Abstract
The objective of the study was to characterize self-reported oral hygiene practices among Mexican older adults aged ≥60 years, and to measure the association between frequency of tooth brushing and a set of sociodemographic, socioeconomic, and dental variables.
We conducted a cross-sectional study of 139 older adults aged ≥60 years in Pachuca, Mexico. A questionnaire and a clinical dental examination were administered to identify specific variables. We determined frequency of tooth brushing (or cleaning of dentures or prostheses) and use of toothpaste, mouthwash, and dental floss among respondents. Non-parametric testing was performed for statistical analysis and a multivariate logistic regression model was generated with Stata 11 software to determine frequency of tooth brushing.
In our study sample, 53.2% of participants reported brushing their teeth at least once a day, 50.4% always using toothpaste, 16.5% using mouthwash and 3.6% using floss for their oral hygiene. In general, younger and female respondents used oral hygiene aids more than the others. Our multivariate model yielded an association (P < .05) between tooth brushing at least once daily and the following variables: having functional dentition (OR = 12.60), lacking health insurance (OR = 3.72), being retired/pensioned (OR = 4.50), and suffering from a chronic disease (OR = 0.43).
The older adults in our sample exhibited deficient oral hygiene behaviors. The results suggest certain socioeconomic inequalities in oral health. The findings of this study should be considered when designing dental care instructions for older adults.
Keywords: older adults, oral health, oral hygiene, tooth brushing
1. Introduction
Population aging represents a passage from high to low and controlled levels of mortality and birth patterns. This shift has caused progressive aging and an increase in the size of the global population.[1] With the elderly expanding more rapidly than other age groups, the phenomenon of an aging population has become one of the major challenges facing Mexico today and will acquire even greater relevance in the forthcoming decades. Older adults aged ≥65 years are expected to reach 22.5% of the population by 2050, up from 3.7% in 1970. Because one of the predominant challenges of aging relates to health, and diseases distinctive of old age require specialized medical care entailing high costs.[2,3]
The mouth does not escape the impact of aging. Poor oral health is an important public health problem affecting both children and adults worldwide. Noted for their progressive and cumulative effects, oral diseases become increasingly complicated over time. Older adults thus tend to experience highly prevalent oral conditions—for example, root caries, periodontal diseases, tooth loss, edentulism, xerostomia, and oral mucosal lesions—necessitating considerable health care.[4] From a social perspective, non-biological factors such as behavior and habits play a central role in oral health promotion, disease prevention, and successful treatments. Understanding oral diseases and improving the oral health of individuals require comprehension of the mechanisms underlying their associated behaviors and attitudes. This knowledge can help dental professionals guide individuals and groups in a healthy direction. Among the key behaviors affecting oral health are those related to oral hygiene practices.[5,6]
Oral health practices involving the self-reported frequency of tooth brushing with toothpaste and the use of oral hygiene aids such as dental floss and mouthwash represent tools for preventing oral diseases by reducing or removing dentobacterial plaque. Plaque can be removed by mechanic means such as a toothbrush and floss, coupled with chemical means such as toothpaste and mouthwash. Research on oral hygiene has focused mostly on frequency of tooth brushing, bypassing oral hygiene aids that can contribute to improving the control of dentobacterial plaque.[7,8] Oral hygiene is a relevant topic for oral public health. Specifically, toothbrushing is one of the public health actions that is recommended by national and international organizations to preserve and maintain oral health at all ages. In Mexico, the frequency of tooth brushing and the use of oral hygiene aids have been explored exclusively in children and adolescents.[8] No record exists of any such studies having been conducted on Mexican older adults. The prevalence rates of tooth brushing identified in other countries vary enormously, between 3% and 82%.[9,10] Considering the dearth of information on the Mexican elderly, we undertook this study with the twofold purpose of characterizing self-reported oral hygiene practices among Mexican older adults aged ≥60 years and measuring the association of tooth brushing frequency with sociodemographic, socioeconomic, and dental variables.
