Abstract
Background:
Chronic non-specific low back pain (LBP) is gradually increasing among populations worldwide and affects their activities. Recently, the Nd:YAG laser has been presented in the rehabilitation field.
Objectives:
This study aims to explore the short-term effects of the Nd:YAG laser on chronic non-specific LBP individuals.
Methods:
Thirty-five individuals with chronic nonspecific LBP were included in the study from December 2019 to March 2020. Randomly, they were categorized to Nd:YAG group (n = 18) and sham laser as a control (n = 17) thrice weekly for a 6-week intervention. Modified Oswestry disability index (MODI), pain disability index (PDI), visual analogue scale (VAS), and lumbar flexion range of motion (ROM) have been assessed pre and post-6 weeks of the intervention.
Results:
Significant improvements were observed in the Nd:YAG group (MODI, P < .001; PDI, P = .007; VAS, P < .001; lumbar ROM, P = .002), whereas the sham group showed no significant changes (MODI, P = .451; PDI, P = .339; VAS, P = .107; lumbar ROM, P = .296) after 6-week intervention. Between-group comparisons showed significant differences in tending toward the Nd:YAG group (MODI, P < .001; PDI, P = .046; VAS, P < .001; lumbar ROM, P = .003).
Conclusions:
Regarding the present study outcomes, short-term pulsed Nd:YAG laser (6 weeks) may reduce functional disabilities and pain intensity, and improve the lumbar flexion ROM in patients with chronic nonspecific LBP. Further well-designed randomized controlled studies with large sample sizes should be conducted regarding laser treatment.
Keywords: functional disability, laser therapy, low back pain, mobility, Nd:YAG
1. Introduction
Low back pain (LBP) is a leading health problem affecting occupational performance and quality of life and reports a great financial cost worldwide.[1] Annually, the incidence of LBP is growing approximately from 15% to 45%, whereas the individuals who suffer from LBP are approximated 70% to 85% of populations at interval periods in their lifestream.[2] Despite several researches have studied this disorder in the industrial countries, LBP is identified as a serious health problem in Arab countries.[3] In Saudi Arabia, the prevalence of LBP is accounted for 18.8% of adult people and commonly heightens among married individuals aged >30 years.[4] Also, another study in Jeddah city has approved that around 26% of school employees suffer from LBP.[5]
Chronic nonspecific LBP is defined as a LBP not attributable to a detectable or recognized specific pathology with a duration of >12 weeks. It is generally related to mechanical reasons and not associated with specific pathological conditions such as fractures, infections, neoplasm, inflammatory diseases, disc spaces, or compression of nerve roots. Chronic LBP usually leads to functional disability and affects individuals’ daily lives.[6–8]
The treatment of chronic nonspecific LBP contains several intervention strategies such as patient's education, behavior modification, back schools, exercise therapy, and physiotherapy interventions including myofascial release, heat and cold applications, lumbar supports, traction, electrical stimulation, and photobiomodulation therapy.[9]
Light amplification by stimulated emission of radiation (LASER) therapy is identified as painless, noninvasive, and simply used for many various diseases in different healthcare places.[10] Previous documents provided that laser intervention extensively lowers severity of pain in sensitive or persistent states including fibromyalgia, osteoarthritis, rheumatoid arthritis, post-surgical pain, shoulder pain, diabetic ulcers, and carpal tunnel syndrome.[11–13]
Although laser therapy with low intensities generates a slight temperature for body tissues,[14] documents have reported that low-intensity laser therapy (LILT) reduces pain, inflammation, and enhance functional performance.[15,16] LILT improves circulation, stimulates the angiogenesis process, and activates immunization and neural repair. Also, it generates analgesic influences by activation the endorphin synthesis.[13]
Lately, the high-intensity laser therapy (HILT) in the form of a neodymium-doped yttrium aluminum garnet laser (Nd:YAG laser) has been presented in the rehabilitation field. Nd:YAG laser is working with a wavelength of 1064 nm, and an extreme power density (12W) characterizing by easily, painless, and noninvasive interventional application. It activates areas that cannot be reached by LILT including deep and large joints.[17] Using of Nd:YAG laser therapy is growing among patients experiencing pain.[18] Moreover, previous publications have reported that the Nd:YAG laser may reduce edema, inflammation, and pain manifestations.[19,20] For that reason, this study was proposed to explore the short-term effects of the Nd:YAG laser therapy on chronic nonspecific LBP individuals hypothesizing that it may reduce pain severity and functional disability among those patients.
