Abstract
Few studies on the individual and combined analysis between serum uric acid (SUA) and body mass index (BMI) and blood pressure (BP) were conducted in individuals aged ≥45 years. We aimed to assess the extent to which BMI and SUA and their interaction affect BP in Chinese middle-aged and older adults.
Data were selected from the China Health and Retirement Longitudinal Study (CHARLS). A total of 5888 individuals aged 45 to 96 was included. Differences between BMI, or between categories of blood pressure were evaluated by t test or chi-square test. The trend of related variables according to four BMI categories was also tested using contrast analysis. The adjusted associations between various characteristics and BP status were first compared using linear regression models, as appropriate. Then, general linear models adjusting for related potential confounders were used to examine the synergistic effect of SUA and BMI level on BP for middle-aged and elderly individuals in China.
Age-adjusted partial Pearson correlation coefficient showed that BMI was significantly and positively correlated with BP both in male and female, SUA positively correlated with both systolic blood pressure (SBP) and diastolic blood pressure (DBP) in males with BMI <24.0 kg/m2 and females with BMI <24.0 kg/m2. However, SUA level significantly and positively correlated with DBP, but not with SBP, in females with BMI ≥24.0 kg/m2. Multiple linear regression analysis showed that BMI was independently associated with BP both in male and female, SUA significantly and positively associated with SBP in both males and females with BMI <24.0 kg/m2, However, SUA level positively correlated with DBP in females with BMI <24.0 kg/m2, but not with males with BMI <24.0 kg/m2, independent of other confounding factors. A general linear model analysis adjusted for confounding factors did not reveal interaction between BMI, SUA levels and SBP (β=-1.404, P = .686 in males; β=-2.583, P = .575 in females) and DBP (β=-2.544, P = .263 in males; β=-2.619, P = .622 in females).
No interaction between BMI, SUA levels, and BP was observed in either males or females; However, BMI was independently associated with BP both in male and female, SUA independently associated with SBP both in males and females with BMI <24.0 kg/m2, and SUA independently associated with DBP in females with BMI ≥24.0 kg/m2.
Keywords: blood pressure, body mass index, combined effect, serum uric acid
1. Introduction
As well known, according to the evidence of increasing risk[1–3] and incidence of cardiovascular disease (CVD),[4–6] the hypertension is defined as a systolic blood pressure (SBP) of >140 mm Hg and/or diastolic blood pressure (DBP) of >90 mm Hg. Hypertension is a cluster of risk factors[7–14] associated with aging, central obesity, overweight, poor lifestyle, family history of hypertension, diabetes and dyslipidemia, lack of physical activities, cigarette smoking, alcohol consumption, high levels of low-density lipoprotein cholesterol (LDL-C), low levels of high-density lipoprotein cholesterol (HDL - C), elevated fasting glucose levels, and elevated triglycerides (TG). Because hypertension is more complex and patients suffer from physical, psychosocial, and economical burden. Recently, it has become an important public health challenges worldwide.[15] The prevalence of hypertension has increased in the past few years in China.[16,17] Furthermore, as the aging population increases, the hypertension rate is disproportionately high among individuals aged ≥45 years in China.[18–20] Hypertension is a complex disease, and patients with hypertension suffer from economic, psychosocial, and physical burden. Recently, hypertension became most important public health challenges worldwide. Therefore, an effective strategy to prevent hypertension and determine its timely associated risks should be carefully implemented. Exploring the its timely associated risks and their interaction of hypertension may provide the insight in public health implications for prevention and management of hypertension in future.
Serum uric acid (SUA) is an endogenous end product and is involved in the production of reactive-oxygen species. It is important to evaluate their status in advance of chronic disease development.[21] In recent years, as a key mark, systemic measured by SUA has become an important marker for chronic disease development. Studies have conduct that SUA is associated with various diseases, such as CVD,[22–25] prehypertension,[26–29] metabolic syndrome,[30–32] and hypertension.[33–35] However, despite the association between SUA levels and these risk conditions, SUA levels may not be regarded as an independent risk factor. Since SUA level is highly associated with overweight, obesity and other risk factors,[36–38] which is in turn associated with risk of hypertension, a causal condition may exist between body mass index (BMI) and risk of hypertension. Therefore, the association between SUA levels and risk of hypertension and the effects BMI on this association are of considerable interest, and a modulating effect between BMI and SUA levels on blood pressure (BP) may also be fully considered.
To date, few studies on the association and interaction analysis between SUA and BMI level and blood pressure (BP) were conducted in individuals aged ≥45 years. Several studies[39,40] have explored the association and/or interaction analysis between BMI and SUA level and BP, but the relationships between SUA and BP of participants categorized by BMI level may be different, especially lack of related research in China culture background. The evidence on the association and interaction analysis between BMI and SUA level and BP in middle-aged and elderly individuals remains unclear.[40] Thus, the present study aimed to determine the prevalence of normotension and hypertension and their association with body mass index, SUA levels, and other confounding factors according to gender using cross-sectional data from community-dwelling individuals aged ≥45 years in China.
