Eccrine hidrocystoma (EH) is a benign tumor derived from the cystic dilatation of the eccrine sweat ducts caused by the retention of eccrine secretions. EH is rare and is found most often in middle-aged women, especially those who work or stay for a long duration in hot and humid environments. The lesions usually involve periocular and malar areas, manifesting as multiple translucent skin-colored to bluish cysts. The sizes and numbers of the lesions can fluctuate according to the season, with exacerbation in warm weather and alleviation in cold weather. EH is histopathologically characterized by unilocular dermal cysts lined by two layers of cuboidal to flattened epithelial cells.
Skin imaging techniques such as dermoscopy and high-frequency ultrasound (HFU) have been increasingly researched and applied in the dermatology field. It has been shown that these non-invasive tools could greatly improve the diagnostic accuracy in both cutaneous tumors and non-neoplastic dermatoses.[1] However, research on the dermoscopic and ultrasonic features of EH is limited, especially in Asian patients. Therefore, we collected four histopathologically proven EH patients and analyzed their clinical, dermoscopic, and ultrasonic features to provide more information on the non-invasive diagnosis of EH.
Three females (31, 35, and 66 years old) and one male (11 years old) presented with similar chronic small, skin-colored to bluish vesicles and cystic papules on their faces. The lesions were asymptomatic and would increase in number or size in hot and humid environments. The durations of the lesions were 2 to 5 years. No treatment was applied before their presentations to our clinic. Physical examination revealed multiple translucent light-brownish to bluish papulovesicles distributed mainly on the patients’ nasal, malar, and periorbital areas, approximately 2 to 4 mm in diameter [Figure 1A]. Dermoscopic evaluation showed multiple well-defined oval bluish homogeneous areas, usually surrounded by blurry pale halos, and clustered white dots (sometimes forming rosettes) were also observed within or near the lesions [Figure 1B]. HFU (20 and 50 MHz) clearly displayed multiple anechoic cysts in the dermis, well demarcated, and occasionally accompanied by lateral acoustic shadows and posterior echogenic enhancement [Figure 1C]. All patients underwent histopathologic investigations, which revealed dermal unilocular cysts lined by cuboidal epithelial cells adjacent to normal eccrine glands, without myoepithelial cells or decapitation secretions, and immunohistochemical staining showed carcinoembryonic antigen positivity in the inner epithelial layer, confirming the diagnosis of EH [Figure 1D–F]. All patients were advised to avoid circumstances that could increase sweat production and were prescribed topical atropine, which led to an obvious decrease in or the disappearance of lesions.
Figure 1.
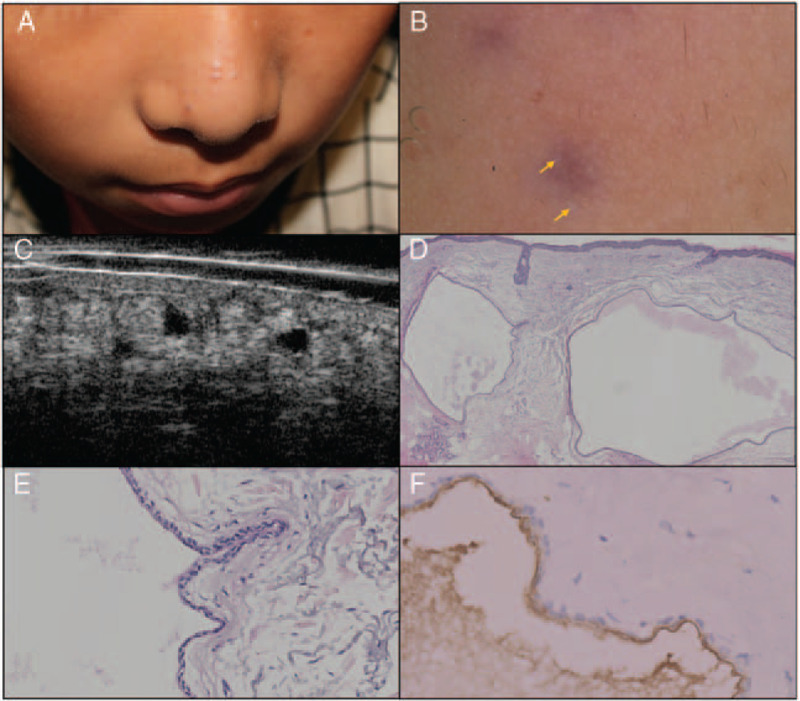
Multi-dimensional skin imaging of an eccrine hidrocystoma patient. (A) Clinical examination showed multiple bluish and skin-colored cystic papules and vesicles on the nasal and malar areas. (B) Dermoscopic evaluation revealed bluish homogeneous areas surrounded by blurred pale halos, with clustered white dots that formed a rosette on the lower part (arrows) (polarized mode; original magnification, ×40). (C) Highfrequency ultrasound at 50 MHz detected multiple well-defined anechoic cystic lesions in the dermis with posterior echogenic enhancement. (D) Histopathologic examination revealed dermal cysts containing clear fluid and few eosinophilic materials (hematoxylin-eosin staining; original magnification, ×40). (E) The cyst was well demarcated and lined by two layers of epithelial cells (hematoxylin-eosin staining; original magnification, ×200). (F) Immunohistochemical staining showed carcinoembryonic antigen positivity in the inner layer of the cyst wall (original magnification, ×400).