2. Materials and methods
2.1. Ethics
The study was ethically approved by the institutional review board of the physiotherapy department, Prince Sattam bin Abdulaziz University (No.: RHPT/019/040) in accordance with ethical standards of Helsinki Declaration 1964 and presented in accordance with CONSORT guidelines.
2.2. Study design and setting
The study was a prospective single-blinded randomized controlled study with a 6-week intervention and was conducted in the outpatient physiotherapy clinic, Prince Sattam bin Abdulaziz University.
2.3. Sample size estimation
According to our preliminary pilot study on 5 patients, at least 8-mark differences in the Oswestry Disability Index (ODI) are required to achieve power of 90% with σ of 2, and confidence level of 95%. The required study participants were calculated 16 individuals for each group. Therefore, 36 patients were recruited in the 2 groups to account for 10% dropout.
2.4. Subjects
Thirty-six individuals experiencing chronic nonspecific LBP were included in the study from December 2019 to March 2020. They were recruited from the orthopedic outpatient clinic of the university hospital. All individuals were assessed for chronic nonspecific LBP applying physical, biochemical, radio-imaging assessments (x-ray). Randomly, they were categorized to Nd:YAG group (n = 18) and sham laser as a control (n = 18). Inclusion criteria were: the experiencing of LBP for 3 months at least, age range of 30 to 50 years, and the compliant ability to conduct the study program. Exclusion criteria were: orthopedic or neurological abnormalities, unacceptable biochemical investigations, positive inflammatory markers, pregnancy, cognitive dysfunction, LBP medications last 3 months, and spinal disorders, injuries, or surgeries. Before starting the study and acceptance of the participants to conduct the study program, each individual was instructed to sign a written consent form.
2.5. Randomization and blinding
Of 43 chronic nonspecific LBP patients, 36 were eligible to participate in the study procedures. Five subjects were not qualified to the inclusion criteria of the study and 2 subjects rejected to participate in the study program without any determined reason. Before commencing the study procedures, randomization was carried out by means of obscure closed envelopes, which randomly arranged by blinded examiner utilizing equal numbers of odd and even numbers inside the envelopes. Even numbers were recruited to conduct Nd:YAG program, whereas odd numbers were recruited to conduct the sham program. For blindness, because of the study design and settings, it was impossible to blind the therapists included in the program of the study. Whereas, the therapists who assessed the outcome measures pre- and post-intervention were blinded to the individual's group and the participants also were recommended to conceal their treatment program during the assessment.
2.6. Intervention
All study participants have conducted a program of easy home exercise without needs for any equipment. The exercise program consisted of mobility, flexibility, stretching, strengthening of back, pelvic, and abdominal muscles. Therapists have trained each participant to conduct properly the exercise program at the first visit before starting the home exercise. One of the family members has proved that the individual performed the home exercises regularly twice daily.
2.6.1. Nd:YAG protocol
Pulsed Nd:YAG laser was carried out thrice weekly for 6-week intervention using BTL-6000 HIL device with a wavelength of 1064 nm, power of 12 Watts, and hot laser source of Nd:YAG.[17] It was applied on the lumbar region with application area of 30 cm2 through 2-phase characteristics. During the 2 phases, HILT was applied continuously rounded movement. The first 2 weeks were characterized by an analgesic influence at the intermediating phase, pertaining a 75 seconds, power of 8 W, and energy of 6 J/cm2, for a total energy density of 300 J. The subsequent 4 weeks were characterized by a biostimulant influence at the continuing phase, pertaining a 30 seconds, power of 6 W, and energy of 120 to 150 J/cm2. Whereas the control group has received a sham laser (0.0 J) for same periods as active HILT within the 6-week intervention.
