Abstract
Introduction:
The purpose of this systematic review is to identify whether poor nutrition, as defined by the more commonly used markers of low albumin, low transferrin, or low total lymphocyte count (TLC), leads to more postoperative complications. We hypothesized that it may be possible to identify the levels of these laboratory values at which point total joint arthroplasty (TJA) may be ill advised. To this end, we analyzed the available literature regarding links between these three variables on postoperative complications after TJA.
Methods:
This systematic review was done in two parts: (1) In the first part, we reviewed the most commonly used malnutrition marker, albumin. (2) In the second part, we reviewed TLC and transferrin. We accessed PubMed, EMBASE, and Cochrane Library using relevant keywords to this study. The biostatistics were visualized using a random-effects forest plot. We compared data from all articles with sufficient data on patients with complications (ie, cases) and patients without complications (ie, noncases) among the two groups, malnourished and normal nutrition, from albumin, transferrin, and TLC data.
Results:
A meta-analysis of seven large-scale articles detailing the complications of albumin led to an all-cause relative risk increase of 1.93 when operating with hypoalbuminemia. This means that in the studies detailed enough to incorporate in this pooled analysis, operating on elective TJAs with low albumin is associated with a 93% increase in all measured complications. In the largest studies, analysis of transferrin levels for the most common complications revealed a relative risk increase of 2.52 when operating on patients with low transferrin levels. There were not enough subjects to do a biostatistical analysis in articles using TLC as the definition of malnutrition.
Conclusion:
The focus is on the trends rather than absolutes. As shown in Table 1, whether the albumin cutoff for albumin was 3.0 g/dL, 3.5 g/dL, or 3.9 g/dL, the trend remains the same. Because low albumin before TJAs tends to increase complications, it is recommended to incorporate albumin levels in preoperative workups. Many patients with hip and knee arthritis undergo months of conservative management (eg, physical therapy and corticosteroid injections) before considering surgery, and it would be wise to optimize their nutritional status in this period to minimize the risk of perioperative complications. The physician should use these data to provide informed consent of the increased risk to patients planning to undergo TJAs with elevated malnutrition markers. Because this research is retrospective in nature, albumin should be studied prospectively in hypoalbuminemic and normoalbuminemic patients and their postoperative outcomes should be measured. Regarding transferrin and TLC, future research should help elucidate their predictive value and determine the value of preoperatively optimizing them and their effect in mitigating postoperative complications.
Poor nutritional status before total joint arthroplasty (TJA) can lead to perioperative complications such as wound complications,1 infection,2-4 or even mortality.5,6 Despite general agreement with this statement, the primary metric by which malnutrition is demonstrated is less clear. Several laboratory markers have been suggested as indicative of poor nutritional status. Among these, the more commonly used markers are albumin,7 transferrin,8 and total lymphocyte count (TLC).1,9
The purpose of this systematic review is to identify whether poor nutrition, as defined by low albumin, low transferrin, or low TLC, leads to more postoperative complications. We hypothesized that it may be possible to identify the levels of these laboratory values at which point TJA may be ill advised. To this end, we analyzed the available literature regarding links between these three variables on postoperative complications after TJA.
Methods
This systematic review was done in two parts:
(1) In the first part, we reviewed the most commonly used malnutrition marker, albumin.
(2) In the second part, we reviewed TLC and transferrin.
During the first part, we accessed PubMed, EMBASE, and Cochrane Library using search phrases with the following keywords: “albumin,” “pre-albumin,” “prealbumin,” “total joint arthroplasty,” “total joint replacement,” “total hip arthroplasty,” “total hip replacement,” “total knee arthroplasty,” “total knee replacement,” “infection,” “complication,” “readmission,” “readmit, “postoperative,” and “perioperative.” This yielded 312 results in PubMed, 15 results in EMBASE, and 88 results in Cochrane Library. These titles were reviewed by independent reviewers. Pertinent English-language articles were considered for inclusion in the final review, as were all duplicates. Screening of the initial titles yielded 23 PubMed articles, five EMBASE articles, and one Cochrane Library article. Of these 29 titles, three were duplicates. One additional article was identified during the full-text article retrieval and was included in the systematic review, yielding a total of 30 articles related to albumin. We reviewed the following items in the 29 obtainable articles: year of publication, primary outcome, albumin cutoff level used to define hypoalbuminemia, patient source, sample size, follow-up duration, study design, complications evaluated, and relative risk (RR) of complications among patients with hypoalbuminemia. The resulting studies are listed in Tables 1–4 and Table 9.
