Abstract
Background
In shoulder arthroplasty, cerclage fixation techniques are used to stabilize osteotomies, fractures, and allografts. Fixation techniques including cerclage with metal and polymer cables have been described. The purpose of this study was to evaluate suture cerclage fixation of the humeral shaft during shoulder arthroplasty.
Materials and methods
Shoulder arthroplasty cases performed from 2012-2017 by 3 fellowship-trained shoulder arthroplasty surgeons were reviewed. Cases in which suture cerclage was used for osteotomy, fracture, or allograft fixation were identified. Demographic data, indications, implant types, fixation techniques, and complications were reviewed. Postoperative radiographs were analyzed for union, component loosening, and loss of fixation. American Shoulder and Elbow Surgeons and Single Assessment Numeric Evaluation scores were collected preoperatively and postoperatively.
Results
A total of 27 patients (3 primary and 24 revision cases) with a mean age of 69.6 years (range, 28-88 years) were available for follow-up at a mean of 12.6 months (range, 0.8-42.3 months) postoperatively. Humeral osteotomy alone was performed in 15 cases. Allograft alone was used in 1 case. Both allograft and osteotomy were used in 6 cases. Complications occurred in 3 patients (11%), comprising 1 postoperative periprosthetic fracture and 2 prosthetic joint infections; all required further surgery. Radiographs at final follow-up showed healing of all osteotomies and fractures. No hardware failure or implant loosening occurred. The mean postoperative American Shoulder and Elbow Surgeons and Single Assessment Numeric Evaluation scores were significantly improved (α = .05) compared with preoperative scores, from 21.4 to 44.5 (P = .002) and from 26.7 to 74.1 (P < .001), respectively.
Conclusion
Suture cerclage is safe and effective for humeral fixation in shoulder arthroplasty.
Keywords: Shoulder arthroplasty, cerclage, suture cerclage, revision shoulder arthroplasty
The incidence of shoulder arthroplasty continues to grow, particularly as indications for reverse total shoulder arthroplasty (RTSA) expand.1,9 With an increasing volume of shoulder arthroplasty procedures, the need for revision surgery has also increased. Revision shoulder arthroplasty presents unique technical challenges. First, bone quality is often impaired owing to osteoporosis or proximal stress shielding, which increases the risk of periprosthetic fracture.3,15 Second, humeral osteotomy is often required to remove a well-fixed humeral stem.15 In these cases, fixation is often accomplished with humeral shaft cerclage, with or without plate fixation.15 Periprosthetic fractures also present fixation challenges, often requiring cerclage for fixation in the zone of the prosthesis where screws cannot be placed. Cerclage fixation has most commonly been described with metal wires, metal cables, or polymer cables. However, such implants may have disadvantages such as metal prominence. Newer suture materials with higher tensile properties have been used in suture cerclage constructs in total hip arthroplasty.8 Suture cerclage, as described in hip arthroplasty, presents an alternative to wires or cables, but few studies have reported on its use in shoulder arthroplasty.2,10,12
The purpose of this case series was to evaluate the performance of suture cerclage fixation of the humeral shaft during shoulder arthroplasty. The hypothesis was that suture cerclage fixation would be safe and effective in stabilizing humeral osteotomies, fractures, and allografts.
Materials and methods
We performed a multicenter retrospective review of all shoulder arthroplasties involving cerclage fixation at 3 centers between 2012 and 2017. The inclusion criteria included a primary or revision shoulder arthroplasty with cerclage fixation of the humeral shaft for an intraoperative fracture, humeral osteotomy, or allograft fixation. There were no exclusion criteria. The mean follow-up period was 12.6 months (range, 0.5-40.9 months).
