To the Editor: Lymphangioma circumscriptum (LC) is a rare benign skin disorder involving hamartomatous lymphatic malformation of deep dermal and subcutaneous lymphatic channels. Cutaneous LC (CLC) is the most common lymphangioma. It rarely occurs in the scrotum. The ability of dermoscopy to help clinicians make the correct diagnosis of CLC has been investigated in previous studies.
A 19-year-old man presented with complaints of asymptomatic multiple fluid-filled lesions involving the skin of the scrotum for 5 years. Occasionally the swelling was rupture, discharging serous fluid from the scrotum. During the past year, he was treated with surgical excision of the affected region without a biopsy. However, the mass above the scrotum occurred over the next few months. He had no history of sexually transmitted diseases, radiotherapy damage, or infections. On physical examination, the entire scrotum was found to be studded with multiple white vesicles of variable sizes, ranging from 1 to 3 mm2. Some vesicles exuded viscous serous fluid after being punctured, and the vesicle spaces were filled with pale yellow crusts. Underlying scrotal skin was diffusely thickened [Figure 1A]. There was no associated lymphadenopathy or lymphedema. Ultrasonography of the scrotum suggested hydrocele of the left testis, and the scrotal wall exhibited edema and thickening. Dermoscopy showed densely distributed white or buff-colored lacunar areas that were surrounded by pale yellow or yellow-white structures, ranging from 1 to 3 mm2, as well as reddish to purplish or mauve homogeneous pigmented spots in the lowest part of the lacunae. The area exhibited a white or yellowish mulberry-like appearance [Figure 1B]. Histopathological features showed papillated epidermal hyperkeratosis and multiple dilated lymphatic vessels lined by a thin wall of endothelial cells with an inflammatory infiltrate in the papillary dermis. These lymphatic vessels were filled with lymphatic fluid. The collagen fibrils around the lymphatics showed significant hyperplasia [Figure 1C]. Some of the vessels also included variable concentrations of red blood cells and eosinophilic proteinaceous substance [Figure 1D]. Immunohistochemistry for D2-40 (+), CD31(+) [Figure 1E and 1F], and CD34(−) was performed.
Figure 1.
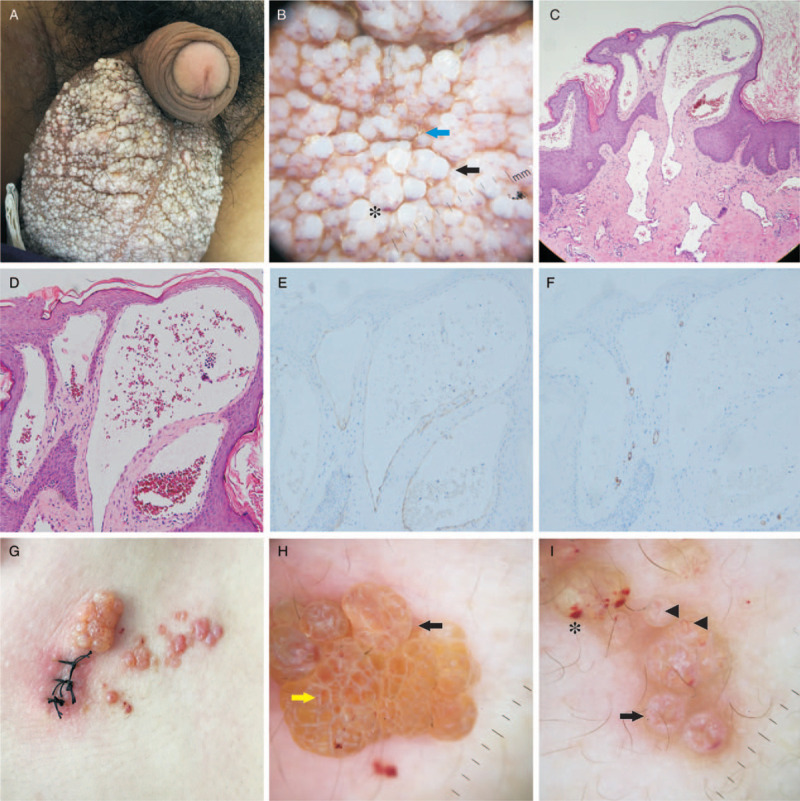
The clinical manifestation, dermoscopic and pathological findings of the patient (A–F) and typical findings of other patients (G–I). Scrotum studded with multiple white or buff-colored vesicles of variable size, ranging from 1 to 3 mm2 (A). Dermoscopy revealing lacunar areas (black arrows) surrounded by pale yellow or yellow–white structures (blue arrow) and homogeneous pigmented spots (asterisk) (B). Histopathology showing papillated epidermal hyperkeratosis, multiple dilated lymphatic vessels lined by a thin wall of endothelial cells. Lymphatic vessels filled with lymphatic fluid and red blood cells and eosinophilic proteinaceous substance (C, D, hematoxylin and eosin staining, original magnification ×40). Immunohistochemical staining showed D2-40 positive (E) and CD31 positive (F) (original magnification ×100). Right axillary plaque composed of vesicles with serous and serohematic filling and some vesicular satellite lesions with serohematic filling (G). Dermoscopy reveals lacunar areas (black arrows) that were surrounded by pale septa (yellow arrows) (H), homogeneous pigmented spots (asterisk), lacunar areas (black arrows), and linear and sharp vessels (triangle) (I).