2.7. Outcome measures
2.7.1. Functional disability
Functional disability of the chronic nonspecific LBP was assessed pre and post 6-week intervention by 2 valid and reliable indices, the modified Oswestry disability index (MODI) and pain disability index (PDI). The MODI includes 10 elements: standing, sitting, walking, lifting, traveling, self-care, employing/home activities, social participation, intensity of pain, and sleep.[21,22] The score of each element is 0 to 5, and total score of the MODI is 0 to 50, 0 suggests nothing and 50 suggest the highest disability. Regarding PDI, it comprises 7-element questionnaire involving self-care, recreation, sexual behavior, occupation, social participation, family/home activities, and life-support activities.[21] The score of each element is 0 to 10, and the total score is 0 to 70, 0 suggests nothing, and 70 suggests the highest disability.
2.7.2. Intensity of pain
The intensity of pain was evaluated through conducting the valid and reliable visual analogue scale (VAS). Each individual was instructed mark a point on the 10-cm line of VAS, 0 suggests no pain, and 10 suggests severe pain.[23]
2.7.3. Lumbar range of motion
Lumbar flexion range of motion (ROM) was measured pre- and post-intervention using a validated and reliable Modified-Modified Schober Test.[24]
2.8. Statistical analysis
Data analyses were carried out using SPSS for windows, version 25 (IBM Corp., Armonk, NY) with significance level at P < .05. Continuous variables were confirmed for the normal distribution using the Kolmogorov-Smirnov test. All analyzed data were presented as mean ± SD. The paired t test was performed for assessing the pre-post changes within each group, whereas unpaired t test was performed for assessing the differences between Nd:YAG and control groups.
3. Results
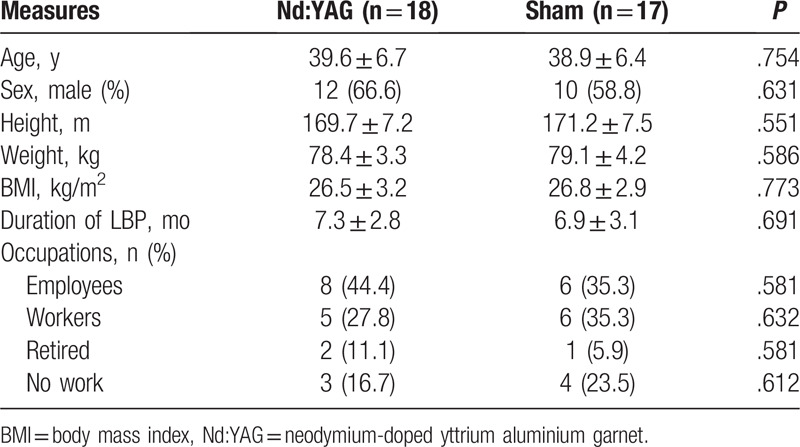
From 36 patients, 1 discontinued the 6-week intervention without any defined reason, whereas 35 patients have completed the study procedures and analyzed, 18 in the ND:YAG group and 17 in the sham group. Figure 1 shows the CONSORT flow diagram of the study. By analyzing the demographic data (age, sex, height, weight, body mass index, and occupations), there were no significant differences between the Nd:YAG and sham groups (P > .05). The employees were affected more than other occupations (40%). The duration of LBP was 7.3 ± 2.8 months in the Nd:YAG group and 6.9 ± 3.1 months in the sham group with nonsignificant difference between the groups (P = .691) as described in Table 1.
Figure 1.