The surgical procedures were performed at 3 centers by 3 different fellowship-trained shoulder arthroplasty surgeons. Demographic data, indications, procedures performed, clinical outcomes, preoperative and postoperative American Shoulder and Elbow Surgeons (ASES) and Single Assessment Numeric Evaluation (SANE) scores, radiographic data, and complications were examined by chart review. Radiographs were reviewed for osteotomy or periprosthetic fracture healing (graded as yes or no). The fracture or osteotomy was considered healed if there was no evidence of a fracture line or humeral stem subsidence. Patients were also assessed for continued pain that would suggest nonunion of the osteotomy. Implant loosening was defined as subsidence or stem shift between the immediate postoperative and final follow-up radiographs, as described by Sperling et al.14
Cerclage technique
Suture-only cerclage was used in all cases requiring cerclage during the study period, with a nonabsorbable polyblend suture or 2-mm suture tape (No. 5 FiberWire or FiberTape; Arthrex, Naples, FL, USA). The suture was folded in half and passed around the humerus with a cerclage passer, avoiding the neurovascular structures (Fig. 1). The passer was passed from medial to lateral, remaining on bone, and the suture was passed lateral to medial. If cerclage was required at the level of the deltoid insertion or below, the radial nerve was exposed and protected. The suture knot was secured by a racking hitch knot, also known as a “cow hitch” knot, and backed up with ≥3 half-hitches7,11 (Fig. 2). Cerclage sutures were spaced approximately 1.5-2 cm apart, and 1-4 suture cerclages were used. In cases requiring bone graft, humeral or tibial allografts were cut and sized as needed. Cerclage sutures were initially placed around the humerus to stabilize the osteotomy. Then, suture cerclages were passed around the humerus–allograft construct.
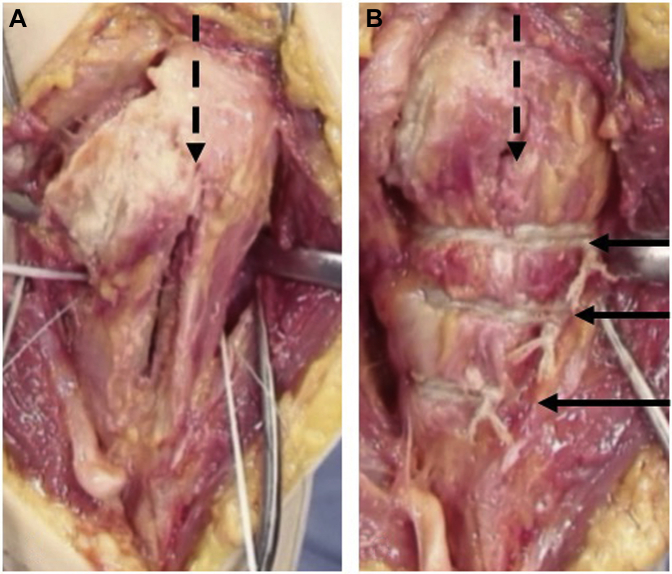
Figure 1.
Cadaveric demonstration of osteotomy and cerclage repair. (A) The osteotomy is visible with 1 cerclage suture passed around the shaft. (B) Three tied cerclage sutures and closure of osteotomy. The  show the osteotomy site, and the
show the osteotomy site, and the  show the 3 cables.
show the 3 cables.
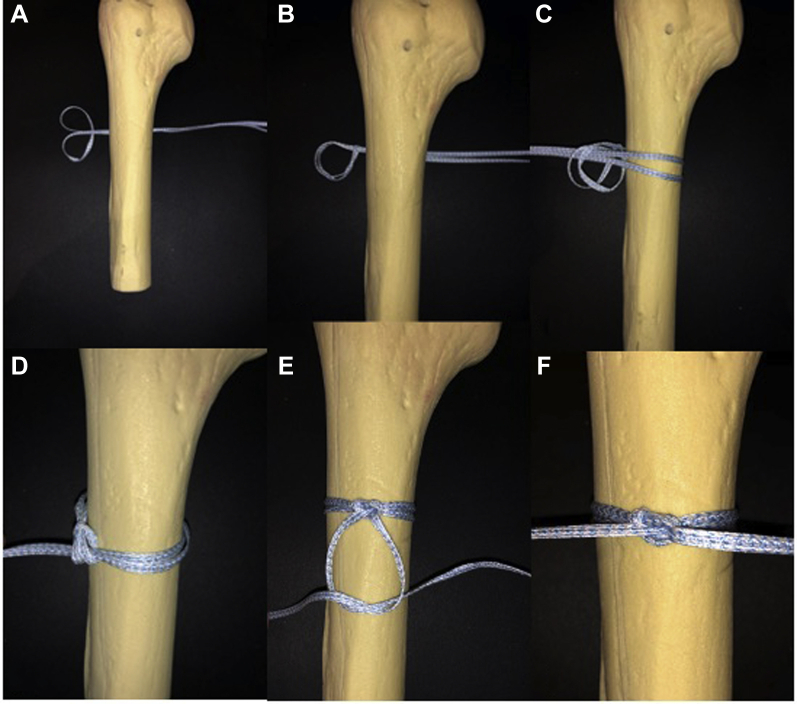
Figure 2.
