Abstract
In recent years, deep venous thrombosis (DVT) after spine surgery has received extensive attention, but perioperative prevalence of DVT in patients undergoing percutaneous kyphoplasty (PKP) is lacking.
To assess the perioperative prevalence of deep vein thrombosis (DVT) in patients undergoing PKP with routinely applied ultrasonography.
We reviewed 1113 consecutive patients undergoing PKP from January 2014 to August 2017. The surgical procedure was bilateral PKP. All patients were routinely examined with ultrasonography when admitted to the hospital and on the first post-operative day. Clinical signs of DVT were checked and recorded before examination.
Forty (3.6%) out of 1113 patients were diagnosed with DVT by ultrasonography. Of the 40 detected cases of DVT, only six (0.54%) patients presented with clinical signs of DVT, demonstrating that there were 34 (3.05%) asymptomatic cases. No patient presenting with clinically suspected pulmonary embolism (PE) was observed. Gender, body mass index (BMI), operative time, hypertension, diabetes, heart disease, and lower limb fracture were not significant risk factors for DVT (P > .05). In contrast, patient age, oncologic conditions, DVT history, and paraplegia appeared to be significant risk factors for DVT (P < .01). There was no significant difference in the incidence of DVT found between the three PKP surgical levels (P > .05).
The total incidence of perioperative DVT diagnosed with ultrasonography in patients undergoing PKP was 3.6%, of which only 0.54% was symptomatic cases. It is necessary to assess DVT using ultrasonography during the perioperative procedure of PKP, especially for high-risk patients.
Level of evidence: Level IV.
Keywords: deep venous thrombosis, percutaneous kyphoplasty, pulmonary embolism, ultrasonography
1. Introduction
Deep vein thrombosis (DVT) is viewed as a relatively rare complication in patients after spine surgery.[1–3] Early diagnosis of DVT is important because of the risk of pulmonary embolism (PE) and potentially fatal sequelae. Reported incidence of DVT after spine surgery ranges from 0.3% to 31% in the literature in different patient populations.[4] Alireza et al,[5] in their single center report, found a cumulative symptomatic incidence of DVT as low as 0.83% after surgery and recommended dalteparin as prophylaxis. However, results from McClendon et al[6] showed a high incidence of DVT (18.7%) with mechanical prophylaxis. In a recent study, the incidence of DVT was reported as high as 22.4% in patients undergoing lumbar Interbody fusion surgery, which may be related to advanced age, high-postoperative VAS scores, and blood transfusion.[7] Several case reports feature an association between application of anticoagulation therapy and spontaneous spinal epidural hematoma (SEH),[8,9] so the benefit of anticoagulation and the risk for SEH should be balanced. In view of the varied evidence regarding DVT in patients undergoing spine surgery, it makes clinicians hesitant of applying thromboprophylaxis.
DVT diagnosis has traditionally been performed using venography or ultrasonography. Ultrasonography is a convenient and noninvasive method for detecting DVT compared with venography. It also has proven safe and cost-effective, with a very high sensitivity and specificity (96% and 98%, respectively) for the diagnosis of DVT.[10] Nowadays, minimally invasive surgery (MIS) is becoming a trend in orthopedic surgery.[11,12] In a retrospective study, the total incidence of DVT after arthroscopic knee surgery was 14.9%.[13] Fukushima et al[14] demonstrated that the incidence of DVT was 6.94% during hip arthroscopy. In a randomized controlled trial (RCT), Xue et al[15] found that the DVT incidence after proximal femoral nail anti-rotation (PFNA) surgery on treatment of intertrochanteric fractures was 3.3% (two out of 60). Based on these literature reports, the perioperative DVT cannot be ignored in MIS. Percutaneous kyphoplasty (PKP), one kind of minimally invasive spine surgery (MISS), can provide significant relief to patients with painful vertebral compression fractures (VCF) related to osteoporosis, multiple myeloma, hemangioma, or metastases.[16–19] More than 50,976 patients reported through published articles have received the treatment of PKP in China.[20]
DVT incidence in PKP was presumed very low in many institutions and patients are normally underwent same-day procedures.[21,22] To our knowledge, no report has described the perioperative prevalence of DVT in patients treated with PKP. The goal of this study was to determine the perioperative prevalence of DVT with ultrasonography in patients treated with PKP without antithrombotic or mechanical prophylaxis.