2. Materials and methods
2.1. Study design and sample
Using an observational and cross-sectional approach, we measured a set of oral health indicators in two groups of older adults aged ≥60 years in the city of Pachuca, Mexico: one residing in two nursing homes, and the other attending the “Looking for a Friend” club of retired pensioners from the Institute of Social Security and Services for Government Workers (ISSSTE by its Spanish initials). Former employees of institutions pertaining to the Teachers’ Union gathered to engage in recreational, cultural, and leisure activities 3 days a week. Our methodology has been partially described elsewhere.[11–15] During recruitment, we informed potential participants of the objectives of our research and of the confidential manner in which their data would be handled. We also explained that they would be free to leave the study at any time. Inclusion criteria involved
-
1.
being ≥60 years old,
-
2.
providing consent for participation, and
-
3.
belonging to one of the above-mentioned groups of older adults.
Exclusion criteria involved
-
1.
suffering from a hearing or language impairment that could hinder the interview and
-
2.
experiencing a physical disability that would render it impossible to administer the clinical dental examination.
No random sampling was performed: respondents were volunteers who had agreed to participate in the study. The initial total study population came to 151 apparently healthy individuals; however, 12 declined our invitation or failed to fulfill the inclusion criteria, leaving a final population of 139 respondents for analysis.
2.2. Variables and data collection
We administered a questionnaire (face to face) to collect data on our independent variables: sociodemographic characteristics including age, sex, and marital status; socioeconomic characteristics including type of nursing home, health insurance, educational level, and access to pension/retirement benefits; and health status, specifically the presence of a chronic disease (as diabetes, hypertension, cardiovascular diseases, etc). As dependent variables, we determined self-reported oral hygiene practices including frequency of tooth brushing (or cleaning of dentures or prostheses) and use of toothpaste, mouthwash, or dental floss.
Participants underwent a clinical dental examination intended to determine the number of missing teeth and presence or absence of functional dentition. The results of the examination were characterized as follows: 0 = participants with <21 teeth in their mouths and 1 = participants with 21 or more teeth in their mouths, excluding prostheses.[16–18] The dental examination was administered by only one examiner, with participants comfortably seated in an artificially lit room. Trained and standardized in our study criteria, the examiner employed a flat dental mirror and a WHO-type periodontal probe for his work. We constructed a multivariate model to identify the frequency of tooth brushing in our sample and characterized the results as follows: 0 = less than once a day and 2 = at least once a day.
2.3. Data analysis
Data were analyzed using Stata 11 software (STATA Corp, College Station, TX). We performed a univariate analysis to obtain measures of central tendency and dispersion for the continuous variables and frequencies and percentages for the categorical variables. We also performed a bivariate analysis based on the chi-square, Kruskall–Wallis and Fisher's exact non-parametric tests. For our multivariate analysis, we developed a binary logistic regression model. The strength of association between the dependent and independent variables was expressed as an odds ratio (OR) with 95% confidence interval (CI 95%). A variance inflation factor test was applied to analyze and, where pertinent, avoid multicollinearity among the independent variables. To construct the model, we considered the variables with a P < .25 value in the bivariate analysis. We adjusted this model globally through the Hosmer-Lemeshow goodness-of-fit test[19] and adjusted the final model for age and sex.
2.4. Ethical considerations
This study was conducted in conformity with the General Health Law for Health Research and the Declaration of Helsinki for research involving human subjects. All participants signed a written informed consent. The study protocol was approved by the Ethics Committee of the Postgraduate and Research Unit of the Academic Area of Dentistry at the Health Sciences Institute of the Autonomous University of the State of Hidalgo.