Racking hitch knot. (A) The folded suture is placed around bone, and the looped end is folded back onto itself. (B) The loop is folded in on itself. (C) The free end of the suture is passed through the loop. (D) The suture is tightened by hand or a tensiometer. (E) The knot is backed up with 3 alternating half-hitches. (F) Final knot construct.
Postoperatively, patients were immobilized in a sling for 4-6 weeks. Passive range of motion was initiated at 4-6 weeks, and patients progressed to active range of motion at 8-12 weeks postoperatively based on pain and postoperative radiographs.
Statistical analysis
Descriptive statistics (mean and range) were used to describe the case series. Patient-reported outcomes (PROs) were described as mean, range, and standard deviation. Statistical significance was determined using the Student t test; the level of significance was defined as α = .05.
Results
This series included 27 cases: 3 primary and 24 revision cases. The average age was 69.5 years (range, 27-88 years). The average follow-up period was 12.6 months (range, 0.8-42.3 months). Of the patients, 16 (59%) were women and 11 (41%) were men. The indications for surgery included the following: failed anatomic total shoulder arthroplasty or hemiarthroplasty requiring osteotomy for stem removal (13), replantation after prosthetic joint infection (4), periprosthetic fracture (4), failed humeral component in RTSA (1), first-stage revision for prosthetic joint infection (1), primary RTSA for proximal humeral fracture requiring proximal humeral cerclage (3), and nonunion of periprosthetic fracture after revision RTSA (1). In 25 cases, an RTSA was implanted; in 1 case, an anatomic total shoulder; and in 1 case, an antibiotic cement spacer. Fifteen cases required osteotomy alone. One case required allograft alone. Six cases required both osteotomy and allograft. A mean of 1.8 cerclage sutures (range, 1-4 cerclage sutures) were used. The mean postoperative ASES and SANE scores were significantly improved (α = .05) compared with preoperative scores, from 21.4 to 44.5 (P = .002) and from 26.7 to 74.1 (P < .001), respectively (Table I).
Table I.
Patient-reported outcomes
| Measure | Preoperative | Postoperative | P value |
|---|---|---|---|
| ASES score | 21.42 (12.4) (2-27) | 44.46 (29.9) (0-65) | .002 |
| SANE score | 26.70 (19.9) (0-75) | 74.05 (28.2) (0-100) | <.001 |
Data are presented as mean (standard deviation) (range). The level of significance was defined as α = .05.
ASES, American Shoulder and Elbow Surgeons; SANE, Single Assessment Numeric Evaluation.
All cases are listed in Table II. All humeral shafts healed (Fig. 3). We noted 3 complications in this series: Two patients sustained postoperative prosthetic joint infections; one patient underwent successful 2-stage revision to RTSA, whereas the other patient was treated with component retention, débridement, and intravenous antibiotics. One patient sustained a ground-level fall that resulted in periprosthetic fracture, requiring revision RTSA. No complications related to the cerclage technique were observed.
Table II.
