Abstract
This study was performed to examine the epidemiological features of maxillofacial fracture, including the incidence, causes, age and sex distribution, methods of treatment, and prognosis, in a local area.
A retrospective study was performed to investigate the epidemiological characteristics of 829 patients with maxillofacial fractures treated in a hospital in northern China from August 2011 to July 2019. Sex, age, etiology, fracture site, and treatment method were obtained from the medical records.
The average age of all 829 patients was 36.1 years, and most patients were in the 20- to 29-year age group. The male to female ratio was 3.04:1.00. Traffic accidents were the main cause of the maxillofacial fractures. The mandible was the most commonly fractured bone, and the parasymphysis was the most frequently affected site. Head injury was the most common associated injury. Open surgery with internal fixation was the first-choice treatment for most cases.
Traffic accidents were the main cause of maxillofacial fractures, followed by falling. Open surgery with internal fixation was the leading treatment choice. Both functional and esthetic outcomes should be considered in the treatment of maxillofacial fractures
Keywords: epidemiology, internal fixation, mandibular fracture, maxillofacial fracture, retrospective study, traffic accident
1. Introduction
Because of the specific anatomical features of the face, maxillofacial fractures are commonly seen in patients with facial trauma such as nasal fractures, jaw fractures, and eye injuries.[1] Facial trauma often leads to functional, esthetic, and psychological problems with resultant social and economic burdens.[2] With the rapid development of the economy and the increase in social activities, the incidence of facial fractures in China is rising. The risk factors for maxillofacial fractures include age and sex, and the etiology varies depending on different geographical, social, cultural, economic, and environmental factors.[3] Considering the complexity of the geographic environment in China, the patterns of facial fractures in different regions of this country need to be studied. A better understanding of the epidemiologic features of fractures can help to promote the implementation of effective preventive actions and improve the clinical treatment.[4] However, studies on the epidemiological features of maxillofacial fractures in China are still lacking. Therefore, the present retrospective study was performed to analyze the epidemiologic features and treatments of such fractures in a metropolitan urban area in northern China.
According to previous studies,[2] traffic accidents and violence are considered the most common causes of maxillofacial fractures in developing and developed countries, respectively.[5] The mandible is the primary bone involved in maxillofacial fractures. Some studies have demonstrated that in terms of prevalence, the condyle and parasymphysis are the most commonly affected sites in patients with mandibular fractures.[5] The treatment of maxillofacial fractures includes both conservative and surgical methods. Because maxillofacial trauma often leads to morbidity and disability, treatment and rehabilitation should be performed with consideration of the psychological and esthetic effects.[6] Furthermore, maxillofacial fractures are usually costly to treat because of both direct costs such as the cost of surgery as well as indirect costs such as time away from work. As a result, maxillofacial trauma is a serious burden on individuals and society.[7]
China is the third largest country by area and possesses the largest portion of the worldwide population. The differences in geographic features among various regions of China not only affect the cultural, economic, and social features of maxillofacial fractures but also affect the patterns of such fractures. The city of Shenyang, where the present study took place, is a central city in the northernmost part of China that is characterized by the coldest weather and shortest daytime. As a result, it has a distinct pattern of facial fractures compared with other areas. For example, the incidence of alcohol intoxication-related facial fractures is higher than that in other areas, especially during the night. This unique feature of facial fractures may be due to the cold weather and long night time. A better understanding of epidemiological patterns may help to allocate health care resources in a more reasonable and fair manner to facilitate the prevention and control of these fractures. In the present study, we retrospectively analyzed the data of patients with maxillofacial fractures treated in a hospital in northern China. The age, sex, etiology, fracture sites, associated injuries, treatments, and outcomes of these patients were investigated and compared.
2. Materials and methods
This retrospective study covered an 8-year time period. All data were collected from the medical records of patients with facial fractures treated at the Department of Oral and Maxillofacial Surgery of Shengjing Hospital, China Medical University, Shenyang, China from August 2011 to July 2019. All patients were evaluated by oral and maxillofacial surgeons, and the findings of clinical and radiographic examinations (mainly computed tomography) were used as evidence for diagnosis. The exclusion criteria were incomplete medical records, the performance of other procedures such as removing a plate from a previous surgery, and immediate treatment on an outpatient basis without hospitalization.