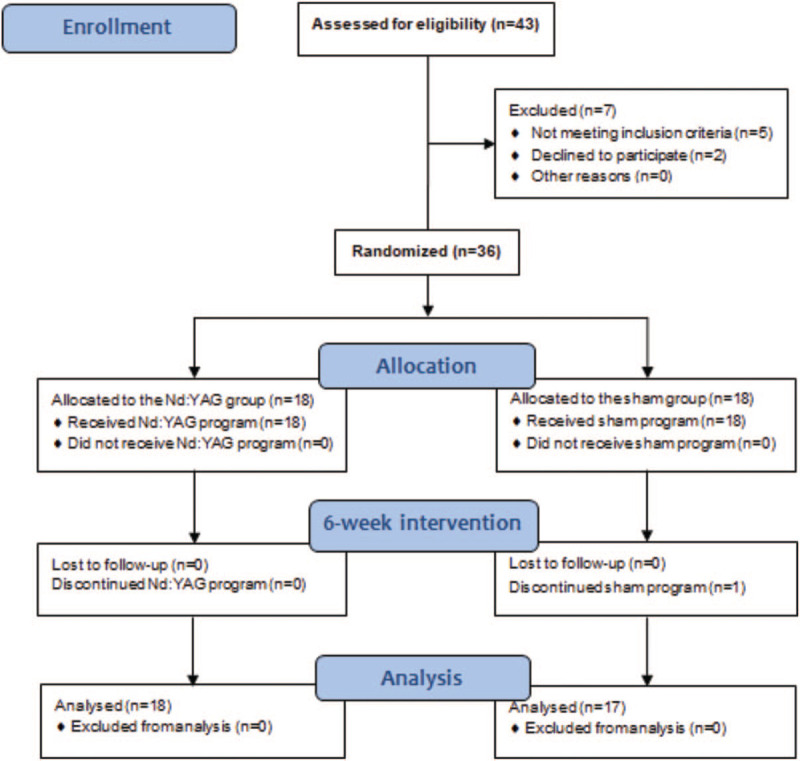
The CONSORT flow diagram of the study.
Table 1.
Baseline demographics of the study participants.
For clinical outcome measures, the preintervention mean values demonstrated nonsignificant differences between the Nd:YAG and sham groups (MODI, P = .796; PDI, P = .831; VAS, P = .706; lumbar ROM, P = .495) as described in Table 2. After 6-week intervention, significant improvements were observed in the Nd:YAG group (MODI, P < .001; PDI, P = .007; VAS, P < .001; lumbar ROM, P = .002), whereas the sham group showed no significant changes (MODI, P = .451; PDI, P = .339; VAS, P = .107; lumbar ROM, P = .296) as detailed in Table 2.
Table 2.
Changes and comparisons of the pre- and post-intervention outcome measures in the Nd:YAG and sham groups.
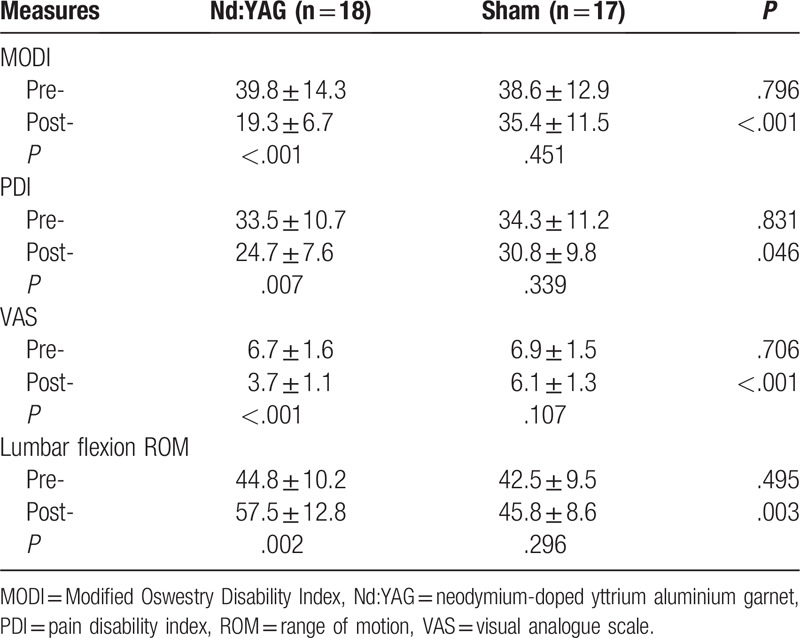
Comparison between mean values of outcome measures after 6-week intervention showed significant differences between the Nd:YAG and sham groups in tending toward the Nd:YAG group (MODI, P < .001; PDI, P = .046; VAS, P < .001; lumbar ROM, P = .003) as described in Table 2.