2. Methods
2.1. Participants
Data were extracted from the China Health and Retirement Longitudinal Study (CHARLS), Wave 1 (2011).[41] Samples of individuals with 45 years of age or older were selected by multistage probability sampling from 150 counties fell within 28 provinces between June 2011 and March 2012. CHARLS respondents are followed using a face-to-face computer-assisted personal interview (CAPI). The study was approved by the institutional ethical committees of Peking University. All participants enrolled for the study signed the consent, and the institutional review board of the Peking University approved the study protocol. The cross-section and observational design follow the STROBE guidelines.[42] The data is publicly available (http://charls.pku.edu.cn/zh-CN), and the research have no direct contact with the individual participants. At baseline, 17708 respondents in wave1 gave the consent to participate, and 7186 respondents were with full socio-demographic characteristics, health behaviors, medical history, and metabolic measures. Subjects who used anti-hypertensive drugs, had impaired kidney function (estimated glomerular filtration rate [eGfr]<60 mL/minute/1.73 m2)[43] and diabetes were excluded from our study. Finally, 5888 subjects were included in our study. The CHARLS involved 5888 individuals aged 45 years or older, out of whom 46.91% were men [mean age=60.15 years, standard deviation (SD)=9.10, range: 45–93] and 53.09% were women (mean age=58.74 years, SD = 9.36, range: 45–96).
2.2. Self-reported factors
Variables like age, educational levels (1= Illiterate, 2= Less than elementary school, 3= High school, 4= Above vocational school), marital status (1= Single, 2= Married), place of residence (1= Rural, 2= Urban), cigarette smoking (1= No, 2= Former smoke,3= Current smoke), alcohol consumption (1= No, 2= Less than once a month, 3= More than once a month), eating habit (1= ≤2 meals per day, 2=3 meals per day, 3= ≥4 meals per day), social events (1= No, 2= Yes), history of accidental injury (1= No, 2= Yes), physical exercise (1= No physical exercise, 2= Less than regular physical exercises, 3= Regular physical exercises), hepatitis history (1= No, 2= Yes), history of CVD (0= No, 1= Yes), history of antilipidemic medication (1= No, 2= Yes) were obtained using a self-reported questionnaire, and most variables based on our previous studies.[44–47]
2.3. Measurements
BMI was defined as the body mass (kg) divided by the square of the body height (m).[48] C-reactive protein (CRP) was measured by immunoturbidimetric assay. Fasting plasma glucose (FPG), TG, LDL-C, and HDL-C were analyzed using the enzymatic colorimetric tests, SUA levels were analyzed using the urinalysis (UA) plus method. The average value of blood pressure was determined by mean of the 3 measurements. eGFR was measured by the chronic kidney disease epidemiology collaboration creatinine-cystatin equations.[49] BMI were divided into 4 categories:
-
(1)
underweight (BMI <18.5 kg/m2),
-
(2)
normal (18.5–24 kg/m2),
-
(3)
overweight (24–28 kg/m2), and
-
(4)
obese (≥28 kg/m2).[50]
Hyperuricemia (HUA) was defined as SUA concentration of >7 mg/dL in men and >6 mg/dL in women.[51] CRP were classified into 4 categories (1= ≤1.00 mg/l, 2= 1.01–3.00 mg/l, 3= 3.01–10.00 mg/l and 4=>10 mg/l).[43,52–54] The blood pressures were measured in quiet environment, and she or he should keep sitting, relaxing, and place the left arm on a flat surface, with the palm of the hand facing up, so that the upper arm was at the same height as the heart, then the tester would press the “start” button in the Omron hem-7200 sphygmomanometer, and the cuff could automatically inflate and deflate. After three measurements, it would take the average of 3 measurements as the final blood pressures. Participants were divided into normotension (defined as not being on antihypertensive therapies with an SBP of <140 mm Hg and DBP of <90 mm Hg), and hypertension (defined as SBP of ≥140 mm Hg and/or DBP of ≥90 mm Hg) groups, the categorization has been widely used in previous studies.[40,46]
2.4. Statistical analysis
Data were analyzed by using SPSS17.0 software for Windows10 (IBM Corp., Armonk, NY) the mean SD or frequency, as appropriate. Differences between groups according to BMI (<18.5 kg/m2, 18.5–24 kg/m2, 24–28 kg/m2, and ≥28 kg/m2) and blood pressure (hypertension and normotension) were evaluated using the Student t test (continuous data) or the chi-square test (categorical data). The trends of the related variables according to the body mass index categories were also tested using contrast analysis. The adjusted associations between various characteristics and blood pressure status were first compared using linear regression models, as appropriate. Then, general linear models adjusting for related potential confounders[55] (socio-demographic characteristics [age, educational level, marital status, place of residence], health behaviors [cigarette smoking, alcohol consumption, eating habits, social events, history of accidental injury, physical activities], medical history [history of CVD, hepatitis history, history of antilipidemic medication], metabolic measures (CRP, low density lipoprotein, high density lipoprotein, TG) were used to examine the synergistic effect of SUA and body mass index level on blood pressure for middle-aged and elderly individuals in China. 2-tailed, and a value of P of .05 were considered significant.