2. Materials and methods
2.1. Patients
This study retrospectively included 1113 patients admitted to Department of Orthopedics in our hospital. All patients underwent PKP, between January 2014 and August 2017. All patients received general anesthesia. The vertebral site lesions were located by C-arm and surgical methods were all used bilateral PKP. No thromboprophylaxis (e.g., mechanical squeezer, Plexi Pulse, or aspirin) were used during the perioperative period. Patients were discharged 2 to 3 days after surgery in average. The risk factors for DVT in these patients were also assessed. This study was approved by the ethics review committee of The First Affiliated Hospital of Soochow University, and written informed consent was obtained from all participants of the study.
2.2. Diagnosis of DVT
All patients underwent lower limb Doppler ultrasonography when admitted to the hospital and on the first post-operative day. The result was read by a physician and another two radiology specialists to get a clear diagnosis. If a vein or venous segment was not fully compressible, the results of ultrasonography were considered positive. Identified DVT was classified as proximal if it involved the iliac, superficial femoral or popliteal veins, with or without calf vein thrombosis, and as distal if it was isolated to the calf veins.[23]
2.3. Inclusion criteria
All patients over 18 years old treated with PKP were included. Patient gender, age, body mass index (BMI), hypertension, diabetes, oncologic conditions, DVT history, paraplegia, lower limb fracture, heart disease, operation time, PKP surgical levels, and distribution of DVT were recorded. Patients were excluded if they took anticoagulant such as aspirin, warfarin before hospital admission.
2.4. Data analysis
Statistical analyses were performed using IBM SPSS Statistics software, version 19 (SPSS, Chicago, IL). Results were expressed as the mean and the standard error of the mean (age, BMI, operative time). The results were compared between the two groups (DVT group vs non-DVT group). A two independent sample T test was used for comparisons of normally distributed data among the groups (age, BMI, operation time). Gender, hypertension, diabetes, oncologic conditions, DVT history, paraplegia, lower limb fracture, heart disease, and PKP surgical levels were statistically compared between the groups using the χ2 test. Statistical significance was defined as P < .01.
3. Results
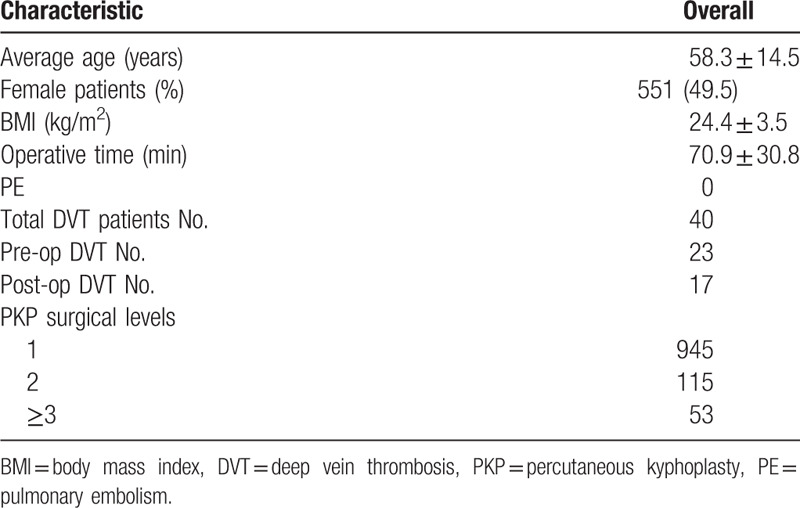
Details of clinical and surgical data for PKP patients are shown in Table 1. During this 20-month period, 1113 patients (551 women) with a mean age (±standard deviation [SD]) of 58.3 ± 14.5 years treated with PKP. The mean duration (±SD) of the operation time was 68.5 ± 9.6 minutes. The mean BMI (±SD) was 24.4 ± 3.5 kg/m2. Nine hundred and forty-five patients underwent single stage PKP, 115 patients were received two-segment PKP and 53 patients were accepted multiple-segment PKP.
