Abstract
We report a case of COVID-19 in third-trimester pregnancy, who required support in an intensive care unit and received remdesivir. After discharge, she had an uncomplicated vaginal delivery at term. COVID-19 in pregnancy may be managed without emergent delivery; a multispecialty team is critical in caring for these patients.
Keywords: COVID-19, remdesivir, SARS-CoV-2, third-trimester pregnancy
SARS-CoV-2 is a single-stranded positive-sense RNA virus, first identified in late December 2019 in Wuhan, China; the clinical illness caused by SARS-CoV-2 was subsequently named COVID-19. As of July 23, 2020, the virus has infected over 15.3 million people [1]. The virus has not spared pregnant women, and numerous cases of pregnant patients presenting with COVID-19 have been reported in the literature [2]. However, few publications discuss the care of COVID-19-positive pregnant women in the intensive care unit (ICU) setting [3, 4]. We offer an example of COVID-19 in third-trimester pregnancy successfully managed by an integrated multispecialty team.
CASE
Our patient is a 39-year-old G2P1001 who presented to Labor and Delivery triage at 34 weeks and 4 days with a chief complaint of dry cough and dyspnea for 8 days, with associated mild anorexia and decreased oral intake. Her medical history was significant only for seasonal allergies, and her pregnancy had thus far been uncomplicated. Our patient is a health care worker caring for COVID-19 patients. Upon symptom onset, she isolated at home; nasopharyngeal swab at an urgent care center tested positive for SARS-CoV-2. She was afebrile on presentation and without supplemental oxygen requirement. She was managed expectantly, received an intravenous fluid bolus, and was discharged home.
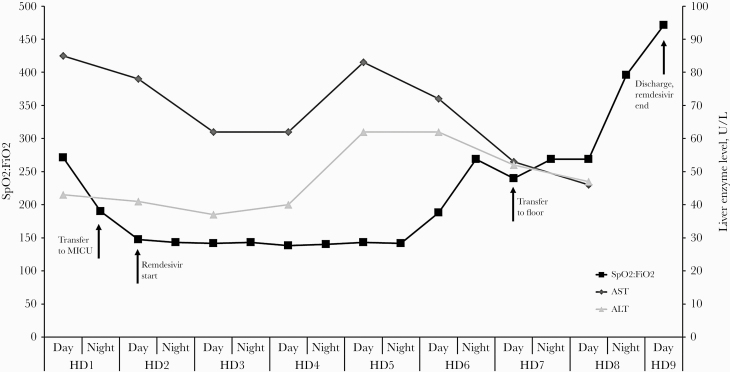
Two days after initial presentation, our patient returned to Labor and Delivery triage, with significant worsening of dyspnea on exertion. On this evaluation, she was noted to be hypoxic to 88% breathing ambient air and was tachypneic to 25 breaths/minute. Her chest x-ray demonstrated bilateral hazy opacities suspicious for COVID-19 pneumonia. Hypoxia improved with supplemental oxygen by nasal cannula. Given her supplemental oxygen requirement, she was admitted to the obstetrics service. Fetal status was initially reassuring and remained so; there was no maternal or fetal indication for delivery. Admission labs were notable for elevated transaminases and D-dimer (Figure 1, Table 1); there was no clinical concern for pre-eclampsia or hemolysis, elevated liver enzymes, low platelets (HELLP) syndrome. Hydroxychloroquine therapy was then standard of care for inpatients at our institution and was initiated. Supplemental oxygen was continued, with the goal of oxygen saturation >95% to support adequate fetal oxygenation.
Figure 1.
Patient’s clinical course. The black line indicates the SpO2:FiO2 ratio, a measure of oxygen requirement used as a representation of the patient’s pulmonary status. Dark and light gray lines indicate AST and ALT, respectively. Labeled arrows indicate significant clinical events. Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; CRP, C-reactive protein; HD, hospital day.
Table 1.
Selected Laboratory Values
| AST, U/L | ALT, U/L | CRP, mg/dL | D-dimer, ng/mL | |
|---|---|---|---|---|
| HD 1 | 85 | 43 | — | 274 |
| HD 2 | 78 | 41 | — | — |
| HD 3 | 62 | 37 | 5.9 | — |
| HD 4 | 62 | 40 | 11.4 | 350 |
| HD 5 | 83 | 62 | 15.3 | 399 |
| HD 6 | 72 | 62 | 12.1 | 700 |
| HD 7 | 53 | 52 | 6.7 | 856 |
| HD 8 | 46 | 47 | 3.8 | 625 |
| HD 9 | — | — | — | — |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; CRP, C-reactive protein; HD, hospital day.
Over the first 12 hours of admission, our patient’s supplemental oxygen requirement increased from nasal cannula to nonrebreather; the ratio of oxygen saturation to fraction of inspired oxygen worsened significantly (SpO2: FiO2) (Figure 1). She was evaluated by pulmonary and critical care medicine (PCCM) and transferred to the medical ICU for closer monitoring (Figure 1). Maternal-fetal medicine (MFM) and infectious disease (ID) teams discussed the case; given the increase in supplemental oxygen requirement since first presentation, the decision was made to apply for compassionate use remdesivir.