Suture cerclage cases
| No. | Age, yr | Sex | Indication | Procedure | Osteotomy | Allograft | Complications |
|---|---|---|---|---|---|---|---|
| 1 | 65 | F | RTSA PJI | Abx spacer | Y | N | No replantation because of ongoing knee infection |
| 2 | 64 | F | Resolution of PJI after hemiarthroplasty | RTSA | Y | N | None |
| 3 | 28 | F | Resolution of PJI after TSA | RTSA | Y | N | None |
| 4 | 74 | M | Resolution of PJI after TSA | RTSA | Y | N | None |
| 5 | 61 | F | Failed TSA | RTSA | Y | N | None |
| 6 | 56 | F | Failed hemiarthroplasty | TSA | Y | Y | None |
| 7 | 60 | M | Failed revision TSA | RTSA | Y | N | None |
| 8 | 72 | M | Failed hemiarthroplasty | RTSA | Y | Y | None |
| 9 | 83 | F | Failed hemiarthroplasty | RTSA | Y | Y | |
| 10 | 71 | F | Failed hemiarthroplasty | RTSA | Y | N | None |
| 11 | 64 | M | Periprosthetic Fx in RTSA | RTSA | Y | N | None |
| 12 | 80 | F | Failed TSA | RTSA | Y | Y | None |
| 13 | 73 | F | Failed hemiarthroplasty | RTSA | N | N | None |
| 14 | 65 | M | Failed TSA | RTSA | Y | N | Revision RTSA after GLF |
| 15 | 63 | M | Failed humeral component in RTSA | Revision humeral-side RTSA | Y | N | None |
| 16 | 65 | M | Failed TSA | RTSA | Y | N | PJI, treated with 2-stage revision RTSA |
| 17 | 67 | M | Resolution of PJI after hemiarthroplasty | RTSA | Y | N | None |
| 18 | 75 | F | Failed hemiarthroplasty | RTSA | Y | Y | None |
| 19 | 84 | F | Prox humeral Fx | RTSA | N | N | None |
| 20 | 85 | M | Periprosthetic Fx in RTSA | RTSA | Y | N | PJI, treated with I&D IV Abx |
| 21 | 85 | M | Prox humeral Fx-dislocation | RTSA | N | N | None |
| 22 | 88 | F | Periprosthetic Fx in RTSA | RTSA | N | N | None |
| 23 | 74 | F | Periprosthetic Fx in RTSA | RTSA | N | N | None |
| 24 | 60 | F | Failed TSA | RTSA | Y | N | None |
| 25 | 66 | F | Prox humeral Fx | RTSA | Y | N | None |
| 26 | 76 | M | Failed hemiarthroplasty | RTSA | Y | Y | None |
| 27 | 78 | F | Nonunion of Fx after revision RTSA for periprosthetic Fx | RTSA | N | Y | None |
F, female; RTSA, reverse total shoulder arthroplasty; PJI, prosthetic joint infection; Abx, antibiotics; Y, yes; N, no; TSA, total shoulder arthroplasty; GLF, ground-level fall; Prox, proximal; Fx, fracture; I&D, irrigation and débridement; IV, intravenous.
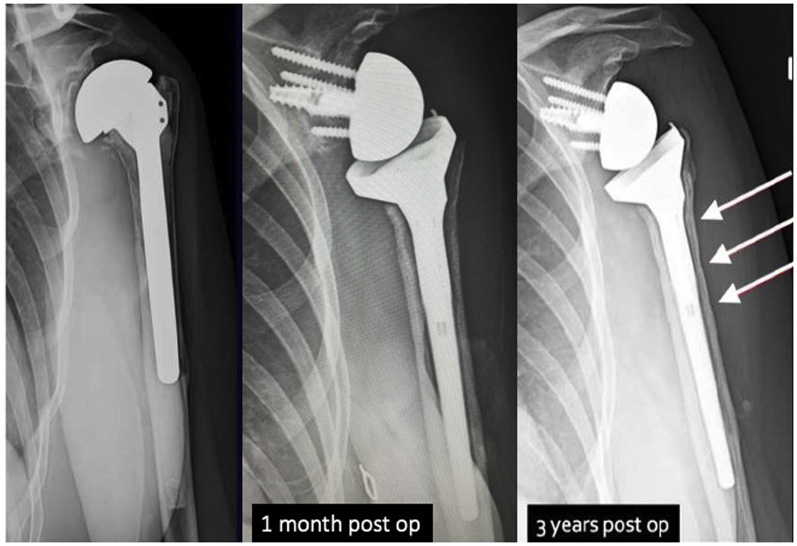
Figure 3.
