Abstract
Purpose:
Veterans with post-traumatic stress disorder (PTSD) lose less weight in the Veterans Affairs (VA) weight management program (MOVE!), so we developed MOVE!+UP.
Design:
Single-arm pre–post pilot to iteratively develop MOVE!+UP (2015–2018).
Setting:
Veterans Affairs Medical Center.
Participants:
Overweight Veterans with PTSD (5 cohorts of n = 5–11 [N = 44]; n = 39 received ≥1 MOVE+UP session, with cohorts 1–4 [n = 31] = “Development” and cohort 5 [n = 8] = “Final” MOVE!+UP).
Intervention:
MOVE!+UP weight management for Veterans with PTSD modified after each cohort. Final MOVE!+UP was coled by a licensed clinical psychologist and Veteran peer counselor in 16 two-hour in-person group sessions and 2 individual dietician visits. Sessions included general weight loss support (eg, behavioral monitoring with facilitator feedback, weekly weighing), cognitive-behavioral skills to address PTSD-specific barriers, and a 30-minute walk to a nearby park.
Measures:
To inform post-cohort modifications, we assessed weight, PTSD, and treatment targets (eg, physical activity, diet), and conducted qualitative interviews.
Analysis:
Baseline to 16-week paired t tests and template analysis.
Results:
Development cohorts suggested improvements (eg, additional sessions and weight loss information, professional involvement) and did not lose weight (mean [M] = 1.8 lbs (standard deviation [SD] = 8.2); P = .29. Conversely, the final cohort reported high satisfaction and showed meaningful weight (M = —14 pounds [SD = 3.7] and 71% lost ≥5% baseline weight) and PTSD (M = —17.9 [SD = 12.2]) improvements, P < .05.
Conclusions:
The comprehensive, 16-week, in-person, cofacilitated Final MOVE!+UP was acceptable and may improve the health of people with PTSD. Iterative development likely produced a patient-centered intervention, needing further testing.
Keywords: physical activity, weight management, health disparities, mental health, PTSD
Purpose
Post-traumatic stress disorder (PTSD) is prevalent among Veterans.1 Among Veterans Affairs (VA)-enrolled Veterans of recent conflicts alone, PTSD was the most commonly diagnosed mental health condition.2 Nearly 80% of VA-enrolled Veterans are overweight or obese,3 and PTSD increases risk for obesity, related conditions,4 and premature mortality.5 PTSD is associated with physical inactivity and poor eating behaviors,6 including binge,7 emotional,8,9 and night10 eating, likely contributing to disease burden.11 PTSD symptoms like behavioral avoidance, diminished interest in activities, negative beliefs and emotions, social isolation, and sleep disturbance may serve as physical activity and healthy eating barriers.12–16
The Department of Veterans Affairs health-care system has offered an evidence-based behavioral weight management program, MOVE!, since 2006.17,18 MOVE! uses techniques like goal setting, self-monitoring, and motivational interviewing19 primarily through in-person group sessions.17 Nearly 20% of those with at least 2 MOVE! sessions lost ≥5% baseline weight at 6 months,17 an amount associated with health benefits.20 Clinically meaningful weight loss was higher (31.6%) for the 14% of those with “intense and sustained” participation (≥8 sessions in 4–6 months).17 While promising, among those with intense and sustained participation, Veterans with PTSD were less likely to have clinically meaningful weight loss (23.7% vs 28.7%).21 Importantly, PTSD was not associated with outcomes in a randomized controlled trial (N = 409 Veterans) comparing 3 conditions: an intervention called small changes, delivered by phone or in-person, and MOVE!.22 Still, other studies found MOVE! participants with PTSD were significantly more likely to report weight loss barriers23 and that they would benefit from mental health symptom management strategies while doing MOVE!.24 Given their unique weight loss barriers and poorer weight loss in MOVE! when delivered as part of routine care, modifying MOVE! to improve effectiveness for Veterans with PTSD is warranted. Despite evidence-based programs to address weight25–27 and related conditions like diabetes28 among individuals with other mental health conditions, there are no such programs for individuals with PTSD. Importantly, VA supports efforts to tailor MOVE! to specific population needs, as indicated by the currently underway virtual Learn, Engage, Act, Process (LEAP) program, providing quality improvement support for enhancing MOVE! participation and outcomes.29
In addition to potentially improving weight loss, tailoring MOVE! for Veterans with PTSD could also potentially address PTSD symptoms, given physical activity and healthy eating can improve psychological well-being,30 including PTSD.31–35 Veterans Affairs promotes evidence-based cognitive processing therapy (CPT), and prolonged exposure (PE) for PTSD,36,37 but only one-third of Veterans who receive them reduce symptoms below the PTSD diagnostic threshold.38 It is therefore important to offer various options as part of mental health treatment for chronic PTSD.39 Tailored weight management could provide an adjunctive treatment to address limitations of weight management and PTSD care, like treatments that have successfully cotreated depression and weight26 and diabetes.28
In summary, Veterans with PTSD experience high obesity and related disease burden, and reduced MOVE! effectiveness. There are potential mental and physical health benefits of a tailored weight loss program for people with PTSD and offering such care would align with VA’s prioritization of patient-centered, whole health-focused care.40 Thus, this article describes the process of developing, piloting, and iteratively refining a tailored behavioral weight management program for Veterans with PTSD: MOVE!+UP.
Methods
Design and Setting
We conducted several pilot acceptability and feasibility tests with sequential modifications to MOVE! UP (December 2015-April 2018) at a major VA Medical Center, VA Puget Sound Health Care System, Seattle Division. This study was approved by that VA site’s institutional review board. Participants provided written informed consent.