3. Results
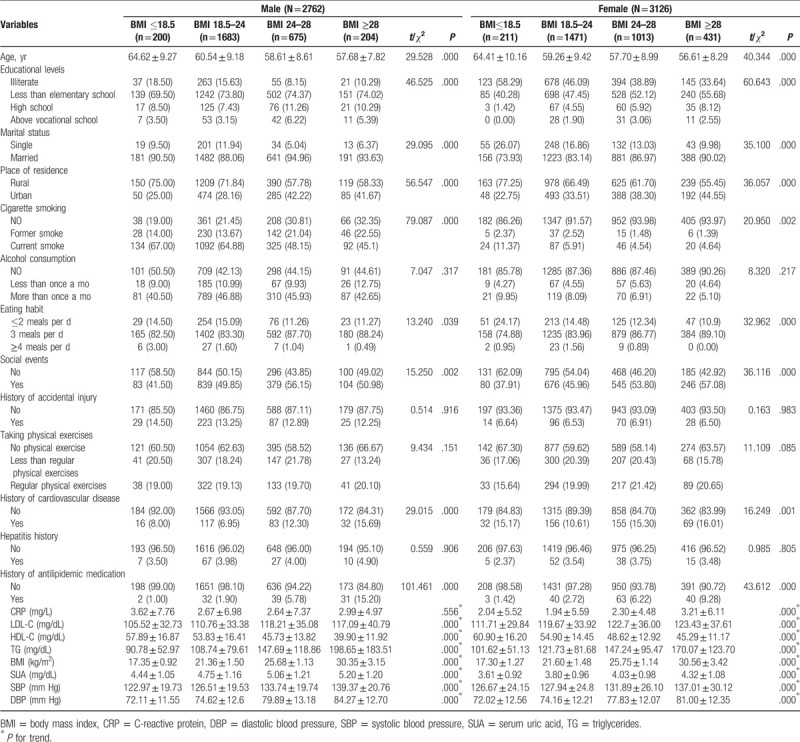
In the study, 5888 participants who effectively completed the questionnaires were included. Various baseline characteristics of participants categorized by BMI were shown in Table 1, and most variables based on our previous studies.[44–47] Overall, 2762(46.91%) of the participants were male, and 3126 (53.09%) of the participants were female. The average ages of the male and female participants were 60.15 ± 9.10 and 58.74 ± 9.36 years old, respectively. The mean serum concentrations of SUA were 4.83 ± 1.18 mg/dL and 3.93 ± 1.00 mg/dL in males and females, respectively. In males, the mean SBP and DBP were 128.97 ± 20.18mm Hg and 76.44 ± 13.09 mm Hg, respectively, and, in females, the mean SBP and DBP were 130.39 ± 26.16 mm Hg and 76.15 ± 12.49 mm Hg, respectively. Considering the modified Chinese criteria for BMI,[50] the mean and SD of BMI were 22.79 ± 3.48 kg/m2 in males, among whom 7.24% were underweight, 60.93% were normal, 24.44% were overweight, and 7.39% were obese, whereas the mean and SD of BMI were 23.89 ± 3.98 kg/m2 in females, among whom 6.75% were underweight, 47.06% were normal, 32.41% were overweight, and 13.79% were obese.
Table 1.
Baseline of demographic variables of participants categorized by BMI in male (N = 2762) and female (N = 3126).
In order to explore the direct associations, the effect between BMI category and SUA levels on BP was observed by the plot in Figure 1. SUA levels had a positive correlation with both DBP and SBP. Analysis of covariance showed that three regression lines in each graph were significantly different from the other groups (In male: SBP, F= 42.171, P = .000 and DBP, F = 57.628, P = .000; In female: SBP, F = 11.469, P = .000 and DBP, F = 42.034, P = .000; respectively).
Figure 1.
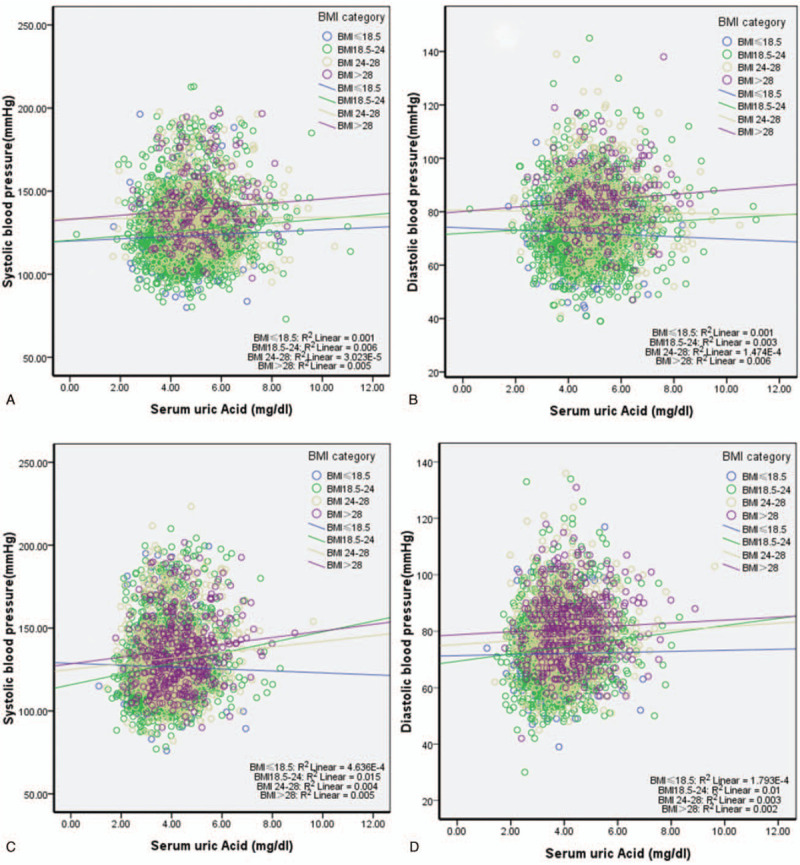
A, B, association between SUA and BP status of participants categorized by BMI in male. C, D, association between SUA and BP status of participants categorized by BMI in female. BMI = body mass index, BP = blood pressure, SUA = serum uric acid.