Radiographs preoperatively and at 1 month and 3 years postoperatively (post op) in suture cerclage case 3. This case required revision of a cemented humeral stem with a loose glenoid. An indolent infection was diagnosed based on preoperative aspirate with positive culture results for Cutibacterium acnes. The patient underwent 2-stage reconstruction, with an extended humeral osteotomy and cement spacer for 6 weeks, followed by reverse shoulder implantation and 6 cerclage sutures. The indentations of the proximal 3 sutures in the cortex (arrow) should be noted. The osteotomy healed, and the patient had no pain and no evidence of subsidence at 3 years postoperatively.
Discussion
The findings of this case series confirm our hypothesis that suture cerclage fixation can be a safe and effective technique for the management of humeral shaft fixation for osteotomies and fractures, as well as allograft incorporation, during shoulder arthroplasty. All cases demonstrated radiographic healing, and no complications related to the cerclage fixation were observed. These findings may have implications for the management of humeral shaft fractures and osteotomies during shoulder arthroplasty.
The indications for shoulder arthroplasty, particularly revision, continue to increase. During revision, when an osteotomy is required or a periprosthetic fracture occurs, fixation may require a combination of plates, screws, and/or cerclages. Historically, metal cerclage cables have been used for stabilization of humeral osteotomies or periprosthetic fractures, adapted from their use in lower-extremity arthroplasty.2,10,12 Although a concern has been raised that cables decrease the periosteal blood supply and may increase rates of component loosening,12 laboratory studies have refuted the notion that the periosteal blood supply is significantly affected.19,20 Our findings provide further clinical evidence that cerclage fixation is safe because all fractures and osteotomies healed and no cases of stem loosening occurred. In addition, no patients required additional surgery for suture cerclage removal.
A variety of materials may be used for cerclage fixation. Traditionally, metal wires or cables have been used. However, these materials are radiopaque, creating challenges during radiographic evaluation of the bone. Moreover, metal wires and cables present a danger to the surgical team when sharp edges become exposed, increasing the risk of sharp injuries intraoperatively. In addition, metal cables can loosen, leading to soft tissue irritation or metallosis and necessitating removal.9
Kuruvalli et al8 used a “suture cord” made of 8 No. 2 Vicryl sutures (Ethicon, Edinburgh, UK) woven together to secure extended trochanteric osteotomies during hip revision surgery and reported healing in 19 of 20 patients. Technological advances have produced new suture materials that can be used for cerclage. Polymer cerclage cables have been shown to be safe and effective in the setting of revision shoulder arthroplasty and periprosthetic hip fractures in the lower extremity.5,16 Edwards et al5 presented a series of 11 patients undergoing shoulder arthroplasty requiring cerclage in whom polymer cables were used. Their results paralleled those of our study in that all osteotomies healed and no complications related to the use of cerclage were noted, despite a complication rate of 46% (5 of 11 patients) in their series. Laboratory testing has shown similar tensile and fatigue strength compared with metal cerclage.13
Westberg et al17 compared 3 sutures—No. 2 FiberWire, No. 2 Ultrabraid (Smith & Nephew, Andover, MA, USA), and No. 5 Ethibond (Johnson & Johnson, Somerville, NJ, USA)—using 3 knot configurations vs. 1.2-mm monofilament wire. Each sample was tested for cyclic loading and load to failure. Compared with monofilament wire, FiberWire and Ethibond failed at statistically significantly higher loads. Knot type did not affect the results. Renner et al11 compared 1.25-mm stainless steel wire (Synthes, Solothurn, Switzerland) and No. 5 FiberWire in a humeral osteotomy model. Comparative testing demonstrated higher compressive forces during tightening favoring stainless steel wire, with similar forces for distraction testing. There was no difference in force restraint on subsidence testing. FiberWire was secured for testing by a cow hitch knot, which is the same knot used in our study. Renner et al stated that nonmetallic cerclage may adapt better to the bone surface and reduce irritation related to crimp and metal debris.