Table 1.
Demographics of Albumin Studies
| Author Name | Study Population | Year | Mean Follow-up Time | Study Type | Hypoalbuminemic Cutoff | Normal Albumin Patient (Total) | Low Albumin Patient (Total) |
| Alfargieny et al2 | THA and TKA | 2015 | 6 mo | R | Not given | Not given | 5 |
| Bohl et al3 | THA and TKA | 2016 | 30 d | R | <3.5 g/dL | 47,639 | 1964 |
| Bohl et al10 | THA and TKA | 2016 | 30 d | R | <3.5 g/dL | 3762 | 755 |
| Courtney et al11 | THA and TKA | 2016 | 6 mo | R | <3.5 g/dL | 587 | 83 |
| Cross et al7 | Not applicable (N/A) | 2014 | N/A | N/A | N/A | N/A | N/A |
| Fu et al12 | THA | 2016 | 30 d | R | <3.5 g/dL | 19,465 | 745 |
| Fu et al5 | TKA | 2017 | 30 d | R | <3.5 g/dL | 33,400 | 1400 |
| Gherini et al8 | THA | Not given | Not given | P | Not given | Not given | Not given |
| Greene et al1 | THA and TKA | 1991 | 1 year | R | <3.5 g/dL | 211 | 6 |
| Gunningberg et al13 | THA, TKA, and coronary artery bypass | 2008 | 30 d | P | <35 g/L | 51 | 4 |
| Huang et al14 | THA and TKA | 2013 | 12 mo | P | Albumin <3.5 mg/dL OR transferrin <200 mg/dL | Not given | Not given |
| Kamath et al15 | THA and TKA | 2016 | Not given | P | <3.5 g/dL | 913 | 185 |
| Kamath et al6 | Revision TKA | 2017 | 30 d | R | <3.5 g/dL | 3838 | 713 |
| Kim et al16 | TKA | 2016 | 4.2 y | R | <3.0 g/dL | 839 | 470 |
| Lavernia et al17 | THA and TKA | 1999 | Not given | P | <or = 34 g/L | 97 | 22 |
| Marín et al9 | THA and TKA | 2002 | Not given | P | <3.5 g/dL | 152 | 18 |
| Mednick et al18 | THA | 2014 | 30 d | R | Not given | Not given | Not given |
| Morey et al19 | TKA | 2016 | 1 year | R | <3.5 g/dL | 2956 | 213 |
| Nelson et al4 | TKA | 2015 | 30 d | R | <3.5 g/dL | 35,573 | 1570 |
| Nelson et al20 | THA | 2019 | 30 d | R | <3.5 g/dL | 23,409 | 1177 |
| Nicholson et al21 | THA | 2012 | Not given | R | Albumin <3.5 g/dL AND TLC <1.50 cells/m | 64 | 26 |
| Nussenbaum et al22 | THA and TKA | 2018 | 2 y | R | Not given | Not given | Not given |
| Rai et al23 | THA and TKA | 2002 | Not given | R | Albumin <3.5 g/dL OR serum transferrin <200 mg/dL, OR TLC <1500 cells/mm3 | Not given | Not given |
| Savio et al24 | THA | 1996 | 1.8 y | R | Albumin <3.5 g/dL, then changed to albumin <3.9 g/dL is normal after the researchers analyzed the data | 51 | 35 |
| Walls et al25 | THA | 2015 | 30 d | R | <3.5 g/dL | 23,116 | 1122 |
| Yi et al26 | Revision THA | 2014 | 90 d | R | <3.5 g/dL | Not given | Not given |
Table 4.
Biostatistical Numbers Used to Decide Albumin RR
| Author | Normal Albumin Total | Normal Albumin Cases | Normal Albumin No cases | Low Albumin Total | Low Albumin Cases | Low Albumin No Cases | Explanation of Where Numbers Come Froma |
| Kim et al16 | 839 | 29 | 810 | 470 | 28 | 442 | AKI |
| Walls et al25 | 23,116 | 250 | 22,866 | 1122 | 33 | 1089 | Any major complication |
| Courtney et al11 | 587 | 48 | 539 | 83 | 23 | 60 | All complicationsb |
| Kamath et al6 | 3838 | 1740 | 2098 | 713 | 427 | 286 | Any complication |
| Bohl et al10 | 3353 | 69 | 3284 | 449 | 20 | 429 | PJI after revision for aseptic indicationc |
| Nelson et al4 | 35,573 | 506 | 35,067 | 1570 | 37 | 1533 | Any major complication |
| Kamath et al15 | 913 | 27 | 886 | 185 | 7 | 178 | Unplanned ICU admission |
ICU = intensive care unit; PJI = periprosthetic joint infection; RR = relative risk, AKI = acute kidney injury
Where in the articles the data were retrieved from.