The remdesivir compassionate use application was approved by the manufacturer and the Food and Drug Administration via emergency investigational new drug application. MFM, ID, and PCCM discussed the medication with the patient and obtained her informed consent for therapy; remdesivir was initiated on hospital day (HD) 2. Per manufacturer recommendation, hydroxychloroquine was held upon initiation of remdesivir. Her liver enzymes were monitored through her hospital course; per manufacturer requirement, remdesivir was to be discontinued should ALT rise above 5 times the upper limit of normal. Her transaminases peaked on HD 5 (remdesivir day 4), then declined to below admission levels (Figure 1). They were never above twice the upper limit of normal. Her blood pressure remained within normal limits, and there was no proteinuria. C-reactive protein (CRP) peaked at 15.3 mg/dL, then declined (Table 1). Fetal status was evaluated twice daily with a nonstress test; fetal status remained reassuring through her ICU course. Given uptrending D-dimer, lower extremity venous dopplers were performed, which demonstrated no evidence of thrombus.
Her supplemental oxygen requirement decreased steadily, and on HD 7 she was transferred to the obstetrics floor (Figure 1). She was discharged on HD 9, after having completed 8 of a planned 10 days of remdesivir. On telephone follow-up 10 days after discharge, our patient reported ongoing cough and dyspnea on exertion, but with significant improvement from admission. No further fetal imaging was indicated at that time. After a full recovery from COVID-19, the patient had an uncomplicated vaginal delivery at term.
DISCUSSION
Our patient highlights several important aspects of care for pregnant patients presenting with COVID-19. A number of studies have discussed COVID-19 in pregnant women, with a study in our city demonstrating that ~15% of women presenting for delivery were SARS-CoV-2 positive; 1.9% of those women were symptomatic [5]. Recent data have demonstrated that pregnant women diagnosed with COVID-19 have an increased risk of ICU admission and mechanical ventilation as compared with nonpregnant women of childbearing age [6].The 3 other cases of third-trimester COVID-19 ICU admission previously reported all noted a need for intubation and delivery [3, 4]; however, decisions regarding emergent delivery are individualized and require consideration of both maternal and fetal status. In our case, there was never a maternal or fetal indication for delivery during this hospitalization. Emergent cesarean delivery in ICUs is reserved for acute and severe maternal or fetal decompensation; we demonstrate that pregnant women critically ill with COVID-19 can be managed in the ICU without the need for emergent delivery. Overall goal oxygen saturation was >95%, in order to ensure adequate fetal oxygenation; our patient required nonrebreather, but never mechanical ventilation, to maintain that oxygen saturation.
Pregnancy is a hypercoagulable state with noted physiologic increases in D-dimer: 1 study demonstrated a median D-dimer of 553 ng/mL at week 35 of gestation, as well as a steady increase over the course of pregnancy [7]. COVID-19 has been associated with elevations in D-dimer and thrombus formation [8]. Our patient had an elevated D-dimer (Table 1) but no evidence of peripheral thrombi. Given underlying hypercoagulability in pregnancy and known venous thromboembolic complications associated with COVID-19, pregnant women positive for SARS-CoV-2 are placed on antepartum and postpartum venous thromboembolism prophylaxis; this was the case for our patient.
Our patient developed an elevated CRP and transaminitis. Both these lab abnormalities have been associated with SARS-CoV-2 infection; however, elevated CRP is also physiologic during pregnancy. Population-based studies have reported median CRP values in uncomplicated pregnancy ranging from 3 to 6 mg/L [9–11]. Thus, CRP may not be useful in determining the severity of COVID-19 illness in pregnant patients with COVID-19.
Regarding treatments, our patient received hydroxychloroquine and remdesivir. Hydroxychloroquine has been postulated to have some efficacy in COVID-19, although more recent data have called these hypotheses into question [12, 13]. At the time of our patient’s presentation, offering hydroxychloroquine was standard of care for patients admitted for COVID-19. More recent data have demonstrated a mortality benefit from dexamethasone in severe COVID-19 [14]. Dexamethasone crosses the placenta and is well studied in pregnancy. While long-term steroids are not recommended in pregnancy, the dexamethasone course for COVID-19 would not be considered long-term. In critically ill COVID-19 pregnant patients, any intervention to improve the maternal condition should be considered; dexamethasone is not contraindicated in pregnancy and should not be withheld if clinically indicated.