The patients’ medical records were analyzed for the following data:
-
(1)
age and sex;
-
(2)
cause of the trauma (traffic accident, fall, violence, industrial injury, sports injury, or blast injury);
-
(3)
fracture site (mandible, orbital region, maxilla, or zygomatic complex);
-
(4)
associated injuries (head injury, limb injury, chest and abdominal injury, visual dysfunction, or cervical vertebra injury); and
-
(5)
treatment [open reduction with internal fixation (ORIF) alone, ORIF combined with intermaxillary fixation (IMF), conservative treatment, or open reduction only].
The fracture type and patient's condition were considered when choosing the treatment method. After the surgery, the patients received antibiotic treatment and specific oral hygiene care. An antibiotic oral mouth rinse was given to the patients three times a day.
Epidemiological data, including age, sex, cause of injury, fracture site, and treatment method, were recorded and analyzed. All data in this study were analyzed by SPSS 16.0 (SPSS Inc., Chicago, IL). The statistical significance of differences between parameters was evaluated with the chi-square test. The significance level was set at P < .05.
The protocols were approved by the Clinical Research Ethics Committee of Shengjing Hospital of China Medical University. All methods were carried out in accordance with relevant guidelines and regulations. The patient's medical records remain completely confidential.
3. Results
3.1. Age and sex
In total, 829 patients with maxillofacial fractures treated from August 2011 to July 2019 were included in this study. Among these patients, 624 (75.27%) were men and 205 (24.73%) were women (male: female ratio, 3.04:1.00). Their average age was 36.1 years (range, 1–89 years). The highest incidence of maxillofacial fracture occurred in the 20- to 29-year age group (21.71%) (Table 1). As shown in Figure 1, the incidence of maxillofacial fracture remained quite stable throughout the 8-year study period. The patients’ demographic profile also remained consistent, and most of the patients were male. During the last year, the female: male ratio was slightly higher than that in other years. The mean age of the patients increased from 34.03 to 37.29 years during the 8-year study period, but the increase was not statistically significant.
Table 1.
The age and gender distribution.
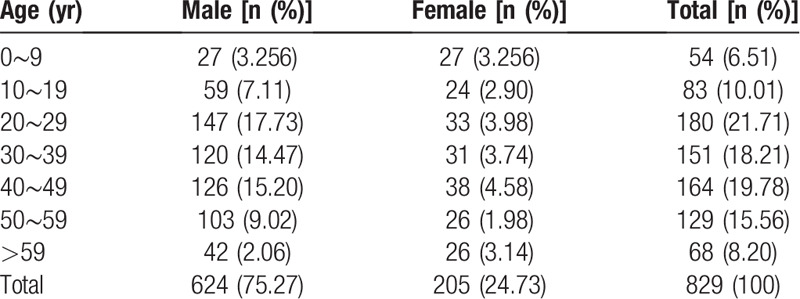
Figure 1.
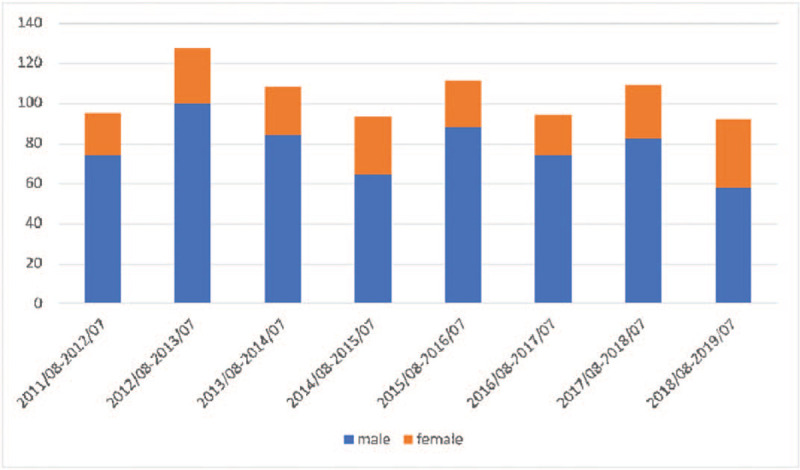
Incidence of maxillofacial fracture.