Table 1.
Clinical and surgical data for PKP patients.
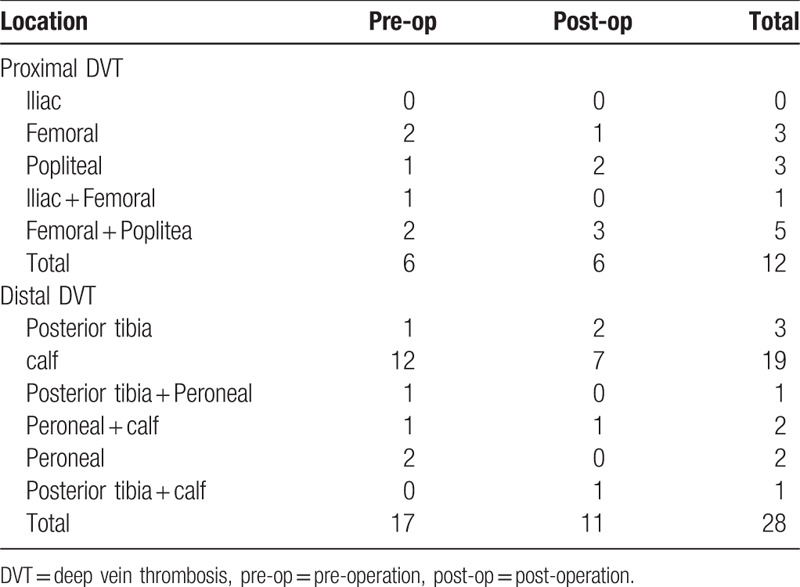
A total of 40 (3.6%) patients were diagnosed with DVT with ultrasonography. Among them, 23 patients (2.1%) had DVT (proximal, six; distal, 17) before surgery. Seventeen patients (1.5%) developed new-onset DVT (proximal, six; distal, 11) after spine surgery. Of these 40 patients, only six (0.54%) had clinical symptoms of DVT, indicating 34 (3.05%) patients would have been missed without ultrasonography. No patient presenting with clinically suspected PE was observed. The distribution of DVT was shown in detail in Table 2. A total of 12 distributed in proximal veins and 28 in distal veins.
Table 2.
Distribution of identified deep vein thrombosis.
