Supplemental Digital Content is available in the text
Keywords: albumin, hospitalization, hypoalbuminemia, outcomes, respiratory failure
Abstract
Serum albumin is a marker of nutritional and frailty status. This study aimed to assess the association between serum albumin at the time of admission and the risk of acute respiratory failure (ARF) in hospitalized patients
This cohort study, performed at a tertiary referral hospital, included all hospitalized adult patients from January 2009 to December 2013 who had serum albumin measurement and were not on mechanical ventilation within 24 hours of hospital admission. Serum albumin was stratified into 2.4, 2.5 to 2.9, 3.0 to 3.4, 3.5 to 3.9, 4.0 to 4.4, and ≥4.5 g/dL. Multivariate logistic regression analysis was performed to obtain adjusted odds ratio (OR) of risk of ARF requiring mechanical ventilation based on various admission serum albumin levels.
Of 12,719 patients, ARF requiring mechanical ventilation occurred in 1128 (8.9%) during hospitalization. Hypoalbuminemia was associated with increased risk of ARF, in particular when serum albumin was ≤2.4 g/dL. Compared with serum albumin of 4.0–4.4 g/dL, serum albumin ≤2.4 g/dL at admission was associated with 2.38-time higher odds of ARF during hospitalization (OR 2.38, 95% confidence interval [CI] 1.84–3.07). In contrast, elevated serum albumin ≥4.5 g/dL was associated with lower odds of ARF (OR 0.68, 95% CI 0.48–0.97).
Admission serum albumin level lower than 3.5 g/dL was associated with a higher risk of ARF requiring mechanical ventilation, whereas elevated serum albumin level at least 4.5 g/dL was associated with a lower risk of ARF. Therefore, admission albumin level at admission might be useful in the prediction of ARF during hospitalization.
1. Introduction
Acute respiratory failure (ARF) is a common and serious complication among hospitalized patients, which leads to morbidity and higher mortality.[1,2] In severe cases, mechanical ventilation is required.[3–6] Main predictors of the need in mechanical ventilation among patients with ARF include hypoalbuminemia, malnutrition, premorbid functional status, and APACHE II score. However, most of the studies primarily focus only on the chronic obstructive pulmonary disease.[7–9]
Serum albumin is a marker for nutritional and frailty.[10] Hypoalbuminemia can lead to reduced pulmonary oncotic pressure, resulting in higher extravascular lung water and hypoxemia.[11–20] Studies have demonstrated that hypoalbuminemia is associated with longer length of mechanical ventilation and poorer clinical outcomes.[10,21,22] Nevertheless, the association between serum albumin and the risk of the need for mechanical ventilation among hospitalized patients with ARF is not clearly stated in the literature.
Thereby, the aim of this study is to investigate the association between serum albumin level and the risk of ARF requiring mechanical ventilation.
2. Materials and methods
2.1. Study population
This is a retrospective single-center cohort study. All hospitalized adult patients in Mayo Clinic Hospital, Rochester, Minnesota, from January 1st, 2009, to December 31st, 2013, with available serum albumin within 24 hours of hospital admission, were included. Patients who were on mechanical ventilation at the time of admission were excluded. This study was approved by the Mayo Institutional Review Board. The need for informed consent was waived due to the minimal risk nature of the study. All included patients provided research authorization for their data use.
2.2. Data collection and clinical outcomes
Clinical characteristics and laboratory data were obtained using automated retrieval from the institutional electronic medical record system. The predictor of interest was the admission serum albumin, defined as the first serum albumin value measured within 24 hours of hospital admission. Estimated glomerular filtration rate (GFR) was calculated based on age, sex, race, and serum creatinine, using the Chronic Kidney Disease Epidemiology Collaboration Equation.[23] Body mass index was calculated using weight in kilograms divided by the square of height in meters at the time of admission. The Charlson Comorbidity score was calculated to assess co-morbidities at the time of admission.[24] Principal diagnoses were grouped based on ICD-9 codes. Acute kidney injury was defined as an increase in serum creatinine of ≥0.3 mg/dL or ≥1.5 times baseline value.[25] The primary outcome was ARF requiring mechanical ventilation during hospitalization. The elective use of mechanical ventilation during procedure was not included as the outcome.