4. Discussion
This study was conducted to explore the short-term effects of the Nd:YAG laser therapy on chronic nonspecific LBP hypothesizing that Nd:YAG could reduce pain severity and functional disability. The main findings of the study showed that 6 weeks of Nd:YAG laser therapy alleviates pain, reduces functional disabilities, and improves lumbar flexion ROM.
Commonly, low-level laser is utilized to treat the individuals experiencing a chronic nonspecific LBP. This type of laser therapy is identified as a safe and useful physiotherapy intervention for improving joint mobility[15,19] and reducing pain intensity,[11] disabilities,[15,19] and lumbar radiculopathy.[25] Lately, the HILT is utilized in several medical disorders in the form of pulsed Nd:YAG. It is usually utilized in diabetic foot for healing ulcers and relieving pain.[26] It is also utilized for relieving a symptomatic shoulder pain,[17] long-lasting ankle pain,[18] osteoarthritis.[20,27] Previous study approved that HILT reduces pain greater than ultrasound intervention within a 3-week comparative study.[28] Also, it was reported that low-intensity Nd:YAG laser may relieve pain moderately and improve functional performance in LBP patients.[29]
The clinical effects of laser treatment have been believed to adjust cellular functions depending on laser characteristics.[30] The 1064 nm Nd:YAG laser provides the waves to easily infiltrate and extent within the deep tissues due to inadequate meditation of the endogenous chromophore which impair the laser absorption. At the level of laser penetration, the tissue is exposed to a multidirectional light distribution increasing the oxidation response of the mitochondria and consequently proliferate the production of DNA, RNA, and ATP.[17]
Pulsed Nd:YAG is more advantageous than LLLT in the innocent therapeutic uses with high-intensity power, 1064 nm wavelength, and short pulsed durations which help to magnify more energy and a deeper penetration to the targeted tissue with a highly cellular safety. The HILT has 3 photoenergy characteristics including photomechanical, photochemical, and photothermal effects that improve the response of the exposed tissue. Our present study suggests that ND: YAG laser has a key role in relieving pain by altering the release of bradykinin and histamine from the affected tissues[31] and substance P from the nociceptors,[32] thereby raising the pain threshold at the level of the targeted tissues.[33]
Another theory declared that the application of laser irradiation could slow down the conduction of pain transmitters through reducing the sensory nerves conductive velocity that subsequently frustrates the transmission of C and Aδ fibers.[34] One more theory clarifies that pain could be centrally frustrated through increasing the release of beta-endogenous morphine-like substances or opioid peptides.[35,36]
The main implication of the study is that the pulsed Nd:YAG is a feasible, easy, and safe physiotherapy modality to relieve chronic nonspecific LBP in a short-term duration (6 weeks). Contrariwise, some limitations were observed. The main limitation was the small sample size. Also, the study lacked for intermediate and long-term follow-up (after 6-month assessment). Lastly, home exercise has not been supervised. Future studies may include larger sample size to involve different types of laser irradiations on chronic nonspecific LBP.
5. Conclusions
Regarding the present study outcomes, short-term pulsed Nd:YAG laser (6 weeks) may reduce functional disabilities and pain intensity, and improve lumbar flexion ROM in patients with chronic nonspecific LBP. Further well-designed randomized controlled studies with large sample sizes should be conducted regarding laser treatment. Future guidelines for clinical intervention have to be considered to inspire the use of pulsed Nd:YAG laser in the treatment of musculoskeletal disorders, specifically chronic nonspecific LBP.