Samples
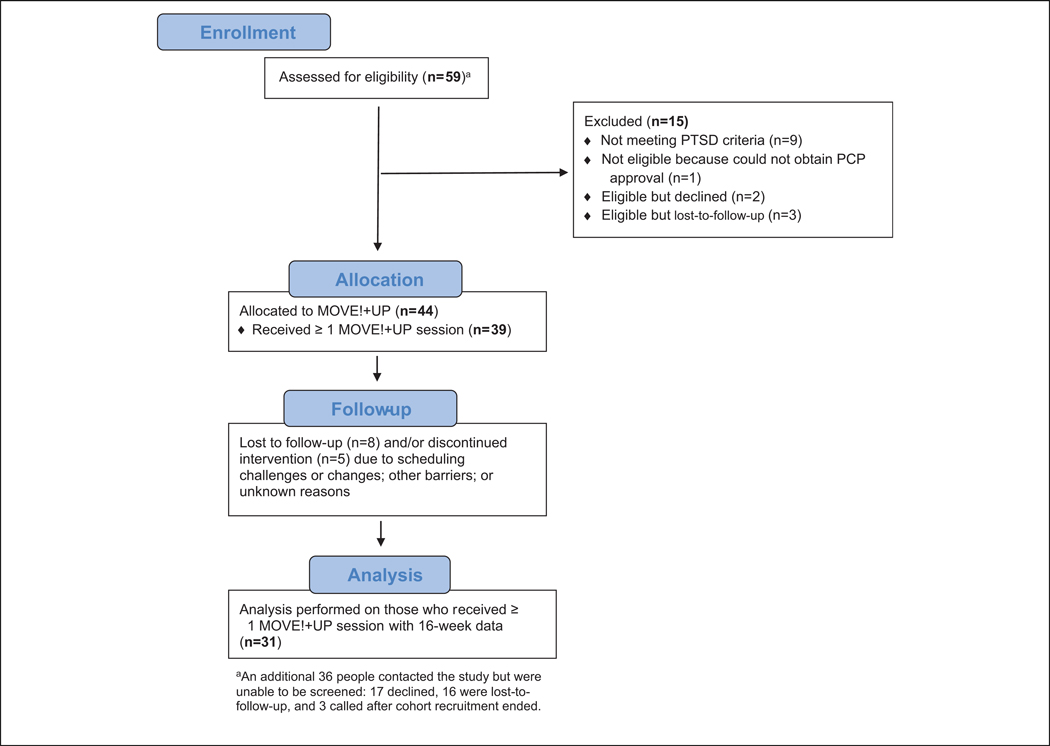
Veterans were recruited by flyers distributed in patient care areas and provider referrals. Veterans Affairs patients who were overweight or obese (body mass index [BMI] ≥25 kg/m2), had experienced trauma and had current PTSD (≥33 on PTSD Checklist 5 [PCL-5]),41 and received primary care provider (PCP) approval were eligible. Exclusion criteria were past-year participation in MOVE!+UP, not being fluent in English, having severe hearing loss, not having phone access, pregnancy, or unable to participate based on clinical judgment (eg, acute mental health or medical condition exacerbations). The Consolidated Standards of Reporting Trials (CONSORT) diagram (Figure 1) shows that 44 Veterans enrolled, 39 of whom participated in ≥1 MOVE!+UP session, and 31 of whom completed the 16-week follow-up assessment. Characteristics for those with ≥1 MOVE!+UP session are given in Table 1, stratified by MOVE!+UP Development (cohorts 1–4; n = 31) and Final (cohort 5; n = 8) Cohorts. Among those assessed for eligibility, most who declined participation cited scheduling conflicts, and the only criteria that excluded potential participants were not meeting PTSD diagnostic criteria (n = 9) or not receiving PCP approval (n = 1).
Figure 1.
MOVE!+UP CONSORT flow diagram.
Table 1.
Baseline Characteristics Among Participants With At Least 1 MOVE!+UP Session, Stratified by and Comparing Cohorts 1 to 4 and Cohort 5.
| Variable | Cohorts 1–4 (n = 31) | Cohort 5 (n = 8) | P Value |
|---|---|---|---|
| Age, mean (SD) | 56.7 (12.1) | 51.9 (12.8) | .32 |
| Male sex, % | 67.7 | 75.0 | .69 |
| Race/ethnicity, % | |||
| Non-Hispanic black | 16.7 | 25.0 | .41 |
| Other (eg, Asian, Native, Hispanic) | 20.0 | 37.5 | |
| Non-Hispanic white | 63.3 | 37.5 | |
| Married or living with significant other | 54.8 | 50.0 | .81 |
| At least high school graduate | 90.3 | 87.5 | .82 |
| Annual household income ≤$40 000 | 48.3 | 50.0 | .24 |
| Employed part- or full-time | 7.7 | 12.5 | .68 |
| Weight (lbs), mean (SD) | 244.5 (60.8) | 242.2 (44.0) | .92 |
| PTSD symptom severity (range: 0–80), mean (SD) | 56.6 (13.2) | 59.1 (9.3) | .62 |
| Insomnia severity (range: 0–28), mean (SD) | 20.7 (4.4) | 20.8 (5.3) | .99 |
| Weekly physical activity minutes, mean (SD) | 372.4 (362.0) | 783.1 (736.7) | .17 |
| Diet quality (range: 0–16; lower = better), mean (SD) | 9.1 (2.5) | 7.8 (3.6) | .23 |
| Emotional eating (range: 0–4; lower = better), mean (SD) | 1.9 (1.0) | 2.0 (0.8) | .86 |
| Mental health quality of life (range: 0–100), mean (SD) | 29.6 (6.2) | 28.9 (6.6) | .78 |
| Physical health quality of life (range: 0–100), mean (SD) | 32.7 (7.6) | 35.2 (8.7) | .43 |
Abbreviations: PTSD, post-traumatic stress disorder; SD, standard deviation.
Intervention
MOVE!+UP was developed to address unique barriers to physical activity, healthy eating, and weight loss for Veterans with PTSD by supplementing weight loss education and support offered by VA’s MOVE!17 with PTSD-relevant cognitive-behavior therapy skills.42 In addition, all MOVE!+UP in-person sessions included walking on a neighborhood sidewalk to a public park adjacent to the VA facility. The walks were intended to provide exercise, which can improve program engagement,43 and also to experientially address hypervigilance-based activity barriers44 and encourage walking in their own communities outside of MOVE!+UP sessions.
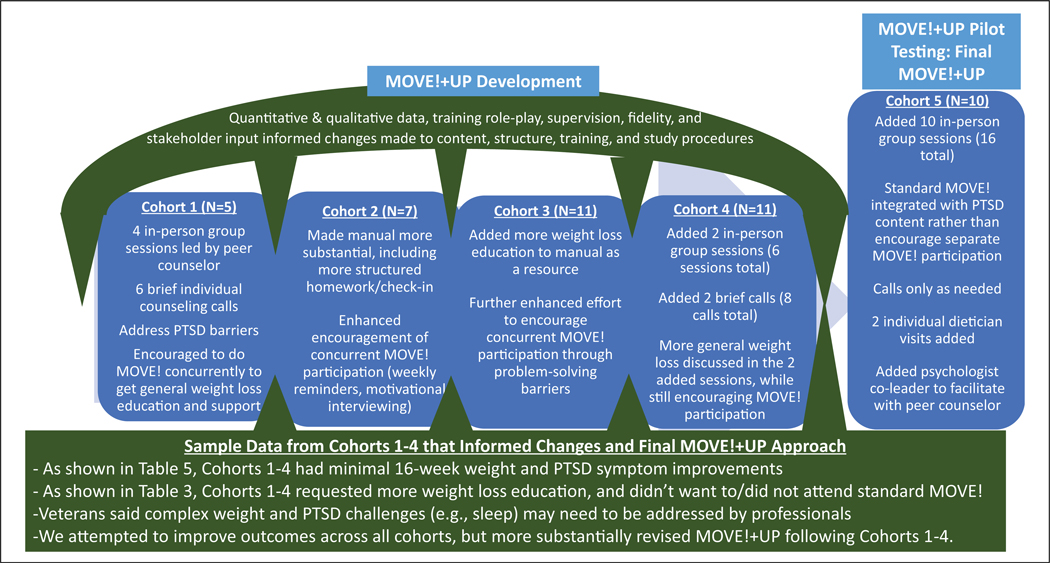
Figure 2 depicts MOVE! UP’s overall iterative refinement process, with several examples of content and structure modified over the course of the pilot. In addition to constant quality improvement based on supervision and fidelity ratings, substantive changes were made after each cohort concluded. Specifically, the principal investigator (PI) synthesized quantitative and qualitative findings, supervision and fidelity assessment process findings, and potential modifications in a 2-page document to discuss with the study team and other key stakeholders (eg, national VA leaders) to determine what changes should be made before repiloting with the following cohort. While not exhaustive of all treatment target measures used to inform refinement, a sampling of key measures and findings informing modifications are discussed in the Measures and Results sections, respectively.
