Supplemental Digital Content is available in the text
Keywords: chronic dysphagia, stroke, swallowing function, transcranial direct current stimulation
Abstract
About 11% to 13% of patients with acute dysphagia induced by stroke remain chronic dysphagia 6 months after stroke which usually leads to many severe complications and poor quality of life.
To investigate the effect of transcranial direct current stimulation (tDCS) on swallowing function in the patients with chronic dysphagia after stroke.
26 post-stroke patients with chronic dysphagia who received tDCS were identified by electronic medical records between July 2016 and April 2018. Of which, 13 were treated by unilateral hemispheric anodal tDCS at affected pharyngeal motor cortex. 13 eligible patients only treated by conventional therapies but without tDCS were randomly selected by matching on date of admission (±2 weeks) of the patients receiving unilateral tDCS. The swallowing function and quality of life were evaluated before and 2 weeks after treatment.
The patients in three groups were comparable. The swallowing function and quality of life of the patients in all the 3 groups had been improved over time. Comparing to the group without tDCS, both the groups with unilateral or bilateral tDCS had shorter oral transit time (1.69 ± 0.95, 0.97 ± 0.71 seconds, respectively) and higher scores of quality of life (159.76 ± 12.59, 179.69 ± 11.81, respectively) after treatment.
Both unilateral and bilateral hemispheric anodal tDCS combined with conventional therapies are helpful for recovery of swallowing function in patients with chronic dysphagia induced by stroke, but bilateral anodal tDCS substantially improve more.
1. Introduction
Dysphagia can be induced by a range of diseases such as oropharyngeal diseases, esophageal diseases, central nervous system diseases, neuromuscular diseases, psychosocial diseases and so on. About 50% of patients with stroke suffer dysphagia. Of which, most post-stroke patients can recover the swallowing function with routine therapies, however about 11% to 13% of post-stroke patients still remain the symptoms until 6 months after stroke.[1] The chronic dysphagia probably leads to several complications such as dehydration, malnutrition and aspiration pneumonia and and so on, which consequently result in poor quality of life.[2] Peripheral motor sensory stimulation techniques are commonly used for treating dysphagia after stroke, including tongue muscle motor stimulation, taste stimulation, cold, and heat stimulation, swallowing muscle group neuromuscular electrical stimulation and compensatory methods (eg, changes in eating position and food characteristics).[3] Recently, increasing evidence has showed that the non-invasive brain electric stimulation techniques such as repetitive transcranial magnetic stimulation and transcranial direct current stimulation (tDCS) are likely helpful for recovery in patients with stroke.[4–8] Particularly, the patients with acute, subacute or chronic dysphagia induced by stroke can achieve substantial improvement of the swallowing function after receiving tDCS.[9–13] However, the sites where the electrodes of tDCS place very in the existing studies. The knowledge regarding whether there is difference between the effect of tDCS over the unaffected, affected or both hemispheres is limited. Better recovery is suggested to be associated with anodal tDCS to affected pharyngeal motor cortex comparing to sham procedure.[11,13] In addition, a previous study found that bilateral anodal tDCS could bring additional benefit on the improvement of swallowing function in patients with post-stroke dysphagia.[9] We hypothesized that bilateral anodal tDCS probably had better recovery on swallowing function in patient with post-stroke dysphagia than unilateral anodal tDCS.
Therefore, we conducted a retrospective cohort study to evaluate whether the tDCS can improve the swallowing function of the patients with chronic dysphagia caused by stroke, and whether bilateral anodal tDCS has better effect than unilateral anodal tDCS.
2. Methods
2.1. Study population and design
The study participants were the patients with chronic dysphagia induced by stroke with unilateral cortical and subcortical lesions and received rehabilitated therapies in the Department of Neurological Rehabilitation, Rehabilitation Center Hospital of Gansu province between July 2016 and April 2018. The electronic hospitalized records with all information (eg, date of admission and discharge, diagnosis, clinical examinations and the results, therapies (including density/dose and duration), assessment of patient's condition etc) were used to identify the patients. The patients were restricted by the age from 25 to 65, the illness course of 6 to 24 months after stroke, no symptoms of consciousness disorders, cognitive disorders and aphasia, and never receiving tDCS before. Stroke with unilateral cortical and subcortical lesions was confirmed by head CT or MRI based on the diagnostic criteria for cerebral infarction and cerebral hemorrhage in American Guidelines for the Diagnosis and Treatment of Acute Ischemic Stroke (2015)[14] and American Guidelines for the Diagnosis and Treatment of Cerebral Hemorrhage (2015).[15] Dysphagia was assessed by clinical evaluation of swallowing function and swallowing X-ray fluoroscopy. Additionally, the patients with one of the conditions below would be excluded:
-
(1)
patients with cardiac pacemaker and brain stimulator,
-
(2)
patients with intracranial metal implants, such as arterial clips, cranioplasty and so on,
-
(3)
patients treated by ventriculoperitoneal shunt,
-
(4)
patients with not well-controlled epilepsy,
-
(5)
patients with local skin lesions or inflammatory reactions or irritation area hyperalgesia.