3. Results
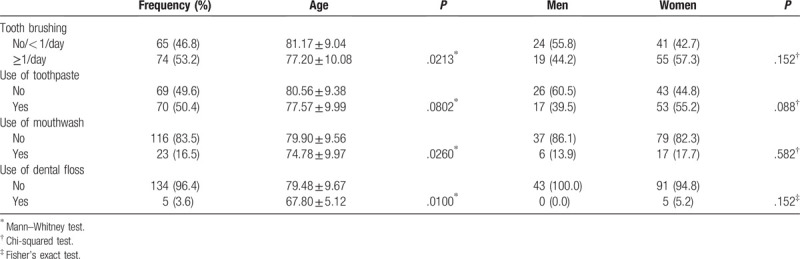
Descriptive results are shown in Table 1. The average age of participants was 79.06 ± 9.78, and 69.1% were women. The average number of missing teeth was 20.02 ± 8.61 (median 24). Table 2 shows the results regarding oral hygiene practices. In our sample, 53.2% reported brushing their teeth at least once a day, 50.4% using toothpaste, 16.5% using mouthwash and 3.6% using dental floss of the participants who reported brushing their teeth, 94.6% stated that they always used toothpaste (Fisher's exact < 0.001). Distribution results regarding oral hygiene practices showed that frequency of tooth brushing (P < .05) as well as the use of toothpaste (P < .10), mouthwash (P < .05) and dental floss (P < .05) differed by age; in general, younger people made greater use of oral hygiene aids. Women used such aids more frequently, but these differences were insignificant.
Table 1.
Univariate analysis of the characteristics of study participants.
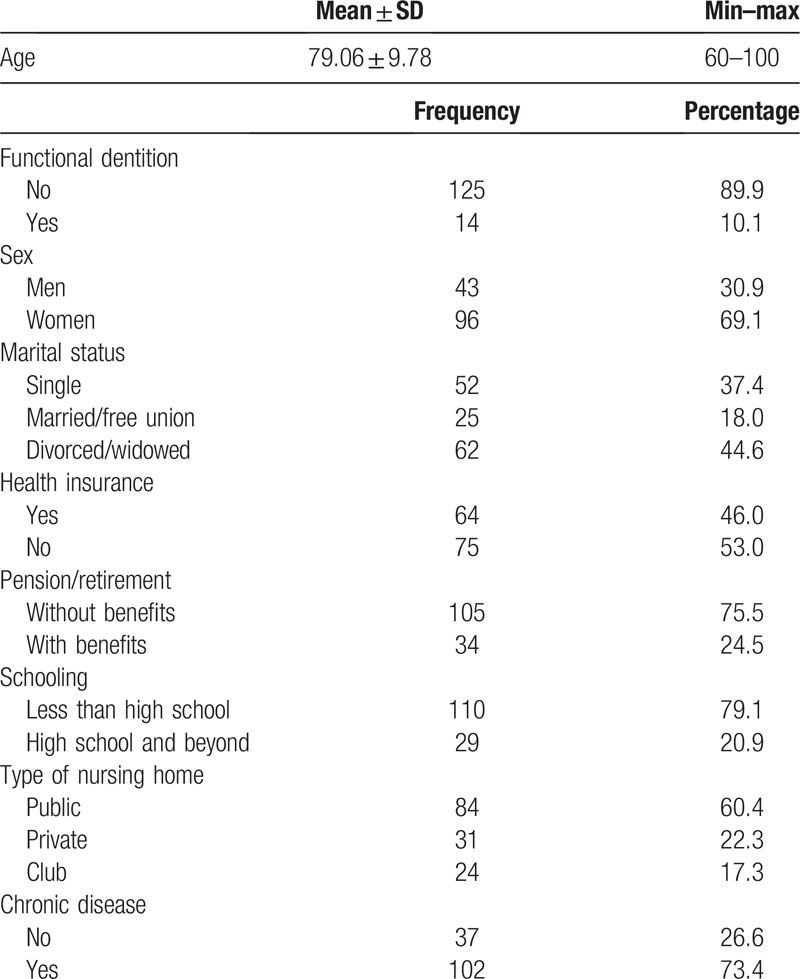
Table 2.