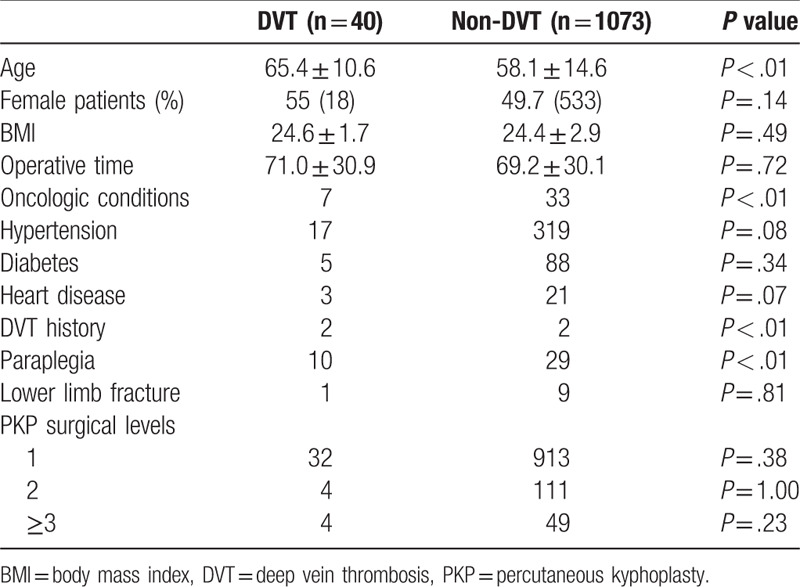
Association between clinical risk factors and DVT were analyzed in Table 3. There was no significant difference in the incidence of DVT found between the three PKP surgical levels (P > .05). Gender, BMI, operative time, hypertension, diabetes, heart disease, and lower limb fracture were not significant risk factors for DVT (P > .05). Age of the DVT group was 65.4 ± 10.6 years old, the non-DVT group was 58.1 ± 14.6 years old. A two independent sample t test showed that DVT group was significantly older than non-DVT group (P < .01). Cancer patients are at significantly increased risk for the development of DVT (17.5% vs 3.1%, P < .01). DVT history is an important high-risk factor for DVT (5.0% vs 0.19%, P < .01). The paraplegia patients in the DVT group were nearly 10 times higher than those in the non-DVT group (25% vs 2.7%, P < .01).
Table 3.
Association between clinical risk factors and deep vein thrombosis.
4. Discussion
A retrospective study of patients undergoing PKP was conducted in order to evaluate the incidence of DVT and the risk factors for perioperative DVT without antithrombotic or mechanical prophylaxis. So far, this study seems to be the first to report the perioperative prevalence of DVT in MISS patients treated with PKP in the literature. With ultrasonography, this study showed a 0.54% incidence of symptomatic DVT and a 3.05% incidence of silent DVT in 1113 patients undergoing PKP. In contrast, Akeda et al,[1] detected that the incidence of perioperative venous thromboembolism (VTE) was 11% in spine surgery. MIS has the advantage of less trauma and shorter operation time. Namboothiri et al,[24] found that the DVT incidence after spine surgery could be as low as 0.78% with no mechanical or chemical prophylaxis. However, ultrasonography was only performed in patients with symptomatic DVT. In addition, our incidence of silent DVT is 3.05%, almost six-fold that of symptomatic DVT. Without ultrasonography, nearly 85% (34 of 40) of the DVT patients will be missed and it could develop into a fatal PE. Besides, silent DVT was reported to increase the incidence of post thrombotic syndrome (PTS), its long-term clinical significance is still unclear.[25] Therefore, the early diagnosis of asymptomatic DVT via ultrasonography should not be underestimated.
Age, oncologic conditions, DVT history, and paraplegia were shown to be significant risk factors for perioperative DVT in patients undergoing PKP in our study (P < .01). Age is a recognized risk factor for DVT, almost consistent with the other studies.[26–28] This may be due to slow flow, hypercoagulability and the decreased in exercise with aging. Cancer patients increased risk for the development of DVT. In our study (17.5% vs 3.1%). Cancer patients are often deconditioned, neurologically impaired, and have chronic pain, which limiting their ability to ambulate, thereby increasing their risk for DVT during immobilization.[29] In addition, DVT history is an important high risk factor for DVT (5.0% vs 0.19%). Stain et al,[30] found a 2.6 (95% CI 1.2–5.9) times increased risk of recurrent VTE in patients with PTS, as compared to those without PTS, indicating patients with a history of DVT should be paid more attention to. In our study, the paraplegia patients in the DVT group were nearly 10 times higher than those in the non-DVT group (25% vs 2.7%). Paraplegia patients lost the motor function of the lower limbs, making the blood flow slow, rendering them at high risk of DVT.
The incidence of preoperative DVT is higher than that of postoperative DVT in our study (2.1% vs 1.5%). Song et al,[31] detected that the incidence of preoperative DVT in patients, who are waiting for elective hip replacement for femoral neck fractures was (29.4%, 35 of 119). Coincidentally, Wakabayashi et al,[32] in their retrospective study, found the prevalence of preoperative DVT in patients for total knee arthroplasty (TKA) was as high as 17.4% (56 of 322). In view of long duration of immobilization, preoperative DVT should not be neglected.