Figure 2.
MOVE!+UP’s Overall Iterative Refinement Process.
MOVE!+UP Development—cohorts 1 to 4. “
Development MOVE!+UP” was intended to augment VA’s general MOVE! or non-VA weight loss interventions, from which participants were expected to receive general weight loss education. Thus, MOVE!+UP was delivered concurrent to MOVE! and was designed to be “light touch,” with few in-person sessions and brief individual counseling calls to support behavior change delivered over 16 weeks, with an emphasis on addressing PTSD-specific barriers. MOVE!+UP delivered to cohorts 1 to 3 consisted of 4 in-person 90-minute group sessions followed by 6 biweekly phone counseling sessions. Because Veterans of these cohorts consistently suggested additional general weight loss education and declined simultaneous participation in MOVE!, the version delivered to cohort 4 continued to run for 16 weeks total but added 2 in-person and 2 additional phone sessions, while still encouraging MOVE! participation. MOVE!+UP for cohorts 1 to 4 was delivered by 1 peer support counselor45,46 because peers can promote social support and community reintegration,45–47 physical activity,48 and weight loss.49
Final MOVE!+UP—cohort 5.
Final MOVE!+UP was more comprehensive and intensive, with 16 in-person 2-hour group sessions that integrated original MOVE!+UP PTSD-specific content with the standard MOVE! curriculum, which involves education, support for goal setting and activity and diet monitoring (including facilitators providing individualized feedback on diet and activity logs), and weekly weighing.50 An overview of the Final MOVE!+UP curriculum is given in Table 2. MOVE!+UP included standard MOVE! materials but most were modified at least slightly to allow for PTSD-specific content. MOVE!+UP addressed basic weight management in initial sessions and maintenance in final sessions. Although PTSD-specific barriers to weight loss were primarily addressed in sessions 5 to 10, every session contained cognitive-behavioral approaches for addressing PTSD-specific activity and healthy diet barriers (eg, thought challenging, relationship support, sleep hygiene). A 30-minute group walk to a nearby park was maintained; however, post-walk learning was enhanced in Final MOVE!+UP with more structured follow-up discussion. In addition to being led by a peer counselor, Final MOVE!+UP substantially increased health-care professional involvement by being coled by a licensed clinical psychologist to better address specialized needs. In general, the psychologist addressed PTSD-focused topics (eg, sleep), and the peer counselor addressed those outlined in VA’s Peer Support Implementation Toolkit (eg, social/community engagement, personal recovery).45 Facilitators alternated leading less specialized sections (eg, weekly check-in). Because Final MOVE!UP was designed to be a comprehensive, though specialized, MOVE! program, we used MOVE!’s clinic stop codes for capturing workload. Two individual dietician visits were also provided, as were brief, only as-needed, counseling calls.
Table 2.
Final Curriculum for MOVE!+UP Group Sessions.
| Week | Contenta |
|---|---|
| 1: Orientation/MOVE!+UP overview | Energy balance, goal setting, behavioral strategies |
| 2: Healthy eating to tip the scale | Healthy plate, portion control, nutrition facts/labels |
| 3: Physical activity to tip the scale | PA benefits and types (eg, strength training); overcoming barriers |
| 4: Eating mindfully and problem-solving barriers | Experiential mindful eating exercise, hunger/fullness scale, mindful eating tips, snack ideas, and problem-solving barriers |
| 5: Coping with PTSD to pursue health | General coping, thought challenging, grocery shopping tips |
| 6: Pursuing wellness | Sleep assessment and improvement plan, finding joy, cooking |
| 7: The role of relationships in healthy living I | Benefits of relationships for health/PTSD; strategies for enhancing relationships to improve health; meal planning |
| 8: Relationships in healthy living II | Family/friend welcome; communication; relationships and PTSD |
| 9: Community engagement | Community engagement benefits/tips, problem-solving review |
| 10: Health at any size | Ways to enhance body image; thought challenging |
| 11: Moving toward maintenance | Overcoming weight plateaus, adding challenge |
| 12: Finesse your food | Review strategies, for example, healthy plate/nutrition facts |
| 13: Stay active! | PA motivators, personal values, long-term planning |
| 14: Handling slips and setbacks | Relapse prevention, review of key diet tips. Thought challenging. |
| 15/16: MOVE!þUP progress review | Review of progress and how to continue gains going forward. |
| Sessions 1–16 | Cognitive behavior therapy for PTSD and mood; set and track activity, diet, and weight goals; and experiential learning activities. |
Abbreviations: PA, physical activity; PTSD, post-traumatic stress disorder.
Content unique to MOVE!+UP is in bold.
Intervention training/competence and fidelity.
One peer support counselor delivered MOVE!+UP to all 5 cohorts, while a licensed clinical psychologist cofacilitated Final MOVE!+UP. Training and supervision were provided by a member of the research team not directly involved in intervention delivery (the PI/first author for cohorts 1 to 4 and a study physician with health behavior change expertise for cohort 5). Training was guided by the VA Peer Support Implementation Toolkit45 and a fidelity framework.51 Procedures were focused on ensuring high-quality delivery and identifying components needing change. To promote safety and confidentiality during MOVE!+UP’s walks to a nearby park, facilitators completed additional training such as basic and cardiac life support. The peer support counselor participated in a 1-day program that teaches basic health coaching and motivational interviewing skills.52
Prior to initiating each cohort, facilitator(s) reviewed facilitator and participant manuals, received general delivery instructions, and engaged in approximately 4 audiorecorded role-play exercises, followed by supervisor feedback. Final MOVE!+UP facilitators participated in an online 1-hour MOVE! training. A 1-hour training on Veterans with PTSD and as-needed consultations were provided to the dietician for the Final MOVE! UP.
All sessions were audiorecorded and rated for delivery of planned content using a standard fidelity form (Online Appendix A provides a sample). We set a fidelity goal of covering ≥80% of session components; nonfidelity was discussed during weekly supervision. Role-play sessions and associated preliminary supervision took approximately 6 hours prior to each cohort. Ongoing supervision took approximately 1 weekly hour while delivering the 16-week MOVE!+UP.