Use of oral hygiene aids: prevalence and distribution among study participants by age and sex.
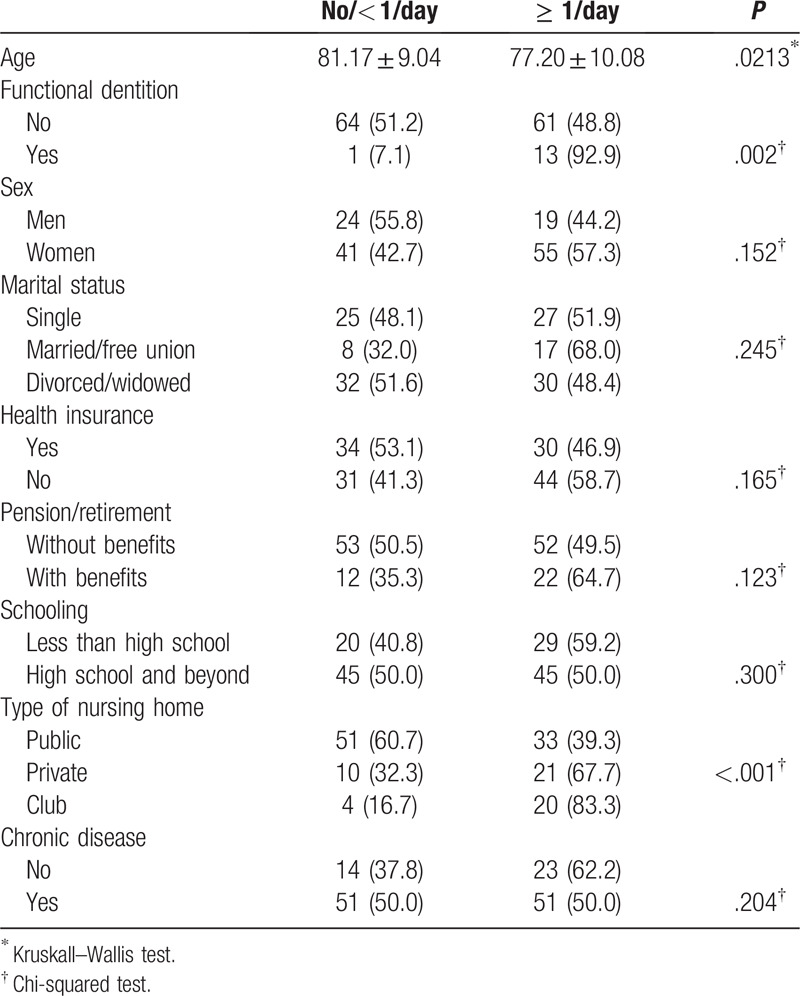
As illustrated in Table 3, the results from the bivariate analysis of tooth brushing frequency indicated that younger participants, those with functional dentition, and those in the private nursing home and the adult day club brushed their teeth more frequently. The remaining variables showed no association.
Table 3.
Bivariate analysis: association between tooth brushing and participant characteristics.