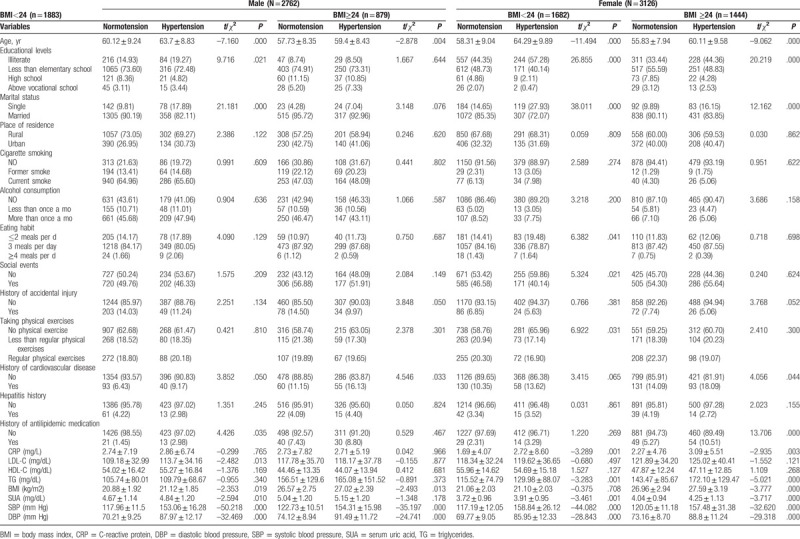
Table 2 show the relationship between various characteristics of participants categorized by BMI and BP status in male and female.
Table 2.
Baseline of demographic variables of participants categorized by BMI and BP in male (N = 2762) and female (N = 3126).
-
(1)
In male with BMI <24.0 kg/m2, BMI, SUA, SBP, and DBP were significantly higher hypertension group than those in the normotension group.
-
(2)
In male with BMI ≥24.0 kg/m2, BMI, SBP, and DBP were significantly higher in hypertension group than those in the normotension group.
-
(3)
In female with BMI <24.0 kg/m2, SUA, SBP, and DBP were significantly higher in hypertension group than those in the normotension group.
-
(4)
In female with BMI ≥24.0 kg/m2, SUA, BMI, SBP, and DBP were significantly higher in hypertension group than those in the normotension group.
Table 3 show age-adjusted relationship between baseline of demographic variables and blood pressure status of participants categorized by gender. First, in male with BMI <24.0 kg/m2, age-adjusted partial Pearson correlation coefficient showed that BMI and SUA were positively correlated with both SBP and DBP. Secondly, in male with BMI ≥24.0 kg/m2, BMI were positively correlated with both SBP and DBP. Thirdly, in female with BMI <24.0 kg/m2, BMI and SUA were positively correlated with both SBP and DBP; Lastly, in female with BMI ≥24.0 kg/m2, BMI were positively correlated with both SBP and DBP; SUA were positively correlated with DBP.
Table 3.
Age-adjusted association between baseline of demographic variables and BP of participants categorized by BMI in male (N = 2762) and female (N = 3126).
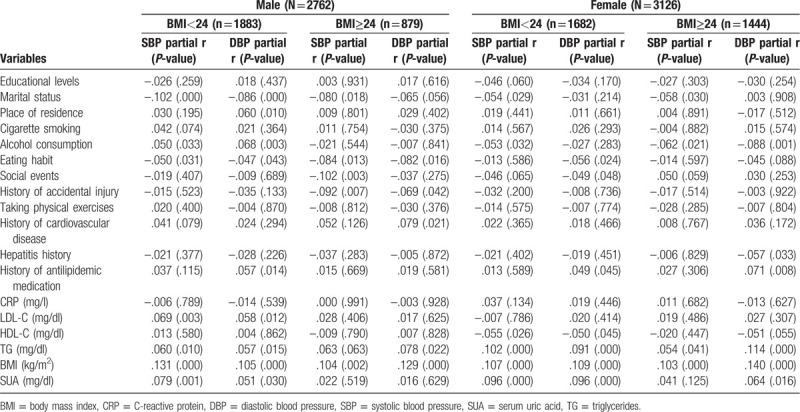
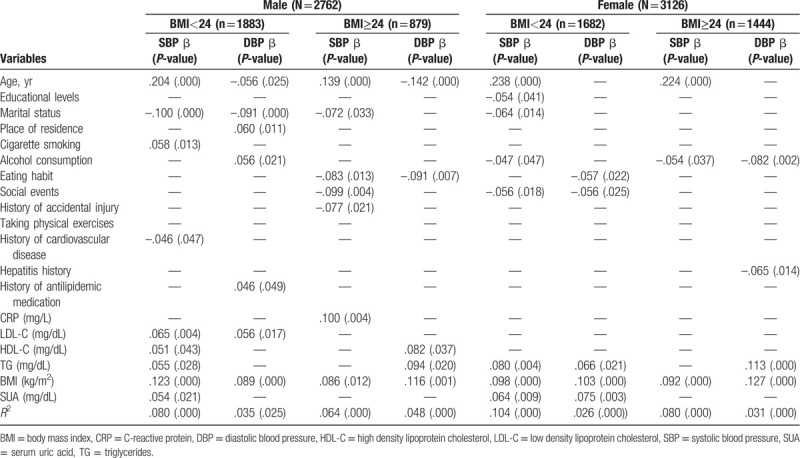
Table 4 show multivariate-adjusted relationship between baseline of demographic variables and blood pressure in participants categorized by gender. The result showed that SUA level was significantly and positively associated with SBP in both men and women with BMI of <24.0 kg/m2, and also significantly and positively associated with DBP in women with BMI of <24.0 kg/m2 (males with BMI <24.0 kg/m2: β=0.054, P = .021; females with BMI <24.0 kg/m2: β=0.064, P = .009; females with BMI ≥24.0 kg/m2: β=0.075, P = .003), independently of other confounding factors.
Table 4.
Multivariate-adjusted association between baseline of demographic variables and BP of participants categorized by BMI in male (N = 2762) and female (N = 3126).