2.3. Statistical analysis
Continuous variables were presented as mean ± standard deviation. Categorical variables were presented as count with percentage. Continuous and categorical variables were compared among admission serum albumin groups, using ANOVA and the Chi-square test, respectively. Admission serum albumin was categorized into 6 groups; ≤2.4, 2.5 to 2.9, 3.0 to 3.4, 3.5 to 3.9, 4.0 to 4.4, and ≥4.5 g/dL. The admission serum albumin level of 4.0 to 4.4 g/dL was selected as the reference group for outcome comparison since it was regarded as the normal range. Multivariate logistic regression analysis was performed to assess the independent association between admission serum albumin levels and ARF requiring mechanical ventilation. Odds ratio (OR) with 95% confidence interval (CI) were reported. The a priori-defined adjusting variables included age, sex, race, baseline GFR, body mass index, Charlson Comorbidity Index, history of coronary artery disease, hypertension, diabetes mellitus, congestive heart failure, chronic obstructive pulmonary disease, asthma, dementia, stroke, cirrhosis, principal diagnosis, acute kidney injury and the use of vasopressor at hospital admission. Linear regression analysis was performed to assess the independent association between admission serum albumin levels and mechanical ventilation duration among ARF. As mechanical ventilation duration had a skewed distribution, it was summarized as median with interquartile range (IQR) and was log-transformed before entering into the model. The relative prolongation, derived from exponential of the regression coefficient, was reported. Missing data was not imputed. All P-values were 2-tailed, and P values of <.05 were considered significant. All analyses were performed using JMP statistical software (version 10, SAS Institute, Cary, NC).
3. Results
3.1. Clinical characteristics
A total of 14,075 patients with available serum albumin measurement within 24 hours of hospital admission were identified. After 1356 patients who were on mechanical ventilation at admission were excluded, 12,719 patients were analyzed. Fifty-three percent of enrolled individuals were male. The mean age was 62 ± 17 years. The mean admission serum albumin was 3.5 ± 0.7 g/dL. At the time of admission, 7% had serum albumin of ≤2.4, 14% had 2.5 to 2.9, 23% had 3.0 to 3.4, 28% had 3.5 to 3.9, 21% had 4.0 to 4.4, and 7% had ≥4.5 g/dL. The clinical characteristics of patients based on admission serum albumin levels were shown in Table 1.
