal cannula versus conventional oxygen therapy in emergency department patients with cardiogenic pulmonary edema: a randomized controlled trial. Ann Emerg Med. 2017;70:465–472.e2. doi: 10.1016/j.annemergmed.2017.03.028. [DOI] [PubMed] [Google Scholar]
- 17.Bell N, Hutchinson CL, Green TC, et al. Randomised control trial of humidified high flow nasal cannulae versus standard oxygen in the emergency department: high flow oxygen randomised control trial. Emerg Med Australas. 2015;27:537–541. doi: 10.1111/1742-6723.12490. [DOI] [PubMed] [Google Scholar]
- 18.Rittayamai N, Tscheikuna J, Praphruetkit N, Kijpinyochai S. Use of high-flow nasal cannula for acute dyspnea and hypoxemia in the emergency department. Respir Care. 2015;60:1377–1382. doi: 10.4187/respcare.03837. [DOI] [PubMed] [Google Scholar]
- 19.Tinelli V, Cabrini L, Fominskiy E, et al. High flow nasal cannula oxygen vs. conventional oxygen therapy and noninvasive ventilation in emergency department patients: a systematic review and meta-analysis. J Emerg Med. 2019;57:322–328. doi: 10.1016/j.jemermed.2019.06.033. [DOI] [PubMed] [Google Scholar]
- 20.Doshi P, Whittle JS, Bublewicz M, et al. High-velocity nasal insufflation in the treatment of respiratory failure: a randomized clinical trial. Ann Emerg Med. 2018;72:73–83.e5. doi: 10.1016/j.annemergmed.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 21.García-de-Acilu M, Marin-Corral J, Vázquez A, et al. Hypoxemic patients with bilateral infiltrates treated with high-flow nasal cannula present a similar pattern of biomarkers of inflammation and injury to acute respiratory distress syndrome patients. Crit Care Med. 2017;45:1845–1853. doi: 10.1097/CCM.0000000000002647. [DOI] [PubMed] [Google Scholar]
- 22.Roca O, Messika J, Caralt B, et al. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: the utility of the ROX index. J Crit Care. 2016;35:200–205. doi: 10.1016/j.jcrc.2016.05.022. [DOI] [PubMed] [Google Scholar]
- 23.Roca O, Caralt B, Messika J, et al. An index combining respiratory rate and oxygenation to predict outcome of nasal high-flow therapy. Am J Respir Crit Care Med. 2019;199:1368–1376. doi: 10.1164/rccm.201803-0589OC. [DOI] [PubMed] [Google Scholar]
- 24.Bellani G, Laffey JG, Pham T, et al. Noninvasive ventilation of patients with acute respiratory distress syndrome. insights from the LUNG SAFE study. Am J Respir Crit Care Med. 2017;195:67–77. doi: 10.1164/rccm.201606-1306OC. [DOI] [PubMed] [Google Scholar]
- 25.Kang BJ, Koh Y, Lim C-M, et al. Failure of high-flow nasal cannula therapy may delay intubation and increase mortality. Intensive Care Med. 2015;41:623–632. doi: 10.1007/s00134-015-3693-5. [DOI] [PubMed] [Google Scholar]
- 26.Nedel WL, Deutschendorf C, Moraes Rodrigues Filho E. High-flow nasal cannula in critically ill subjects with or at risk for respiratory failure: a systematic review and meta-analysis. Respir Care. 2017;62:123–132. doi: 10.4187/respcare.04831. [DOI] [PubMed] [Google Scholar]
- 27.Mokart D, Geay C, Chow-Chine L, et al. High-flow oxygen therapy in cancer patients with acute respiratory failure. Intensive Care Med. 2015;41:2008–2010. doi: 10.1007/s00134-015-3994-8. [DOI] [PubMed] [Google Scholar]
- 28.Coudroy R, Jamet A, Petua P, et al. High-flow nasal cannula oxygen therapy versus noninvasive ventilation in immunocompromised patients with acute respiratory failure: an observational cohort study. Ann Intensive Care. 2016;6:45. doi: 10.1186/s13613-016-0151-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Frat J-P, Ragot S, Girault C, et al. Effect of non-invasive oxygenation strategies in immunocompromised patients with severe acute respiratory failure: a post hoc analysis of a randomised trial. Lancet Respir Med. 2016;4:646–652. doi: 10.1016/S2213-2600(16)30093-5. [DOI] [PubMed] [Google Scholar]