The complication is the number of patients having a PJI after revision for an aseptic indication. Amount of albumin w/aseptic revisions = 3802 in Figure 1, which separates low albumin from norm albumin. The amount of normal albumin and low albumin w/complications is written in the last paragraph of the results section and is graphed out in Figure 3 of Bohl et al.10
Table 9.
Summary of Studies Using Transferrin or TLC as a Marker of Malnutrition
| Definition of Nutrition | Definition of Malnutrition | Amount of Studies Showing Significancea | Total No. of Patients With Notable Results | Complications Which Reached Significance |
| All parameters within normal limits | Low albumin or transferrin or TLC | 135 | 463 | Chronic septic failure and acute PJI complicating aseptic revision arthroplasty |
| Normal transferrin | Low transferrin | 027 | 3111 | Wound complicationsb |
| All parameters within normal limits | Low albumin or transferrin | 114 | 2161 | LOS, neurovascular, renal, hematoma/seroma, and any complications |
| Normal TLC | Low TLC | 117 | 101 | Cost/charges, anesthesia time, surgical time, in-hospital costs, and LOS |
| All parameters within normal limits | Low albumin or TLC | 22,19 | 3169 | Function score on the American Knee Society range of motion scale and19 low preoperative S. albumin associated with increased risk for SSIs2 |
PJI = periprosthetic joint infection; TLC = total lymphocyte count, LOS = length of stay
The superscript next to the number refers to the article in which the data were extracted in each associated row. It is not an exponent.
The single study showing significance did not list specific P-values, although it stated that a value of less than 0.05 was significant. It demonstrated, using percentages, that a low transferrin level led to an increased OR for wound complications. Although the study does not explicitly state that the data are significant, the words and the phrasing are highly suggestive of this.
Table 2.
Outcomes and Conclusions of Albumin Studies
| Author Name | Outcomes | Conclusions |
| Alfargieny et al2 | SSI | Perioperative albumin was a notable risk factor for SSI |
| Bohl et al3 | 30-day postoperative outcomes—wound dehiscence, deep vein thrombosis, and other | Patients with hypoalbuminemia had a higher risk of SSI, pneumonia, extended length of stay, and readmission |
| Bohl et al10 | Aseptic indications for revision arthroplasty, septic indications for revision arthroplasty, and PJI | Patients with hypoalbuminemia were three times as likely to have septic indication for revision arthroplasty as compared to patients with normal albumin levels. For those with aseptic indications for revision arthroplasty, patients with hypoalbuminemia had a risk of developing a PJI twice as great as those with normal albumin levels. |
| Courtney et al11 | Postoperative complications: cardiac, pulmonary, and other | Hypoalbuminemic patients were more likely to have a postoperative complication. Morbidly obese patients were more likely to be hypoalbuminemic than nonmorbidly obese patients. When comparing hypoalbuminemic morbidly obese patients with hypoalbuminemic nonmorbidly obese patients, no differences were observed in complication rates. When comparing morbidly obese patients with normal albumin to nonmorbidly obese patients, no differences were observed in complication rates. |
| Cross et al7 | N/A | N/A |
| Fu et al12 | Postoperative complications: cardiac (ie, myocardial infarction or cardiac arrest), septic (ie, sepsis or septic shock), and other | Malnutrition incidence increased markedly from obese I to obese III patients and was a stronger and more consistent predictor of complications after THA than was obesity. |
| Fu et al5 | Postoperative complications: wound (ie, superficial infection, deep SSI, organ space surgical site infection, or wound dehiscence) and other | Hypoalbuminemia was a more consistent independent predictor of complications after TKA than was obesity. |
| Gherini et al8 | Delayed wound healing | Only preoperative serum transferrin levels showed notable value in predicting which patients would have delayed wound healing. None of the other serologic variables, including serum albumin and TLC, proved to be a predictor of delayed wound healing. |
| Greene et al1 | Persistent serous drainage and wound dehiscence | Low albumin and low transferrin, independently or concurrently, were associated with more postoperative complications. |
| Gunningberg et al13 | Surgical wound infection | Low preoperative S-albumin was identified as the only notable predictor for surgical wound infection. |
| Huang et al14 | Complications: cardiovascular, neurovascular, and other | The incidence of complications was higher in malnourished patients than in nonmalnourished patients, regardless of whether they were obese. Renal complications were the most common complication experienced by malnourished patients and occurred at markedly higher rates than for nonmalnourished patients. Age was not a notable factor in developing malnutrition, but the incidence increased steadily through age 70. |
