Supplemental Digital Content is available in the text
Keywords: cross-sectional, glucose, HDL, meditation, menopause, pilot, women
Abstract
Owing to hormonal changes, women experience various psychophysiological alterations over a wide age range, which may result in decreased quality of life as well as in increased risks of diseases, such as cardiovascular diseases. Although studies have been performed to research complementary methods, such as meditation, the research field still requires an adequate amount of studies for public health guidelines. This pilot cross-sectional study aims to investigate a potential association of meditation with menopausal symptoms and blood chemistry for healthy women. In this study, data of 65 healthy women (age range 25–67) including 33 meditation practitioners and 32 meditation-naïve controls were analyzed to compare the Menopausal Rating Scale scores and blood chemistry with 7 more dropouts in the blood chemistry. For blood chemistry, nine components including glucose (GLU) and high-density lipoprotein cholesterol (HDL) were measured. Two-way analysis of variance was performed by dividing the total participants into 2 groups: premenopausal and postmenopausal participants. Compared to the control group, the meditation group showed a trend of reductions in the Menopausal Rating Scale total score (P = .054) and its 2 subcomponents: depressive mood (P = .064) and irritability (P = .061). In HDL level, there was a significant interaction between group and menopausal state (P = .039) with following post hoc results: among the premenopausal participants, a significant increase in the meditation group compared to the control group (P = .005); among the control group, a significant increase in the postmenopausal compared to the premenopausal participants (P = .030). In GLU level, there was a mild interaction between group and menopausal state (P = .070) with following post hoc results: among the postmenopausal participants, a trend of increase in the control group compared to the meditation group (P = .081); among the control group, a significant increase in the postmenopausal compared to the premenopausal participants (P = .040). Our research suggests a potential association of practicing meditation with alleviations in menopausal symptoms and changes in blood chemistry, warranting further studies with a longitudinal study design and larger populations to understand the underlying causal relationships.
1. Introduction
Women experience hormonal changes over long periods of time. Throughout their 20s to 50s, the levels of follicle-stimulating hormone and luteinizing hormone increase,[1–3] while estradiol levels gradually decrease especially through their 30s to 40s.[4] Along with the hormonal changes, multiple physical and psychological changes occur. During the perimenopausal period, the decline in estrogen levels in the blood is thought to be the causative factor responsible for vasomotor symptoms, including feelings of intense heat that are usually coupled with sweating and tachycardia, which generally last for minutes to up to half an hour. The vasomotor symptoms are the main causes of sleep disturbances in perimenopausal women.[5] During the menopausal transition, estrogen fluctuations affect the serotonin pathway to various degrees and may increase the risk of mood disorders, such as depression.[6] A longer period of exposure to endogenous estrogens, which is related to a later onset of menopause and longer reproductive period, is associated with a lower risk of depression in later life.[7]
The early onset of menopause was found to be positively correlated with the occurrence of cardiovascular diseases, independent of traditional risk factors,[8] thereby indicating that menopausal hormonal changes critically affect cardiovascular health. Along with the onset of menopause, the reduction in the production of estradiol that exhibits strong antioxidant effects induces the accumulation of risk factors for chronic inflammation.[9] Based on the results of a meta-analysis involving the data of 257,384 adults who were 45, 55, 65, and 75 years old, the risk of cardiovascular diseases increases with age in women.[10] Cardiovascular disease-related factors, such as high-density lipoprotein cholesterol (HDL) levels, have been extensively researched. HDL has been known for its protective effects against arteriosclerosis; however, it has also been reported that it loses its function in certain situations.[11]
Evidence has been put forward to indicate that mind-body training techniques, such as meditation, yoga, tai chi, and qi gong, are safe and effective alternative methods that can be practiced for decreasing the risk factors of cardiovascular disease and for improving an individual's mood and well-being. Symptoms similar to those related to menopause are often observed in young women of reproductive age.[12] Regarding the period of occurrence of menopausal symptoms, some researchers have reported that it can span through a period of 25 years from the ages of approximately 35 to 60 years.[13,14] Further, 8% of women experience the first onset of menopause under the age of 40, and therefore, they experience menopausal symptoms in their 30s.[15] Approximately 7% of patients with breast cancer, the most common invasive cancer type in women,[16] are diagnosed under the age of 40 (age 20–39), and this disease accounts for more than 40% of the cases involving all the types of cancer affecting in women of the same age range.[17] A substantial number of breast cancer survivors in their 30s experience bothersome menopausal symptoms.[18] This suggests that menopausal symptoms are issues that affect women from a relatively wide age range and that preventive approaches are required to improve their long-term quality of life.