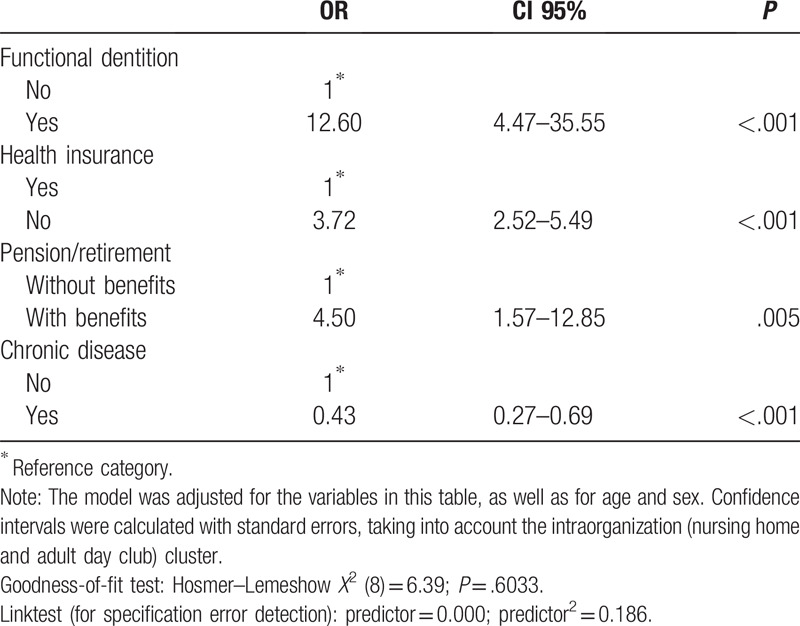
The multivariate model (Table 4) indicated that the following were the characteristics of participants who demonstrated an increased likelihood of brushing their teeth at least once a day: having functional dentition (OR = 12.60; CI 95% = 4.47–35.55), lacking health insurance (OR = 3.72; CI 95% = 2.52–5.49), and being pensioned/retired (OR = 4.50; CI 95% = 1.57–12.85); meanwhile, suffering from a chronic disease diminished the likelihood of tooth brushing at least once a day (OR = 0.43; CI 95% = 0.27–0.69).
Table 4.
Multivariate analysis: association between tooth brushing and participant characteristics.
4. Discussion
Study results showed that tooth brushing was the oral hygiene practice most frequently employed by the older adults in our sample, although the observed percentage was low compared to the general population and other, younger groups.[10,20] In general, oral health—and particularly oral hygiene practices—among older adults have been little studied, thus limiting comparisons with other research initiatives. A Hong Kong study of older adults—59 with dementia and 59 apparently healthy—indicated that the frequency of tooth brushing was 5% and 31%, respectively.[9] Meanwhile, a study in Nigeria reported a tooth brushing prevalence of 82% among ≥60-year-old participants.[10] The discrepancy among studies may be attributable to differing methodologies, study populations or case definitions. Tooth brushing is the principal method of self-care for preventing the most common oral diseases. Consequently, is a universally accepted recommendation for maintaining good dental and periodontal health among all age groups.[20,21] Nonetheless, it has been shown that tooth brushing alone is not sufficient for eliminating interproximal plaque; additional techniques such as the use of dental floss, rubber points and interdental brushes are recommended.[22]
Tooth brushing is beneficial for oral health preservation among adults, since it produces pressure, stretching and mechanical vibratory stimulation of the tongue, periodontal ligament (through pressure on the teeth), gums and palate. Therefore, it has been assumed that tooth brushing modulates the salivary flow rate and thus favors maintaining oral equilibrium among older people.[23] In turn, this leads to a reduction in caries and periodontal disease, as well as preventing tooth loss. Studies among older adults have found that the rate of tooth brushing diminishes with the loss of natural teeth.[24] The present study, which found that the frequency of tooth brushing was greater among those with functional dentition (21 or more teeth), confirms these findings. As older adults lose teeth they also lose interest in caring for their remaining teeth. They begin to abandon the “role of suffering from a disease” and, consequently, submit themselves to an even greater deterioration in their oral health. Some never even assume this role given the low mortality rate associated with oral diseases.[25]
As the population ages, patients having two or more illnesses cease to be the exception, becoming almost the rule. The term comorbidity has been coined to designate this condition.[26] Oral diseases also coexist with chronic diseases. Various studies have shown an association between tooth brushing and a reduced risk of chronic diseases.[27–31] A number of theories have posited that various aspects of lifestyle behavior are interrelated. The relationship between systemic diseases and self-care activities favoring oral health and hygiene may thus be influenced by other lifestyle behaviors.[27] Our study found that people suffering from a systemic disease reduced the frequency of tooth brushing. Therefore, from a public health perspective, improving tooth brushing habits is conducive not only to preventing the most generalized dental diseases, but also, and more importantly, to reducing common risk factors for the principal non-communicable diseases.[20] It has been reported that the intraoral environment affects intestinal microbiota and may cause systemic inflammation.[24]
In recent decades, it has been established that oral health among the general population varies according to social determinants. Different approaches have been used to measure oral health, with subjective and objective variables yielding varying results. However, overall, research has revealed the existence of an oral health gradient differing according to socioeconomic position.[6,32,33] It has been recognized that socioeconomic conditions are related to healthy behavior. Similarly, our study demonstrated that having health insurance and a pension were associated with the frequency of tooth brushing[10]; however, these associations were in contrast with each another: We had anticipated that having health insurance (additional resources) would be associated with an increase in the frequency of tooth brushing, as was the case for participants having pension/retirement benefits (a better socioeconomic position). Nonetheless, contrary to expectations, having health insurance correlated with a lower frequency of brushing. The importance of socioeconomic position as regards the magnitude of inequality needs to be explored in order to adequately plan and evaluate public health interventions, as well as to reduce the impact of socioeconomic position on oral health.