- 30.Tu G, He H, Yin K, et al. High-flow nasal cannula versus noninvasive ventilation for treatment of acute hypoxemic respiratory failure in renal transplant recipients. Transpl Proc. 2017;49:1325–1330. doi: 10.1016/j.transproceed.2017.03.088. [DOI] [PubMed] [Google Scholar]
- 31.Lemiale V, Resche-Rigon M, Mokart D, et al. High-flow nasal cannula oxygenation in immunocompromised patients with acute hypoxemic respiratory failure: a groupe de recherche respiratoire en réanimation onco-hématologique study. Crit Care Med. 2017;45:e274–e280. doi: 10.1097/CCM.0000000000002085. [DOI] [PubMed] [Google Scholar]
- 32.Azoulay E, Lemiale V, Mokart D, et al. Effect of high-flow nasal oxygen vs standard oxygen on 28-day mortality in immunocompromised patients with acute respiratory failure: the HIGH randomized clinical trial. JAMA. 2018;320:2099–2107. doi: 10.1001/jama.2018.14282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dumas G, Chevret S, Lemiale V, et al. Oxygenation/non-invasive ventilation strategy and risk for intubation in immunocompromised patients with hypoxemic acute respiratory failure. Oncotarget. 2018;9:33682–33693. doi: 10.18632/oncotarget.26069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Azoulay E, Pickkers P, Soares M, et al. Acute hypoxemic respiratory failure in immunocompromised patients: the Efraim multinational prospective cohort study. Intensive Care Med. 2017;43:1808–1819. doi: 10.1007/s00134-017-4947-1. [DOI] [PubMed] [Google Scholar]
- 35.Cortegiani A, Crimi C, Sanfilippo F, et al. High flow nasal therapy in immunocompromised patients with acute respiratory failure: a systematic review and meta-analysis. J Crit Care. 2019;50:250–256. doi: 10.1016/j.jcrc.2018.12.015. [DOI] [PubMed] [Google Scholar]
- 36.Wang Y, Ni Y, Sun J, Liang Z. Use of high-flow nasal cannula for immunocompromise and acute respiratory failure: a systematic review and meta-analysis. J Emerg Med. 2020;58:413–423. doi: 10.1016/j.jemermed.2020.01.016. [DOI] [PubMed] [Google Scholar]
- 37.Pisani L, Vega ML. Use of nasal high flow in stable COPD: rationale and physiology. COPD J Chron Obstruct Pulmon Dis. 2017;14:346–350. doi: 10.1080/15412555.2017.1315715. [DOI] [PubMed] [Google Scholar]
- 38.Ritchie JE, Williams AB, Gerard C, Hockey H. Evaluation of a humidified nasal high-flow oxygen system, using oxygraphy, capnography and measurement of upper airway pressures. Anaesth Intensive Care. 2011;39:1103–1110. doi: 10.1177/0310057X1103900620. [DOI] [PubMed] [Google Scholar]
- 39.Bräunlich J, Beyer D, Mai D, et al. Effects of nasal high flow on ventilation in volunteers, COPD and idiopathic pulmonary fibrosis patients. Respiration. 2013;85:319–325. doi: 10.1159/000342027. [DOI] [PubMed] [Google Scholar]
- 40.Biselli P, Fricke K, Grote L, et al. Reductions in dead space ventilation with nasal high flow depend on physiological dead space volume: metabolic hood measurements during sleep in patients with COPD and controls. Eur Respir J. 2018;51:1702251. doi: 10.1183/13993003.02251-2017. [DOI] [PubMed] [Google Scholar]
- 41.Fraser JF, Spooner AJ, Dunster KR, et al. Nasal high flow oxygen therapy in patients with COPD reduces respiratory rate and tissue carbon dioxide while increasing tidal and end-expiratory lung volumes: a randomised crossover trial. Thorax. 2016;71:759–761. doi: 10.1136/thoraxjnl-2015-207962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pisani L, Fasano L, Corcione N, et al. Change in pulmonary mechanics and the effect on breathing pattern of high flow oxygen therapy in stable hypercapnic COPD. Thorax. 2017;72:373–375. doi: 10.1136/thoraxjnl-2016-209673. [DOI] [PubMed] [Google Scholar]