With age, women experience multiple psychological and physical changes, accompanied by an increased number of risk factors for various diseases, including cardiovascular diseases. In the current study, we hypothesized that the meditation training may have associations with psychophysiological features of healthy women and examined the menopausal symptoms based on the Menopausal Rating Scale and physiological changes based on the blood chemistry in healthy adult women who practiced meditation for a long duration (>6 months) and in those who did not have any experience in practicing meditation. In this pilot cross-sectional study, we aimed to uncover a potential association of practicing meditation with the menopausal symptoms and blood chemistry of women.
2. Methods
2.1. Participants
This study is a part of the project that was designed to understand the association between health and meditation, which was conducted from September to November 2018 in the University of Brain Education, Cheonan, the Republic of Korea. The meditation type which was used in this study is Brain Education Sangdahnjeon meditation (BESM), the roots of which are found in the ancient Korean tradition of mind and body practice.[19] The BESM class is based on Brain Education 5 steps[20] and is characterized by 2 main features: a static focused attention meditation session[21] and a dynamic movement meditation session called brain wave vibration (BWV).[22–25] The current report involves a cross-sectional research study that compares the menopausal symptoms and blood chemistry between the BESM-training group and the control group. The participants were recruited from local meditation centers and universities in Seoul, Cheonan, Daejeon, and Pusan in the Republic of Korea through flyers and announcements for a period of 1 month. The inclusion criterion for the overall study sample in the current study was healthy adult women. The inclusion criteria for the long-term meditation group were women who practiced BESM for at least 6 months with a regularity of at least once per week. The control group inclusion criteria included women with no previous experience in meditation training. The exclusion criteria for both groups included physical disabilities, psychiatric diagnoses, and the use of medications that could affect blood chemistry. In the current study, participants filled self-reports including age, education, religion, details regarding the duration of practice, daily practice time, frequency of practice a day and Menopausal Rating Scale. Then they were subjected to venipuncture. Participants who reported the cessation of their menstrual cycles (≥12 months) were defined as “postmenopausal”, while others who did not were described as “premenopausal”. The current research was approved by the Ethics Committee of the University of Brain Education. The research was carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. All the participants provided written informed consent.
2.2. Menopausal Rating Scale
Menopausal Rating Scale assesses the health-related quality of life of women and is composed of an 11-item questionnaire that measures the intensity of symptoms, such as periodic sweating or hot flashes, nervousness, and bone and joint complaints, with higher scores indicating more severe symptoms.[26] We used this scale for all the participants whose menopausal state and ages spanned over a broad range from premenopause to postmenopause, as reported earlier.[27]
2.3. Blood sample collection and blood chemistry
For the blood sample collection, the participants were directed to maintain an 8 hour fast before the blood collection process. Blood samples were collected via venipuncture in 10 mL ethylenediaminetetraacetic acid tubes between the hours of 08:00 and 10:00 am following an overnight fast. The blood samples were immediately mixed gently 10 times, following which they were centrifuged at 2500×g for 10 min at room temperature in order to separate the plasma for the blood chemistry tests. The plasma samples were immediately frozen after the separation until the measurement. They were examined by a technician who was blinded to the codes of the samples in order to reduce the possibility of any potential bias influencing the experiment's results. The following parameters were measured in the separated plasma: HDL, glucose (GLU), triglyceride (TG), total protein (TP), creatinine (CREA), blood urea nitrogen (BUN), lactate dehydrogenase (LDH), aspartate aminotransferase (AST), and alanine aminotransferase (ALT). The biochemical measurements were performed using the BS-200 Chemistry Analyzer (Mindray, China).