3.2. Etiology
The causes of maxillofacial fractures included traffic accidents, falls, violence, sports injuries, and blast injuries. Traffic accidents were the most common cause of maxillofacial fractures with 379 cases (45.72%), followed by falls with 256 cases (30.88%). Industrial injuries and violence accounted for 5.91% and 8.68%, respectively. Sport injuries, blast injuries, and crash injuries accounted for 73 cases (8.81%). The etiology pattern varied among the different age groups. However, traffic accidents were still the main cause among all age groups (Table 2). The incidence rates for different types of traffic accidents are summarized as follows: car accident, n = 188 (49.6%); motorcycle accident, n = 140 (36.9%); and bicycle accident, n = 51 (13.5%). Analysis of the etiology in terms of sex showed that traffic accidents and falls were the leading causes of maxillofacial fracture in both male and female patients (Fig. 2). The highest incidence rate of violence-related maxillofacial fractures occurred in the 19- to 29-year age group, and industrial injury-related fractures mostly occurred in middle-aged patients (40–49 years of age). Traffic accidents as a cause of fractures significantly increased during the 8-year study period (from 44.04% in the first 4 years to 47.04% in the last 4 years, P = .034). Falling as a cause of maxillofacial fractures also significantly increased from 22.93% to 26.35% (P = .028). Among patients involved in traffic accidents, there was a significant decrease in the proportion of male patients (from 72.34% in the first 4 years to 68.59% in the last 4 years, P = .023) but a significant increase in the proportion of female patients (from 27.66% to 31.41%, P = .018). The proportions of male and female patients in the falling group remained steady throughout the study.
Table 2.
The etiology distribution of maxillofacial fracture.
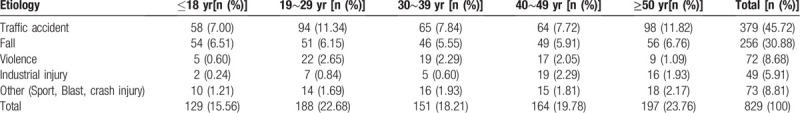
Figure 2.
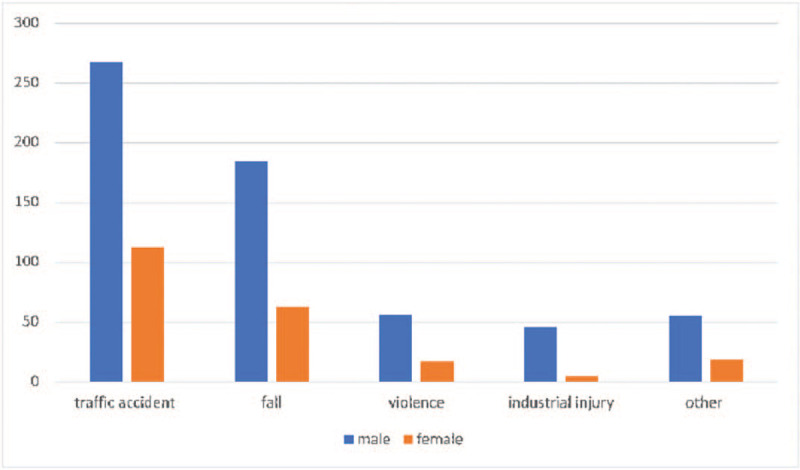
Sex-related pattern of the causes of maxillofacial fracture.
3.3. Fracture site
There were 1486 fracture sites among the 829 patients, meaning that each patient had 1.79 fracture sites. Mandibular fractures were the most common, affecting 389 patients (47%) and accounting for 588 sites (40%). The next most common site was the orbital bone, affecting 242 patients (30%) and accounting for 435 sites (29%). Among orbital fractures, lower rim and floor fractures were the most commonly seen (n = 197, 13.26%), followed by fractures of the medial wall (n = 140, 9.42%) and lateral wall (n = 98, 6.59%). In total, 241 (29%) patients had maxillary fractures and 222 (27%) had zygomatic fractures. Among the patients with mandibular fractures, the parasymphysis was the most commonly affected site, and the next most common was the condyle. Among the patients with maxillary fractures, 32 had Le Fort type I fractures, 59 had Le Fort type II, and 28 had Le Fort type III (Table 3). In terms of the etiological distribution of the maxillofacial fracture sites, road traffic accidents were the main cause of fractures at any site. As shown in Figure 3, falling was the cause of mandibular fractures in a significantly higher proportion of cases (P = .029), and violence was the cause of zygomatic fractures in a significantly higher proportion of cases (P = .017). Notably, the mandibular third molar is a proven risk factor for mandibular angle fractures and has a relationship with condyle fractures.