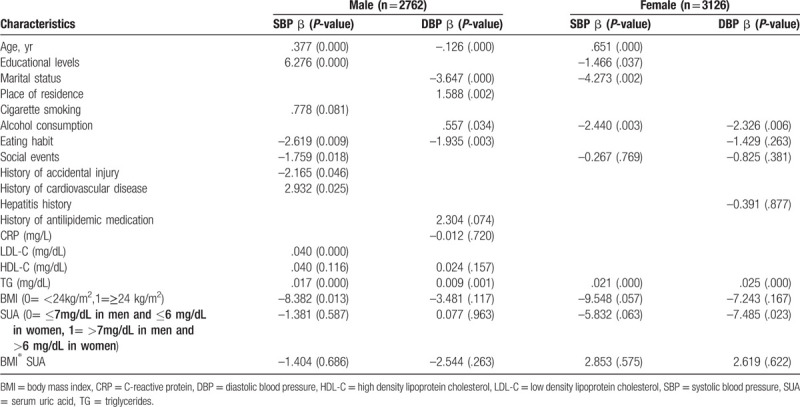
A general linear model adjusted for confounding factors (socio-demographic characteristics [age, educational level, marital status, place of residence], health behaviors [cigarette smoking, alcohol consumption, eating habits, social events, history of accidental injury, physical activities], medical history [history of CVD, hepatitis history, history of antilipidemic medication], metabolic measures [C-reactive protein, low density lipoprotein, high density lipoprotein, TG] was used to assessed the statistical significance of the synergistic relationship between BMI and SUA. Evidence of interaction between BMI and SUA level on SBP (β=-1.404, P = 0.686 in males; β=-2.583, P = .575 in females) and DBP (β=-2.544, P = .263 in males; β=-2.619, P = .622 in females) (Table 5).
Table 5.
Interaction between BMI and SUA on BP in male and female (N = 5888).
4. Discussion
The individual and combined effects of BMI and SUA level and level with BP varied in middle-aged and elderly individuals. In our study, we attempted to explore the prevalence of hypertension and its association with BMI and SUA level. The results show that prevalence of hypertension was 28.13% in males and 30.07% in females, similar to those of the English individuals (men, 36.8%; women, 38.6%).[56] Moreover, SUA levels were positively associated with SBP and DBP in both males and females with BMI <24 kg/m2. In females with BMI ≥24.0 kg/m2, SUA levels were positively correlated with DBP, but not with SBP.
Although previous studies[39,40,48] have explored the individual and combined analysis between BMI and SUA levels and BP, there are no consistent results. Lee et al[48] found that SUA levels were positively associated with SBP and DBP in males aged <40 years after adjustment for age, diabetes, dyslipidemia, BMI, and eGFR; however, no significant associations were found in males aged 60 years or older. Lyngdoh et al,[39] using 549 individuals aged 19 to 20 years, found that SUA levels tended to be positively associated with DBP and SBP in males, while the strength of the SUA-BP association was similar in females. Kawamoto et al[40] found that increased SUA levels were positively associated with SBP and DBP in participants with BMI <21.0 kg/m2, while there was a negative association between SUA levels, SBP and DBP in those with BMI ≥ 21.0 kg/m2, in whom the interaction between BMI and SUA levels was a significant and independent determinant for both SBP and DBP. However, since the sample size was relatively small, and individuals were not randomly selected, the analyses did not rely on gender (it was included the men). In our study, participants were divided into four categories according to the BMI. SUA levels positively correlated with both SBP and DBP in males with BMI <24.0 kg/m2. Among females, the SUA levels significantly correlated with SBP and DBP in participants with BMI <24.0 kg/m2 and positively correlated with DBP in those with BMI ≥24.0 kg/m2. However, no correlation was found between SBP and SUA levels in females with BMI ≥24.0 kg/m2. In addition, multiple linear regression analysis showed that the SUA levels were significantly and positively associated with SBP in both males and females with BMI <24.0 kg/m2, and with DBP in females with BMI <24.0 kg/m2, regardless of other confounding factors. In contrast, no effects of the interaction between BMI and SUA levels on BP were observed in both males and females, although their independent effects on BP were observed. The mechanisms that lead to hypertension in individuals with high BMI or SUA levels are not completely understood.[40] Choi et al[57] reported that high SUA levels induced endothelial dysfunction through vascular resistance in insulin-induced NO production, potentially leading to hypertension. Maxwell et al[58] suggested that the association of high SUA levels with CVD may be a consequence of impaired NO activity in the blood vessels. Papezikova et al[59] demonstrated that high SUA levels lead to a decreased NO bioavailability through multiple mechanisms. These studies may provide insights on the pathogenic mechanism by which SUA induces hypertension. Moreover, SUA is significantly associated with inflammation,[60–62] insulin resistance,[63–65] oxidative stress[66–68] and other risk factors for CVD, such as BMI, total cholesterol, HDL-C, blood pressure, TG, and fasting plasma glucose.[40] Risk factors associated with hypertension may lead to decreased vasomotor reactivity, endothelial dysfunction, and arterial stiffness,[40] ultimately causing hypertension. Our study suggests that SUA may play an important role in hypertension, and gender-specific factors may also be crucial. The SUA levels were higher in males than in females, which can partially explain the underlying mechanisms that possibly account for gender differences, such as alcohol consumption, whose prevalence is usually higher in males. Additionally, body fat and steroid hormones, and their interaction in middle-aged and older adults may also be associated with hypertension. Middle-aged and older females with higher BMI have higher concentrations of estrogen in blood, which may result in a strong protective effect against hypertension.