- 43.Longhini F, Pisani L, Lungu R, et al. High-flow oxygen therapy after noninvasive ventilation interruption in patients recovering from hypercapnic acute respiratory failure: a physiological crossover trial. Crit Care Med. 2019;47:e506–e511. doi: 10.1097/CCM.0000000000003740. [DOI] [PubMed] [Google Scholar]
- 44.Bräunlich J, Mauersberger F, Wirtz H. Effectiveness of nasal highflow in hypercapnic COPD patients is flow and leakage dependent. BMC Pulm Med. 2018;18:14. doi: 10.1186/s12890-018-0576-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Möller W, Feng S, Domanski U, et al. Nasal high flow reduces dead space. J Appl Physiol. 2017;122:191–197. doi: 10.1152/japplphysiol.00584.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bräunlich J, Dellweg D, Bastian A, et al. Nasal high-flow versus noninvasive ventilation in patients with chronic hypercapnic COPD. COPD. 2019;14:1411–1421. doi: 10.2147/COPD.S206111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pisani L, Betti S, Biglia C, et al. Effects of high-flow nasal cannula in patients with persistent hypercapnia after an acute COPD exacerbation: a prospective pilot study. BMC Pulm Med. 2020;20:12. doi: 10.1186/s12890-020-1048-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50:1602426. doi: 10.1183/13993003.02426-2016. [DOI] [PubMed] [Google Scholar]
- 49.Spoletini G, Mega C, Pisani L, et al. High-flow nasal therapy vs standard oxygen during breaks off noninvasive ventilation for acute respiratory failure: a pilot randomized controlled trial. J Crit Care. 2018;48:418–425. doi: 10.1016/j.jcrc.2018.10.004. [DOI] [PubMed] [Google Scholar]
- 50.Lee MK, Choi J, Park B, et al. High flow nasal cannulae oxygen therapy in acute-moderate hypercapnic respiratory failure. Clin Respir J. 2018;12:2046–2056. doi: 10.1111/crj.12772. [DOI] [PubMed] [Google Scholar]
- 51.Pilcher J, Eastlake L, Richards M, et al. Physiological effects of titrated oxygen via nasal high-flow cannulae in COPD exacerbations: a randomized controlled cross-over trial. Respirology. 2017;22:1149–1155. doi: 10.1111/resp.13050. [DOI] [PubMed] [Google Scholar]
- 52.Ricard J-D, Dib F, Esposito-Farese M, et al. Comparison of high flow nasal cannula oxygen and conventional oxygen therapy on ventilatory support duration during acute-on-chronic respiratory failure: study protocol of a multicentre, randomised, controlled trial. The “HIGH-FLOW ACRF” study. BMJ Open. 2018;8:e022983. doi: 10.1136/bmjopen-2018-022983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cortegiani A, Longhini F, Carlucci A, et al. High-flow nasal therapy versus noninvasive ventilation in COPD patients with mild-to-moderate hypercapnic acute respiratory failure: study protocol for a noninferiority randomized clinical trial. Trials. 2019;20:450. doi: 10.1186/s13063-019-3514-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ricard JD, Gaborieau B, Bernier J, et al. Use of high flow nasal cannula for preoxygenation and apneic oxygenation during intubation. Ann Transl Med. 2019;7:S380. doi: 10.21037/atm.2019.12.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ricard JD. Hazards of intubation in the ICU: role of nasal high flow oxygen therapy for preoxygenation and apneic oxygenation to prevent desaturation. Minerva Anestesiol. 2016;82:1098–1106. [PubMed] [Google Scholar]