2.4. Statistical analysis
An optimal total sample size of 52 participants required to perform a two-way analysis of variance (ANOVA) (effect size f = 0.4 with a significance level set at α = .05, power 1 – β = .80) was calculated using the G-Power software application. Statistical analyses were performed using the SPSS, version 25. Group differences in the number of pre/postmenopausal participants and in religions of participants were tested using χ2 tests. T tests were used to investigate the differences of age, education, duration of practice, daily practice time or frequency of daily practice between groups. Two-way ANOVA was used to investigate the effects of the group, menopausal status, and interaction between the group and menopausal status on the blood chemistry data and self-report results. A statistical significance was based on two-sided statistical tests and was evaluated at a .05 level of significance.
3. Results
3.1. Demographics
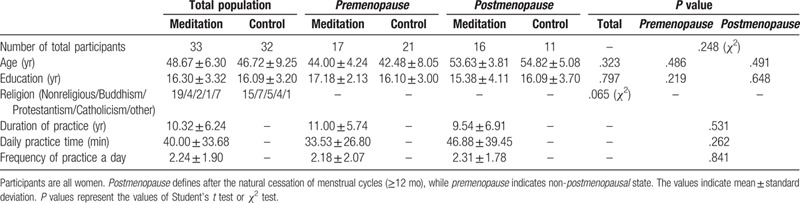
Sixty-six women were participated in the current study. As 1 person did not complete her self-report, the data of 65 women (Table 1) were finally analyzed. The average age of the total participants was 48.67 ± 6.30 years (mean ± standard deviation) in the meditation group and 46.72 ± 9.25 years in the control group (P = .323, Student's t test). The education period was not significantly different between the 2 groups (P = .797, Student's t test). The distribution of religions was similar in both groups (P = .065, χ2 test). Each group included women who reported the cessation of menstrual cycles (≥12 months) (postmenopause: N = 16, meditation; N = 11, control, Table 1), without a significant group difference (P = .248, χ2 test). In both the pre and postmenopausal participants, the average age of the participants was not significantly different between the meditation and the control groups (premenopause, P = .486; postmenopause, P = .491, Student's t test). In the meditation group, the total period of meditation practice was 10.32 ± 6.24 years. Daily practice time and frequency was 40.00 ± 33.68 minutes and 2.24 ± 1.91 times per day, respectively. There were no significant differences between the premenopause and postmenopause meditation participants in terms of total duration, daily practice time, and frequency (Table 1). Regarding blood chemistry, 7 more participants were excluded because of breaking the 8 hour fast, thereby resulting in the inclusion of 58 participants in the blood chemistry analysis (Supplementary material 1). No significant differences were found in any demographically investigated items between groups.
Table 1.
Subject demographics.
3.2. Menopausal Rating Scale
The meditation group exhibited a certain trend toward significant reduction in the total Menopausal Rating Scale score compared to the control group (Table 2, P = .054, two-way ANOVA), while there was no significant difference in the menopausal state or in the interaction between group and menopausal state.
Table 2.
Menopausal Rating Scale.
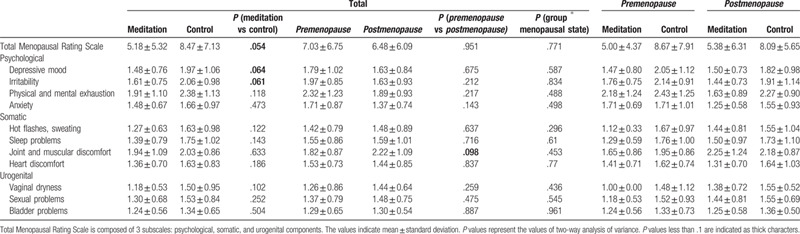
The Menopausal Rating Scale consists of 3 domains: the psychological, somatic, and urogenital domains.[28] Within the psychological domain, trends of reduction were found in depressive moods (P = .064) and irritability (P = .061) in the meditation group compared to the control group. In the other factors in psychological, somatic and urogenital domains, the means of each item were consistently lower in the meditation group than the control group, although there were no significant differences or any trends of changes. The data of participants were divided by their menopausal state for further analysis. Interestingly, the means of postmenopausal participants were higher in most components of the somatic and urogenital domains, but lower in all components of the psychological domain, than premenopausal participants in both the meditation and control groups. Moreover, in joint and muscular discomfort, a statistical trend of increase was observed in postmenopausal women compared to premenopausal women (P = .098).