According to the patients’ conditions (eg, the infarction area, severity of dysphagia, etc), a rehabilitation therapist introduced and recommended the protocol of tDCS to the patients and relatives. An extra protocol of tDCS would be performed if the patients and relatives took the suggestion. A total of 26 eligible patients with post-stroke dysphagia accepted unilateral or bilateral hemispheric anodal tDCS during that period. Of which, 13 patients received unilateral hemispheric anodal tDCS at affected pharyngeal motor cortex. In order to evaluate the effect of tDCS on improvement of swallowing function, we further randomly selected 13 eligible patients without tDCS who were appropriate for tDCS as reference group (1:1) by matching on hospitalized date (±2 weeks) of the patients receiving unilateral hemispheric anodal tDCS.
Ethical approval for the study was obtained from the Ethics Committee at Rehabilitation Center Hospital of Gansu province (2018/03/19).
2.2. Treatment
All the patients were treated with conventional swallowing therapies (such as ice stimulation therapy, deglutition reflex trigger training, tongue control training, muscle strength training of levator muscle group of larynx, Mendelssohn method, direct feeding training, low frequency electrical stimulation for submandibular muscles). The duration and frequency of conventional swallowing therapies were 20 minutes per time, once per day, and 6 days per week for 2 weeks.
The duration and frequency of tDCS was similar as that of conventional swallowing therapies. The tDCS treatment was performed by IS300 Intelligent Electric Stimulator (Sichuan Intelligent Electronics Industry Co., Ltd.). The stimulation site was pharyngeal motor cortex, which the anodes were put at the points 2 cm forward and 15 cm beside the Cz point in the top center and the cathodes were put at the contralateral supraorbital region (Fig. 1).[9] The electrode area was 5cm×7 cm. A piece of thin cotton pad with saturated saline water was put under the electrode to make the electrode fully contact with skin. The stimulation current density was lower than 0.04 mA/cm2, and the stimulation intensity was 1.4 mA. Elastic bandage was utilized to fix the electrode.
Figure 1.
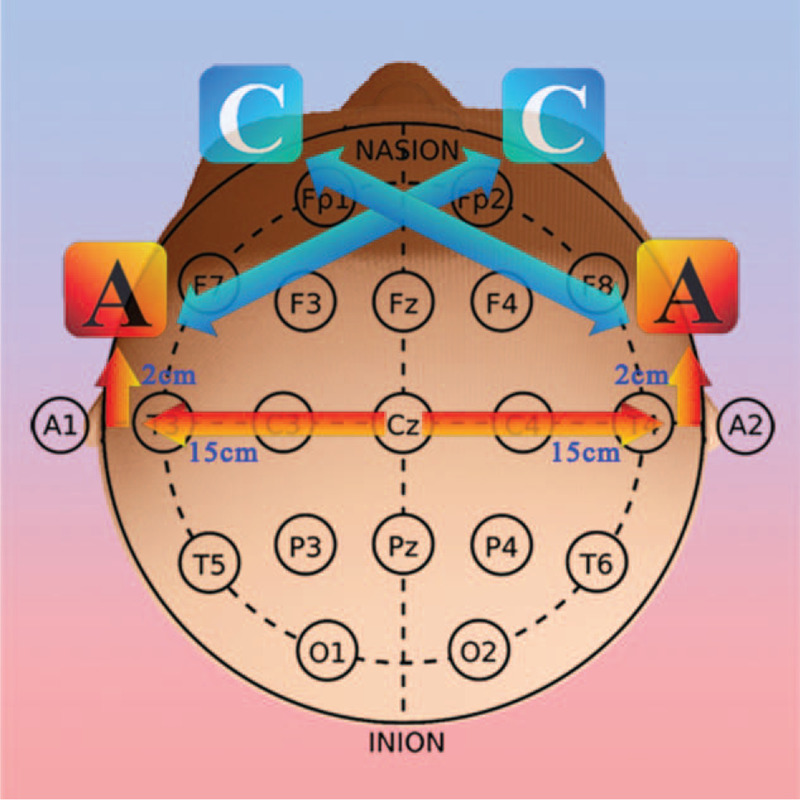
tDCS stimulation site of pharyngeal motor cortex. transcranial direct current stimulation. tDCS = transcranial direct current stimulation.