Measures
Quantitative measures were taken at baseline and 16 weeks post-baseline, at MOVE!+UP’s conclusion, to inform iterative refinement modifications. All qualitative and quantitative measures were administered by trained research staff. The PI observed and provided feedback intermittently throughout the study. Participants received $15 for completing each major assessment component (eg, questionnaire, 1-hour qualitative interview) at each time point. Where relevant, quantitative measure score ranges are included in Table 1.
Sociodemographic characteristics.
Veterans self-reported age, sex, marital status, educational attainment, employment status, and annual household income. Participants were asked whether they were “of Hispanic, Latino or Spanish origin.” If yes, they recorded the specific origin. They were also asked to record whether they were white, black or African-American, American Indian or Alaskan Native, Asian or Pacific Islander, and/or other. Because of small cell sizes, race/ethnicity was combined to be non-Hispanic white, non-Hispanic black, and other race/ethnicities.
MOVE!+UP and MOVE! engagement.
Because cohorts were offered different numbers of in-person sessions, we calculated the proportion who attended at least half of planned in-person sessions. Because cohort 5 was offered 16 sessions, the Final MOVE!+UP indicator was compatible with MOVE!’s definition of optimal “intense and sustained” engagement (≥8 sessions 4 to 6 months after enrollment17). Because we encouraged cohorts 1 to 4 to participate in MOVE!, we assessed their 16-week intervention period MOVE! engagement.
Body mass index and weight.
Height and weight were measured at baseline to assess eligibility BMI. Follow-up weight was collected using the same medical-grade scale. We calculated change in pounds, percentage of baseline weight lost, and percentage achieving clinically meaningful weight loss (≥5% loss of baseline weight).20
Mental health.
Symptoms of PTSD were measured with the PCL-541,53 to evaluate eligibility and assess change. The Insomnia Severity Index was used to assess sleep difficulties.54 Higher scores reflect greater symptom severity.
Physical activity.
We calculated total weekly walking, moderate, and vigorous leisure and active transportation physical activity minutes with the long-form International Physical Activity Questionnaire,55 using standard cleaning and scoring procedures.56
Eating behaviors.
Diet quality was measured with the 8-item Starting the Conversation,57 a self-report measure that assesses frequency of consuming unhealthy snacks, fast food, desserts, sugar-sweetened beverages, and fats; fruits and vegetables; and healthy proteins. Emotional eating was assessed with the Emotional Overeating Questionnaire.58 Higher scores suggest poorer eating behaviors.
Health-related quality of life.
The Short-Form Health Survey (SF-12)’s two subscales mental (MCS) and physical (PCS) component summaries were administered.59 Higher scores reflect greater quality of life (QoL).
Qualitative interviews.
An approximately 1-hour semistructured qualitative interview was conducted at the conclusion of the full set of in-person sessions for that cohort (cohorts 1–3: 4 weeks; cohort 4: 6 weeks; and cohort 5: 16 weeks). Interview topics included impressions of MOVE!+UP content and study procedures; suggestions for improvement; and comparison with MOVE!, among those with any MOVE! experience. Cohorts 1 to 4 were reinterviewed for approximately 20 minutes at 16 weeks regarding experiences with brief counseling calls. Guides were modified iteratively to ensure thoroughness and relevance.
Satisfaction.
Cohort 5 completed a 30-item questionnaire assessing satisfaction with MOVE!+UP content and structure on a 1 to 5 Likert scale and could provide suggestions for each domain.
Analysis
Data analysis was conducted following each cohort to identify areas needing modification.
Quantitative analysis.
Questionnaire and health outcome data were entered into a Microsoft Access database and analyzed with SAS (statistical program). Frequencies and descriptive statistics were calculated. Change in baseline to 16-week outcomes was evaluated by calculating unadjusted paired t tests; P values of .05 or less were considered statistically significant. Quantitative analyses did not emphasize hypothesis testing or detecting an effect60 and were conducted among treatment and assessment completers, rather than as intent-to-treat. This was due to the small overall and within-cohort sample sizes for this pilot study and because the purpose of analyses was to establish proof of concept and identify potential areas needing change based on whether or not treatment target signals were detected.
Qualitative analysis.
Following each of cohorts 1 to 4, the PI read each qualitative interview transcript, highlighting and summarizing key findings, particularly those with implications for change. At the conclusion of the pilot, we conducted a formal template analysis of all transcripts for all cohorts using Atlas.ti qualitative analysis software to further summarize findings and confirm the post-cohort rapid process used to guide refinement. Template analysis is well suited when the aim is to investigate themes that have a clear structure,61 appropriate for the present study because we were focused narrowly on acceptability and usefulness of main MOVE!+UP domains, rather than on generating theory or emergent themes. Prior to conducting the template analysis, we developed a template of a priori codes to capture acceptability and areas of suggested change for each of the main MOVE!+UP components: overall structure, walks, weight loss and PTSD education and support, and facilitation. We then reviewed all transcripts, applying that template of codes, to identify central themes, corresponding to relevant quotations. Findings generally confirmed those from the post-cohort rapid refinement phase and are summarized in Tables 3 and 4.
Table 3.
Qualitative Feedback From Cohort 1 to 4 Participants.
| Domain | Overall Takeaways | Participant Quotes That Highlight the Takeaway |
|---|---|---|
| Structure | • Appreciated group support, but wanted more opportunities to connect and for longer duration. • Many found calls unstructured and less helpful. Many weren’t clear about the function/purpose and requested more in-person sessions instead. Calls were challenging to coordinate/track. |
“4 weeks, 1 hour a week, isn’t enough … ” “It seemed to me that the phone calls didn’t really do anything for me.” |
| Walk | • Appreciated the opportunity to exercise and connect with others but didn’t highlight the experiential learning focus. | “It gives you an accomplishment that you’ve done, that you can take to the bank so to speak.” |
| Weight Loss | • Many wanted more specific, directed support and feedback for improving physical activity and healthy eating. | “The log would be great if. … somebody. … went back through that log with you … ” “They did not get into specifics about what you should or shouldn’t eat … ” |
| PTSD | • Wanted more emphasis on how PTSD affects weight and related behaviors and what to do about it. | “Not enough on the relationship between PTSD and [weight], other than the fact that PTSD is one of those detriment factors in making that move to improve.” |
| Facilitators | • Appreciated the peer support’s common ground. • Wanted complementary input from other healthcare professional(s) regarding weight loss and PTSD. |
“[Peer support is] helpful because I know … that it’s another veteran and they’ve gone through some of the things that I’ve gone through.” “I’d [have] someone there that’s a counselor or something like that … They would probably hold more weight in conversation … To me, that needs to be addressed by someone who is a professional, instead of a layman.” |
| Compared to MOVE! | • Several participated in MOVE! before. Few wanted to participate in MOVE!, preferring MOVE!+UP because it addressed PTSD. | “[MOVE!] didn’t teach you how to deal with yourself and your emotions or when you are having your symptoms.” |
Abbreviation: PTSD, post-traumatic stress disorder.