Table 3.
Injury sites of maxillofacial fractures.
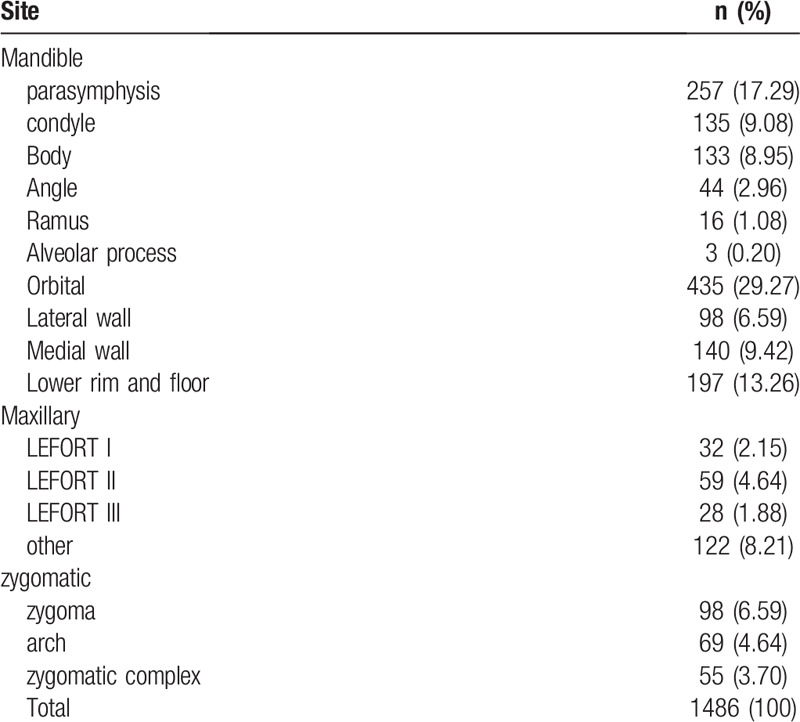
Figure 3.
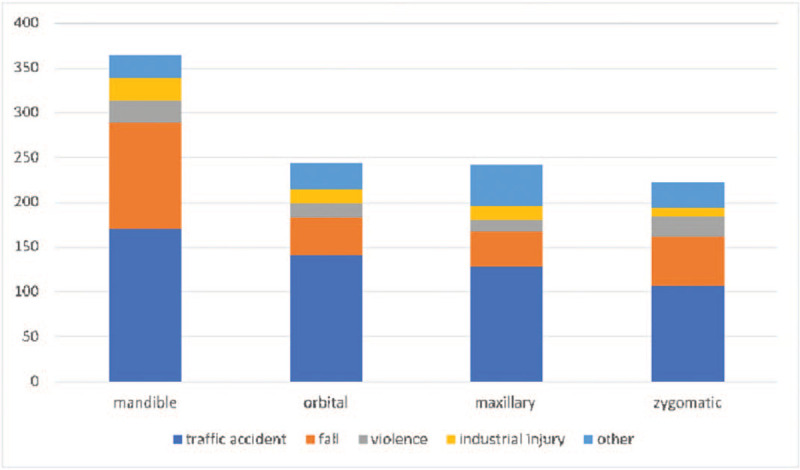
Distribution of etiologies at different fracture sites.
3.4. Associated injuries
Head injuries were found in 154 (19%) of the 829 patients and were the most common associated injury of maxillofacial fractures. The next most common associated injures were limb injuries (n = 142, 17%), chest and abdominal injuries (n = 129, 16%), visual dysfunction (n = 92, 11%), and cervical vertebra injuries (n = 35, 4%) (Fig. 4).
Figure 4.