To further understand the relationships between age and the menopausal symptoms in the 2 groups, we analyzed the menopausal symptoms by dividing the participants into 3 age domains: ≤40, 41–50, and >50 (N = 11, 26, and 28, respectively, Supplementary material 2–5). In a two-way ANOVA, a mild interaction was found between age and group in the case of hot flashes/sweating (P = .067), but not in other factors (Supplementary material 2). In the participants of age 41 to 50, the occurrence of hot flashes/sweating was especially higher in the control group than in the meditation group. While the meditation group showed a relatively flat slope throughout the investigated age ranges, the control group showed a specifically high occurrence of hot flashes/sweating in 41 to 50 more than the other age ranges (Supplementary material 3).
3.3. Blood chemistry
In the two-way ANOVA on the blood chemistry test, there were significant or mild interactions between group and menopausal state in HDL and GLU but not in other factors (P = .039 and.070; HDL and GLU, respectively, Table 3). In the post hoc Holm-Sidak comparisons of HDL, the meditation group showed a significantly higher value than the control group only in the premenopausal (P = .005), but not in the postmenopausal participants. In the control group, there was a significant increase in HDL levels of the postmenopausal compared to the premenopausal participants (P = .030, post hoc Holm-Sidak comparisons). In the post hoc Holm-Sidak comparisons of GLU in postmenopausal participants, there was a mild reduction in the meditation group compared to the control group (P = .081), while there were no mild or significant changes in the premenopausal participants. Similar to HDL, in the control group, there was a significant increase in GLU levels of the postmenopausal compared to the premenopausal participants (P = .040, post hoc Holm-Sidak comparisons). In addition, we found the total postmenopausal participants exhibit significant increases in the levels of BUN, LDH, AST, and ALT, compared to the total premenopausal participants (P = .011, .001, <.001, and.028, respectively).
Table 3.
Blood chemistry.
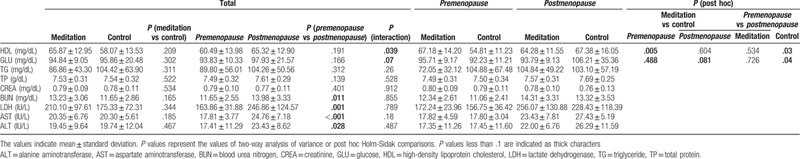
To further understand whether there were any potential interactions between age and group in the level of blood chemistry, we divided the participants into 3 age domains: ≤40, 41 to 50, and >50 (Supplementary material 4). We found that there was a statistically significant interaction in HDL, but not in other factors (P = .043, two-way ANOVA). In the control group, the HDL level of the age domain >50 was significantly higher compared to that of the age domain 41 to 50 (P = .012, post hoc Holm-Sidak comparisons, Supplementary material 5). In contrast, within the meditation group, there were no significant changes in the HDL levels among the age groups. In the participants under age 50, the HDL levels in the meditation group were significantly higher compared to those of the control group (P = .026 for age ≤40; P = .015 for age 41–50, post hoc Holm-Sidak comparisons). Due to the sudden increase of HDL in the control group over age 50, there were no significant differences in HDL levels between 2 groups over age 50.
4. Discussion
In this pilot cross sectional study, we compared Menopausal Rating Scale scores and blood chemistry results between the meditation-practicing group and the meditation-naive control group in order to understand whether there are any potential associations of meditation with menopausal symptoms and blood chemistry. We found potential associations of Menopausal Rating Scale scores as well as some components of blood chemistry with meditation practice.