Table 4.
Qualitative Feedback From Cohort 5 Participants.
| Domain | Overall Takeaways | Participant Quotes That Highlight the Takeaway |
|---|---|---|
| Structure | • Found the structure of sessions and homework supported their goals. | “When I was called to doing my weekly food intake, and my weekly exercise, there was a structured sheet that I filled out. And that started me out on being structured and paying attention.” |
| Walk | • Provided opportunities to exercise and connect with other group members, while further incorporating educational content. | “I think it really did help. It showed me that I could do it.” “Me and 2 or 3 guys bonded, We’d talk about what was going on at home and how we were trying to follow the program. We formed a little camaraderie.” |
| Weight Loss | • Felt they were educated about how to lose weight, and that this resulted in weight loss. | “Reading labels, food labels. Serving portions and all of that. And talking about being mindful of what you’re eating … It helped me and my wife be more aware of what we were doing, what we were buying and stuff … ” “My eating changed, my physical activity changed … now it has become a habit … ” “I went out and bought another pair of pants. One size smaller … which felt good.” |
| PTSD | •Participants identified how PTSD symptoms impeded weight loss efforts. • Sessions addressed PTSD symptoms. |
“It opened up my eyes to how I was eating … Basically, if I was getting.depressed or into my thoughts, or being alone or with the PTSD I’d eat more.” “[It helped me] do things that are more relaxing for me to do, and get me out of my shell. And interact with other people that are suffering from PTSD too.” |
| Facilitators | • Participants regarded facilitators and the input of affiliated professionals positively. | “Besides just the support, knowledge and positive feedback that they gave us, they were just people that I trusted, which says a lot for someone with PTSD.” “I liked also knowing that [the peer] had been there, he’s been in the service and … knows … the things that go on.” |
| Compared to Move! | • MOVE!+UP was regarded as more comprehensive and helpful due to the explicit focus on PTSD. | “It’s more thorough. It’s different for people with PTSD too. The other MOVE! they didn’t ask you what your symptoms were … But this one it’s geared specifically for people with PTSD. The other one, they don’t care, whatever is going on.” |
Abbreviation: PTSD, post-traumatic stress disorder.
Results
Quantitative and Qualitative Findings
Table 1 presents baseline characteristics for MOVE! UP participants with 1 MOVE!+UP session, stratified by cohorts 1 to 4 and cohort 5. Most participants were male, had completed at least high school, and/or were unemployed. Approximately half were married or living with a significant other and/or had an annual household income of $40,000 or less. Insomnia severity was high, and mental and physical health QoL were low. Participants reported high but variable levels of physical activity. There were no significant differences in characteristics of those in cohorts 1 to 4 versus cohort 5.
Development participants (cohorts 1 to 4).
Among the n = 31 with ≥1 MOVE!+UP session, 74% attended at least half of in-person sessions (data not in tables). However, among the subset (n = 24) who also attended the 16-week assessment, only 12.5% lost ≥5% of baseline weight, which corresponded to an average percentage baseline weight loss of 0.7% (SD = 3.6; data not in tables). Despite substantial efforts to promote simultaneous participation, only 2 participated in any MOVE! sessions, one of whom completed an orientation and declined further involvement, and another who participated in several MOVE! sessions concurrent with MOVE!+UP (data not in tables). Table 5 presents baseline to 16-week changes for the n 24 who participated in ≥1 MOVE!+UP session and the 16-week follow-up assessment. Cohorts 1 to 4 demonstrated only modest improvements on weight and other outcomes, though several were statistically significant: PTSD symptom severity, diet quality, emotional eating, and mental health QoL.
Table 5.
Changes From Baseline to 16 Weeks Among Participants With At Least 1 MOVE!+UP Session.a
| Cohorts 1–4 (n = 24) | Cohort 5 (n = 7) | |||
|---|---|---|---|---|
| Outcomes | Mean (SD) | P Value | Mean (SD) | P Value |
| Weight change | ||||
| Weight change, lbs | −1.8 (8.2) | .291 | −14.0 (3.7) | <.001 |
| Mental health | ||||
| PTSD symptom severity (range: 0–80) | −6.7 (11.7) | .013 | −17.9 (12.2) | .008 |
| Insomnia severity (range: 0–28) | −1.0 (5.6) | .398 | −7.7 (4.2) | .003 |
| Health behavior | ||||
| Weekly physical activity minutes | 282.8 (773.9) | .094 | 290.0 (611.2) | .298 |
| Diet quality (range: 0–16; lower = better) | −2.6 (3.7) | .003 | −2.9 (3.1) | .052 |
| Emotional eating (range 0–4) | −0.6 (0.9) | .005 | −0.5 (0.4) | .015 |
| Quality of life | ||||
| Mental health (range: 0–100) | 4.0 (5.7) | .004 | 3.7 (12.8) | .472 |
| Physical health (range: 0–100) | 1.5 (6.7) | .321 | −0.9 (7.3) | .769 |
Abbreviations: PTSD, post-traumatic stress disorder; SD, standard deviation.
Results presented for those who attended the 16-week assessment.
Qualitative findings for cohorts 1 to 4 are presented in Table 3. Participants had overall positive impressions and were particularly positive about the group walk to a nearby park and benefits of connecting with other group members. Despite substantial efforts to promote simultaneous MOVE! engagement, participants reported being hesitant to attend MOVE! due to perceived inconvenience, lack of PTSD tailoring, or having found it unhelpful during previous MOVE! participation. Many instead requested more specific, in-depth weight loss education such as that offered in MOVE! be integrated with MOVE!+-UP’s PTSD content. Many requested more sessions in order to be able to build group cohesion, obtain more support for weight loss, and more fully address the connection between PTSD and weight. While some appreciated the counseling calls, several found them less beneficial than in-person sessions. While participants greatly appreciated the peer counselor’s support, they requested additional health professional involvement to address specialized PTSD and weight loss needs.
Final MOVE!+UP participants (cohort 5).
Among the n = 8 who participated in ≥1 MOVE!+UP session, three-quarters participated in at least half of in-person sessions (data not in tables). Among the subset (n = 7) who also attended the 16-week assessment, 71% experienced clinically meaningful baseline weight loss of 5%, corresponding to an average percentage baseline weight loss of 6.1% (SD = 2.1; data not in tables). Baseline to 16-week changes are presented in Table 5 for the n = 7 who participated in ≥1 MOVE! UP session and the 16-week assessment. Participants lost a statistically significant amount of weight and reported statistically significant improvements on PTSD symptom severity, insomnia, diet quality, and emotional eating.
Qualitative findings for cohort 5 are presented in Table 4. Cohort 5 pilot participants reported strong satisfaction in both qualitative interviews and in the cohort 5 satisfaction measure, with an average mean score of 4.3 (SD = 0.3). They described comprehensive improvements in health, mental health, and QoL.