Few studies have reported on cerclage fixation of the humeral shaft in the clinical setting of shoulder arthroplasty. To our knowledge, our study is the first to evaluate PROs in the setting of cerclage in shoulder arthroplasty. Our data showed statistically significant changes in ASES and SANE scores; both also represented minimal clinically important differences (MCIDs) in PROs as reported in the current MCID literature. The MCID for the ASES score ranges from 6.4-17 (MCID of 23 in our study), and the MCID for the SANE score after shoulder arthroplasty was most recently defined as 28.8 (MCID of 48 in our study),4,6,18 illustrating both statistical and, more important, clinical significance. PROs more likely reflect the outcome of the procedure and do not necessarily reflect the use of suture cerclage cables.
There are several limitations to this study. First, the number of patients is limited, and the series is retrospective in design. Second, the population is heterogeneous with multiple indications. Most important, no comparative group was included. However, we suggest that a comparison group was not required for this study. The intent was to establish suture cerclage as a safe alternative to other devices. In this study, no reoperations were performed and no failures were identified; therefore, any comparative group would be at best equal and possibly inferior if surgery was required for hardware pain or nonunion. It is not the intent of this study to suggest superiority to other fixation devices. We simply suggest this is a reasonable and safe alternative.
Conclusion
Suture cerclage fixation of the humeral shaft appears to be a safe method for fixation of a humeral periprosthetic fracture, osteotomy, or allograft fixation. This technique may be used as an alternative to metallic or polymer materials for cerclage fixation of the humerus during shoulder arthroplasty.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was received from Salus IRB prior to commencing the study (protocol no. ESL-002, Suture Cerclage of Fractures and Osteotomies of the Proximal Humerus—A Retrospective Medical Chart Review; August 9, 2018).
References
- 1.Abdel M.P., Hattrup S.J., Sperling J.W., Cofield R.H., Kreofsky C.R., Sanchez-Sotelo J. Revision of an unstable hemiarthroplasty or anatomical total shoulder replacement using a reverse design prosthesis. Bone Joint J. 2013;95-B:668–672. doi: 10.1302/0301-620X.95B5.30964. [DOI] [PubMed] [Google Scholar]
- 2.Angelini A., Battiato C. Past and present of the use of cerclage wires in orthopedics. Eur J Orthop Surg Traumatol. 2015;25:623–635. doi: 10.1007/s00590-014-1520-2. [DOI] [PubMed] [Google Scholar]
- 3.Boyd A.D., Thornhill T.S., Barnes C.L. Fractures adjacent to humeral prostheses. J Bone Joint Surg Am. 1992;74:1498–1504. [PubMed] [Google Scholar]
- 4.Copay A.G., Chung A.S., Eyberg B., Olmscheid N., Chutkan N., Spangehl M.J. Minimum clinically important difference: current trends in the orthopaedic literature, part I: upper extremity: a systematic review. JBJS Rev. 2018;6:e1. doi: 10.2106/JBJS.RVW.17.00159. [DOI] [PubMed] [Google Scholar]
- 5.Edwards T.B., Stuart K.D., Trappey G.J., O'Connor D.P., Sarin V.K. Utility of polymer cerclage cables in revision shoulder arthroplasty. Orthopedics. 2011;34 doi: 10.3928/01477447-20110228-13. [DOI] [PubMed] [Google Scholar]
- 6.Gowd A.K., Charles M.D., Liu J.N., Lalehzarian S.P., Cabarcas B.C., Manderle B.J. Single Assessment Numeric Evaluation (SANE) is a reliable metric to measure clinically significant improvements following shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28:2238–2246. doi: 10.1016/j.jse.2019.04.041. [DOI] [PubMed] [Google Scholar]