| Kamath et al15 | Unplanned postoperative intensive care unit admission | Patients with low albumin had a higher risk of unplanned postoperative intensive care unit admission. |
| Kamath et al6 | Mortality, superficial wound infection, and other | Patients in the low serum albumin group were statistically more likely to develop deep SSI, organ space SSI, and other complications. |
| Kim et al16 | Incidence of acute kidney injury, hospital stay, and overall mortality | Low albumin within two postoperative days was an independent risk factor for acute kidney injury and increased length of hospital stay in patients undergoing TKA. |
| Lavernia et al17 | Complications, resource consumption, length of stay, and number of in-hospital medical or surgical consults obtained | Patients with low albumin levels had higher charges, higher severity of illness, and longer length of stay. |
| Marín et al9 | Delayed wound healing | Preoperative lymphocyte count of less than 1500 cells/mm3 was associated with a three times greater frequency of healing complications, whereas preoperative serum albumin and transferrin levels had no notable predictive value. |
| Mednick et al18 | Readmission | The risk of readmission after THA increased with growing preoperative comorbidity burden. It specifically increased in patients with a body mass index of greater than or equal to 40 kg/m2, a history of corticosteroid use, and low preoperative serum albumin and in patients with postoperative SSI, a thromboembolic event, and sepsis. |
| Morey et al19 | Wound complications (ie, drainage, hemarthrosis, skin necrosis, and dehiscence) or PJI | Findings called into question the values of serum albumin level and TLC as a surrogate of malnutrition for predicting wound complications after TKA. |
| Nelson et al4 | Mortality, superficial wound infection, and other | Morbid obesity was not independently associated with most perioperative complications measured by the ACS-NSQIP and was associated only with increases in progressive renal insufficiency, superficial SSI, and sepsis among the 21 perioperative variables measured. Low serum albumin was associated with increased mortality and multiple additional major perioperative complications after TKA. Low serum albumin, more so than morbid obesity, was associated with major perioperative complications. |
| Nelson et al20 | Major complications, wound infections, and systemic infections | ORs increased or trended higher for all complications for albumin levels under 3.0 g/dL |
| Nicholson et al21 | Length of stay, intraoperative complications, and postoperative complications | The rate of malnourishment was marked higher in patients having trauma-related surgery than in those having elective surgery. Malnourished patients were at greater risk of prolonged hospital stay. |
| Nussenbaum et al22 | SSI, return to operating room, and other | The investigators saw a statistically significant decrease in both SSI and total complications after the implementation of preoperative screening criteria for elective TKA and THA. No single criterion was found to individually predict the complication and infection reductions. |
| Rai et al23 | Wound healing categories: normal/healthy scar after suture removal, delayed wound healing, and infected | Preoperative nutritional status was among several factors governing postoperative wound healing. Preoperative malnourishment as assessed by the low levels of serum albumin, serum transferrin, and TLC did not necessarily lead to delayed wound healing. Although several authors found high incidences of delayed wound healing and wound infection in malnourished patients, there were none in this study. The risk imposed by malnutrition on wound healing can be modified by surgeon-dependent factors. |
| Savio et al24 | Length of stay | Preoperative serum albumin was the only preoperative serum test associated with length of stay. Albumin was inversely related with length of stay. |
| Walls et al25 | Mortality, superficial incisional SSI, and other | Hypoalbuminemia was a notable risk factor for mortality and major morbidity among THA patients, whereas morbid obesity was only associated with an increased risk of superficial SSI. |
| Yi et al26 | Septic revision and aseptic revision | The presence of one or more laboratory parameters suggestive of malnutrition (ie, low albumin, low transferrin, and low lymphocyte count), although common in both normal weight and overweight patients, was independently associated with both chronic PJI and the development of an acute postoperative infection after an aseptic revision arthroplasty. |
ACS-NSQIP = the American College of Surgeons National Surgical Quality Improvement Program; OR = odds ratio; PJI = periprosthetic joint infection; SSI = surgical site infection; THA = total hip arthroplasty; TLC = total lymphocyte count.