Table 1.
Baseline clinical characteristics based on admission serum albumin levels.
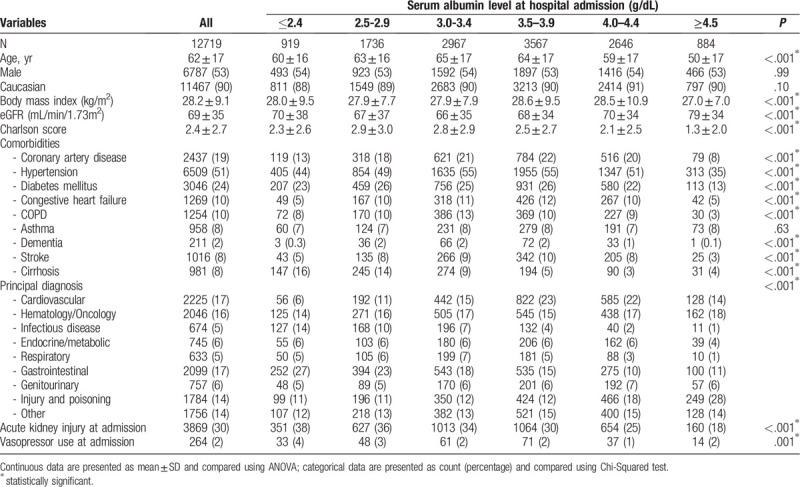
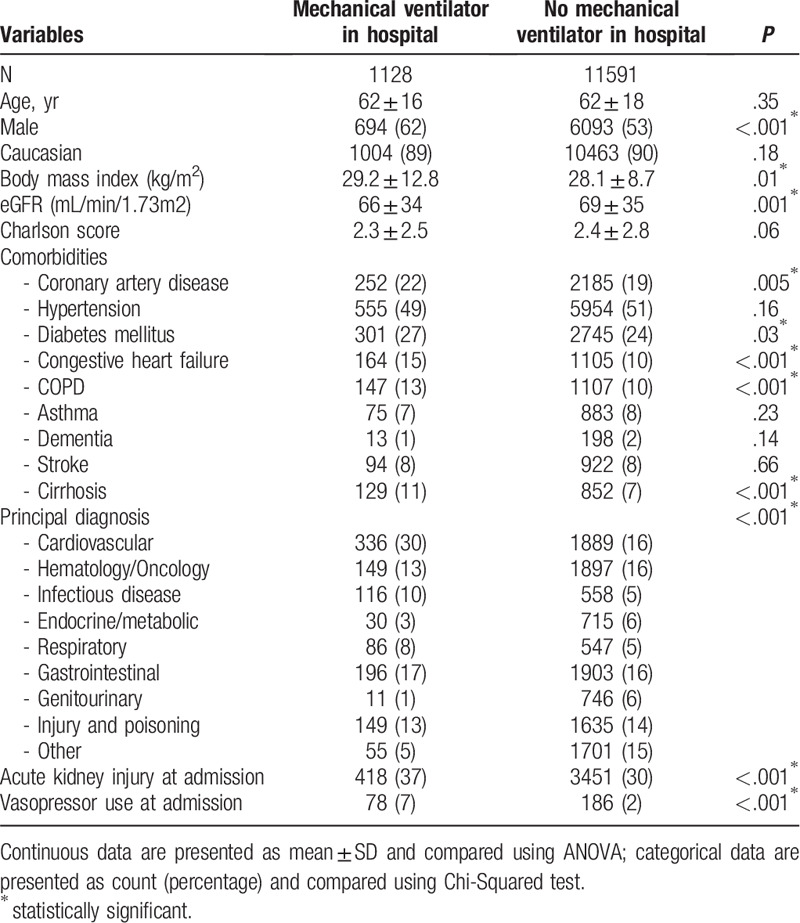
Table 2 compared clinical characteristics between patients who developed ARF requiring mechanical ventilation. Patients with ARF requiring in-hospital mechanical ventilation were more likely to be male, have higher body mass index, lower estimated GFR, more history of coronary artery disease, diabetes mellitus, congestive heart failure, chronic obstructive pulmonary disease, cirrhosis, be admitted for cardiovascular, infectious, and respiratory diseases, had higher incidence of acute kidney injury and need for vasopressors at hospital admission than patients without ARF.
Table 2.
Baseline clinical characteristics based on the status of acute respiratory failure requiring mechanical ventilation.
3.2. Admission serum albumin and risk of in-hospital respiratory failure
Of 12,719 patients, the overall incidence of ARF requiring mechanical ventilation during hospitalization was 8.9%. The lowest incidence of ARF requiring mechanical ventilation was when admission serum albumin of ≥4.5 g/dL (4.9%), while the highest incidence was when admission serum albumin of ≤2.4 g/dL (16.8%) (Table 3). Progressively increased incidence of ARF requiring mechanical ventilation was observed with decreased admission serum albumin (Fig. 1). Multivariable analysis adjusting for potential confounders showed that increased risk of ARF requiring mechanical ventilation was significantly associated with admission serum albumin of ≤2.4 (OR 2.38; 95% CI 1.84–3.07), 2.5 to 2.9 (OR 1.34; 95% CI 1.05–1.69), 3.0 to 3.4 (OR 1.32; 95% CI 1.07–1.62) g/dL compared to admission serum albumin of 4.0 to 4.4 g/dL. In contrast, admission serum albumin of ≥4.5 g/dL was significantly associated with 32% decreased the risk of ARF requiring mechanical ventilation (OR 0.68; 95% CI 0.48–0.97) compared to admission serum albumin of 4.0 to 4.4 g/dL. A decrease in admission serum albumin by 1 g/dL was associated with increased risk of ARF requiring mechanical ventilation with adjusted OR of 1.52 (95% CI 1.37–1.69). The receiver operating characteristics analysis (ROC) showed a C-statistic of 0.57 using admission serum albumin alone, and of 0.71 using multivariable models of serum albumin and other clinical characteristics.