Remdesivir is a prodrug intracellularly metabolized into an adenosine triphosphate analog that inhibits viral RNA polymerase. After the emergence of SARS-CoV-2, in vitro testing demonstrated that remdesivir has activity against that virus; however, data on its use in pregnancy are limited. Manufacturer safety data indicate no reproductive developmental toxicity in animals at clinically relevant doses; embryonic toxicity was only noted when systemically toxic doses were administered to female animals before conception (Remdesivir Investigator’s Brochure, Gilead Sciences). Initial analysis of patients treated with compassionate use remdesivir demonstrated a low rate of adverse effects and possible mortality benefit [15]. The National Institutes of Health Adaptive COVID-19 Treatment Trial-1 (ACTT-1) study demonstrated that remdesivir was superior to placebo in decreasing time to recovery in hospitalized adults and may have mortality benefit [16]. However, neither of these studies included pregnant women. Our patient will be included in a forthcoming analysis of patients receiving remdesivir via an updated compassionate use protocol. Before COVID-19, an Ebola treatment study included remdesivir as 1 of 4 arms [17]; 6 of the 175 patients enrolled in that arm had a positive pregnancy test at the time of enrollment. No specific adverse outcomes in pregnant women were recorded in this arm of the study; however, the study report does not provide specific information regarding outcomes in these patients. In this case, our patient tolerated the medication well.
One of the noted side effects of remdesivir is transaminitis [15–17]. Remdesivir may further complicate interpretation of elevated liver enzymes in a population where they could represent pre-eclampsia, viral effect, or physiologic elevation. Our patient did develop an increase in her transaminases while on remdesivir; whether this was due to COVID-19 or to remdesivir is not clear. She had no proteinuria or hypertension to suggest pre-eclampsia as a cause of transaminitis.
All of the above points underscore the need for close interdepartmental collaboration in caring for pregnant patients presenting with COVID-19. For our patient, discussions between MFM, ID, and PCCM were vital in determining treatment course and level of care for our patient through her hospital course. The current paucity of data for remdesivir use in pregnancy underscores the importance of early inclusion of pregnant women in randomized clinical trials for the assessment of therapeutic agents.
Acknowledgments
Financial support. This patient was seen as part of routine clinical service at our institution. External funding did not play a role in her care.
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. COVID-19 Map. Johns Hopkins Coronavirus Resource Center Available at: https://coronavirus.jhu.edu/map.html. Accessed 23 July 2020.
- 2. Zaigham M, Andersson O. Maternal and perinatal outcomes with COVID-19: A systematic review of 108 pregnancies. Acta Obstet Gynecol Scand 2020; 99:823–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Breslin N, Baptiste C, Miller R, et al. Coronavirus disease 2019 in pregnancy: early lessons. Am J Obstet Gynecol MFM 2020; 2:100111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Liu Y, Chen H, Tang K, Guo Y. Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy [published online ahead of print, 2020 Mar 4]. J Infect 2020. doi: 10.1016/j.jinf.2020.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sutton D, Fuchs K, D’Alton M, Goffman D. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med 2020; 382:2163–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ellington S, Strid P, Tong VT, et al. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status - United States, January 22-June 7, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:769–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Murphy N, Broadhurst DI, Khashan AS, et al. Gestation-specific D-dimer reference ranges: a cross-sectional study. BJOG 2015; 122:395–400. [DOI] [PubMed] [Google Scholar]
- 8. Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood 2020; 135:2033–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Belo L, Santos-Silva A, Rocha S, et al. Fluctuations in C-reactive protein concentration and neutrophil activation during normal human pregnancy. Eur J Obstet Gynecol Reprod Biol 2005; 123:46–51. [DOI] [PubMed] [Google Scholar]
- 10. Ferguson KK, McElrath TF, Chen Y-H, Mukherjee B, Meeker JD. Longitudinal profiling of inflammatory cytokines and C-reactive protein during uncomplicated and preterm pregnancy. Am J Reprod Immunol 2014; 72: 326–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Perichart-Perera O, Muñoz-Manrique C, Reyes-López A, et al. Metabolic markers during pregnancy and their association with maternal and newborn weight status. PLoS One 2017; 12:e0180874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cavalcanti AB, Zampieri FG, Rosa RG, et al. Hydroxychloroquine with or without azithromycin in mild-to-moderate Covid-19 [published online ahead of print, 2020 Jul 23]. N Engl J Med 2020. doi: 10.1056/NEJMoa2019014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Satlin MJ, Goyal P, Magleby R, et al. Safety, tolerability, and clinical outcomes of hydroxychloroquine for hospitalized patients with coronavirus 2019 disease. PLoS One 2020; 15. doi: 10.1371/journal.pone.0236778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with Covid-19 - preliminary report [published online ahead of print, 2020 Jul 17]. N Engl J Med 2020. doi: 10.1056/NEJMoa2021436. [DOI] [Google Scholar]
- 15. Grein J, Ohmagari N, Shin D, et al. Compassionate Use of Remdesivir for Patients with Severe Covid-19. N Engl J Med 2020; 382:2327–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the Treatment of Covid-19 - Preliminary Report [published online ahead of print, 2020 May 22]. N Engl J Med 2020. doi: 10.1056/NEJMoa2007764. [DOI] [PubMed] [Google Scholar]
- 17. Mulangu S, Dodd LE, Davey RT Jr, et al. ; PALM Writing Group; PALM Consortium Study Team A randomized, controlled trial of Ebola virus disease therapeutics. N Engl J Med 2019; 381:2293–303. [DOI] [PMC free article] [PubMed] [Google Scholar]