There are several strengths and limitations in our study. The individual and combined effects of BMI and SUA level and BP is unclear. In addition, we only considered the above mentioned confounders, and other unknown confounders are likely to exist. The relationship should be studied prospectively; however, this was a cross-sectional study including middle-aged and elderly participants. Follow-up was relatively short to comprehensively observe changes in the next phase. Our results contradict the results of a Japanese study that found an association between BMI and SUA in community-dwelling male individuals[40]; however, no interaction between BMI, SUA, and BP was observed either in males or females. In summary, our findings are unique, especially because we evaluated the association between SUA and BP in different BMI groups, where individuals were classified as obese, overweight, normal weight, and underweight, as defined by the Chinese criteria.[50] The BMI cut-off values of the Chinese population are lower than those of western populations, but higher than those of most Asian populations.[69]
5. Conclusions
No interaction between BMI, SUA levels, and BP was observed in either males or females; However, BMI was independently associated with BP both in male and female, SUA independently associated with SBP both in males and females with BMI <24.0 kg/m2, and SUA independently associated with DBP in females with BMI ≥24.0 kg/m2.
Acknowledgments
We are grateful to the participants and members of the CHARLS.
Author contributions
Conceptualization: Lin Zhang.
Formal analysis: Lin Zhang.
Writing – original draft: Lin Zhang.
Writing – review and editing: Lin Zhang, Jin-long Li, Li-li Zhang, Lei-lei Guo, Hong Li, Dan Li.
Footnotes
Abbreviations: BMI = body mass index, CHARLS = China Health and Retirement Longitudinal Study, CRP = C-reactive protein, CVD = cardiovascular disease, DBP = diastolic blood pressure, eGFR = estimated glomerular filtration rate, HDL-C = high density lipoprotein cholesterol, LDL-C = low density lipoprotein cholesterol, SBP = systolic blood pressure, SD = standard deviation, SUA = serum uric acid, TG = triglycerides.
How to cite this article: Zhang L, Li Jl, Zhang Ll, Guo Ll, Li H, Li D. Body mass index and serum uric acid level: Individual and combined effects on blood pressure in middle-aged and older individuals in China. Medicine. 2020;99:9(e19418).
CHARLS was supported by the National Natural Science Foundation of China (G030602) and National Intelligence Agency. The funding body was not involved in the design of the study, data collection, analysis and interpretation, or in writing the manuscript.
The authors have no conflicts of interest to disclose.
References
- [1].Glynn RJ, L’Italien GJ, Sesso HD, et al. Development of predictive models for long-term cardiovascular risk associated with systolic and diastolic blood pressure. Hypertension 2002;39:105–10. [DOI] [PubMed] [Google Scholar]
- [2].Yu D, Huang J, Hu D, et al. Association between prehypertension and clustering of cardiovascular disease risk factors among Chinese adults. J Cardiovasc Pharmacol 2009;53:388–400. [DOI] [PubMed] [Google Scholar]
- [3].Gu D, Chen J, Wu X, et al. Prehypertension and risk of cardiovascular disease in Chinese adults. J Hypertens 2009;27:721–9. [DOI] [PubMed] [Google Scholar]
- [4].Fagard RH. Predicting risk of fatal cardiovascular disease and sudden death in hypertension. J Hypertens 2017;35:2165–7. [DOI] [PubMed] [Google Scholar]
- [5].James JE. Hypertension control and cardiovascular disease. Lancet 2017;389:154. [DOI] [PubMed] [Google Scholar]
- [6].Lackland DT, Weber MA. Global burden of cardiovascular disease and stroke: hypertension at the core. Can J Cardiol 2015;31:569–71. [DOI] [PubMed] [Google Scholar]
- [7].Gui ZH, Zhu YN, Cai L, et al. Sugar-sweetened beverage consumption and risks of obesity and hypertension in Chinese Children and Adolescents: a national cross-sectional analysis. Nutrients 2017;9.: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Lee MS, Chang CH, Lin RY, et al. Risks of hypertension associated with cyclosporine, nonsteroidal anti-inflammatory drugs, and systemic glucocorticoids in patients with psoriasis: a nationwide population-based nested case-control study in Taiwan. Pharmacoepidemiol Drug Saf 2016;25:133–40. [DOI] [PubMed] [Google Scholar]
- [9].Kannel WB. Hypertension: reflections on risks and prognostication. Med Clin North Am 2009;93:541–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Beilin L. Alcohol and hypertension: balancing the risks and benefits. J Hypertens 2005;23:1953–5. [DOI] [PubMed] [Google Scholar]
- [11].Cartier A, Malo JL, Gautrin D, et al. Glucocorticoid use and risks of ocular hypertension and glaucoma. Jama 1997;277:1929–30. [DOI] [PubMed] [Google Scholar]
- [12].Isezuo SA, Sabir AA, Ohwovorilole AE, et al. Prevalence, associated factors and relationship between prehypertension and hypertension: a study of two ethnic African populations in Northern Nigeria. J Hum Hypertens 2011;25:224–30. [DOI] [PubMed] [Google Scholar]
- [13].Kawamoto R, Kohara K, Tabara Y, et al. Insulin resistance and prevalence of prehypertension and hypertension among community-dwelling persons. J Atheroscler Thromb 2010;17:148–55. [DOI] [PubMed] [Google Scholar]
- [14].Kawamoto R, Tabara Y, Kohara K, et al. Increased high-density lipoprotein cholesterol is associated with a high prevalence of pre-hypertension and hypertension in community-dwelling persons. Endocrine 2012;42:321–8. [DOI] [PubMed] [Google Scholar]
- [15].Cloutier L, Morris D, Bruneau J, et al. World Health Organization celebrates World Health Day, April 7,2013--focusing on hypertension. Can J Cardiovasc Nurs 2013;23:9–11. [PubMed] [Google Scholar]