2.3. Measurement
During the stay in hospital, the videofluoroscopic swallowing examinations[16] and swallow quality of life questionnaire (SWAL-QOL) were performed for evaluating patients’ swallowing function by 2 speech therapist before and 2 weeks after treatment. The patients were asked to seat comfortably and eat the foods mixed with barium (50 ml 60% barium sulfate suspension (made by 200 grams barium powder + 286 grams water) + 1.5 grams Audi Shunyan Thickener (produced by Guangzhou Audi Biotechnology Co. Ltd.)). A radiographic video was used for observing and recording swallowing images (see video, Supplemental Video, which illustrates the procedure of swallowing). All the patients were asked to swallow 5 mL barium food per time twice. A swallowing therapist would assess the parameters below by reviewing the video at a rate of 30 frames per second.
-
(1)
Oral transit time[17]: the time from the shape of the food group started to be changed by the tongue muscle in the mouth until the head of the food group reached the junction of the mandibular branch and the tongue root.
-
(2)
Stage transition duration (STD): the time from the arrival of bolus head at the junction of the lingual and mandibular branches and the initiation of swallowing in the pharynx which was marked as the superior-anterior hyoid movement. But up and down hyoid movement would be ignored if a swallow did not occur.
-
(3)
Hyoid movement time: the interval that the hyoid bone started to move forward and upward until it returned to the resting position.
-
(4)
Upper esophageal sphincter (UES) opening time (UOT): the time from UES started to open until it fully closed after the food group arrived at UES.
-
(5)
Laryngeal closure time: the time from closure to open on the laryngeal vestibule, precisely from touching to separation between spoon cartilage and the lower surface of epiglottis.
There were 11 domains (totally 44 items) in SWAL-QOL. Of which, 8 were related to swallowing, including psychological burden, eating time, appetite, food choice, language communication, eating fear, mental health and social interaction; 2 were general domains which were about fatigue and sleep; and 1 was frequency of dysphagia. A 5-point Likert scale was used ranging from 1 = “severely impaired quality of life” to 5 = “no impairment”.
2.4. Statistical analysis
Shapiro-Wilk test was used for testing normal distribution of the data on parameters of swallowing function. Paired-samples T test and independent-samples T test were used to test the differences of swallowing function before and after treatment in the same group, and of swallowing function after treatment between the 2 groups separately. One-way analysis of variance was applied to assess the difference of swallowing function across the 3 groups. The data analysis was performed by SPSS18.0 software.
3. Results
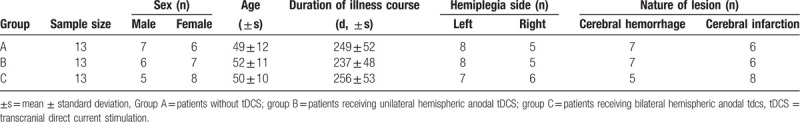
The average age of the patients in each group ranged from 49 to 52 years old. All the patients had almost suffered post-stroke dysphagia for an average of 8 months. Meanwhiles, gender, affected hemispheric and types of lesion were equal within each group (Table 1).
Table 1.
Characteristics of the patients in the 3 groups.
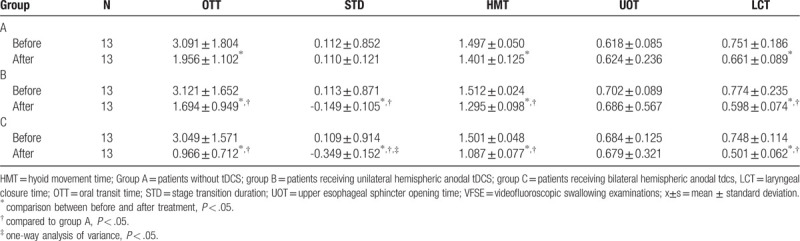
There was no difference on swallowing function and quality of life across the 3 groups before treatment. Two weeks after the treatments were finished, the swallowing functions of all the patients in three groups were improved except for UOT and STD in patients without tDCS (Table 2). Compared to the patients without tDCS, all the swallowing functions after treatment but not UOT in the patients with unilateral and bilateral hemispheric tDCS were substantially recovered to some extent after treatment. However, we only found that there was difference on STD after treatment across the groups which the patients with bilateral hemispheric tDCS got largest reduction on STD, followed by the patients received unilateral hemispheric tDCS (Table 2).