CLC is an uncommon benign disorder of the lymphatic channels. It is usually congenital, although it may arise at any age.[1] Acquired LC develops at an advanced age, possibly due to injury to deep collecting lymphatics caused by radiotherapy damage or infections such as filariasis, lymphogranuloma venereum, or tuberculosis. CLC commonly appears in the upper part of the body, but rarely occurs in the genital area. It is generally characterized by persistent, multiple clusters of translucent or hazy vesicles that usually contain clear lymph fluid with or without hemorrhage [Figure 1G] or, less commonly, as diffuse swelling to a particular area. On the genitals, such as in our case, the vesicles may be misdiagnosed as molluscum contagiosum, condyloma acuminate, or idiopathic calcinosis cutis. The definitive diagnosis is usually made by biopsy. Histopathology shows many greatly dilated lymph channels in the upper dermis. These channels are filled with lymphatic fluid and may contain erythrocytes, lymphocytes, macrophages, or neutrophils.
Dermoscopy is a non-invasive technique that has considerably improved the diagnostic accuracy for lymphangioma circumscriptum. It has been suggested that dermoscopically, CLC displays two distinct patterns: yellow lacunae surrounded by pale septa without inclusion of blood [Figure 1H) and yellow to pink lacunae alternating with dark-red or bluish lacunae [Figure 1I] due to the inclusion of blood.[2] These findings were well correlated with histologic features.[3] The former is characterized by dilated dermal or subcutaneous lymphatic vessels or both. These are filled with lymphatic fluid. The latter include variable concentrations of red blood cells. Several reports[4,5] have provided an indicator that has been described as a “hypopyon-like feature.” Some cases consist of colored areas varying from yellowish-white to diffuse rose with linear and sharp vessels[1,3,5] [Figure 1I].
In our scrotal LC case, dermoscopy showed densely distributed white and yellowish lacunar areas with red-violet spots in the lower portion, and pale yellow or yellowish-white structures separating the lacunae. The area resembled a white or yellowish mulberry rather than resembling the hypopyon of the eye, and unlike common sites, the vesicles did not show a transparent or translucent appearance. This may be due to the hyperplasia of collagen fibers around lymphatic vessels. This inference is consistent with the report that the histopathological correlation of the white lines could be the presence of fibroplasia in cases of CLC.[5] Linear or sharp vessels were not observed. The pale yellow and yellow-white structures around lacunae may correspond to eosinophilic keratin in pathology.
In conclusion, the presence of lacunae, vascular structures, and hypopyon-like features are very important dermoscopic criteria for the diagnosis of CLC.[5] However, in scrotal LC, the dermoscopic features may be different.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for images and other clinical information to be reported in the article. The patient understands that his name and initials will not be published and due efforts will be made to conceal the identity of the patient, although anonymity cannot be guaranteed.
Funding
This work was supported by a grant from the Wuhan Science and Technology Foundation (No. 2019010701011418).
Conflicts of interest
None.
Footnotes
How to cite this article: Dong J, Lin EY, Zhang L, Chen LQ. Dermoscopic features of cutaneous lymphangioma circumscriptum of the scrotum. Chin Med J 2020;133:2126–2128. doi: 10.1097/CM9.0000000000000957
References
- 1.Patel GA, Schwartz RA. Cutaneous lymphangioma circumscriptum: frog spawn on the skin. Int J Dermatol 2009; 48:1290–1295.. doi: 10.1111/j.1365-4632.2009.04226.x. [DOI] [PubMed] [Google Scholar]
- 2.Arpaia N, Cassano N, Vena GA. Dermoscopic features of cutaneous lymphangioma circumscriptum. Dermatol Surg 2006; 32:852–854.. doi: 10.1111/j.1524-4725.2006.32174.x. [DOI] [PubMed] [Google Scholar]
- 3.Amini S, Kim NH, Zell DS, Oliviero MC, Rabinovitz HS. Dermoscopic- histopathologic correlation of cutaneous lymphangioma circumscriptum. Arch Dermatol 2008; 144:1671–1672.. doi: 10.1001/archderm.144.12.1671. [DOI] [PubMed] [Google Scholar]
- 4.Gencoglan G, Inanir I, Ermertcan AT. Hypopyon-like features: new dermoscopic criteria in the differential diagnosis of cutaneous lymphangioma circumscriptum and haemangiomas. J Eur Acad Dermatol Venereol 2012; 26:1023–1025.. doi: 10.1111/j.1468-3083.2011.04136.x. [DOI] [PubMed] [Google Scholar]
- 5.Zaballos P, Del Pozo LJ, Argenziano G, Karaarslan IK, Landi C, Vera A, et al. Dermoscopy of lymphangioma circumscriptum: a morphological study of 45 cases. Australas J Dermatol 2017; 59:e189–e193.. doi: 10.1111/ajd.12668. [DOI] [PubMed] [Google Scholar]