Acknowledgments
This research was funded by the Deanship of Scientific Research at Princess Nourah Bint Abdulrahman University through the Fast-track Research Funding Program. The authors would like to acknowledge all individuals who participated in the study.
Author contributions
Conceptualization: Walid Kamal Abdelbasset, Gopal Nambi, Shereen H. Elsayed, Saud M. Alrawaili, Ahmed M. Abodonya, Ayman K. Saleh, Samah A. Moawd.
Data curation: Walid Kamal Abdelbasset, Gopal Nambi, Saud M. Alrawaili, Ahmed M. Abodonya, Ayman K. Saleh.
Formal analysis: Walid Kamal Abdelbasset, Gopal Nambi, Shereen H. Elsayed, Saud M. Alrawaili, Nahla N. Ataalla, Ahmed M. Abodonya, Ayman K. Saleh, Samah A. Moawd.
Funding acquisition: Shereen H. Elsayed.
Investigation: Walid Kamal Abdelbasset, Saud M. Alrawaili, Nahla N. Ataalla, Ayman K. Saleh.
Methodology: Walid Kamal Abdelbasset, Gopal Nambi, Shereen H. Elsayed, Saud M. Alrawaili, Ahmed M. Abodonya, Ayman K. Saleh, Samah A. Moawd.
Project administration: Walid Kamal Abdelbasset.
Resources: Ahmed M. Abodonya.
Software: Ahmed M. Abodonya, Ayman K. Saleh, Samah A. Moawd.
Supervision: Walid Kamal Abdelbasset, Gopal Nambi.
Validation: Gopal Nambi, Samah A. Moawd.
Visualization: Saud M. Alrawaili, Ayman K. Saleh.
Writing – original draft: Walid Kamal Abdelbasset, Gopal Nambi, Shereen H. Elsayed, Saud M. Alrawaili, Nahla N. Ataalla, Ahmed M. Abodonya, Ayman K. Saleh, Samah A. Moawd.
Writing – review & editing: Walid Kamal Abdelbasset, Gopal Nambi, Shereen H. Elsayed, Saud M. Alrawaili, Nahla N. Ataalla, Ahmed M. Abodonya, Ayman K. Saleh, Samah A. Moawd.
Footnotes
Abbreviations: HILT = high-intensity laser therapy, LBP = low back pain, LILT = low-intensity laser therapy, MODI = Modified swestry disability index, Nd:YAG = neodymium-doped yttrium aluminum garnet, PDI = pain disability index, VAS = visual analogue scale.
How to cite this article: Abdelbasset WK, Nambi G, Elsayed SH, Alrawaili SM, Ataalla NN, Abodonya AM, Saleh AK, Moawd SA. Short-term clinical efficacy of the pulsed Nd:YAG laser therapy on chronic nonspecific low back pain: A randomized controlled study. Medicine. 2020;99:36(e22098).
The authors report no conflicts of interest.