Table 2.
The swallowing function assessed by VFSE before and after treatment in the 3 groups (±s).
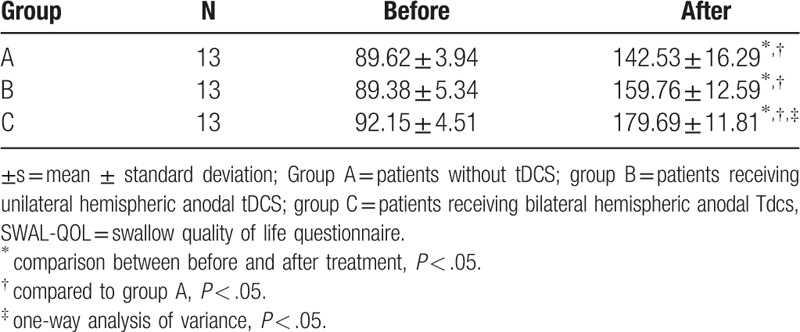
Regarding to the quality of life, the SWAL-QOL score was substantially increased in three groups over time (Table 3). The quality of life after treatment between groups was apparently different, which the quality of life had been sharply improved with largest score in the patients received bilateral hemispheric tDCS followed by the patients with unilateral hemispheric tDCS.
Table 3.
The swallow quality of life assessed by SWAL-QOL before and after treatment in the 3 groups (±s).
4. Discussion
The swallowing functions (not UES opening duration) and quality of life in post-stroke patients with chronic dysphagia were improved after 2-week treatment of conventional therapies combining with or without tDCS. Both unilateral and bilateral hemispheric anodal tDCS could bring extra reduction on the STD and improvement on the swallow quality of life, but bilateral hemispheric tDCS did more than unilateral hemispheric tDCS.
To our knowledge, this is the first study to investigate the difference of the effect of tDCS at differing sites on the swallowing function in patients with chronic dysphagia induced by stroke. Out findings corroborate the results of the previous studies[8,9,12] evaluating the effect of tDCS for post-stroke dysphagia which tDCS can improve the swallowing function in patients with dysphagia induced by stroke. However, there is only single comparison between sham procedure and unilateral hemispheric anodal tDCS over the pharyngeal motor cortex of the ipsilesional or affected hemisphere, or bilateral hemispheric anodal tDCS in each single previous study. Those studies have suggested whichever the anodal electrodes were placed at ipsilesional, affected or both sides, higher improvement on swallowing function was obtained in the tDCS groups comparing to conventional therapy.[9,11,13] We found the similar evidence in the present study. Additionally, we still observed that the patients receiving bilateral tDCS had better recovery on swallowing function than those who only received anodal tDCS at the affected side. Hamdy et al found that the unaffected hemisphere could compensate the cortical activity of the contralesional hemisphere for swallowing function.[18] Thus, there is higher cortical excitability for swallowing function by stimulating both affected and unaffected sides than that by affected side only. Because bilateral pharyngeal motor cortex anodal tDCS not only improve the recovery of swallowing function of the affected pharyngeal motor cortex, but also strengthen the swallowing function of the unaffected pharyngeal motor cortex.
There were still several limitations in our study. First, we did have the long-term follow-up data after discharge. However, the study participants in our study were those who had had dysphagia for more than six months, which the influence of spontaneous recovery of swallowing function is eliminated. Second, we did not have big sample to investigated whether the effect of tDCS on dysphagia differing by sex, age and length of disease course. Thus, the group which may gain greater benefit from the treatment of tDCS couldn’t be pointed out. Further study with larger sample and longer follow-up is necessary to confirm our findings.
5. Conclusion
Both unilateral and bilateral hemispheric anodal tDCS combined with conventional therapies are helpful for recovery of swallowing function in patients with chronic dysphagia induced by stroke, but bilateral anodal tDCS substantially improve more. If confirmed in the future studies, the findings may be informative for the treatment of post-stroke chronic dysphagia.
Author contributions
YL and HF contributed to conception and design of this study. YL, JL, HW, NC and JY contributed to the acquisition, analysis, or interpretation of the study. YL and HF drafted the manuscript. All the authors critically revised the manuscript and gave final approval to the final article.