In all the sub-items of the Menopausal Rating Scale, the mean values observed in the meditation group were lower than those in the control group, with a trend of significance in total score and 2 sub-item scores (Table 2). This suggests that meditation may have potential benefits that can alleviate menopausal symptoms, although further investigation is required to uncover the causal relationship. A systemic review has reported that practicing mind-body therapies, such as meditation, yoga, and tai chi, can alleviate overall menopausal symptoms including vasomotor symptoms, issues related to mood and sleep, and muscular skeletal pain.[29] Our findings support the previous findings that mind-body care can help in easing menopausal symptoms.
In the meditation group, there was a trend of reduction in depression and irritability (Table 2). BESM, a meditation method used in the current research, is a form which combined static focused attention meditation[21] and dynamic BWV meditation.[25] In the comparative randomized controlled trial of BWV and other 2 mind-body trainings, BWV exhibited the biggest effect on depression alleviation among the 3.[25] Moreover, in another study, the depression scale was significantly decreased in the long term BWV-training group than in the control group.[23] The depression reduction effect of the meditation in the current finding is consistent with the above mentioned reports. According to Jung et al,[30] neuroticism, defined by items referring to irritability and anger,[31] was significantly reduced in the BWV-training group compared to the control group, which is consistent with our current finding. In the study which reported changes in functional connectivity of insula with other brain regions between the BWV-training group and the meditation-naïve control group, BWV training associates with functional changes in brain regions related with focused attention, executive control, emotional awareness and regulation.[22] Furthermore, compared to the control participants, BWV practitioners exhibited significantly thicker cortex and white matter structures in the medial prefrontal cortex which regulates emotions.[32] Above mentioned previous researches about the effects of BWV on brain function and structures support emotional changes in the meditation group, found in the current study. The two-way ANOVA in which participants were divided into 3 groups by age showed a mild interaction between age and group in hot flashes/sweating (Supplementary material 2). The relation between age and hot flashes/sweating showed a relatively flat slope in the meditation group, but a sudden increase during 41 to 50 in the control group (Supplementary material 3). Carmody et al[33] reported that meditation clinically significantly decreases hot flashes and night sweats, which is consistent with our current finding.
HDL was increased in the meditation group compared to the control group among premenopausal participants, while the group difference disappeared by increment of HDL in the control group among postmenopausal participants (Table 3, Supplementary material 5). Among the postmenopausal participants, the mean value of HDL of the meditation group was even slightly lower than that of the control group (Table 3). In a study that researched 213 healthy women, it was found that HDL levels increased after menopause.[34] In another study that researched 1380 women, the HDL levels were found to be higher in postmenopausal women compared to in perimenopausal women.[35] Furthermore, the measurements reported in yet another study support this finding by indicating a slight increase in the HDL subclasses in a population close to menopause.[36] Our finding indicating higher HDL levels in postmenopausal compared to in premenopausal participants in the control group is consistent with the previous findings described above. Carotid intima-media thickness can be an indication of subclinical arteriosclerosis. According to El Khoudary et al,[37] increased HDL levels during the premenopause stage relate to the prevention of the progression of carotid intima-media thickness, while increased HDL levels during the postmenopause stage relate to increments in the progression of carotid intima-media thickness. As the menopausal transition progresses, the levels of the potent antioxidant, estradiol, decrease, thereby leading to chronic inflammation being induced in the body.[9] Systemic inflammation converts HDL into its dysfunctional form, and therefore, potentially stops its function in arteriosclerosis prevention.[38] Among women over 52, a high HDL level is significantly related to high risks of non-fatal stroke and cerebral infarction.[39] In postmenopausal women, the HDL level positively correlates with carotid intima-media thickness.[40] These accumulated studies suggest that the function of HDL in the prevention of cardiovascular diseases during premenopause may not last after the menopause. Therefore, our current findings, that HDL levels are higher in the meditation group compared to in the control group among the premenopausal participants but not among the postmenopausal participants, suggest that the risk factors for cardiovascular diseases are lower in the meditation group than in the control group during the premenopause stage and are at least not higher during the postmenopause stage.