Table 3.
The association between admission serum albumin levels and in-hospital acute respiratory failure requiring mechanical ventilation.
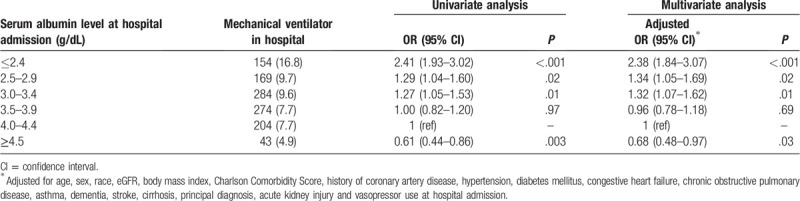
Figure 1.
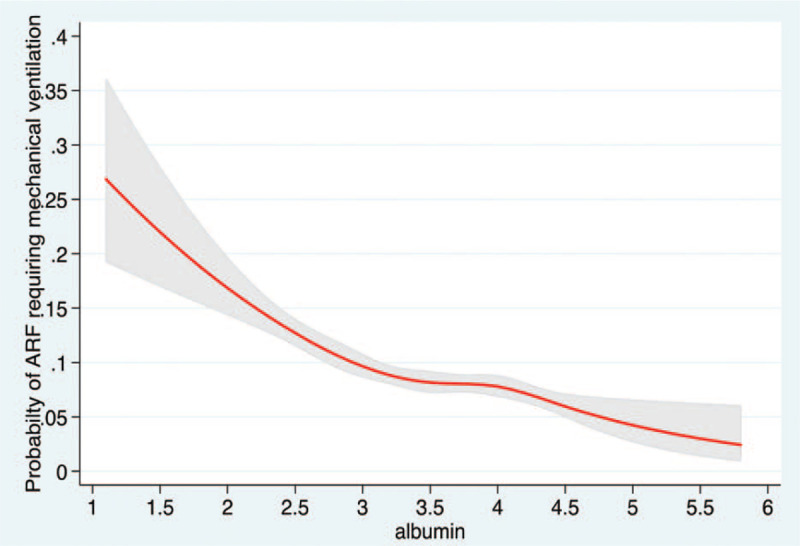
The restricted cubic spline showing the association between admission serum albumin and risk of acute respiratory failure requiring mechanical ventilation.
In multivariable logistic regression analysis with backward stepwise selection, admission serum albumin was an independent predictor of ARF requiring mechanical ventilation. Admission serum albumin of ≤3.4 g/dL, male sex, increased body mass index, history of congestive heart failure, cirrhosis, being primarily admitted for cardiovascular disease, hematology/oncology disease, infectious disease, respiratory disease, gastrointestinal disease, injury and poisoning, acute kidney injury, and vasopressor use predicted higher risk of ARF requiring mechanical ventilation. In contrast, admission serum albumin of ≥4.5 g/dL, and being admitted for genitourinary disease were associated with lower risk of ARF requiring mechanical ventilation (Table S1).
3.3. Admission serum albumin and the mechanical ventilation duration
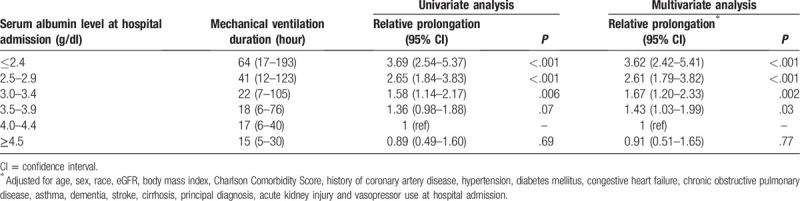
The median mechanical ventilation duration was 24 (IQR 8–92) hours. The median mechanical ventilation duration was progressively increased with lower admission serum albumin from 15 hours in admission serum albumin of ≥4.5 g/dL to 64 hours in ≤2.4 g/dL. After adjusting for confounders, admission serum albumin ≤3.9 g/dL was progressively associated with increased mechanical duration from 1.43-time longer in serum albumin of 3.5–3.9 g/dL to 3.62-time longer in serum albumin of ≤2.4 g/dL (Table 4).