- 7.Kelly J.D., II, Vaishnav S., Saunders B.M., Schrumpf M.A. Optimization of the racking hitch knot: how many half hitches and which suture material provide the greatest security? Clin Orthop Relat Res. 2014;472:1930–1935. doi: 10.1007/s11999-014-3478-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuruvalli R.R., Landsmeer R., Debnath U.K., Suresh S.P., Thomas T.L. A new technique to reattach an extended trochanteric osteotomy in revision THA using suture cord. Clin Orthop Relat Res. 2008;466:1444–1448. doi: 10.1007/s11999-008-0233-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Merolla G., Wagner E., Sperling J.W., Paladini P., Fabbri E., Porcellini G. Revision of failed shoulder hemiarthroplasty to reverse total arthroplasty: analysis of 157 revision implants. J Shoulder Elbow Surg. 2018;27:75–81. doi: 10.1016/j.jse.2017.06.038. [DOI] [PubMed] [Google Scholar]
- 10.Perren S.M., Fernandez Dell'Oca A., Lenz M., Windolf M. Cerclage, evolution and potential of a Cinderella technology. An overview with reference to periprosthetic fractures. Acta Chir Orthop Traumatol Cech. 2011;78:190–199. [PubMed] [Google Scholar]
- 11.Renner N., Wieser K., Lajtai G., Morrey M.E., Meyer D.C. Stainless steel wire versus FiberWire suture cerclage fixation to stabilize the humerus in total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1568–1574. doi: 10.1016/j.jse.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 12.Ritter M.A., Lutgring J.D., Davis K.E., Berend M.E., Meding J.B. A clinical, radiographic, and cost comparison of cerclage techniques: wires vs cables. J Arthroplasty. 2006;21:1064–1067. doi: 10.1016/j.arth.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 13.Sarin V.K., Mattchen T.M., Pratt W.R., Hack B. Novel isoelastic cerclage cable for fracture (Abstract) Orthopaedic Proceedings. 2008;90B(Suppl 1):189. [Google Scholar]
- 14.Sperling J.W., Cofield R.H., O'Driscoll S.W., Torchia M.E., Rowland C.M. Radiographic assessment of ingrowth total shoulder arthroplasty. J Shoulder Elbow Surg. 2000;9:507–513. doi: 10.1067/mse.2000.109384. [DOI] [PubMed] [Google Scholar]
- 15.Steinmann S.P., Cheung E.V. Treatment of periprosthetic humerus fractures associated with shoulder arthroplasty. J Am Acad Orthop Surg. 2008;16:199–207. doi: 10.5435/00124635-200804000-00003. [DOI] [PubMed] [Google Scholar]
- 16.Ting N.T., Wera G.D., Levine B.R., Della Valle C.J. Early experience with a novel nonmetallic cable in reconstructive hip surgery. Clin Orthop Relat Res. 2010;468:2382–2386. doi: 10.1007/s11999-010-1284-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Westberg S.E., Acklin Y.P., Hoxha S., Ayranci C., Adeeb S., Bouliane M. Is suture comparable to wire for cerclage fixation? A biomechanical analysis. Shoulder Elbow. 2019;11:225–232. doi: 10.1177/1758573217735323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wickman J.R., Lau B.C., Scribani M.B., Wittstein J.R. Single Assessment Numeric Evaluation (SANE) correlates with American Shoulder and Elbow Surgeons score and Western Ontario Rotator Cuff index in patients undergoing arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2020;29:363–369. doi: 10.1016/j.jse.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 19.Wilson J.W. Effect of cerclage wires on periosteal bone in growing dogs. Vet Surg. 1987;16:299–302. doi: 10.1111/j.1532-950x.1987.tb00956.x. [DOI] [PubMed] [Google Scholar]
- 20.Wilson J.W., Rhinelander F.W., Stewart C.L. Microvascular and histologic effect of circumferential wire on appositional bone growth in immature dogs. J Orthop Res. 1985;3:412–417. doi: 10.1002/jor.1100030403. [DOI] [PubMed] [Google Scholar]