Similar to HDL, only among the control participants, GLU increased significantly in the postmenopausal participants compared to the premenopausal participants (Table 3). As a result, the meditation group exhibited a significantly lower GLU level than the control group among postmenopausal participants (Table 3). Regulation disruption of GLU during menopause correlates with aging not with decline of ovarian function.[41] Therefore, the significant increment of GLU in the control group in the postmenopausal participants compared to the premenopausal participants seems to be induced by aging. On the other hand, the reason why such a change was not observed in the meditation group might be due to the association of meditation with delayed aging.[42,43] In both the meditation and control groups, postmenopausal participants showed a significant increase compared to premenopausal participants in several factors: joint and muscular discomfort among Menopausal Rating Scale (Table 2); BUN, LDH, AST, and ALT among blood chemistry components (Table 3). This suggests that these factors are especially sensitive to menopausal state or aging.
The current study was designed as a pilot cross-sectional study to compare the menopausal symptoms and blood chemistry between the meditation group and the meditation-naïve group comprised of healthy women. There was a trend of reduction in total Menopausal Rating Scale score in the meditation group compared to in the control group. In blood chemistry, there was a significant increase of HDL level in the meditation group compared to the control group among premenopausal participants, while there was a trend of increase of GLU in the control group compared to the meditation group among postmenopausal participants. There are limitations in the current study. As this study is a cross-sectional study, causal relationships between the meditation training and the indicated measurements cannot be discussed, therefore a longitudinal study is required to reveal the causal relationships. Moreover, as menopause is the natural phenomena along with aging of women, it is unclear whether the observations are related with aging or altered ovarian function by menopause. To answer this question, an experimental design with specific clinical setting is required. However, our current pilot study suggests the possibility of an association of meditation practice with the alleviation of menopausal symptoms as well as changes in HDL and GLU levels, warranting further studies with a longitudinal design and a larger study population to reveal the causal relationships involved.
Acknowledgments
The authors would like to thank Ji-Yeon Park, PharmD; Jin-Hee Lee, MD; So-Young Moon, MA; Ji-Hee Kim, MA; Young-Jin Lee, MA; Min-Seo Kim, BS; Yun-Sik Sim, MA; Seon-Ah Yoon, PhD for fruitful discussions, and support for the study. The authors thank the participants who gave their consents to participate in this study.
Author contributions
Min-Kyu Sung: Data curation, Validation, Formal analysis, Visualization, Writing. Ul Soon Lee: Conceptualization. Na Hyun Ha: Funding acquisition, Investigation. Eugene Koh: Investigation, Writing. Hyun-Jeong Yang: Funding acquisition, Conceptualization, Methodology, Project administration, Writing, Supervision.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: ALT = alanine aminotransferase, ANOVA = analysis of variance, AST = aspartate aminotransferase, BESM = Brain Education Sangdahnjeon meditation, BUN = blood urea nitrogen, BWV = brain wave vibration, CREA = creatinine, GLU = glucose, HDL = high-density lipoprotein cholesterol, LDH = lactate dehydrogenase, TG = triglyceride, TP = total protein.
How to cite this article: Sung MK, Lee US, Ha NH, Koh E, Yang HJ. A potential association of meditation with menopausal symptoms and blood chemistry in healthy women: a pilot cross-sectional study. Medicine. 2020;99:36(e22048).
This work was supported by University of Brain Education [grant number 2018-03] and Global Cyber University [grant number 23018-1]. The funding sources had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
The authors have no competing interests to report.