- [16].Zhao Y, Yan H, Marshall RJ, et al. Trends in population blood pressure and prevalence, awareness, treatment, and control of hypertension among middle-aged and older adults in a rural area of Northwest China from 1982 to 2010. PloS One 2013;8:e61779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Wu Y, Huxley R, Li L, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation 2008;118:2679–86. [DOI] [PubMed] [Google Scholar]
- [18].Liu X, Gu W, Li Z, et al. Hypertension prevalence, awareness, treatment, control, and associated factors in Southwest China: an update. J Hypertens 2017;35:637–44. [DOI] [PubMed] [Google Scholar]
- [19].Wu L, He Y, Jiang B, et al. Trends in prevalence, awareness, treatment and control of hypertension during 2001-2010 in an Urban elderly population of China. PloS One 2015;10:e0132814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wang S, Chen R, Liu Q, et al. Prevalence, awareness and treatment of chronic kidney disease among middle-aged and elderly: the China Health and Retirement Longitudinal Study. Nephrology 2015;20:474–84. [DOI] [PubMed] [Google Scholar]
- [21].Kim Y, Kim YJ, Lim Y, et al. Combination of diet quality score, plasma carotenoids, and lipid peroxidation to monitor oxidative stress. Oxid Med Cell Longev 2018;2018:8601028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Borghi C. The role of uric acid in the development of cardiovascular disease. Curr Med Res Opin 2015;31 Suppl 2:1–2. [DOI] [PubMed] [Google Scholar]
- [23].Wu AH, Gladden JD, Ahmed M, et al. Relation of serum uric acid to cardiovascular disease. Int J Cardiol 2016;213:4–7. [DOI] [PubMed] [Google Scholar]
- [24].Tian Y, Chen K, Xie Z, et al. The association between serum uric acid levels, metabolic syndrome and cardiovascular disease in middle aged and elderly Chinese: results from the DYSlipidemia International Study. BMC Cardiovasc Disord 2015;15:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Alderman M. Uric acid in hypertension and cardiovascular disease. Can J Cardiol 1999;15 Suppl F:20F–2F. [PubMed] [Google Scholar]
- [26].Kuwabara M, Hisatome I, Niwa K, et al. Uric acid is a strong risk marker for developing hypertension from prehypertension: a 5-year Japanese cohort study. Hypertension 2018;71:78–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Jiang M, Gong D, Fan Y. Serum uric acid levels and risk of prehypertension: a meta-analysis. Clin Chem Lab Med 2017;55:314–21. [DOI] [PubMed] [Google Scholar]
- [28].Soletsky B, Feig DI. Uric acid reduction rectifies prehypertension in obese adolescents. Hypertension 2012;60:1148–56. [DOI] [PubMed] [Google Scholar]
- [29].Syamala S, Li J, Shankar A. Association between serum uric acid and prehypertension among US adults. J Hypertens 2007;25:1583–9. [DOI] [PubMed] [Google Scholar]
- [30].Bouhenni H, Daoudi H, Djemai H, et al. Metabolic syndrome, leptin-insulin resistance and uric acid: a trinomial foe for Algerian city-dweller adolescents’ health. Int J Adolesc Med Health 2018;31:6. [DOI] [PubMed] [Google Scholar]
- [31].King C, Lanaspa MA, Jensen T, et al. Uric acid as a cause of the metabolic syndrome. Contrib Nephrol 2018;192:88–102. [DOI] [PubMed] [Google Scholar]
- [32].Cibickova L, Langova K, Vaverkova H, et al. Correlation of uric acid levels and parameters of metabolic syndrome. Physiol Res 2017;66:481–7. [DOI] [PubMed] [Google Scholar]
- [33].Wu L, He Y, Jiang B, et al. Association between serum uric acid level and hypertension in a Chinese elderly rural population. Clin Exp Hypertens 2017;39:505–12. [DOI] [PubMed] [Google Scholar]
- [34].Cui LF, Shi HJ, Wu SL, et al. Association of serum uric acid and risk of hypertension in adults: a prospective study of Kailuan Corporation cohort. Clin Rheumatol 2017;36:1103–10. [DOI] [PubMed] [Google Scholar]
- [35].Feig DI. Uric acid and hypertension. Semin Nephrol 2011;31:441–6. [DOI] [PubMed] [Google Scholar]
- [36].Kuwahara E, Murakami Y, Okamura T, et al. Increased childhood body mass index is associated with young adult serum uric acid levels: a linkage study from Japan. Pediatr Res 2016; 81:293–8. [DOI] [PubMed] [Google Scholar]
- [37].Tanaka K, Ogata S, Tanaka H, et al. The relationship between body mass index and uric acid: a study on Japanese adult twins. Environ Health Prev Med 2015;20:347–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Yue JR, Huang CQ, Dong BR. Association of serum uric acid with body mass index among long-lived Chinese. Exp Gerontol 2012;47:595–600. [DOI] [PubMed] [Google Scholar]
- [39].Lyngdoh T, Viswanathan B, Myers GJ, et al. Impact of different adiposity measures on the relation between serum uric acid and blood pressure in young adults. J Hum Hypertens 2012;26:677–83. [DOI] [PubMed] [Google Scholar]
- [40].Kawamoto R, Ninomiya D, Senzaki K, et al. Interaction between body mass index and serum uric acid in relation to blood pressure in community-dwelling Japanese men. Clin Hypertens 2018;24:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Zhao Y, Hu Y, Smith JP, et al. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol 2014;43:61–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Chen CH, Liu LK, Chen MJ, et al. Associations between vitamin D deficiency, musculoskeletal health, and cardiometabolic risk among community-living people in Taiwan: age and sex-specific relationship. Medicine 2018;97:e13886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Wang H, Liu T, Cai YY, et al. Kidney function and cognitive impairment in people aged 80 years and over with untreated hypertension: a cross-sectional survey. Kidney Blood Press Res 2016;41:70–7. [DOI] [PubMed] [Google Scholar]