Table 4.
The association between admission serum albumin levels and mechanical ventilation duration among patients with in-hospital acute respiratory failure requiring mechanical ventilation.
4. Discussion
The results of our study indicate a significant association between serum albumin at hospital admission and ARF requiring mechanical ventilation. Lower serum albumin below 3.5 g/dL was associated with significantly increased risk of ARF requiring mechanical ventilation during hospitalization. On the other hand, serum albumin level at hospital admission at least 4.5 g/dL was associated with lower risk of ARF requiring mechanical ventilation. We also demonstrated a progressive increase in risk of mechanical ventilation as admission albumin level decreased below the normal range. The association remained significant after adjusting for potential confounders.
This is the first observational study to show the association between admission serum albumin levels and the risk of in-hospital ARF requiring mechanical ventilation The underlying mechanism might be explained by a few reasons. First, serum albumin is a marker of nutritional status, with lower levels associated with malnutrition. Malnutrition can lead to respiratory muscle dysfunction caused by atrophy of diaphragmatic muscle and loss of muscle mass. In addition, malnourished patients also have an impaired immune response, leading to increased infection risk, specifically pneumonia. Second, we hypothesize that lower serum albumin causes a lower lung oncotic pressure, which contributes to higher extravascular lung water.[11–20] Moreover, leaky capillary membranes due to malnutrition and underlying cause of ARF would increase vascular permeability, worsening edema in the lungs and perpetuates more acute lung injury, while decreasing serum albumin levels as albumin is a negative acute phase reactant.[26] Hypoalbuminemia can affect the pharmacokinetics of some drugs that are bound to albumin, such as propofol and midazolam. This can exaggerate their efficiency and lead to respiratory depression.[27,28] Hypoalbuminemia also complicates the interpretation of the anion gap in clinical practice.[29] With the base-excess approach, no distinction is found between a deficit/excess of weak or strong nonvolatile acids. Thus, the alkalinizing effect of hypoalbuminemia (related to deficit of a weak nonvolatile acid) may offset and mask the detection of unmeasured anions, leading to a misinterpretation of acid-base disorders,[29] which, in turn, may influence clinicians’ decision to prescribe mechanical ventilation. Furthermore, serum albumin plays an essential role as antioxidants in the respiratory tract.[11,13–20] Hence, lower serum albumin reduces the ability to combat oxidative stress, and further increases risk of lung injury, and decreased oxygenation.[30] However, the role of raising serum albumin is still conflicting in reducing mortality and risk of mechanical ventilation among hospitalized patients.[31–34]
Our study has some limitations. First, even after adjusting for several known confounders, there would still be some residual confounders. Owing to the retrospective observational study design, it is impossible to adjust for every possible confounder. Moreover, apart from BMI, we do not have data to represent nutritional status, which might be a potential confounder in this case. Second, the type of respiratory failure was not investigated. There are also some strengths to our study that should be highlighted. Our study included a large cohort of 14,075 patients which allowed us to extensively adjust for several confounders in order to investigate for an independent association between serum albumin level at admission and in-hospital ARF requiring mechanical ventilation. Because ARF is a significant problem during hospitalization, the findings from our study will help future investigators to develop a prognostic model at the time of hospital admission to estimate the risk of in-hospital ARF in order to identify high-risk patients among hospitalized patients and to implement prevention measures. In addition, further study should investigate the benefit of hypoalbuminemia correction through nutritional support on the risk of ARF in hospitalized patients.
In summary, our study pinpoints the role of a serum albumin level at admission as a predictor of ARF requiring mechanical ventilation. Serum albumin level at admission lower than 3.5 g/dL is associated with higher risk of ARF requiring mechanical ventilation while serum albumin level at admission above 4.5 g/dL is associated with a lower risk of ARF requiring mechanical ventilation.
Author contributions
Conceptualization: Charat Thongprayoon, Wisit Cheungpasitporn, Kianoush Kashani.
Data curation: Charat Thongprayoon.
Formal Analysis: Charat Thongprayoon, Api Chewcharat.