The raw data that supports the findings of this study are available on request from the corresponding author, H-J Y.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Xu ZR, Wang AH, Wu XP, et al. Relationship of age-related concentrations of serum FSH and LH with bone mineral density, prevalence of osteoporosis in native Chinese women. Clin Chim Acta 2009;400:8–13.. [DOI] [PubMed] [Google Scholar]
- [2].Sowers MR, Zheng H, McConnell D, et al. Follicle stimulating hormone and its rate of change in defining menopause transition stages. J Clin Endocrinol Metab 2008;93:3958–64.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Raeissi A, Torki A, Moradi A, et al. Age-specific serum anti-mullerian hormone and follicle stimulating hormone concentrations in infertile Iranian women. Int J Fertil Steril 2015;9:27–32.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Dimitrakakis C, Bondy C. Androgens and the breast. Breast Cancer Res 2009;11:212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Jehan S, Jean-Louis G, Zizi F, et al. Sleep, melatonin, and the menopausal transition: What are the links? Sleep Sci 2017;10:11–8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lokuge S, Frey BN, Foster JA, et al. Depression in women: windows of vulnerability and new insights into the link between estrogen and serotonin. J Clin Psychiatry 2011;72:e1563–9.. [DOI] [PubMed] [Google Scholar]
- [7].Georgakis MK, Thomopoulos TP, Diamantaras AA, et al. Association of age at menopause and duration of reproductive period with depression after menopause: a systematic review and meta-analysis. JAMA Psychiatry 2016;73:139–49.. [DOI] [PubMed] [Google Scholar]
- [8].Wellons M, Ouyang P, Schreiner PJ, et al. Early menopause predicts future coronary heart disease and stroke: the Multi-Ethnic Study of Atherosclerosis. Menopause 2012;19:1081–7.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Shaw LJ, Bugiardini R, Merz CN. Women and ischemic heart disease: evolving knowledge. J Am Coll Cardiol 2009;54:1561–75.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Berry JD, Dyer A, Cai X, et al. Lifetime risks of cardiovascular disease. N Engl J Med 2012;366:321–9.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Rosenson RS, Brewer HB, Jr, Ansell BJ, et al. Dysfunctional HDL and atherosclerotic cardiovascular disease. Nat Rev Cardiol 2016;13:48–60.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hahn PM, Wong J, Reid RL. Menopausal-like hot flashes reported in women of reproductive age. Fertil Steril 1998;70:913–8.. [DOI] [PubMed] [Google Scholar]
- [13].Fishbein EG. Women at midlife. The transition to menopause. Nurs Clin North Am 1992;27:951–7.. [PubMed] [Google Scholar]
- [14].Li S, Lanuza D, Gulanick M, et al. Perimenopause: the transition into menopause. Health Care Women Int 1996;17:293–306.. [DOI] [PubMed] [Google Scholar]
- [15].Pinkerton JV, Woodson SA. Perimenopause: easing the transition. Contemporary OB/GYN 1998;43:93–94, 97–98, 100. [Google Scholar]
- [16].McGuire A, Brown JA, Malone C, et al. Effects of age on the detection and management of breast cancer. Cancers (Basel) 2015;7:908–29.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Anders CK, Johnson R, Litton J, et al. Breast cancer before age 40 years. Semin Oncol 2009;36:237–49.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Leining MG, Gelber S, Rosenberg R, et al. Menopausal-type symptoms in young breast cancer survivors. Ann Oncol 2006;17:1777–82.. [DOI] [PubMed] [Google Scholar]
- [19].Hanmunhwa, SH L The Secret of Sangdahnjeon. 1996. [Google Scholar]
- [20].Lee SH, Hwang SM, Kang DH, et al. Brain education-based meditation for patients with hypertension and/or type 2 diabetes: a pilot randomized controlled trial. Medicine (Baltimore) 2019;98:e15574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Hanmunhwa, Lee SH. Grow the power of the brain hidden inside the child. 2005. [Google Scholar]
- [22].Jang JH, Kim JH, Yun JY, et al. Differences in functional connectivity of the insula between brain wave vibration in meditators and non-meditators. Mindfulness 2018;s12671-12018-10928-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Lee DH, Park HY, Lee US, et al. The effects of brain wave vibration on oxidative stress response and psychological symptoms. Compr Psychiatry 2015;60:99–104.. [DOI] [PubMed] [Google Scholar]