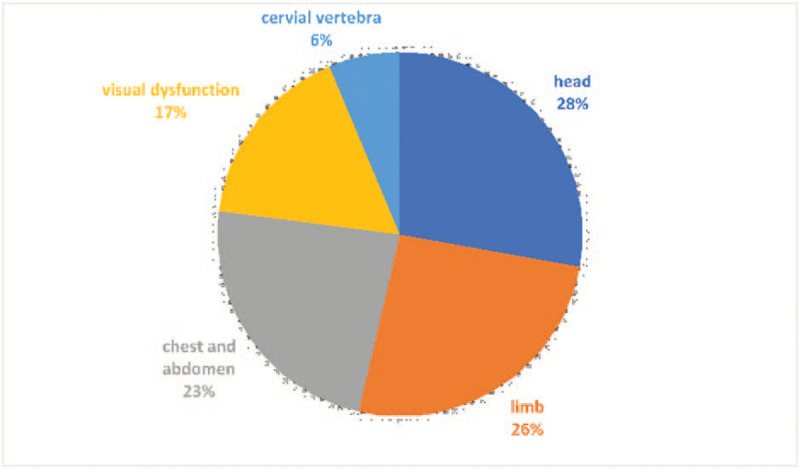
Distribution of associated injuries.
3.5. Treatment
Among the 829 patients, 287 (35%) were treated with ORIF alone, 261 (31%) were treated with ORIF combined with IMF, 142 (17%) received conservative treatment, and 35 (4%) were treated with open reduction alone (Fig. 5). Conservative treatment was mostly performed for zygomatic fractures and condyle fractures; 23.5% of zygomatic fractures and 35.0% of condyle fractures were treated conservatively. Most of the mandibular and orbital fractures were treated by ORIF. Most condyle fractures in pediatric patients were treated conservatively.
Figure 5.
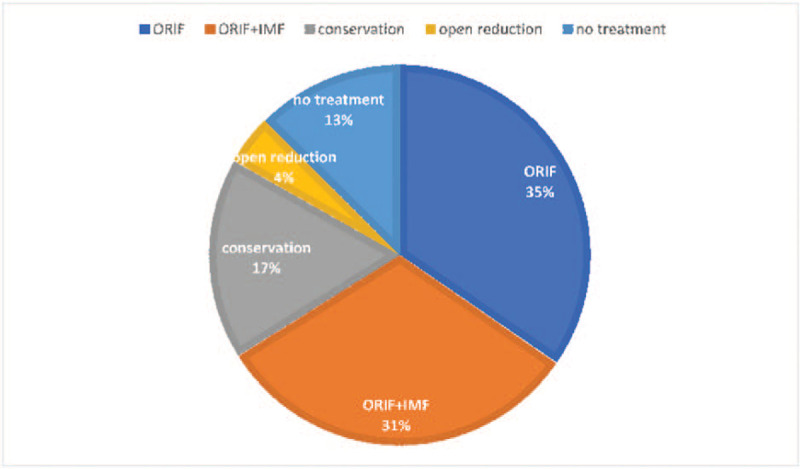
Distribution of treatment methods. ORIF = open reduction with internal fixation, IMF = intermaxillary fixation.
4. Discussion
Many patients are transferred or referred to Shengjing Hospital of China Medical University because of its favorable location and advanced medical devices. In total, 829 patients with maxillofacial fractures were treated in our department from August 2011 to July 2019. In this retrospective study, we obtained useful epidemiological information by analyzing the medical records of these patients. Such an investigation can help us to improve our treatment and more effectively manage facial trauma.
The incidence rate of maxillofacial trauma has been rising in recent years worldwide.[8] Maxillofacial trauma has a higher morbidity rate than other types of trauma because the facial region is an exposed and unprotected region.[9] Most maxillofacial fractures occur in young adults, usually causing occlusal function problems, facial disfigurement, facial paralysis, and visual and hearing problems. As a result, maxillofacial fractures and their complications may seriously affect patients’ quality of life and lead to great social and economic burdens.[9]
The epidemiological features of fractures are influenced by many factors, including demographic, social, economic, and cultural factors.[10] In the present study, we retrospectively analyzed the data of 829 patients from Shenyang and surrounding cities to elucidate the epidemiological pattern of maxillofacial fractures. From August 2011 to July 2019, the incidence of maxillofacial fractures remained steady. There was no significant change in the demographic profile each year, and most of the patients with facial fractures were men. The mean age of the patients increased during the 8-year study period, but not significantly. Excluding other possible reasons, the whole- population aging trend might be a plausible explanation for this observation.