Methodology: Charat Thongprayoon, Wisit Cheungpasitporn.
Software: Charat Thongprayoon.
Supervision: Michael Mao, Kianoush Kashani.
Validation: Api Chewcharat, Sorkko Thirunavukkarasu, Michael Mao.
Writing – original draft: Charat Thongprayoon, Wisit Cheungpasitporn, Api Chewcharat.
Writing – review & editing: Michael Mao, Sorkko Thirunavukkarasu, Kianoush Kashani.
Supplementary Material
Footnotes
Abbreviations: ARF = acute respiratory failure, CI = confidence interval, GFR = glomerular filtration rate, IQR = interquartile range, OR = odds ratio.
How to cite this article: Thongprayoon C, Cheungpasitporn W, Chewcharat A, Mao MA, Thirunavukkarasu S, Kashani KB. Risk of acute respiratory failure among hospitalized patients with various admission serum albumin levels: A cohort study. Medicine. 2020;99:9(e19352).
This work was performed at Mayo Clinic in Rochester, MN.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Elsevier Inc, Goldman LSA. Goldman's Cecil Medicine. 24th ed2012. [Google Scholar]
- [2]. Thongprayoon C, Cheungpasitporn W, Chewcharat A, Mao MA, Thirunavukkarasu S, Kashani KB. Admission serum phosphate levels and the risk of respiratory failure [published online ahead of print, 2019 Dec 12]. Int J Clin Pract. 2019;e13461. doi:10.1111/ijcp.13461. [DOI] [PubMed] [Google Scholar]
- [3].Carson SS, Cox CE, Holmes GM, et al. The changing epidemiology of mechanical ventilation: a population-based study. J Intensive Care Med 2006;21:173–82. [DOI] [PubMed] [Google Scholar]
- [4].Stefan MS, Shieh M-S, Pekow PS, et al. Epidemiology and outcomes of acute respiratory failure in the United States, 2001 to 2009: a national survey. J Hosp Med 2013;8:76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Thongprayoon C, Cheungpasitporn W, Chewcharat A, et al. The Association of Low Admission Serum Creatinine with the Risk of Respiratory Failure Requiring Mechanical Ventilation: a retrospective Cohort study. Sci Rep 2019;9:18743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Thongprayoon C, Cheungpasitporn W, Srivali N, et al. Admission serum magnesium levels and the risk of acute respiratory failure. Int J Clin Pract 2015;69:1303–8. [DOI] [PubMed] [Google Scholar]
- [7].Kumar S, Khilnani GC, Banga A, et al. Predictors of requirement of mechanical ventilation in patients with chronic obstructive pulmonary disease with acute respiratory failure. Lung India 2013;30:178–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Vitacca M, Clini E, Porta R, et al. Acute exacerbations in patients with COPD: predictors of need for mechanical ventilation. Eur Respir J 1996;9:1487–93. [DOI] [PubMed] [Google Scholar]
- [9].Madkour AM, Adly NN. Predictors of in-hospital mortality and need for invasive mechanical ventilation in elderly COPD patients presenting with acute hypercapnic respiratory failure. Egyptian Journal of Chest Diseases and Tuberculosis 2013;62:393–400. [Google Scholar]
- [10]. Thongprayoon C, Cheungpasitporn W, Chewcharat A, Mao MA, Thirunavukkarasu S, Kashani KB. Impacts of Admission Serum Albumin Levels on Short-Term and Long-Term Mortality in Hospitalized Patients [published online ahead of print, 2019 Nov 20]. QJM. 2019;hcz305. doi:10.1093/qjmed/hcz305. [DOI] [PubMed] [Google Scholar]
- [11].Namendys-Silva SA, Gonzalez-Herrera MO, Texcocano-Becerra J, et al. Hypoalbuminemia in critically ill patients with cancer: incidence and mortality. Am J Hosp Palliat Care 2011;28:253–7. [DOI] [PubMed] [Google Scholar]
- [12].Vincent JL. Relevance of albumin in modern critical care medicine. Best Pract Res Clin Anaesthesiol 2009;23:183–91. [DOI] [PubMed] [Google Scholar]
- [13].Yu MY, Lee SW, Baek SH, et al. Hypoalbuminemia at admission predicts the development of acute kidney injury in hospitalized patients: a retrospective cohort study. PLoS One 2017;12:e0180750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Herrmann FR, Safran C, Levkoff SE, et al. Serum albumin level on admission as a predictor of death, length of stay, and readmission. Arch Intern Med 1992;152:125–30. [PubMed] [Google Scholar]