- [24].Bowden DE, McLennan D, Gruzelier J. A randomised controlled trial of the effects of Brain Wave Vibration training on mood and well-being. J Complement Integr Med 2014;11:223–32.. [DOI] [PubMed] [Google Scholar]
- [25].Bowden D, Gaudry C, An SC, et al. A comparative randomised controlled trial of the effects of brain wave vibration training, iyengar yoga, and mindfulness on mood, well-being, and salivary cortisol. Evid Based Complement Alternat Med 2012;2012:234713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Heinemann LA, DoMinh T, Strelow F, et al. The Menopause Rating Scale (MRS) as outcome measure for hormone treatment? A validation study. Health Qual Life Outcomes 2004;2:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Yisma E, Eshetu N, Ly S, et al. Prevalence and severity of menopause symptoms among perimenopausal and postmenopausal women aged 30–49 years in Gulele sub-city of Addis Ababa, Ethiopia. BMC Womens Health 2017;17:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Heinemann K, Ruebig A, Potthoff P, et al. The Menopause Rating Scale (MRS) scale: a methodological review. Health Qual Life Outcomes 2004;2:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Innes KE, Selfe TK, Vishnu A. Mind-body therapies for menopausal symptoms: a systematic review. Maturitas 2010;66:135–49.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Jung YH, Lee US, Jang JH, et al. Effects of mind-body training on personality and behavioral activation and inhibition system according to BDNF Val66Met polymorphism. Psychiatry Investig 2016;13:333–40.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Lahey BB. Public health significance of neuroticism. Am Psychol 2009;64:241–56.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Kang DH, Jo HJ, Jung WH, et al. The effect of meditation on brain structure: cortical thickness mapping and diffusion tensor imaging. Soc Cogn Affect Neurosci 2013;8:27–33.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Carmody JF, Crawford S, Salmoirago-Blotcher E, et al. Mindfulness training for coping with hot flashes: results of a randomized trial. Menopause 2011;18:611–20.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].El Khoudary SR, Hutchins PM, Matthews KA, et al. Cholesterol efflux capacity and subclasses of HDL particles in healthy women transitioning through menopause. J Clin Endocrinol Metab 2016;101:3419–28.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].El Khoudary SR, Ceponiene I, Samargandy S, et al. HDL (high-density lipoprotein) metrics and atherosclerotic risk in women. Arterioscler Thromb Vasc Biol 2018;38:2236–44.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Wang Q, Ferreira DLS, Nelson SM, et al. Metabolic characterization of menopause: cross-sectional and longitudinal evidence. BMC Med 2018;16:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].El Khoudary SR, Wang L, Brooks MM, et al. Increase HDL-C level over the menopausal transition is associated with greater atherosclerotic progression. J Clin Lipidol 2016;10:962–9.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Barter PJ, Nicholls S, Rye KA, et al. Antiinflammatory properties of HDL. Circ Res 2004;95:764–72.. [DOI] [PubMed] [Google Scholar]
- [39].Bots ML, Elwood PC, Nikitin Y, et al. Total and HDL cholesterol and risk of stroke. EUROSTROKE: a collaborative study among research centres in Europe. J Epidemiol Community Health 2002;56: Suppl 1: i19–24.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Fan AZ, Dwyer JH. Sex differences in the relation of HDL cholesterol to progression of carotid intima-media thickness: the Los Angeles Atherosclerosis Study. Atherosclerosis 2007;195:e191–6.. [DOI] [PubMed] [Google Scholar]
- [41].Matthews KA, Crawford SL, Chae CU, et al. Are changes in cardiovascular disease risk factors in midlife women due to chronological aging or to the menopausal transition? J Am Coll Cardiol 2009;54:2366–73.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Chaix R, Alvarez-Lopez MJ, Fagny M, et al. Epigenetic clock analysis in long-term meditators. Psychoneuroendocrinology 2017;85:210–4.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Conklin QA, King BG, Zanesco AP, et al. Insight meditation and telomere biology: the effects of intensive retreat and the moderating role of personality. Brain Behav Immun 2018;70:233–45.. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