The highest incidence of maxillofacial fractures in this study occurred among patients aged 20 to 29 years, and the male to female ratio was 3.04:1.00. These observations are consistent with those in previous studies.[11,12] The higher proportion of affected men may be explained by men, when compared with women, being generally engaged in more social activities and are more likely to be involved in violent incidents and high-risk driving.[13,14]
Road traffic accidents were the main cause of maxillofacial fractures, which is consistent with most studies from different countries.[2,9,13] The major risk factors for road traffic accidents are speeding, drunk driving, and failure to follow traffic laws. During the study period, the incidence of maxillofacial fractures caused by motorcycle and bicycle accidents decreased, while increasingly more fractures were caused by car accidents. Violence and falls were also considered to be main causes of maxillofacial fractures in this study, although they had a lower incidence rate. Notably, recent studies have shown that in developed countries such as the United Kingdom, violence and falls were found to be the main etiologies instead of road traffic accidents.[14] The reason for this may be that economic development, traffic law enforcement, road safety measures, and the sense of road safety among citizens still require more improvement in developing than developed countries.[15] Because of the construction activities in cities, industrial injuries were another common cause of maxillofacial fractures. Analysis of age showed that traffic accidents and falling were the leading causes of facial fractures regardless of age. Analysis of sex showed that most affected patients were male regardless of etiology. Especially in the industrial injuries group, the female: male ratio was significantly lower than that in the other groups. Considering that women are much less often involved in industrial activities than are men, women's lower exposure to risk factors might be a reason for the observed lower incidence rate of maxillofacial fractures in female patients.
In the present study, mandibular fractures were the most common type of maxillofacial fractures, which is consistent with previous studies in China and other countries.[4,5,10,13,16] The orbital bone was the second most common fracture site in this study, consistent with a study by Cagatay et al.[17] This is because the orbital bone is too weak to resist external forces considering its anatomic features. The medial orbital wall and orbital floor are considered the weakest areas of the orbital bone. The mandibular fractures in this study occurred at the parasymphysis, condyle, and body. The mandibular fracture sites were strongly related to the cause of the injury and the direction of the force. Parasymphysis fractures had the highest incidence in this study, which is consistent with previous studies.[18,19] However, other studies have shown that the condyle was the most common site of mandibular fractures.[20,21] Among zygomatic fractures, violence was the most common cause. This might be explained by the features of interpersonal violence.
Most of the midfacial fractures occurred in the maxilla, which is in accordance with previous studies.[22,23] Traffic accidents caused most of the midfacial fractures in this study. Le Fort type II fractures are the most common type of maxillary fractures.[24] However, because of the complexity of the injury, typical Le Fort type II fractures are uncommon in the clinical setting.
The most common type of associated injuries were head injuries, which is in accordance with a study by Obimakinde et al[22] but contrary to the findings of Chen et al.[25] Some studies have shown that limb injuries or orthopedic injuries were the most common associated injuries, indicating that the associated injuries vary in different areas.[8]
ORIF combined with IMF was the primary treatment modality in this study, which is consistent with other findings.[26] Previous studies have shown that ORIF and IMF are still the standard treatments and are effective management methods for maxillofacial fractures.[27] ORIF can provide stable and precise anatomical reduction of fracture fragments, facilitating more rapid bone healing and functional recovery.[8] Open reduction without internal fixation was used in 35 cases, all of which were zygomatic fractures. A total of 142 patients underwent conservative treatment, and 104 patients received no treatment for financial and subjective reasons. The choice of treatment method is mainly based on the patient's condition and type of fracture. The patient's subjective desires and economic factors are also considered. In pediatric and advanced-age patients, conservative treatment and closed reduction were the most commonly used treatment methods. In pediatric patients, ORIF may increase the risk of developmental asymmetry, which may limit the use of ORIF. Similarly, the limited systemic health condition and the decreased recovery capacity of advanced-age patients may also limit the use of ORIF.[28,29]
This retrospective study had some limitations. First, in the classification of etiologies, only the main etiology was considered. However, some patients had more than one cause of facial fracture. For example, a road traffic accident could have occurred while a man was in a working situation. In this study, however, such cases were only classified as traffic accidents, not work-related or industrial accidents. Second, in the classification of treatments, only the treatment for the main fracture site was used in the analysis. For example, when fractures occurred in both the mandibular body and condyle, ORIF for treatment of the mandibular body fracture was used as the classification; the conservative treatment for the condylar fracture was not. Moreover, because ours is a large tertiary-care hospital, we encountered many complex facial fractures, and the patients’ conditions may not typical of the general population.