DVT especially proximal DVT is significantly associated with secondary PE.[33] Furthermore, isolated distal DVT (e.g., calf muscle DVT) of the lower limbs can also be associated with subsequent proximal DVT and/or acute PE.[34,35] In our study, ultrasonography scan was routinely performed from the iliac vein to the calf muscle vein, rather than only of the proximal vein. Indeed, nearly 70% (28 of 40) of the total DVTs were distributed at the distal side in our study. Therefore, the distal DVT should be normally scanned in clinical practice.
5. Limitations
Our study has several limitations. This study is a retrospective study, with a prospective study; we could come to a better conclusion with not being affected by too many risk factors for DVT. We only took CTA for the suspected patients for the diagnosis of PE. The incidence of symptomatic PE was historically low in our institution in PKP patients or for patients with any other spine surgeries so the asymptomatic PE patients may be missed. In addition, the incidence of this study was for patients during hospitalization. DVT may also occur in patients after discharge. Thus, the actual incidence of DVT after PKP could be higher than the findings in our study. At last, PKP patients in our institution were historically discharge 2 to 3 days after surgery. Furthermore, early exercise was encouraged, so DVT should be ruled out to prevent secondary PE on the first postoperative day with ultrasonography. For these reasons, we regret the lack of forward data.
6. Conclusions
The total incidence of perioperative DVT diagnosed with ultrasonography in patients treated with PKP was 3.6%, of which only 0.54% was symptomatic cases. It is necessary to assess DVT using ultrasonography during the perioperative procedure of PKP, especially for high-risk patients (advanced age, oncologic conditions, DVT history, and paraplegia).
Author contributions
Conceptualization: Wencan Fan, Tianzhu Qiao.
Data curation: Wencan Fan, Tianzhu Qiao, Yongqing You, Jun Zhang.
Formal analysis: Wencan Fan, Tianzhu Qiao, Yongqing You, Jun Zhang.
Investigation: Jun Zhang.
Methodology: Tianzhu Qiao, Yongqing You.
Validation: Wencan Fan.
Writing – original draft: Wencan Fan, Tianzhu Qiao.
Writing – review & editing: Tianzhu Qiao, Yongqing You, Jijian Gao.
Footnotes
Abbreviations: BMI = body mass index, DVT = deep venous thrombosis, MIS = minimally invasive surgery, MISS = minimally invasive spine surgery, PE = pulmonary embolism, PFNA = proximal femoral nail anti-rotation, PKP = percutaneous kyphoplasty, RCT = randomized controlled trial, SD = standard deviation, SHE = spinal epidural hematoma.
How to cite this article: Fan W, Qiao T, You Y, Zhang J, Gao J. Perioperative prevalence of deep vein thrombosis in patients with percutaneous kyphoplasty: a retrospective study with routine ultrasonography. Medicine. 2020;99:10(e19402).
WF and TQ contributed equally to this study.
This study was approved by the ethics review committee of The First Affiliated Hospital of Soochow University, and written informed consent was obtained from all participants of the study.
This study was performed in Department of Orthopedics of The First Affiliated Hospital of Soochow University.
The authors have no conflicts of interest to disclose.