- 56.Baillard C, Fosse J-P, Sebbane M, et al. Noninvasive ventilation improves preoxygenation before intubation of hypoxic patients. Am J Respir Crit Care Med. 2006;174:171–177. doi: 10.1164/rccm.200509-1507OC. [DOI] [PubMed] [Google Scholar]
- 57.Baillard C, Prat G, Jung B, et al. Effect of preoxygenation using non-invasive ventilation before intubation on subsequent organ failures in hypoxaemic patients: a randomised clinical trial. Br J Anaesth. 2018;120:361–367. doi: 10.1016/j.bja.2017.11.067. [DOI] [PubMed] [Google Scholar]
- 58.Papazian L, Corley A, Hess D, et al. Use of high-flow nasal cannula oxygenation in ICU adults: a narrative review. Intensive Care Med. 2016;42:1336–1349. doi: 10.1007/s00134-016-4277-8. [DOI] [PubMed] [Google Scholar]
- 59.Miguel-Montanes R, Hajage D, Messika J, et al. Use of high-flow nasal cannula oxygen therapy to prevent desaturation during tracheal intubation of intensive care patients with mild-to-moderate hypoxemia. Crit Care Med. 2015;43:574–583. doi: 10.1097/CCM.0000000000000743. [DOI] [PubMed] [Google Scholar]
- 60.Guitton C, Ehrmann S, Volteau C, et al. Nasal high-flow preoxygenation for endotracheal intubation in the critically ill patient: a randomized clinical trial. Intensive Care Med. 2019;45:447–458. doi: 10.1007/s00134-019-05529-w. [DOI] [PubMed] [Google Scholar]
- 61.Vourc’hVourc’h M, Asfar P, Volteau C, et al. High-flow nasal cannula oxygen during endotracheal intubation in hypoxemic patients: a randomized controlled clinical trial. Intensive Care Med. 2015;41:1538–1548. doi: 10.1007/s00134-015-3796-z. [DOI] [PubMed] [Google Scholar]
- 62.Simon M, Wachs C, Braune S, et al. High-flow nasal cannula versus bag-valve-mask for preoxygenation before intubation in subjects with hypoxemic respiratory failure. Respir Care. 2016;61:1160–1167. doi: 10.4187/respcare.04413. [DOI] [PubMed] [Google Scholar]
- 63.De Jong A, Jaber S. Apneic oxygenation for intubation in the critically ill. Let’s not give up! Am J Respir Crit Care Med. 2016;193:230–232. doi: 10.1164/rccm.201510-1998ED. [DOI] [PubMed] [Google Scholar]
- 64.Frat J-P, Ricard J-D, Quenot J-P, et al. Non-invasive ventilation versus high-flow nasal cannula oxygen therapy with apnoeic oxygenation for preoxygenation before intubation of patients with acute hypoxaemic respiratory failure: a randomised, multicentre, open-label trial. Lancet Respir Med. 2019;7:303–312. doi: 10.1016/S2213-2600(19)30048-7. [DOI] [PubMed] [Google Scholar]
- 65.Jaber S, Monnin M, Girard M, et al. Apnoeic oxygenation via high-flow nasal cannula oxygen combined with non-invasive ventilation preoxygenation for intubation in hypoxaemic patients in the intensive care unit: the single-centre, blinded, randomised controlled OPTINIV trial. Intensive Care Med. 2016;42:1877–1887. doi: 10.1007/s00134-016-4588-9. [DOI] [PubMed] [Google Scholar]
- 66.Esteban A, Frutos-Vivar F, Ferguson ND, et al. Noninvasive positive-pressure ventilation for respiratory failure after extubation. N Engl J Med. 2004;350:2452–2460. doi: 10.1056/NEJMoa032736. [DOI] [PubMed] [Google Scholar]
- 67.Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113:1338–1350. doi: 10.1097/ALN.0b013e3181fc6e0a. [DOI] [PubMed] [Google Scholar]
- 68.Stéphan F, Barrucand B, Petit P, et al. High-flow nasal oxygen vs noninvasive positive airway pressure in hypoxemic patients after cardiothoracic surgery: a randomized clinical trial. JAMA. 2015;313:2331–2339. doi: 10.1001/jama.2015.5213. [DOI] [PubMed] [Google Scholar]
- 69.Futier E, Paugam-Burtz C, Godet T, et al. Effect of early postextubation high-flow nasal cannula vs conventional oxygen therapy on hypoxaemia in patients after major abdominal surgery: a French multicentre randomised controlled trial (OPERA) Intensive Care Med. 2016;42:1888–1898. doi: 10.1007/s00134-016-4594-y. [DOI] [PubMed] [Google Scholar]