Discussion
This study reports the development and initial evaluation of a novel weight loss intervention called MOVE!+UP, designed to address weight loss barriers for people with PTSD that interfere with traditional weight loss program effectiveness.21 Quantitative and qualitative findings suggest MOVE!+UP may be an acceptable and feasible approach for improving the health and mental health of Veterans with PTSD.
Qualitative and quantitative findings informed numerous changes made to MOVE!+UP. The version delivered to cohorts 1 to 4 was brief and meant to augment MOVE!, delivered solely by a peer support counselor. MOVE! UP was modified to be more intensive and comprehensive because cohort 1 to 4 participants were unwilling to attend the separate, nontailored MOVE! despite substantial efforts to promote simultaneous engagement, had minimal weight loss, and requested more health-care professional involvement. Thus, Final MOVE!+UP combined MOVE!’s general weight loss materials and approach with the PTSD focus of MOVE!+UP, was co-delivered by a licensed clinical psychologist and peer support counselor, and included 2 individual dietician visits. Although changes made MOVE! UP more resource-intensive, preliminary pilot findings suggest it was likely worthwhile, given Final MOVE!+UP cohort participants reported high satisfaction and meaningful weight,20 PTSD symptom,62 and insomnia63 improvements. Given more promising weight and PTSD changes among cohort 5 participants relative to earlier cohorts, it was surprising that diet and physical activity change indicators were comparable across Development and Final Cohorts (and mental health QoL superior for cohorts 1–4). Insomnia severity, on the other hand, is one factor that was more explicitly targeted in Final MOVE! UP and it improved significantly and meaningfully for cohort 5 but not cohorts 1 to 4, offering one possible explanation for cohort 5’s improved PTSD and weight outcomes.
Given the breadth of changes and the uncontrolled pilot design, it is impossible to know whether and which modified MOVE!+UP features might have contributed to MOVE!+-UP’s positive outcomes. Still, Final MOVE! UP is consistent with behavioral weight loss treatment recommendations to provide more intensive, longer-term interventions.20 It also integrated 2 individualized dietician visits, which can improve weight loss.64 Because Final MOVE!+UP was delivered by 2 providers—a psychologist and peer support counselor—findings may offer insights into optimal facilitation. In general, group cofacilitation has been associated with increased satisfaction and perceived benefit for a variety of possible reasons.65 For example, in Final MOVE!+UP, cofacilitation may have eased the peer facilitator’s burden for handling logistics, better allowing for participant learning during weekly weigh-ins and providing individualized feedback on activity and diet logs. Moreover, having a licensed psychologist and a peer support counselor facilitate exposed participants to a wider range of resources, perspectives, and expertise. Cofacilitating behavioral weight management may be particularly important in the context of MOVE!+UP, given the high medical complexity of Veterans with PTSD,4 necessitating more specialized content. Although prior research has shown peer support/community health workers can effectively support weight loss,66 our findings may suggest that outcomes could be enhanced with the complementary support of a licensed health-care professional. Such a cofacilitation model aligns with VA peer support recommendations,45 which encourage peer support counselors to provide support and health-care community connection that draws on their lived experiences, rather than replacing health-care professionals trained to deliver complex behavioral interventions.
MOVE!+UP was refined over the course of this pilot study based on quantitative and qualitative data, stakeholder input, and process observations. We continuously evaluated whether MOVE! UP was affecting key intervention targets and if not, sought to understand why, informing changes to intervention content and structure, as well as other procedures (eg, supervision process, measures administered based on new intervention targets). Although iteratively refining MOVE! UP appears to have yielded a more valuable, acceptable, and feasible program and study procedures, there were challenges. We made frequent modifications to human subjects protocols, training procedures, and study databases, and sought additional funding to run cohort 5’s pilot. In addition, we could not combine and analyze data for all participants, given cohorts 1 to 4 and cohort 5 received very different interventions, reducing statistical power we otherwise could have derived from the combined sample. Finally, rather than a traditional investigator-driven study, iterative refinement required centering the voices of Veterans and other stakeholders, necessitating flexibility and humility. Future studies should consider how various intervention features will affect iterative refinement timing and process. For example, a shorter program is easier to turn around and repilot. Group-based MOVE! UP provided natural markers between cohorts for refinement, while an individual program would require developing a priori evaluation and modification time points. Challenges notwithstanding, we believe iterative refinement was valuable, given it likely produced a more patient-centered, whole-health intervention that may improve weight and PTSD.
Limitations
Several factors may limit generalizability. This study was conducted among overweight Veterans with PTSD receiving VA care, so it is unclear whether findings generalize to non-Veterans or Veterans receiving non-VA care. Given civilians with PTSD may also benefit from MOVE!+UP, future studies should include non-Veterans. Because the purpose of this uncontrolled pilot’s analyses was not to determine effectiveness but to establish proof of concept and to identify needed changes based on the experiences of those who actually received the intervention, we describe the 39 of 44 participants with 1 MOVE!+UP session and assessed changes among 31 of 39 with 16-week data. Thus, findings cannot generalize to those who did not participate or those who did not complete follow-up assessment. Nonetheless, characteristics were similar to Veterans with PTSD receiving MOVE!, although this study had more women Veterans.21 Few participants were employed, so MOVE! UP may need adaptation to reach employed people (eg, incorporating telehealth).
We conducted a series of small uncontrolled pilots; as such observed outcomes may not be attributable to the intervention. MOVE!+UP must be tested further using a fully powered and randomized design with adequate controls. While this study’s primary quantitative outcome, weight, was measured directly, others were self-reported. While we made every effort to encourage Veterans to provide honest and open responses—making it clear we would use their data to inform modifications—responses were subject to social desirability bias.
Conclusions
Final MOVE!+UP may provide an alternative treatment for overweight people with PTSD, which could be delivered as a specialized MOVE! program, with anticipated VA support given increasing efforts to enhance MOVE! to meet specific population needs.29 Further research should determine whether MOVE!+UP outperforms usual care for Veterans with PTSD in addressing PTSD and weight. Iteratively developing MOVE!+UP appears to have produced a more patient-centered and potentially beneficial intervention. Engaging participants as cocreators in intervention development is a valuable approach for health promotion intervention development.
Supplementary Material
So What?
What is already known on this topic?
Veterans with post-traumatic stress disorder (PTSD) have high obesity rates and worse weight loss outcomes, likely due to unique weight loss barriers.
What does this article add?
This article describes a novel weight loss program, MOVE!+UP, which was developed and piloted to address barriers to weight loss for Veterans with PTSD. The article also describes a practical iterative refinement process used to develop the program.
What are the implications for health promotion practice or research?
MOVE!+UP shows promise for improving weight and PTSD among Veterans but should be tested in a randomized controlled trial to determine whether it outperforms existing weight management and PTSD care. This study’s iterative refinement approach could be used to develop other health behavior programs.
Acknowledgments
We thank Marie Lutton, Jeff Rodenbaugh, and Katherine Raffle for their work on this project. We also extend heartfelt thanks to the Veteran participants who co-created MOVE! UP through their participation in this study.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a VA Health Services Research & Development Career Development Award [CDA 12-263; 2015-2020] and local VA Puget Sound Research & Development seed grant funding.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental Material
Supplemental material for this article is available online.