References
- [1].Akeda K, Matsunaga H, Imanishi T, et al. Prevalence and countermeasures for venous thromboembolic diseases associated with spinal surgery: a follow-up study of an institutional protocol in 209 patients. Spine 2014;39:791–7. [DOI] [PubMed] [Google Scholar]
- [2].Schulte LM, O’Brien JR, Bean MC, et al. Deep vein thrombosis and pulmonary embolism after spine surgery: incidence and patient risk factors. Am J Orthop 2013;42:267–70. [PubMed] [Google Scholar]
- [3].Nicol M, Sun Y, Craig N, et al. Incidence of thromboembolic complications in lumbar spinal surgery in 1,111 patients. Eur Spine J 2009;18:1548–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Glotzbecker MP, Bono CM, Wood KB, et al. Thromboembolic disease in spinal surgery: a systematic review. Spine 2009;34:291. [DOI] [PubMed] [Google Scholar]
- [5].Moayer AF, Mohebali N, Razmkon A. Incidence of deep vein thrombosis in patients undergoing degenerative spine surgery on prophylactic dalteparin; a single center report. Bull Emerg Trauma 2016;4:38–42. [PMC free article] [PubMed] [Google Scholar]
- [6].McClendon J, Jr, Oʼshaughnessy BA, Smith TR, et al. Comprehensive assessment of prophylactic preoperative inferior vena cava filters for major spinal reconstruction in adults. Spine 2012;37:1122. [DOI] [PubMed] [Google Scholar]
- [7].Yang S-D, Ding WY, Yang DL, et al. Prevalence and risk factors of deep vein thrombosis in patients undergoing lumbar interbody fusion surgery: a single-center cross-sectional study. Medicine 2015;94: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Connolly ES, Jr, Winfree CJ, Mccormick PC. Management of spinal epidural hematoma after tissue plasminogen activator. A case report. Spine 1996;21:1694–8. [DOI] [PubMed] [Google Scholar]
- [9].Van Schaeybroeck P, Van Calenbergh F, Van De Werf F, et al. Spontaneous spinal epidural hematoma associated with thrombolysis and anticoagulation therapy: report of three cases. Clin Neurol Neurosurg 1998;100:283–7. [DOI] [PubMed] [Google Scholar]
- [10].Gaitini D. Current approaches and controversial issues in the diagnosis of deep vein thrombosis via duplex Doppler ultrasound. J Clin Ultrasound 2006;34:289–97. [DOI] [PubMed] [Google Scholar]
- [11].Agarwal N, Choi P, Sekula R. Minimally invasive spine surgery for unstable thoracolumbar burst fractures: a case series. Surg J 2016;02:e131–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Liu G, Liu S, Zuo YZ, et al. Recent advances in technique and clinical outcomes of minimally invasive spine surgery in adult scoliosis. Chin Med J 2017;130:2608–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sun Y, Chen D, Xu Z, et al. Incidence of symptomatic and asymptomatic venous thromboembolism after elective knee arthroscopic surgery: a retrospective study with routinely applied venography. Arthroscopy 2014;30:818–22. [DOI] [PubMed] [Google Scholar]
- [14].Fukushima K, Takahira N, Uchiyama K, et al. The incidence of deep vein thrombosis (DVT) during hip arthroscopic surgery. Arch Orthop Trauma Surg 2016;136:1431–5. [DOI] [PubMed] [Google Scholar]
- [15].Xue L, Zha L, Chen Q, et al. Randomized controlled trials of proximal femoral nail antirotation in lateral decubitus and supine position on treatment of intertrochanteric fractures. ScientificWorldJournal 2013;2013:276015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Yuan WH, Hui-Chen H, Lai KL. Vertebroplasty and balloon kyphoplasty versus conservative treatment for osteoporotic vertebral compression fractures: a meta-analysis. Medicine 2016;95:e4491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Nieuwenhuijse MJ, Erkel ARV, Dijkstra PDS. Cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: identification of risk factors. Spine J 2011;11:839–48. [DOI] [PubMed] [Google Scholar]