We used a similar approach in the second part of the study, substituting the keywords “transferrin” and “total lymphocyte count.” There were 125 relevant article titles in PubMed, 108 relevant article titles in EMBASE, and three in Cochrane Library, totaling 236 relevant titles based on the question of interest. The same independent reviewers reviewed the titles, which yielded 66 relevant article abstracts. Of these 66, 54 full-text articles were selected after abstract evaluation. Including duplicates, 29 unique full-text articles were chosen for the final systematic review. On retrieval of the articles, we reviewed the following variables: primary outcome, secondary outcome, transferrin cutoff level used to define malnutrition, albumin cutoff level used to define hypoalbuminemia, TLC cutoff level used to define malnutrition, patient source, sample size, study design, and the number of cases and noncases among patients classified as normal nutrition and malnutrition. The resulting studies are listed in Tables 5–9.
Table 5.
Demographics of Transferrin Articles With Enough Subjects to Perform Pooled Analysis
Table 6.
Outcomes and Conclusions of Transferrin Studies
| Authors | Outcomes | Conclusions |
| Roche et al27 | Postoperative infection, wound complications, concomitant infection with wound complications, and infection after wound complications | Patients with lower values of nutritional markers had higher incidences, and hence, odds ratios of complications. |
| Huang et al14 | Multiple complications and length of stay | Malnutrition had higher rates of postoperative complications and length of stay. |
Table 7.
RR of Transferrin as Risk of Postoperative Complications
Table 8.
Biostatistical Numbers Used to Determine RR of Transferrin
| Author | Normal Transferrin Total | Normal Transferrin Cases | Normal Transferrin No Cases | Low Transferrin | Low Transferrin Cases | Low Transferrin No Cases | Explanation of Where Numbers Come From |
| Roche | 2339 | 240 | 2099 | 622 | 104 | 518 | Postoperative infection |
| Huang | 1977 | 58 | 1919 | 184 | 22 | 162 | Any complication |
RR = relative risk
The biostatistics were visualized using a random-effects forest plot. We compared data from all studies with sufficient data on patients with complications (ie, cases) and patients without complications (ie, noncases) among the two groups, normal albumin and hypoalbuminemia, to calculate a pooled RR combining the number of patients from all studies. A random-effects forest plot was also used to visualize information from the two studies with sufficient transferrin data.
Results
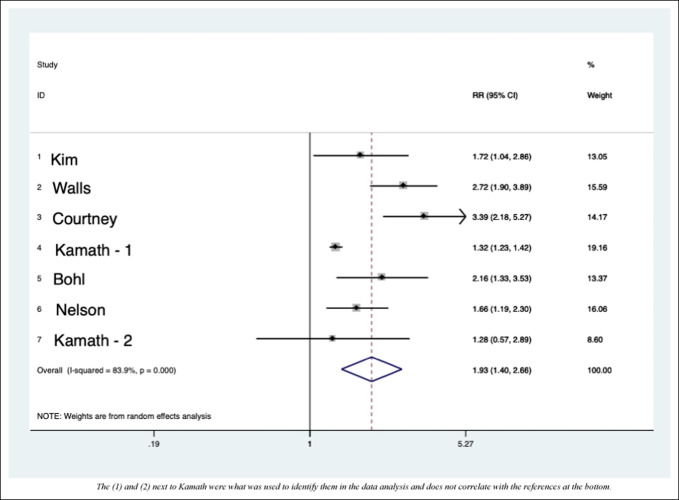
When determining which studies had adequate detail regarding the numbers of cases and noncases, we found that seven studies had sufficient data for inclusion in the pooled analysis (Figure 1 and Tables 3 and 4). For each of the seven included studies, we chose only the complication of interest, “major complications” or “any complication,” if presented.
Figure 1.
Graph showing the forest plot for the role of malnutrition in albumin articles based on studies with enough subjects. The (1) and (2) next to Kamath were what was used to identify them in the data analysis and does not correlate with the references at the bottom.
Table 3.