Our study has limitations which must be taken into account in order to properly interpret the results. The most important limitation concerns our cross-sectional design, which may present problems of temporal ambiguity, with the result that associations cannot be regarded as causally related. Another limitation that must be considered when generalizing results is that our sample consisted primarily of isolated individuals. On the other hand, the type of sampling (non-probabilistic) could introduce some type of bias (selection bias). Thus, the conditions in which they lived and their behavior as regards oral hygiene may differ from those of the general population. Also, being data collected using questionnaires, the data given by the participants may be inaccurate and subject to bias.
5. Conclusions
The older adults in our study exhibited poor oral hygiene practices. The results suggest certain socioeconomic inequalities in oral health. Our findings should be taken into account in the design of dental care instructions for older adults. We have seen from other studies that this population group does not generally receive instruction in oral hygiene for caring for their natural teeth or dentures. Interventions are therefore urgently needed among this age group in order to improve their oral health conditions. Maintaining optimal oral health is a challenge for those caring for elderly institutionalized persons. Aging of the population inevitably leads to a greater number of dependent elderly persons.[34,35]
Author contributions
Horacio Islas-Granillo, Juan Fernando Casanova-Rosado, Rubén de la Rosa-Santillana, José de Jesús Navarrete-Hernández, and Carlo Eduardo Medina-Solís were involved in the design study, analyzed the data, and wrote the first draft of the manuscript. Alejandro José Casanova-Rosado, Rosalina Islas-Zarazúa, María de Lourdes Márquez-Corona, Vicente Rueda-Ibarra, and Sandra Isabel Jiménez-Gayosso, were involved in the conception of the paper, analysis, and interpretation of the results. All authors discussed the methods, summaries, analyses, and results in the study and were involved in the writing of this paper. All the authors were involved in the critical review and made intellectual contributions, and they also accepted the final version.
Footnotes
Abbreviations: 95% CI = 95% confidence intervals, NA = not available, OR = odds ratio, SD = standard deviation.
How to cite this article: Islas-Granillo H, Casanova-Rosado JF, de la Rosa-Santillana R, Casanova-Rosado AJ, Islas-Zarazúa R, Márquez-Corona Md, Rueda-Ibarra V, Jiménez-Gayosso SI, Navarrete-Hernández Jd, Medina-Solís CE. Self-reported oral hygiene practices with emphasis on frequency of tooth brushing: A cross-sectional study of Mexican older adults aged 60 years or above. Medicine. 2020;99:36(e21622).
Publication supported by the Ministry of Education, Mexican Federal Government, through of The Faculty Development Program (PRODEP) and the Program to Strengthen Educational Excellence (PROFEXCE).
Data availability statement: Data is available on request from the authors.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the present study are available from the corresponding author on reasonable request.