Funding: This research was funded by the deanship of Scientific Research at Princess Nourah Bint Abdulrahman University through the Fast-track Research Funding Program.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Ganesan S, Acharya AS, Chauhan R, et al. Prevalence and risk factors for low back pain in 1,355 young adults: a cross-sectional study. Asian Spine J 2017;11:610–7.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Freburger JK, Holmes GM, Agans RP, et al. The rising prevalence of chronic low back pain. Arch Intern Med 2009;169:251–8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Abdulbari B, Omer F, Abdulrahim S, et al. Epidemiology of low back pain in the United Arab Emirates. J APLAR Rheumatol 2004;7:189–95.. [Google Scholar]
- [4].Al-Arfaj AS, Al-Saleh SS, Alballa SR, et al. How common is back pain in Al-Qaseem region. Saudi Med J 2003;24:170–3.. [PubMed] [Google Scholar]
- [5].Abalkhail BA, Bahnassy AA, Ghabrah TM. Low back pain among Saudi school workers in Jeddah. Saudi Med J 1998;19:491–5.. [PubMed] [Google Scholar]
- [6].Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet 2017;389:736–47.. [DOI] [PubMed] [Google Scholar]
- [7].Chenot JF, Greitemann B, Kladny B, et al. Non-specific low back pain. Dtsch Arztebl Int 2017;114:883–90.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Oliveira CB, Maher CG, Pinto RZ, et al. Clinical practice guidelines for the management of non-specific low back pain in primary care: an updated overview. Eur Spine J 2018;27:2791–803.. [DOI] [PubMed] [Google Scholar]
- [9].van Middelkoop M, Rubinstein SM, Kuijpers T, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur Spine J 2011;20:19–39.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Brown AW, Weber DC. Braddom RL. Physical agent modalities. Physical Medicine and Rehabilitation.. London: WB Saunders, Harcourt Health Sciences Company; 2000. 440–58.. [Google Scholar]
- [11].Tantawy SA, Abdelbasset WK, Kamel DM, et al. Laser photobiomodulation is more effective than ultrasound therapy in patients with chronic nonspecific low back pain: a comparative study. Lasers Med Sci 2019;34:793–800.. [DOI] [PubMed] [Google Scholar]
- [12].Tantawy SA, Abdelbasset WK, Kamel DM, et al. A randomized controlled trial comparing helium-neon laser therapy and infrared laser therapy in patients with diabetic foot ulcer. Lasers Med Sci 2018;33:1901–6.. [DOI] [PubMed] [Google Scholar]
- [13].Peplow PV, Chung T, Baxter GD. Application of low level laser technologies for pain relief and wound healing overview of scientific bases. Phys Ther Rev 2010;15:253–85.. [Google Scholar]
- [14].Ozdemir F, Birtane M, Kokino S. The clinical efficacy of low-power laser therapy on pain and function in cervical osteoarthritis. Clin Rheumatol 2001;20:181–4.. [DOI] [PubMed] [Google Scholar]
- [15].Gur A, Karakoc M, Cevik R, et al. Efficacy of low power laser therapy and exercise on pain and functions in chronic low back pain. Lasers Surg Med 2003;32:233–8.. [DOI] [PubMed] [Google Scholar]
- [16].Nambi G, Kamal W, Es S, et al. Spinal manipulation plus laser therapy versus laser therapy alone in the treatment of chronic non-specific low back pain: a randomized controlled study. Eur J Phys Rehabil Med 2018;54:880–9.. [DOI] [PubMed] [Google Scholar]
- [17].Zati A, Valent A. Physical therapy: new technologies in rehabilitation medicine (translated to English). Edizioni Minerva Medica 2006;2006:162–85.. [Google Scholar]
- [18].Santamato A, Solfrizzi V, Panza F, et al. Short-term effects of high-intensity laser therapy versus ultrasound therapy in the treatment of people with subacromial impingement syndrome: a randomized clinical trial. Phys Ther 2009;89:643–52.. [DOI] [PubMed] [Google Scholar]
- [19].Saggini R, Bellomo RG, Cancelli F. Hilterapia and chronic ankle pain syndromes. Energy for Health Int J İnf Sci Cult 2009;3:22–5.. [Google Scholar]