RR of Postoperative Complications of Albumin Levels
| Study | RR | Lower Limit CI | Upper Limit CI | % Weight |
| Kim et al16 | 1.724 | 1.038 | 2.861 | 13.05 |
| Walls et al25 | 2.720 | 1.901 | 3.890 | 15.59 |
| Courtney et al11 | 3.389 | 2.181 | 5.266 | 14.17 |
| Kamath et al6 | 1.321 | 1.232 | 1.416 | 19.16 |
| Bohl et al10 | 2.165 | 1.329 | 3.526 | 13.37 |
| Nelson et al4 | 1.657 | 1.191 | 2.304 | 16.06 |
| Kamath et al15 | 1.279 | 0.566 | 2.894 | 8.60 |
| D + L pooled RRa (P-value: < 0.001) | 1.933 | 1.401 | 2.665 | 100.00 |
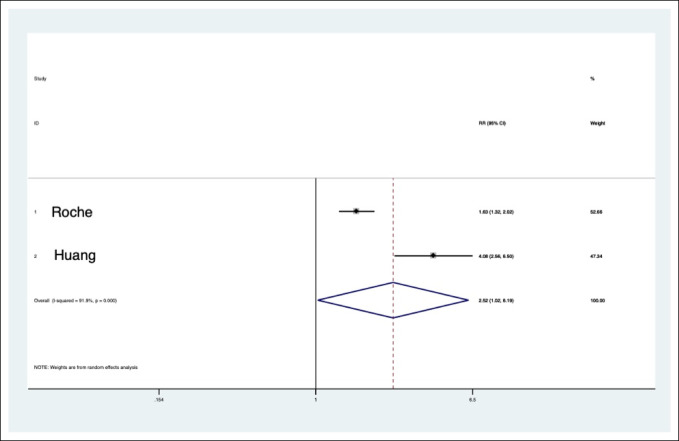
When malnutrition was defined as low transferrin, Roche et al27 identified an association with increased risk of postoperative infection (odds ratio [OR]: 1.87) and wound complications (OR: 1.9).
The study by Huang et al14 is the only study that describes malnutrition as low albumin or transferrin in the second half of the study. It found an increased length of stay (1.7 days), renal complications (OR: 2.85), and any complication (OR: 2.42).
Figure 2.
Graph showing the forest plot of transferrin articles.
The study by Yi et al26 is the only study that describes malnutrition as low albumin or transferrin or TLC in the second half of the study. It found an increased risk of chronic septic failure (OR: 2.13) and acute postoperative infection complicating an aseptic revision arthroplasty (OR: 5.9).
The study by Lavernia et al,17 the only study that describes malnutrition as low TLC in the second half of the study, found increased risks with increased cost/charges (P-value: 0.004), increased anesthesia time (P-value: 0.02), increase in surgical time (P-value: 0.002), increased in-hospital consults (P-value: 0.004), and increased length of stay (0.3 days).
The study by Morey et al,19 the only study that describes malnutrition as low albumin or TLC in the second half of the study, found the complication with increased risk was a decrease in range of motion in function score according to the American Knee Society scale (P-value: 0.009, amount of decrease in degrees: 1.5).
Meta-analysis of seven large-scale studies detailing the complications of albumin led to an all-cause RR increase of 1.93 when operating with hypoalbuminemia. This means that in the studies detailed enough to incorporate in this pooled analysis, operating on elective TJAs with low albumin is associated with a 93% increase in all measured complications. In the largest studies, analysis of transferrin levels for the most common complications revealed a RR increase of 2.52 when operating on patients with low transferrin levels. There were not enough subjects to do a biostatistical analysis in articles using TLC as the definition of malnutrition.
Discussion
Most of the articles use 3.5 g/dL as the cutoff for hypoalbuminemia, with the range varying from 3.0 to 3.9 g/dL (Table 1). In the studies isolating only albumin, hypoalbuminemia is associated with increased risk for postoperative complications. Based on this systematic review, sufficient evidence is not available to make a statement regarding the risk for postoperative complications in patients with malnutrition as defined by low transferrin or low TLC.
As shown in Table 9, one article isolated TLC and one article isolated transferrin as markers for malnutrition, with a maximum study cohort size of 3111. The other articles included albumin as a component of their definitions and did not separate out the patients with only low albumin, which makes it difficult to identify whether, in their patient cohorts, low transferrin alone or low TLC alone led to increased risks of complications. Although there is not enough conclusive evidence to state that transferrin or TLC levels alone warrant delaying an elective TJA, that does not mean low transferrin or TLC are not present when there is low albumin. The articles studying albumin along with TLC or transferrin do not describe the relationship between them and treat them only as separate, isolated cohorts. Therefore, we are not able to state that low TLC or transferrin levels tend to accompany low albumin levels. In addition, only one19 of the 27 unique articles isolating albumin claims that albumin is not a reliable test of choice for identifying malnutrition. Despite the variability in methodologies, with certain studies selecting from the American College of Surgeons National Surgical Quality Improvement Program3,5,10,12 and certain studies26 being performed by a single surgeon on a team to limit variability, albumin seems to lead to an increased risk of postoperative complications, including mortality, unplanned readmissions, and increased length of stay.