References
- 1.Gradus J. Epidemiology of PTSD; 2013. https://www.mentalhealth.va.gov/coe/cih-visn2/Documents/Provider_Education_Handouts/Epidemiology_of_PTSD_Version_3.pdf. Accessed May 1, 2019.
- 2.Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Arch Intern Med. 2007;167(5): 476–482. [DOI] [PubMed] [Google Scholar]
- 3.Breland JY, Phibbs CS, Hoggatt KJ, et al. The Obesity epidemic in the veterans health administration: prevalence among key populations of women and men veterans. J Gen Intern Med. 2017;32(suppl 1):11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dedert EA, Calhoun PS, Watkins LL, Sherwood A, Beckham JC. Posttraumatic stress disorder, cardiovascular, and metabolic disease: a review of the evidence. Ann Behav Med. 2010;39(1): 61–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kilbourne AM, Ignacio RV, Kim HM, Blow FC. Datapoints: Are VA patients with serious mental illness dying younger? Psychiatr Serv. 2009;60(5):589. [DOI] [PubMed] [Google Scholar]
- 6.Hall KS, Hoerster KD, Yancy WS Jr. Post-traumatic stress disorder, physical activity, and eating behaviors. Epidemiol Rev. 2015;37:103–115. [DOI] [PubMed] [Google Scholar]
- 7.Hoerster KD, Jakupcak M, Hanson R, et al. PTSD and depression symptoms are associated with binge eating among US Iraq and Afghanistan veterans. Eat Behav. 2015;17:115–118. [DOI] [PubMed] [Google Scholar]
- 8.Talbot LS, Maguen S, Epel ES, Metzler TJ, Neylan TC. Posttraumatic stress disorder is associated with emotional eating. J Trauma Stress. 2013;26(4):521–525. [DOI] [PubMed] [Google Scholar]
- 9.Dorflinger LM, Masheb RM. PTSD is associated with emotional eating among veterans seeking treatment for overweight/obesity. Eat Behav. 2018;31:8–11. [DOI] [PubMed] [Google Scholar]
- 10.Dorflinger LM, Ruser CB, Masheb RM. Night eating among veterans with obesity. Appetite. 2017;117:330–334. [DOI] [PubMed] [Google Scholar]
- 11.Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009; 6(4):e1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baron KG, Reid KJ, Zee PC. Exercise to improve sleep in insomnia: exploration of the bidirectional effects. J Clin Sleep Med. 2013;9(8):819–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boutcher SH, Dunn SL. Factors that may impede the weight loss response to exercise-based interventions. Obes Rev. 2009;10(6): 671–680. [DOI] [PubMed] [Google Scholar]
- 14.St-Onge MP. The role of sleep duration in the regulation of energy balance: effects on energy intakes and expenditure. J Clin Sleep Med. 2013;9(1):73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brug J. Determinants of healthy eating: motivation, abilities and environmental opportunities. Fam Pract. 2008;25(suppl 1): i50–55. [DOI] [PubMed] [Google Scholar]
- 16.Sherwood NE, Jeffery RW. The behavioral determinants of exercise: implications for physical activity interventions. Annu Rev Nutr. 2000;20:21–44. [DOI] [PubMed] [Google Scholar]
- 17.Kahwati LC, Lance TX, Jones KR, Kinsinger LS. RE-AIM evaluation of the Veterans Health Administration’s MOVE! Weight Management Program. Transl Behav Med. 2011;1(4):551–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kinsinger LS, Jones KR, Kahwati L, et al. Design and dissemination of the MOVE! Weight-Management Program for Veterans. Prev Chronic Dis. 2009;6(3):A98. [PMC free article] [PubMed] [Google Scholar]
- 19.Samdal GB, Eide GE, Barth T, Williams G, Meland E. Effective behaviour change techniques for physical activity and healthy eating in overweight and obese adults; systematic review and meta-regression analyses. Int J Behav Nutr Phys Act. 2017; 14(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129(25 suppl 2):S102–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hoerster KD, Lai Z, Goodrich DE, et al. Weight loss after participation in a National VA weight management program among veterans with or without PTSD. Psychiatr Serv. 2014;65(11): 1385–1388. [DOI] [PubMed] [Google Scholar]
- 22.Janney CA, Masheb RM, Lutes LD, et al. Mental health and behavioral weight loss: 24-month outcomes in Veterans. J Affect Disord. 2017;215:197–204. [DOI] [PubMed] [Google Scholar]
- 23.Klingaman EA, Hoerster KD, Aakre JM, Viverito KM, Medoff DR, Goldberg RW. Veterans with PTSD report more weight loss barriers than Veterans with no mental health disorders. Gen Hosp Psychiatry. 2016;39:1–7. [DOI] [PubMed] [Google Scholar]
- 24.Hoerster KC, Afari N, Gundy J, et al. Mental health considerations for optimizing behavioral weight management interventions with obese Veterans (symposium). Symposium presented at: 35th Annual Meeting of the Society of Behavioral Medicine; 2014; Philadelphia, PA Annals of Behavioral Medicine;47:s145. [Google Scholar]
- 25.Daumit GL, Dickerson FB, Wang NY, et al. A behavioral weight-loss intervention in persons with serious mental illness. N Engl J Med. 2013;368(17):1594–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ma J, Rosas LG, Lv N, et al. Effect of integrated behavioral weight loss treatment and problem-solving therapy on body mass index and depressive symptoms among patients with obesity and depression: the RAINBOW randomized clinical trial. JAMA. 2019;321(9):869–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Naslund JA, Whiteman KL, McHugo GJ, Aschbrenner KA, Marsch LA, Bartels SJ. Lifestyle interventions for weight loss among overweight and obese adults with serious mental illness: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2017;47:83–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cummings DM, Lutes LD, Littlewood K, et al. Randomized trial of a tailored cognitive behavioral intervention in type 2 diabetes with comorbid depressive and/or regimen-related distress symptoms: 12-month outcomes from COMRADE. Diabetes Care. 2019;42(5):841–848. [DOI] [PubMed] [Google Scholar]
- 29.Damschroder LJ. Learn, Engage, Act, Process (LEAP) for MOVE. VA Office of Research and Development (QUERI 15–286); 2016. https://clinicaltrials.gov/ct2/show/NCT02825680. Accessed October 31, 2019.