5. Conclusion
Maxillofacial fractures have become a serious health problem in China in recent years. Such fractures lead to serious physical and physiological problems and great social and economic burdens. In the present study, the epidemiological features of maxillofacial fractures demonstrated a strong correlation with age, sex, and etiology. As the first investigation of the epidemiological features of maxillofacial fractures in Shenyang, this study may improve our knowledge of the incidence rate and characteristics of maxillofacial fractures in high-latitude regions and shed new light on how to organize emergency care in a more reasonable way.
Author contributions
Conceptualization: Xiaodong Liu, Qiuxu Wang, Weixian Liu.
Data curation: Xiaodong Liu.
Formal analysis: Xiaodong Liu.
Funding acquisition: Xiaodong Liu.
Investigation: Xiaodong Liu.
Methodology: Xiaodong Liu.
Project administration: Xiaodong Liu.
Resources: Xiaodong Liu.
Software: Xiaodong Liu.
Supervision: Xiaodong Liu.
Validation: Xiaodong Liu.
Visualization: Xiaodong Liu.
Writing – original draft: Xiaodong Liu.
Writing – review & editing: Xiaodong Liu.
Footnotes
Abbreviations: IMF = intermaxillary fixation, ORIF = open reduction and internal fixation, RTA = road traffic accident.
How to cite this article: Xiao-Dong L, Qiu-Xu W, Wei-Xian L. Epidemiological pattern of maxillofacial fractures in northern China: A retrospective study of 829 cases. Medicine. 2020;99:9(e19299).
The authors have no funding and conflicts of interest to disclose.
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
- [1].Andreas ZJ, Benoit S, Olivier L, et al. Incidence, aetiology and pattern of mandibular fractures in central Switzerland. Swiss Med Wkly 2011;141:132–7. [DOI] [PubMed] [Google Scholar]
- [2].Oginni FO, Oladejo T, Alake DP. Facial bone fractures Inile-Ife, Nigeria: an update on pattern of presentation and care. J Maxillofac Oral Surg 2016;15:184–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].van Beek GJ, Merkx CA. Changes in the pattern of fractures of the maxillofacial skeleton. Int J Oral Maxillofac Surg 1999;286:424–8. [DOI] [PubMed] [Google Scholar]
- [4].Hogg NJ, Stewart TC, Armstrong JE, et al. Epidemiology of maxillofacial injuries at trauma hospitals in Ontario, Canada, between 1992 and 1997. J Trauma 2000;49:425–32. [DOI] [PubMed] [Google Scholar]
- [5].Iida S, Kogo M, Sugiura T, et al. Retrospective analysis of 1502 patients with facial fractures. Int J Oral Maxillofac Surg 2001;30:286–90. [DOI] [PubMed] [Google Scholar]
- [6].Wittchen HU, Jacobi F, Rehm J, et al. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsych Pharmacol 2011;21:655–79. [DOI] [PubMed] [Google Scholar]
- [7].Nalliah RP, Allareddy V, Kim MK, et al. Economics of facial fracture reductions in the United States over 12 months. Dent Traumatol 2013;29:115–20. [DOI] [PubMed] [Google Scholar]
- [8].Samieirad S, Tohidi E, Shahidi-Payam A, et al. Retrospective study maxillofacial fractures epidemiology and treatment plans in Southeast of Iran. Med Oral Patol Oral Cir Bucal 2015;20:e729–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Smith H, Peek-Asa C, Nesheim D, et al. Etiology, diagnosis, and characteristics of facial fracture at a midwestern level I trauma center. J Trauma Nurs 2012;19:57–65. [DOI] [PubMed] [Google Scholar]
- [10].Brucoli M, Boffano P, Pezzana A, et al. The “European Mandibular Angle” research project: the analysis of complications after unilateral angle fractures. Oral Surg Oral Med Oral Pathol Oral Radiol 2019;128:14–7. [DOI] [PubMed] [Google Scholar]