- [44].Zhang L, Liu K, Li H, et al. Relationship between body mass index and depressive symptoms: the “fat and jolly” hypothesis for the middle-aged and elderly in China. BMC public health 2016;16:1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Zhang L, Li JL, Zhang LL, et al. No association between C-reactive protein and depressive symptoms among the middle-aged and elderly in China Evidence from the China Health and Retirement Longitudinal Study. Medicine 2018;97: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Zhang L, Li JL, Zhang LL, et al. Association and interaction analysis of body mass index and triglycerides level with blood pressure in elderly individuals in China. BioMed Res Int 2018;2018:8934534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Zhang L, Li JL, Zhang LL, et al. Relationship between adiposity parameters and cognition: the “fat and jolly” hypothesis in middle-aged and elderly people in China. Medicine 2019;98: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Lee JJ, Ahn J, Hwang J, et al. Relationship between uric acid and blood pressure in different age groups. Clin Hypertens 2015;21:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Zhu Y, Ye X, Zhu B, et al. Comparisons between the 2012 new CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) equations and other four approved equations. PloS One 2014;9:e84688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Zhou BF. Effect of body mass index on all-cause mortality and incidence of cardiovascular diseases--report for meta-analysis of prospective studies open optimal cut-off points of body mass index in Chinese adults. Biomed Environ Sci 2002;15:245–52. [PubMed] [Google Scholar]
- [51].Cheng W, Wen S, Wang Y, et al. The association between serum uric acid and blood pressure in different age groups in a healthy Chinese cohort. Medicine 2017;96:e8953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Ridker PM. Clinical application of C-reactive protein for cardiovascular disease detection and prevention. Circulation 2003;107:363–9. [DOI] [PubMed] [Google Scholar]
- [53].Wium-Andersen MK, Orsted DD, Nielsen SF, et al. Elevated C-reactive protein levels, psychological distress, and depression in 73, 131 individuals. JAMA Psychiatry 2013;70:176–84. [DOI] [PubMed] [Google Scholar]
- [54].Cepeda MS, Stang P, Makadia R. Depression is associated with high levels of C-reactive protein and low levels of fractional exhaled nitric oxide: results from the 2007-2012 National Health and Nutrition Examination Surveys. J Clin Psychiatry 2016. [DOI] [PubMed] [Google Scholar]
- [55].Chang HH, Yen ST. Association between obesity and depression: evidence from a longitudinal sample of the elderly in Taiwan. Aging Ment Health 2012;16:173–80. [DOI] [PubMed] [Google Scholar]
- [56].Steptoe A, McMunn A. Health behaviour patterns in relation to hypertension: the English Longitudinal Study of Ageing. J hypertens 2009;27:224–30. [DOI] [PubMed] [Google Scholar]
- [57].Choi YJ, Yoon Y, Lee KY, et al. Uric acid induces endothelial dysfunction by vascular insulin resistance associated with the impairment of nitric oxide synthesis. FASEB J 2014;28:3197–204. [DOI] [PubMed] [Google Scholar]
- [58].Maxwell AJ, Bruinsma KA. Uric acid is closely linked to vascular nitric oxide activity. Evidence for mechanism of association with cardiovascular disease, J Am Coll Cardiol 2001;38:1850–8. [DOI] [PubMed] [Google Scholar]
- [59].Papezikova I, Pekarova M, Kolarova H, et al. Uric acid modulates vascular endothelial function through the down regulation of nitric oxide production. Free Radic Res 2013;47:82–8. [DOI] [PubMed] [Google Scholar]
- [60].Turak O, Ozcan F, Tok D, et al. Serum uric acid, inflammation, and nondipping circadian pattern in essential hypertension. J Clin Hypertens 2013;15:7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Zhou Y, Fang L, Jiang L, et al. Uric acid induces renal inflammation via activating tubular NF-kappaB signaling pathway. PloS One 2012;7:e39738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Kalay N, Aytekin M, Kaya MG, et al. The relationship between inflammation and slow coronary flow: increased red cell distribution width and serum uric acid levels. Turk Kardiyol Dern Ars 2011;39:463–8. [DOI] [PubMed] [Google Scholar]
- [63].Liu ZM, Ho SC. The association of serum C-reactive protein, uric acid and magnesium with insulin resistance in Chinese postmenopausal women with prediabetes or early untreated diabetes. Maturitas 2011;70:176–81. [DOI] [PubMed] [Google Scholar]
- [64].Mangge H, Pilz S, Haj-Yahya S, et al. Uric acid indicates a high cardiovascular risk profile but is not closely associated with insulin resistance in obese adolescents. Diabetes care 2008;31:e21. [DOI] [PubMed] [Google Scholar]
- [65].Chen LK, Lin MH, Lai HY, et al. Uric acid: a surrogate of insulin resistance in older women. Maturitas 2008;59:55–61. [DOI] [PubMed] [Google Scholar]
- [66].Corry DB, Eslami P, Yamamoto K, et al. Uric acid stimulates vascular smooth muscle cell proliferation and oxidative stress via the vascular renin-angiotensin system. J Hypertens 2008;26:269–75. [DOI] [PubMed] [Google Scholar]
- [67].Strazzullo P, Puig JG. Uric acid and oxidative stress: relative impact on cardiovascular risk? Nutr Metab Cardiovasc Dis 2007;17:409–14. [DOI] [PubMed] [Google Scholar]
- [68].Glantzounis GK, Tsimoyiannis EC, Kappas AM, et al. Uric acid and oxidative stress. Curr Pharm Des 2005;11:4145–51. [DOI] [PubMed] [Google Scholar]
- [69].Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157–63. [DOI] [PubMed] [Google Scholar]