- 30.Walsh R. Lifestyle and mental health. Am Psychol. 2011;66(7): 579–592. [DOI] [PubMed] [Google Scholar]
- 31.Goldstein LA, Mehling WE, Metzler TJ, et al. Veterans group exercise: a randomized pilot trial of an integrative exercise program for veterans with posttraumatic stress. J Affect Disord. 2018; 227:345–352. [DOI] [PubMed] [Google Scholar]
- 32.Hall KS, Gregg J, Bosworth HB, et al. Physical activity counseling promotes physical and psychological resilience in older veterans with posttraumatic stress disorder. Ment Health Phys Act. 2016;11:53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johannessen KB, Berntsen D. Losing the symptoms: weight loss and decrease in posttraumatic stress disorder symptoms. J Clin Psychol. 2013;69(6):655–660. [DOI] [PubMed] [Google Scholar]
- 34.LeardMann CA, Kelton ML, Smith B, et al. Prospectively assessed posttraumatic stress disorder and associated physical activity. Public Health Rep. 2011;126(3):371–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smith E, Schuler P, Cosio-Lima L, et al. A treatment for rape victims with posttraumatic stress disorder utilizing therapy and aerobic exercise. Paper presented at: American College of Sports Medicine 58th Annual Meeting; June 2011; Denver, CO Medicine & Science in Sports & Exercise;43:818. [Google Scholar]
- 36.U.S. Department of Veterans Affairs, U.S. Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder; 2017. https://www.healthquality.va.gov/guidelines/MH/ptsd/VADoDPTSDCPGFinal012418.pdf. Accessed May 1, 2019.
- 37.Watkins LE, Sprang KR, Rothbaum BO. Treating PTSD: a review of evidence-based psychotherapy interventions. Front Behav Neurosci. 2018;2(12):258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Steenkamp MM, Litz BT, Hoge CW, Marmar CR. Psychotherapy for military-related PTSD: a review of randomized clinical trials. JAMA. 2015;314(5):489–500. [DOI] [PubMed] [Google Scholar]
- 39.Shalev A, Liberzon I, Marmar C. Post-traumatic stress disorder. N Engl J Med. 2017;376:2459–2469. [DOI] [PubMed] [Google Scholar]
- 40.U.S. Department of Veterans Affairs Office of Patient Centered Care and Cultural Transformation. Whole health; 2019. https://www.va.gov/wholehealth/. Accessed November 20, 2019.
- 41.Bovin MJ, Marx BP, Weathers FW, et al. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL-5) in veterans. Psychol Assess. 2016;28(11):1379–1391. [DOI] [PubMed] [Google Scholar]
- 42.Abramowitz JS. The practice of exposure therapy: relevance of cognitive-behavioral theory and extinction theory. Behav Ther. 2013;44(4):548–558. [DOI] [PubMed] [Google Scholar]
- 43.Spring B, Sohn MW, Locatelli SM, et al. Individual, facility, and program factors affecting retention in a national weight management program. BMC Public Health. 2014;14:363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rutter LA, Weatheril RP, Krill SC, Orazem R, Taft CT. Posttraumatic stress disorder symptoms, depressive symptoms, exercise, and health in college students. Psychol Trauma. 2013;5(1):56–61. [Google Scholar]
- 45.Chinman M, Henze K, Sweeney P. Peer specialist toolkit: implementing peer support services in VHA. 2012. http://www.mirecc.va.gov/visn4/docs/Peer_Specialist_Toolkit_FINAL.pdf. Accessed September 22, 2013.
- 46.Jain S, McLean C, Adler E, et al. Does the integration of peers into the treatment of adults with posttraumatic stress disorder improve access to mental health care? A literature review and conceptual model. J Trauma Stress Disor Treat. 2013;2:3. [Google Scholar]
- 47.Chinman M, Oberman RS, Hanusa BH, et al. A cluster randomized trial of adding peer specialists to intensive case management teams in the veterans health administration. J Behav Health Serv Res. 2015;42(1):109–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Webel AR, Okonsky J, Trompeta J, Holzemer WL. A systematic review of the effectiveness of peer-based interventions on health-related behaviors in adults. Am J Public Health. 2010;100(2): 247–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leahey TM, Wing RR. A randomized controlled pilot study testing three types of health coaches for obesity treatment: professional, peer, and mentor. Obesity. 2013;21(5):928–934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.U.S. Department of Veterans Affairs. MOVE! weight management program; 2018. https://www.move.va.gov/. Accessed March 15, 2018.
- 51.Resnick B, Bellg AJ, Borrelli B, et al. Examples of implementation and evaluation of treatment fidelity in the BCC studies: where we are and where we need to go. Ann Behav Med. 2005; 29(suppl):46–54. [DOI] [PubMed] [Google Scholar]
- 52.Kearney LK, Post EP, Zeiss A, Goldstein MG, Dundon M. The role of mental and behavioral health in the application of the patient-centered medical home in the Department of Veterans Affairs. Transl Behav Med. 2011;1(4):624–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489–498. [DOI] [PubMed] [Google Scholar]
- 54.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297–307. [DOI] [PubMed] [Google Scholar]
- 55.Craig CL, Marshall AL, Sjostrom M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. [DOI] [PubMed] [Google Scholar]
- 56.International Physical Activity Questionnaire (IPAQ). Guidelines for data processing and analysis of the international physical activity questionnaire (IPAQ)–short and long forms; 2005. www.ipaq.ki.se/scoring.pdf. Accessed October 10, 2011.
- 57.Paxton AE, Strycker LA, Toobert DJ, Ammerman AS, Glasgow RE. Starting the conversation performance of a brief dietary assessment and intervention tool for health professionals. Am J Prev Med. 2011;40(1):67–71. [DOI] [PubMed] [Google Scholar]
- 58.Masheb RM, Grilo CM. Emotional overeating and its associations with eating disorder psychopathology among overweight patients with binge eating disorder. Int J Eat Disord. 2006; 39(2):141–146. [DOI] [PubMed] [Google Scholar]
- 59.Ware J Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. [DOI] [PubMed] [Google Scholar]
- 60.Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63(5): 484–489. [DOI] [PubMed] [Google Scholar]
- 61.King N. Template analysis In: Syman C, Cassell G, eds. Qualitative Methods and Analysis in Organisational Research: A Practical Guide. London: Sage; 1998. [Google Scholar]
- 62.Stefanovics EA, Rosenheck RA, Jones KM, Huang G, Krystal JH. Minimal Clinically Important Differences (MCID) in assessing outcomes of post-traumatic stress disorder. Psychiatr Q. 2018; 89(1):141–155. [DOI] [PubMed] [Google Scholar]
- 63.Morin CM, Belleville G, Belanger L, Ivers H. The Insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Williams LT, Barnes K, Ball L, Ross LJ, Sladdin I, Mitchell LJ. How effective are dietitians in weight management? A systematic review and meta-analysis of randomized controlled trials. Health-care (Basel). 2019;7(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kivlighan DM, London K, Miles JR. Are two heads better than one? The relationship between number of group leaders and group members, and group climate and group member benefit from therapy. Group Dyn-Theor Res. 2012;16(1):1–13. [Google Scholar]
- 66.Katula JA, Vitolins MZ, Rosenberger EL, et al. One-year results of a community-based translation of the diabetes prevention program: healthy-living partnerships to prevent diabetes (HELP PD) project. Diabetes Care. 2011;34(7):1451–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.