Supplementary Material
Footnotes
Abbreviations: STD = stage transition duration, SWAL-QOL = swallow quality of life questionnaire, tDCS = transcranial direct current stimulation, UES = upper esophageal sphincter, UOT = upper esophageal sphincter opening time, VFSE = videofluoroscopic swallowing examinations.
How to cite this article: Li Y, Feng H, Li J, Wang H, Chen N, Yang J. The effect of transcranial direct current stimulation of pharyngeal motor cortex on swallowing function in patients with chronic dysphagia after stroke: A retrospective cohort study. Medicine. 2020;99:10(e19121).
The authors have no conflicts of interest to disclose.
This study was funded by Lanzhou Personnel Innovation and Entrepreneurship program (2019-RC-40). The sponsor didn’t play any role on study design, data analysis and publication.
Supplemental Digital Content is available for this article.
References
- [1].Martino R, Foley N, Bhogal S, et al. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 2005;36:2756–63. [DOI] [PubMed] [Google Scholar]
- [2].Gonzalez-Fernandez M, Ottenstein L, Atanelov L, et al. Dysphagia after Stroke: an Overview. Curr Phys Med Rehabil Rep 2013;1:187–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Bulow M, Speyer R, Baijens L, et al. Neuromuscular electrical stimulation (NMES) in stroke patients with oral and pharyngeal dysfunction. Dysphagia 2008;23:302–9. [DOI] [PubMed] [Google Scholar]
- [4].Kubis N. Non-Invasive brain stimulation to enhance post-stroke recovery. Front Neural Circuits 2016;10:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Schlaug G, Renga V, Nair D. Transcranial direct current stimulation in stroke recovery. Arch Neurol 2008;65:1571–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Gomez Palacio Schjetnan A, Faraji J, Metz GA, et al. Transcranial direct current stimulation in stroke rehabilitation: a review of recent advancements. Stroke Res Treat 2013;2013:170256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Baker JM, Rorden C, Fridriksson J. Using transcranial direct-current stimulation to treat stroke patients with aphasia. Stroke 2010;41:1229–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ghandehari K, Erfani M, Kiadarbandsari E, et al. Transcranial direct current stimulation in post-stroke dysphagia: a systematic review of randomized controlled trials. Rev Clin Med 2016;3:117–21. [Google Scholar]
- [9].Ahn YH, Sohn HJ, Park JS, et al. Effect of bihemispheric anodal transcranial direct current stimulation for dysphagia in chronic stroke patients: a randomized clinical trial. J Rehabil Med 2017;49:30–5. [DOI] [PubMed] [Google Scholar]
- [10].Pisegna JM, Kaneoka A, Pearson WG, Jr, et al. Effects of non-invasive brain stimulation on post-stroke dysphagia: a systematic review and meta-analysis of randomized controlled trials. Clin Neurophysiol 2016;127:956–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Yang EJ, Baek SR, Shin J, et al. Effects of transcranial direct current stimulation (tDCS) on post-stroke dysphagia. Restor Neurol Neurosci 2012;30:303–11. [DOI] [PubMed] [Google Scholar]
- [12].Suntrup-Krueger S, Ringmaier C, Muhle P, et al. Randomized trial of transcranial direct current stimulation for poststroke dysphagia. Ann Neurol 2018;83:328–40. [DOI] [PubMed] [Google Scholar]
- [13].Shigematsu T, Fujishima I, Ohno K. Transcranial direct current stimulation improves swallowing function in stroke patients. Neurorehabil Neural Repair 2013;27:363–9. [DOI] [PubMed] [Google Scholar]
- [14].Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014;45:2160–236. [DOI] [PubMed] [Google Scholar]
- [15].Hemphill JC, 3rd, Greenberg SM, Anderson CS, et al. Guidelines for the management of sontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2015;46:2032–60. [DOI] [PubMed] [Google Scholar]
- [16].Palmer JB, Drennan JC, Baba M. Evaluation and treatment of swallowing impairments. Am Fam Physician 2000;61:2453–62. [PubMed] [Google Scholar]
- [17].Soares TJ, Moraes DP, de Medeiros GC, et al. Oral transit time: a critical review of the literature. Arq Bras Cir Dig 2015;28:144–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Hamdy S, Aziz Q, Rothwell JC, et al. Recovery of swallowing after dysphagic stroke relates to functional reorganization in the intact motor cortex. Gastroenterology 1998;115:1104–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