- 70.Thille AW, Boissier F, Ben Ghezala H, et al. Risk factors for and prediction by caregivers of extubation failure in ICU patients: a prospective study. Crit Care Med. 2015;43:613–620. doi: 10.1097/CCM.0000000000000748. [DOI] [PubMed] [Google Scholar]
- 71.Ferrer M, Valencia M, Nicolas JM, et al. Early noninvasive ventilation averts extubation failure in patients at risk: a randomized trial. Am J Respir Crit Care Med. 2006;173:164–170. doi: 10.1164/rccm.200505-718OC. [DOI] [PubMed] [Google Scholar]
- 72.Hernández G, Vaquero C, Colinas L, et al. Effect of postextubation high-flow nasal cannula vs noninvasive ventilation on reintubation and postextubation respiratory failure in high-risk patients: a randomized clinical trial. JAMA. 2016;316:1565–1574. doi: 10.1001/jama.2016.14194. [DOI] [PubMed] [Google Scholar]
- 73.Salam A, Tilluckdharry L, Amoateng-Adjepong Y, Manthous CA. Neurologic status, cough, secretions and extubation outcomes. Intensive Care Med. 2004;30:1334–1339. doi: 10.1007/s00134-004-2231-7. [DOI] [PubMed] [Google Scholar]
- 74.Hernández G, Vaquero C, González P, et al. Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA. 2016;315:1354–1361. doi: 10.1001/jama.2016.2711. [DOI] [PubMed] [Google Scholar]
- 75.Zhu Y, Yin H, Zhang R, et al. High-flow nasal cannula oxygen therapy versus conventional oxygen therapy in patients after planned extubation: a systematic review and meta-analysis. Crit Care. 2019;23:180. doi: 10.1186/s13054-019-2465-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Thille AW, Muller G, Gacouin A, et al. Effect of postextubation high-flow nasal oxygen with noninvasive ventilation vs high-flow nasal oxygen alone on reintubation among patients at high risk of extubation failure: a randomized clinical trial. JAMA. 2019;322:1465–1475. doi: 10.1001/jama.2019.14901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ruangsomboon O, Dorongthom T, Chakorn T, et al. High-flow nasal cannula versus conventional oxygen therapy in relieving dyspnea in emergency palliative patients with do-not-intubate status: a randomized crossover study. Ann Emerg Med. 2020;75:615–626. doi: 10.1016/j.annemergmed.2019.09.009. [DOI] [PubMed] [Google Scholar]
- 78.Epstein AS, Hartridge-Lambert SK, Ramaker JS, et al. Humidified high-flow nasal oxygen utilization in patients with cancer at Memorial Sloan-Kettering Cancer Center. J Palliat Med. 2011;14:835–839. doi: 10.1089/jpm.2011.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Peters SG, Holets SR, Gay PC. Nasal high flow oxygen therapy in do-not-intubate patients with hypoxemic respiratory distress. Respir Care. 2013;58:597–600. doi: 10.4187/respcare.01887. [DOI] [PubMed] [Google Scholar]
- 80.Koyauchi T, Hasegawa H, Kanata K, et al. Efficacy and tolerability of high-flow nasal cannula oxygen therapy for hypoxemic respiratory failure in patients with interstitial lung disease with do-not-intubate orders: a retrospective single-center study. Respiration. 2018;96:323–329. doi: 10.1159/000489890. [DOI] [PubMed] [Google Scholar]
- 81.Zemach S, Helviz Y, Shitrit M, et al. The use of high-flow nasal cannula oxygen outside the ICU. Respir Care. 2019;64:1333–1342. doi: 10.4187/respcare.06611. [DOI] [PubMed] [Google Scholar]
- 82.Hui D, Morgado M, Chisholm G, et al. High-flow oxygen and bilevel positive airway pressure for persistent dyspnea in patients with advanced cancer: a phase II randomized trial. J Pain Symptom Manage. 2013;46:463–473. doi: 10.1016/j.jpainsymman.2012.10.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.