Conclusion
The focus is on the trends rather than absolutes. As shown in Table 1, whether the albumin cutoff for albumin was 3.0 g/dL, 3.5 g/dL, or 3.9 g/dL, the trend remains the same. Because low albumin before TJAs tends to increase complications, it is recommended to incorporate albumin levels in preoperative workups. Many patients with hip and knee arthritis undergo months of conservative management (eg, physical therapy and corticosteroid injections) before considering surgery, and it would be wise to optimize their nutritional status in this period to minimize the risk of perioperative complications. The physician should use these data to provide informed consent of the increased risk to patients planning to undergo TJAs with elevated malnutrition markers. Because this research is retrospective in nature, albumin should be studied prospectively in hypoalbuminemic and normoalbuminemic patients and their postoperative outcomes should be measured. Regarding transferrin and TLC, future research should help elucidate their predictive value and determine the value of preoperatively optimizing them and their effect in mitigating postoperative complications.
Footnotes
Dr. Sloan or an immediate family member serves as a paid consultant to KCI, Inc. Dr. Baldwin or an immediate family member has stock or stock options held in Pfizer. Dr. Kamath or an immediate family member has received IP royalties from Innomed; is a member of a speakers' bureau or has made paid DePuy, A Johnson & Johnson Company, and Zimmer; serves as a paid consultant to DePuy, A Johnson & Johnson Company, and Zimmer; has stock or stock options held in Johnson & Johnson, Procter & Gamble, and Zimmer; has received research or institutional support from Signature Orthopaedics; serves as a board member, owner, officer, or committee member of the AAOS, American Association of Hip and Knee Surgeons, and Anterior Hip Foundation. Dr. Nelson or an immediate family member serves as a paid consultant to Exactech, Inc, Zimmer-Biomet; serves as a board member, owner, officer, or committee member of the American Board of Orthopaedic Surgery, Inc., American Orthopaedic Association, and Knee Society. None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Mbagwu, Dr. Neuwirth, Dr. Charette, and Dr. Mason.
References
- 1.Greene KA, Wilde AH, Stulberg BN: Preoperative nutritional status of total joint patients. J Arthroplasty 1991;6:321-325. [DOI] [PubMed] [Google Scholar]
- 2.Alfargieny R, Bodalal Z, Bendardaf R, El-Fadli M, Langhi S: Nutritional status as a predictive marker for surgical site infection in total joint arthroplasty. Avicenna J Med 2015;5:117-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bohl DD, Shen MR, Kayupov E, Valle CJD: Hypoalbuminemia independently predicts surgical site infection, pneumonia, length of stay, and readmission after total joint arthroplasty. J Arthroplasty 2016;31:15-21. [DOI] [PubMed] [Google Scholar]
- 4.Nelson CL, Elkassabany NM, Kamath AF, Liu J: CORR Insights®: Low albumin levels, more than morbid obesity, are associated with complications after TKA. Clin Orthop Relat Res 2015;473:3163-3172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fu MC, Mclawhorn AS, Padgett DE, Cross MB: Hypoalbuminemia is a better predictor than obesity of complications after total knee arthroplasty: A propensity score-adjusted observational analysis. HSS J 2016;13:66-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kamath AF, Nelson CL, Elkassabany N, Guo Z, Liu J: Low albumin is a risk factor for complications after revision total knee arthroplasty. J Knee Surg 2016;30:269-275. [DOI] [PubMed] [Google Scholar]
- 7.Cross MB, Yi PH, Thomas CF, Garcia J, Valle CJ: Evaluation of malnutrition in orthopaedic surgery. J Am Acad Orthop Surg 2014;22:193-199. [DOI] [PubMed] [Google Scholar]
- 8.Gherini S, Vaughn BK, Lombardi AV, Mallory TH: Delayed wound healing and nutritional deficiencies after total hip arthroplasty. Clin Orthop Relat Res 1993;293:188-195. [PubMed] [Google Scholar]
- 9.Marín LA, Salido JA, López A, Silva A: Preoperative nutritional evaluation as a prognostic tool for wound healing. Acta Orthop Scand 2002;73:2-5. [DOI] [PubMed] [Google Scholar]