- [11].Obuekwe ON, Ojo MA, Akpata O, et al. Maxillofacial trauma due to road traffic accidents in Benin City, Nigeria. A prospective study. Ann Afr Med 2004;2:58–63. [Google Scholar]
- [12].Chrcanovic BR. Factors influencing the incidence of maxillofacial fractures. J Oral Maxillofac Surg 2012;16:3–17. [DOI] [PubMed] [Google Scholar]
- [13].Adeyemo WL, Ladeinde AL, Ogunlewe MO, et al. Trends and characteristics of oral and maxillofacial injuries in Nigeria: a review of the literature. Head Face Med 2005;1:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Agnihotri A, Galfat D, Agnihotri D. Incidence and pattern of maxillofacial trauma due to road traffic accidents: a prospective study. J Maxillofac Oral Surg 2014;13:184–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Sakr K, Farag IA, Zeitoun IM. Review of 509 mandibular fractures treated at the University Hospital, Alexandria, Egypt. Br J Oral Maxillofac Surg 2006;44:107–11. [DOI] [PubMed] [Google Scholar]
- [16].Munante-Cardenas JL, Facchina Nunes PH, Passer LA. Etiology, treatment, and complications of mandibular fractures. J Craniofac Surg 2015;26:611–5. [DOI] [PubMed] [Google Scholar]
- [17].Cagatay HH, Ekinci M, Pamukcu C, et al. Retrospective analysis of 132 patients with orbital fracture. Ulus Travma Acil Cerrahi Derg 2013;19:449–55. [DOI] [PubMed] [Google Scholar]
- [18].Motamedi MH. An assessment of maxillofacial fractures: a 5-year study of 237 patients. J Oral Maxillofac Surg 2003;61:61–4. [DOI] [PubMed] [Google Scholar]
- [19].Kaur R, Lehl G. Retrospective analysis of maxillofacial injuries in the dental department of a medical college. Indian J Dent Sci 2012;4:30–2. [Google Scholar]
- [20].Ugboko VI, Olasoji HO, Ajike SO, et al. Facial injuries caused by animals in northern Nigeria. Br J Oral Maxillofac Surg 2002;40:433–7. [PubMed] [Google Scholar]
- [21].Matos FPD, Arnez MFM, Sverzut CE, et al. A retrospective study of mandibular fracture in a 40-month period. Int J Oral Maxillofac Surg 2010;39:10–5. [DOI] [PubMed] [Google Scholar]
- [22].Obimakinde OS, Ogundipe KO, Rabiu TB, et al. Maxillofacial fractures in a budding teaching hospital: a study of pattern of presentation and care. Pan Afr Med J 2017;26:218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Brasileiro BF, Passeri LA. Epidemiological analysis of maxillofacial fractures in Brazil: a 5 year prospective study. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 2006;102:28–34. [DOI] [PubMed] [Google Scholar]
- [24].Erol B, Tanrikulu R, Gorgun B. Maxillofacial fractures. Analysis of demographic distribution and treatment in 2901 patients (25-year experience). J Craniomaxillofac Surg 2004;2:308–13. [DOI] [PubMed] [Google Scholar]
- [25].de Matos FP, Arnez MF, Sverzut CE, et al. A retrospective study of mandibular fracture in a 40-month period. Int J Oral Maxillofac Surg 2010;39:10–5. [DOI] [PubMed] [Google Scholar]
- [26].Singh V, Malkunje L, Mohammad S, et al. The maxillofacial injuries: a study. Natl J Maxillofac Surg 2012;3:166–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Ozkaya O, Turgut G, Kayali MU, et al. A retrospective study on the epidemiology and treatment of maxillofacial fractures. Turk J Trauma Emerg Surg 2009;15:262–6. [PubMed] [Google Scholar]
- [28].Samieirad S, Tohidi E, Pakravan M. A conservative method for treating severely displaced pediatric mandibular fractures: an effective alternative technique. J Dent Mater Tech 2016;5:53–8. [Google Scholar]
- [29].Atisha DM, van Rensselaer Burr T, Allori AC, et al. Facial fractures in the aging population. Plastic Recon Surg 2016;137:587–93. [DOI] [PubMed] [Google Scholar]