Many dermatoses could manifest as multiple vesicles or papules on the face. Due to cosmetic considerations, the application of skin biopsy is usually restricted. Therefore, the diagnosis of these diseases depends largely on the clinical manifestations alone. With the development of skin imaging techniques, more valuable information can be acquired non-invasively by dermatologists and contribute to the differential diagnosis process. EH is relatively rare and often misdiagnosed in clinical practice. Differential diagnosis includes eruptive vellus hair cyst, steatocystoma, syringoma, and acne comedones. Both dermoscopy and HFU can help to differentiate these conditions. Dermoscopic features of eruptive vellus hair cyst are roundish, light yellow-white structures with erythematous halos and peripheral radiating vessels. Steatocystoma under dermoscopic evaluation displays a circumscribed, yellowish, structureless area with diffuse margins. Dermoscopic evaluation of syringoma shows a central homogeneous light brownish area with a delicate pigment network at the periphery. Dermoscopic examination of acne comedones reveals skin-colored or light brown areas with a white-yellowish central pore in closed comedones, while the pore tends to be larger and brownish in open comedones. HFU of acne comedones reveals widening of the hair follicles and heterogeneous echogenicity of the surrounding dermis instead of cystic lesions.[2] Confirming the diagnosis of EH is important since EH can be easily improved by the avoidance of hot and humid environments. Dermoscopic studies in Caucasian patients have revealed that EH is characterized by a central homogeneous area, skin-colored or bluish, sometimes surrounded by a pale halo.[3,4] Our observations were consistent with those reported in the literature, but we also noticed the clustered white dots that correlated with the adnexal openings (plugged with horny materials where rosettes formed). HFU studies of EH are even more limited.[5] We applied HFU in our patients and found that HFU could easily detect the cystic nature of EH lesions, emphasizing the usefulness of HFU to exclude other non-cystic diseases. In conclusion, non-invasive skin imaging techniques such as dermoscopy and HFU can provide important information for the diagnosis and evaluation of EH, helping to lessen unnecessary skin biopsy of the facial area.
Declaration of patient consent
All patients signed written consent forms. In the consent form, each patient was informed that the dermoscopic and HFU images and clinical information might be used for research and reported in scientific publications. All the patients were aware that their names would not appear in the contents and necessary coverings would be used to ensure the concealment of identity.
Funding
This work was supported by grants from the Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (No. 2019XK320024), the National Natural Science Foundation of China (No. 61871011), the Chinese Academy of Medical Sciences (CAMS) Innovation Fund for Medical Sciences (No. 2017-I2M-3-020), the National Key Research and Development Program of China (No. 2016YFC0901500), and the Beijing Natural Science Foundation (No. 7182127).
Conflicts of interest
None.
Footnotes
How to cite this article: Wang YK, Gao YJ, Liu J, Zhu QL. Multi-dimensional skin imaging evaluation of eccrine hidrocystoma. Chin Med J 2020;133:2107–2108. doi: 10.1097/CM9.0000000000000975
References
- 1.Wang SQ, Liu J, Zhu QL, Zhao CY, Qu T, Li F, et al. High-frequency ultrasound features of basal cell carcinoma and its association with histological recurrence risk. Chin Med J 2019; 132:2021–2026.. doi: 10.1097/cm9.0000000000000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang J, Luo Y, Liu J, Zhu Q, Wang Y, Jin H. High-frequency ultrasonography and scoring of acne at 20 MHz and 50 MHz. J Eur Acad Dermatol Venereol 2020; published ahead of print. doi: 10.1111/jdv.16584. [DOI] [PubMed] [Google Scholar]
- 3.Correia O, Duarte AF, Barros AM, Rocha N. Multiple eccrine hidrocystomas--from diagnosis to treatment: the role of dermatoscopy and botulinum toxin. Dermatology 2009; 219:77–79.. doi: 10.1159/000218155. [DOI] [PubMed] [Google Scholar]
- 4.Duman N, Duman D, Sahin S. Pale halo surrounding a homogeneous bluish-purplish central area: dermoscopic clue for eccrine hidrocystoma. Dermatol Pract Concept 2015; 5:43–45.. doi: 10.5826/dpc.0504a11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chin K, Finger PT, Iacob C. High-frequency ultrasound imaging of periocular hidrocystomas. Optometry 2003; 74:760–764.. [PubMed] [Google Scholar]