References
- [1].Montoya-Arce J, Montes de Oca-Vargas H. Population aging in the State of Mexico: current situation and future perspectives. Pap Poblac 2006;12:117–46.. [Google Scholar]
- [2].Consejo Nacional de Población Diagnóstico socio-demográfico del envejecimiento en México. Serie Documentos Técnicos. México DF: CONAPO; 2011. [Google Scholar]
- [3].Mendoza-Núñez VM, González-Mantilla F, Correa-Muñoz E, et al. Relationship between social support networks and physical functioning in older community-dwelling Mexicans. Int J Environ Res Public Health 2017;14:993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Castrejón-Pérez JC. Salud bucal en los adultos mayores y su impacto en la calidad de vida. Mexico City: Instituto Nacional de Geriatría; 2010. [Google Scholar]
- [5].Lindmark U, Hakeberg M, Hugoson A. Sense of coherence and its relationship with oral health-related behaviour and knowledge of and attitudes towards oral health. Community Dent Oral Epidemiol 2011;39:542–53.. [DOI] [PubMed] [Google Scholar]
- [6].Shin HS. Social gradients in oral health status in Korea population. Arch Oral Biol 2018;95:89–94.. [DOI] [PubMed] [Google Scholar]
- [7].Zanatta FB, Antoniazzi RP, Pinto TMP, et al. Supragingival plaque removal with and without dentifrice: a randomized controlled clinical trial. Braz Dent J 2012;23:235–40.. [DOI] [PubMed] [Google Scholar]
- [8].Hernández-Martínez CT, Medina-Solís CE, Robles-Bermeo NL, et al. Oral hygiene customs in 6-12 year old schoolchildren. Rev Invest Clin 2014;66:157–63.. [PubMed] [Google Scholar]
- [9].Chu CH, Ng A, Chau AM, et al. Oral health status of elderly Chinese with dementia in Hong Kong. Oral Health Prev Dent 2015;13:51–7.. [DOI] [PubMed] [Google Scholar]
- [10].Olusile AO, Adeniyi AA, Orebanjo O. Self-rated oral health status, oral health service utilization, and oral hygiene practices among adult Nigerians. BMC Oral Health 2014;14:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Islas-Granillo H, Borges-Yañez SA, Medina-Solís CE, et al. Tooth loss experience and associated variables among adult Mexicans 60 years and older. P R Health Sci J 2016;35:88–92.. [PubMed] [Google Scholar]
- [12].Islas-Granillo H, Borges-Yáñez A, Fernández-Barrera MÁ, et al. Relationship of hyposalivation and xerostomia in Mexican elderly with socioeconomic, sociodemographic and dental factors. Sci Rep 2017;7:40686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Islas-Granillo H, Borges-Yañez SA, Medina-Solís CE, et al. Dental prosthetic treatment needs in Mexican elders: Influence of socioeconomic position. Dent Med Probl 2017;54:383–7.. [Google Scholar]
- [14].Islas-Granillo H, Medina-Solís CE, Márquez-Corona ML, et al. Prevalence of multimorbidity in institutionalized subjects aged 60 and over in a developing country. Clin Interv Aging 2018;13:1129–33.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Islas-Granillo H, Borges-Yañez SA, Navarrete-Hernández JJ, et al. Indicators of oral health in older adults with and without the presence of multimorbidity: a cross-sectional study. Clin Interv Aging 2019;14:219–24.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hobdell M, Petersen PE, Clarkson J, et al. Global goals for oral health 2020. Int Dent J 2003;53:285–8.. [DOI] [PubMed] [Google Scholar]
- [17].Ervin RB, Dye BA. The effect of functional dentition on Healthy Eating Index scores and nutrient intakes in a nationally representative sample of older adults. J Public Health Dent 2009;69:207–16.. [DOI] [PubMed] [Google Scholar]