- [15].Thongprayoon C, Cheungpasitporn W, Mao MA, et al. U-shape association of serum albumin level and acute kidney injury risk in hospitalized patients. PLoS ONE 2018;13:e0199153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Wiedermann CJ, Wiedermann W, Joannidis M. Hypoalbuminemia and acute kidney injury: a meta-analysis of observational clinical studies. Intensive Care Med 2010;36:1657–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Sung J, Bochicchio GV, Joshi M, et al. Admission serum albumin is predicitve of outcome in critically ill trauma patients. Am Surg 2004;70:1099–102. [PubMed] [Google Scholar]
- [18].Fleck A, Raines G, Hawker F, et al. Increased vascular permeability: a major cause of hypoalbuminaemia in disease and injury. Lancet 1985;1:781–4. [DOI] [PubMed] [Google Scholar]
- [19].Blunt MC, Nicholson JP, Park GR. Serum albumin and colloid osmotic pressure in survivors and nonsurvivors of prolonged critical illness. Anaesthesia 1998;53:755–61. [DOI] [PubMed] [Google Scholar]
- [20].Reinhardt GF, Myscofski JW, Wilkens DB, et al. Incidence and mortality of hypoalbuminemic patients in hospitalized veterans. JPEN J Parenter Enteral Nutr 1980;4:357–9. [DOI] [PubMed] [Google Scholar]
- [21].Akirov A, Masri-Iraqi H, Atamna A, et al. Low albumin levels are associated with mortality risk in hospitalized patients. Am J Med 2017;130:1465.e11-e19. [DOI] [PubMed] [Google Scholar]
- [22].Ali M, Alekh K, Mathew J, et al. Hypoalbuminemia and length of mechanical ventilation in ARDS. CHEST 2011;140:200A. [Google Scholar]
- [23].Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009;150:604–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245–51. [DOI] [PubMed] [Google Scholar]
- [25]. Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO Clinical Practice Guideline for Acute Kidney Injury. idney inter., Suppl. 2012; 2: 1–138. [Google Scholar]
- [26].Maskara S, Sen N, Raj JP, et al. Correlation between lung injury score and serum albumin levels in patients at risk for developing acute lung injury. Nutrition 2000;16:91–4. [DOI] [PubMed] [Google Scholar]
- [27].Trapani G, Altomare C, Liso G, et al. Propofol in anesthesia. Mechanism of action, structure-activity relationships, and drug delivery. Curr Med Chem 2000;7:249–71. [DOI] [PubMed] [Google Scholar]
- [28].Reves JG, Fragen RJ, Vinik HR, et al. Midazolam: pharmacology and uses. Anesthesiology 1985;62:310–24. [PubMed] [Google Scholar]
- [29].Oh YK. Acid-base disorders in ICU patients. Electrolyte Blood Press 2010;8:66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hackett TL, Scarci M, Zheng L, et al. Oxidative modification of albumin in the parenchymal lung tissue of current smokers with chronic obstructive pulmonary disease. Respir Res 2010;11:180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Patel A, Laffan MA, Waheed U, et al. Randomised trials of human albumin for adults with sepsis: systematic review and meta-analysis with trial sequential analysis of all-cause mortality. BMJ 2014;349:g4561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Roberts I, Blackhall K, Alderson P, et al. Human albumin solution for resuscitation and volume expansion in critically ill patients. Cochrane Database Syst Rev 2011;Cd001208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Mendez CM, McClain CJ, Marsano LS. Albumin therapy in clinical practice. Nutr Clin Pract 2005;20:314–20. [DOI] [PubMed] [Google Scholar]
- [34].Caraceni P, Domenicali M, Tovoli A, et al. Clinical indications for the albumin use: still a controversial issue. Eur J Intern Med 2013;24:721–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