- [18].Sun ZY, Li XF, Zhao H, et al. Percutaneous balloon kyphoplasty in treatment of painful osteoporotic occult vertebral fracture: a retrospective study of 89 cases. Med Sci Monit 2017;23:1682–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Yang S, Chen C, Wang H, et al. A systematic review of unilateral versus bilateral percutaneous vertebroplasty/percutaneous kyphoplasty for osteoporotic vertebral compression fractures. Acta Orthop Traumatol Turc 2017;51:290–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Yang H, Liu H, Wang S, et al. Review of percutaneous kyphoplasty in China. Spine 2016;41: suppl 19: B52. [DOI] [PubMed] [Google Scholar]
- [21].Al-Dujaili TM, Majer CN, Madhoun TE, et al. Deep venous thrombosis in spine surgery patients: incidence and hematoma formation. Int Surg 2012;97:150–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Yang SD, Liu H, Sun YP, et al. Prevalence and risk factors of deep vein thrombosis in patients after spine surgery: a retrospective case-cohort study. Medicine 2015;5:e2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Sun Y, Chen D, Xu Z, et al. Deep venous thrombosis after knee arthroscopy: a systematic review and meta-analysis. Arthroscopy 2014;30:406–12. [DOI] [PubMed] [Google Scholar]
- [24].Namboothiri S. Incidence of deep vein thrombosis after major spine surgeries with no mechanical or chemical prophylaxis. Evid Based Spine Care J 2012;3:29–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].W-J P, LN J, M C. Asymptomatic postoperative deep vein thrombosis and the development of postthrombotic syndrome. A systematic review and meta-analysis. Thromb Haemost 2005;93:236–41. [DOI] [PubMed] [Google Scholar]
- [26].Buerba RA, Giles E, Webb ML, et al. Increased risk of complications after anterior cervical discectomy and fusion in the elderly: an analysis of 6253 patients in the American College of Surgeons National Surgical Quality Improvement Program database. Spine 2014;39:2062–9. [DOI] [PubMed] [Google Scholar]
- [27].Yoshioka K, Murakami H, Demura S, et al. Prevalence and risk factors for development of venous thromboembolism after degenerative spinal surgery. Spine 2014;40:301–6. [DOI] [PubMed] [Google Scholar]
- [28].Strom RG, Frempongboadu AK. Low-molecular-weight heparin prophylaxis 24 to 36 hours after degenerative spine surgery: risk of hemorrhage and venous thromboembolism. Spine 2013;38:1498–502. [DOI] [PubMed] [Google Scholar]
- [29].Zacharia BE, Kahn S, Bander ED, et al. Incidence and risk factors for preoperative deep venous thrombosis in 314 consecutive patients undergoing surgery for spinal metastasis. J Neurosurg Spine 2017;27:189–97. [DOI] [PubMed] [Google Scholar]
- [30].Stain M, Schönauer V, Minar E, et al. The post-thrombotic syndrome: risk factors and impact on the course of thrombotic disease. J Thromb Haemost 2005;3:2671–6. [DOI] [PubMed] [Google Scholar]
- [31].Song K, Yao Y, Rong Z, et al. The preoperative incidence of deep vein thrombosis (DVT) and its correlation with postoperative DVT in patients undergoing elective surgery for femoral neck fractures. Arch Orthop Trauma Surg 2016;136:1459–64. [DOI] [PubMed] [Google Scholar]
- [32].Wakabayashi H, Hasegawa M, Niimi R, et al. The risk factor of preoperative deep vein thrombosis in patients undergoing total knee arthroplasty. J Orthop Sci 2017;22:698–702. [DOI] [PubMed] [Google Scholar]
- [33].Oda T, Fuji T, Kato Y, et al. Deep venous thrombosis after posterior spinal surgery. Spine 2000;25:2962–7. [DOI] [PubMed] [Google Scholar]
- [34].Brateanu A, Patel K, Chagin K, et al. Probability of developing proximal deep-vein thrombosis and/or pulmonary embolism after distal deep-vein thrombosis. Thromb Haemost 2016;115:608–14. [DOI] [PubMed] [Google Scholar]
- [35].Masuda EM, Kistner RL, Musikasinthorn C, et al. The controversy of managing calf vein thrombosis. J Vasc Surg 2012;55:550–61. [DOI] [PubMed] [Google Scholar]