- [20].Viliani T, Ricci E, Mangone G, et al. Effects of hilterapia vs. viscosupplementation in knee osteoarthritis patients: a randomized controlled clinical trial. Energy for Health Int J Inf Sci Cult 2009;3:14–7.. [Google Scholar]
- [21].Grönblad M, Hupli M, Wennerstrand P, et al. Intercorrelation and test-retest reliability of the Pain Disability Index (PDI) and the Oswestry Disability Questionnaire (ODQ) and their correlation with pain intensity in low back pain patients. Clin J Pain 1993;9:189–95.. [DOI] [PubMed] [Google Scholar]
- [22].Yakut E, Düger T, Oksüz C, et al. Validation of the Turkish version of the Oswestry Disability Index for patients with low back pain. Spine (Phila Pa 1976) 2004;29:581–5.. [DOI] [PubMed] [Google Scholar]
- [23].Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health 1990;13:227–36.. [DOI] [PubMed] [Google Scholar]
- [24].Tousignant M, Poulin L, Marchand S, et al. The Modified-Modified Schober Test for range of motion assessment of lumbar flexion in patients with low back pain: a study of criterion validity, intra- and inter-rater reliability and minimum metrically detectable change. Disabil Rehabil 2005;27:553–9.. [DOI] [PubMed] [Google Scholar]
- [25].Jovicić M, Konstantinović L, Lazović M, et al. Clinical and functional evaluation of patients with acute low back pain and radiculopathy treated with different energy doses of low level laser therapy. Vojnosanit Pregl 2012;69:656–62.. [PubMed] [Google Scholar]
- [26].Ebid AA, Thabet AA, Helal OF. Effect of pulsed high intensity Nd:YAG laser in treatment of chronic diabetic foot ulcer. Energy for Health Int J Inf Sci Cult 2011;7:25–30.. [Google Scholar]
- [27].Stiglić-Rogoznica N, Stamenković D, Frlan-Vrgoc L. Analgesic effect of high intensity laser therapy in knee osteoarthritis. Coll Antropol 2011;35:183–5.. [PubMed] [Google Scholar]
- [28].Fiore P, Panza F, Cassatella G, et al. Short-term effects of high-intensity laser therapy versus ultrasound therapy in the treatment of low back pain: a randomized controlled trial. Eur J Phys Rehabil Med 2011;47:367–73.. [PubMed] [Google Scholar]
- [29].Basford JR, Sheffield CG, Harmsen WS. Laser therapy: a randomized, controlled trial of the effects of low-intensity Nd:YAG laser irradiation on musculoskeletal back pain. Arch Phys Med Rehabil 1999;80:647–52.. [DOI] [PubMed] [Google Scholar]
- [30].Basford JR. Low intensity laser therapy: still not an established clinical tool. Lasers Surg Med 1995;16:331–42.. [DOI] [PubMed] [Google Scholar]
- [31].Hochman B, Pinfildi CE, Nishioka MA, et al. Low-level laser therapy and light emitting diode effects in the secretion of neuropeptides SP and CGRP in rat skin. Lasers Med Sci 2014;29:1203–8.. [DOI] [PubMed] [Google Scholar]
- [32].Hsieh YL, Hong CZ, Chou LW, et al. Fluence-dependent effects of low-level laser therapy in myofascial trigger spots on modulation of biochemicals associated with pain in a rabbit model. Lasers Med Sci 2015;30:209–16.. [DOI] [PubMed] [Google Scholar]
- [33].King CE, Clelland JA, Knowles CJ, et al. Effect of helium-neon laser auriculotherapy on experimental pain threshold. Phys Ther 1990;70:24–30.. [DOI] [PubMed] [Google Scholar]
- [34].Chow R, Armati P, Laakso EL, et al. Inhibitory effects of laser irradiation on peripheral mammalian nerves and relevance to analgesic effects: a systematic review. Photomed Laser Surg 2011;29:365–81.. [DOI] [PubMed] [Google Scholar]
- [35].Hagiwara S, Iwasaka H, Hasegawa A, et al. Pre-irradiation of blood by gallium aluminum arsenide (830 nm) lowlevel laser enhances peripheral endogenous opioid analgesia in rats. Anesth Analg 2008;107:1058–63.. [DOI] [PubMed] [Google Scholar]
- [36].S GN, Kamal W, George J, et al. Radiological and biochemical effects (CTX-II, MMP-3, 8, and 13) of low-level laser therapy (LLLT) in chronic osteoarthritis in Al-Kharj, Saudi Arabia. Lasers Med Sci 2017;32:297–303.. [DOI] [PubMed] [Google Scholar]