- [18].Ribeiro CG, Cascaes AM, Silva AE, et al. Edentulism, severe tooth loss and lack of functional dentition in elders: a study in Southern Brazil. Braz Dent J 2016;27:345–52.. [DOI] [PubMed] [Google Scholar]
- [19].Bagley SC, White H, Golomb BA. Logistic regression in the medical literature: standards for use and reporting, with particular attention to one medical domain. J Clin Epidemiol 2001;54:979–85.. [DOI] [PubMed] [Google Scholar]
- [20].Honkala S, Vereecken C, Niclasen B, et al. Trends in toothbrushing in 20 countries/regions from 1994 to 2010. Eur J Public Health 2015;25: Suppl 2: 20–3.. [DOI] [PubMed] [Google Scholar]
- [21].Rothen M, Cunha-Cruz J, Zhou L, et al. Northwest PRECEDENT network. Oral hygiene behaviors and caries experience in Northwest PRECEDENT patients. Community Dent Oral Epidemiol 2014;42:526–35.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Warren PR, Chater BV. An overview of established interdental cleaning methods. J Clin Dent 1996;7:65–9.. [PubMed] [Google Scholar]
- [23].Affoo RH, Trottier K, Garrick R, et al. The effects of tooth brushing on whole salivary flow rate in older adults. Biomed Res Int 2018;2018:3904139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Bando S, Tomata Y, Aida J, et al. Impact of oral self-care on incident functional disability in elderly Japanese: the Ohsaki Cohort 2006 study. BMJ Open 2017;7:e017946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Reisine ST. Theoretical considerations in formulating sociodental indicators. Soc Sci Med A 1981;15:745–50.. [DOI] [PubMed] [Google Scholar]
- [26].Lifshitz A. Sobre la asociación de enfermedades. Gac Med Mex 2015;151:149. [PubMed] [Google Scholar]
- [27].Tsutsumi C, Kakuma T. Regular toothbrushing is associated with a decreased risk of metabolic syndrome according to a medical check-up database. Kurume Med J 2015;61:43–52.. [DOI] [PubMed] [Google Scholar]
- [28].Sato F, Oze I, Kawakita D, et al. Inverse association between toothbrushing and upper aerodigestive tract cancer risk in a Japanese population. Head Neck 2011;33:1628–37.. [DOI] [PubMed] [Google Scholar]
- [29].Huang J, He B1, Chen F, et al. Association between oral hygiene, chronic diseases, and oral squamous cell carcinoma. Zhonghua Yu Fang Yi Xue Za Zhi 2015;49:688–92.. [PubMed] [Google Scholar]
- [30].Matsui S, Kajikawa M, Maruhashi T, et al. Decreased frequency and duration of toothbrushing is a risk factor for endothelial dysfunction. Int J Cardiol 2017;241:30–4.. [DOI] [PubMed] [Google Scholar]
- [31].Kuwabara M, Motoki Y, Sato H, et al. Low frequency of toothbrushing practices is an independent risk factor for diabetes mellitus in male and dyslipidemia in female: a large-scale, 5-year cohort study in Japan. J Cardiol 2017;70:107–12.. [DOI] [PubMed] [Google Scholar]
- [32].Hakeberg M, Wide Boman U. Self-reported oral and general health in relation to socioeconomic position. BMC Public Health 2017;18:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Heredia-Ponce E, Irigoyen-Camacho AE, Sánchez-García S. Oral health status of institutionalized older women from different socioeconomic positions. J Health Care Poor Underserved 2017;28:1462–76.. [DOI] [PubMed] [Google Scholar]
- [34].Osmari D, Fraga S, Braun KO, et al. Behaviour of the elderly with regard to hygiene procedures for and maintenance of removable dentures. Oral Health Prev Dent 2016;14:21–6.. [DOI] [PubMed] [Google Scholar]
- [35].Maille G, Saliba-Serre B, Ferrandez AM, et al. Objective and perceived oral health status of elderly nursing home residents: a local survey in southern France. Clin Interv Aging 2019;14:1141–51.. [DOI] [PMC free article] [PubMed] [Google Scholar]