- 10.Bohl DD, Shen MR, Kayupov E, Cvetanovich GL, Valle CJD: Is hypoalbuminemia associated with septic failure and acute infection after revision total joint arthroplasty? A study of 4517 patients from the National Surgical Quality Improvement Program. J Arthroplasty 2016;31:963-967. [DOI] [PubMed] [Google Scholar]
- 11.Courtney PM, Rozell JC, Melnic CM, Sheth NP, Nelson CL: Effect of malnutrition and morbid obesity on complication rates following primary total joint arthroplasty. J Surg Orthop Adv 2016;25:99-104. [PubMed] [Google Scholar]
- 12.Fu MC, Dambrosia C, Mclawhorn AS, Schairer WW, Padgett DE, Cross MB: Malnutrition increases with obesity and is a stronger independent risk factor for postoperative complications: A propensity-adjusted analysis of total hip arthroplasty patients. J Arthroplasty 2016;31:2415-2421. [DOI] [PubMed] [Google Scholar]
- 13.Gunningberg L, Persson C, Åkerfeldt T, Stridsberg M, Swenne CL: Pre- and postoperative nutritional status and predictors for surgical-wound infections in elective orthopaedic and thoracic patients. Eur J Clin Nutr Metab 2008;3:E93-E101. [Google Scholar]
- 14.Huang R, Greenky M, Kerr GJ, Austin MS, Parvizi J: The effect of malnutrition on patients undergoing elective joint arthroplasty. J Arthroplasty 2013;28:21-24. [DOI] [PubMed] [Google Scholar]
- 15.Kamath AF, McAuliffe CL, Kosseim LM, Pio F, Hume E: Malnutrition in joint arthroplasty: Prospective study indicates risk of unplanned ICU admission. Arch Bone Joint Surg 2016;4:128-131. [PMC free article] [PubMed] [Google Scholar]
- 16.Kim HJ, Koh WU, Kim SG, et al. : Early postoperative albumin level following total knee arthroplasty is associated with acute kidney injury. Medicine 2016;95:e4489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lavernia CJ, Sierra RJ, Baerga L: Nutritional parameters and short term outcome in arthroplasty. J Am Coll Nutr 1999;18:274-278. [DOI] [PubMed] [Google Scholar]
- 18.Mednick RE, Alvi HM, Krishnan V, Lovecchio F, Manning DW: Factors affecting readmission rates following primary total hip arthroplasty. J Bone Joint Surg Am Vol 2014;96:1201-1209. [DOI] [PubMed] [Google Scholar]
- 19.Morey VM, Song YD, Whang JS, Kang YG, Kim TK: Can serum albumin level and total lymphocyte count be surrogates for malnutrition to predict wound complications after total knee arthroplasty? J Arthroplasty 2016;31:1317-1321. [DOI] [PubMed] [Google Scholar]
- 20.Nelson CL, Kamath AF, Elkassabany NM, Guo Z, Liu J: The serum albumin threshold for increased perioperative complications after total hip arthroplasty is 3.0 g/dL. Hip Int 2018;29:166-171. [DOI] [PubMed] [Google Scholar]
- 21.Nicholson JA, Dowrick AS, Liew SM: Nutritional status and short-term outcome of hip arthroplasty. J Orthop Surg 2012;20:331-335. [DOI] [PubMed] [Google Scholar]
- 22.Nussenbaum FD, Rodriguez-Quintana D, Fish SM, Green DM, Cahill CW: Implementation of preoperative screening criteria lowers infection and complication rates following elective total hip arthroplasty and total knee arthroplasty in a veteran population. J Arthroplasty 2018;33:10-13. [DOI] [PubMed] [Google Scholar]
- 23.Rai J, Gill SS, Kumar BR: The influence of preoperative nutritional status in wound healing after replacement arthroplasty. Orthopedics 2002;25:417-421. [DOI] [PubMed] [Google Scholar]
- 24.Savio GCD, Zelicof SB, Wexler LM, et al. : Preoperative nutritional status and outcome of elective total hip replacement. Clin Orthop Relat Res 1996;326:153-161. [DOI] [PubMed] [Google Scholar]
- 25.Walls JD, Abraham D, Nelson CL, Kamath AF, Elkassabany NM, Liu J: Hypoalbuminemia more than morbid obesity is an independent predictor of complications after total hip arthroplasty. J Arthroplasty 2015;30:2290-2295. [DOI] [PubMed] [Google Scholar]
- 26.Yi PH, Frank RM, Vann E, Sonn KA, Moric M, Valle CJD: Is potential malnutrition associated with septic failure and acute infection after revision total joint arthroplasty? Clin Orthop Relat Res 2014;473:175-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Roche M, Law TY, Kurowicki J, et al. : Albumin, prealbumin, and transferrin may be predictive of wound complications following total knee arthroplasty. J Knee Surg 2018;31:946-951. [DOI] [PMC free article] [PubMed] [Google Scholar]