Acromioclavicular (AC) joint dislocation associated with a coracoid process fracture is an uncommon injury. It generally occurs in young male adults in the context of high-energy injuries such as traffic accidents, falls from height, or sports injuries. According to some authors,7,25 their mechanism of injury is comparable to that of AC joint dislocations, except that instead of a rupture of the coracoclavicular (CC) ligaments, the tensile forces transmitted by these ligaments cause a fracture in the coracoid process, allowing the vertical displacement of the clavicle.
The AC joint and its stabilizing ligaments are part of the superior shoulder suspensory complex (SSSC), a bone and ligament ring structure, described by Goss in 1993,8 whose integrity is essential to maintain the stability and biomechanics of the shoulder. According to this model,9 isolated SSSC lesions are relatively frequent and do not significantly alter the anatomic and functional stability of the ring. However, lesions that affect 2 or more points are much rarer (Fig. 1) and compromise the integrity of the ring, causing a potentially unstable situation that can lead to complications such as delayed union, loss of strength, and even degenerative arthritis.22 Therefore, although it is a controversial issue, some authors advocate for a surgical treatment of these lesions, whereas others prefer a conservative treatment. Besides, in cases where surgery is chosen, the suitability of fixing one or both injured points is controversial.
Figure 1.
Scheme representing the injury pattern of our cases: rupture of the superior shoulder suspensory complex in 2 points: AC dislocation and base of the coracoid fracture. AC, acromioclavicular.
Because of its oddity, the current literature on the subject is scarce and mainly comes from single case reports,14 being the reason why there are no standardized treatment strategies. We provide 2 cases that hold this combination of injuries treated by an open reduction and internal fixation of one point of the SSSC and the satisfying radiologic and functional results obtained. Understanding the complex anatomic relationships that coexist among these structures and its importance in the shoulder girdle biomechanics helps us make an optimal therapeutic decision.
Case 1
A 40-year-old man came to the emergency department because of pain and functional impairment in his left shoulder after falling while cycling. On examination, he had deformity and pain localized to the AC joint, with limitation for abduction and forward elevation of the shoulder above 90º, as well as pain with adduction. Shoulder radiographs showed a type III AC dislocation according to Rockwood classification. A computed tomographic scan was performed to rule out associated lesions, demonstrating the coexistence of a fracture of the base of the coracoid process (type I of Ogawa) (Fig. 2). The shoulder was immobilized in a sling at first and the patient was programmed for deferred surgical intervention. Under general anesthesia, in the beach chair position and using fluoroscopic control, an open reduction of the AC dislocation and fixation with a 6-hole and 18-mm clavicle hook plate and screws was performed through a distal clavicle approach.
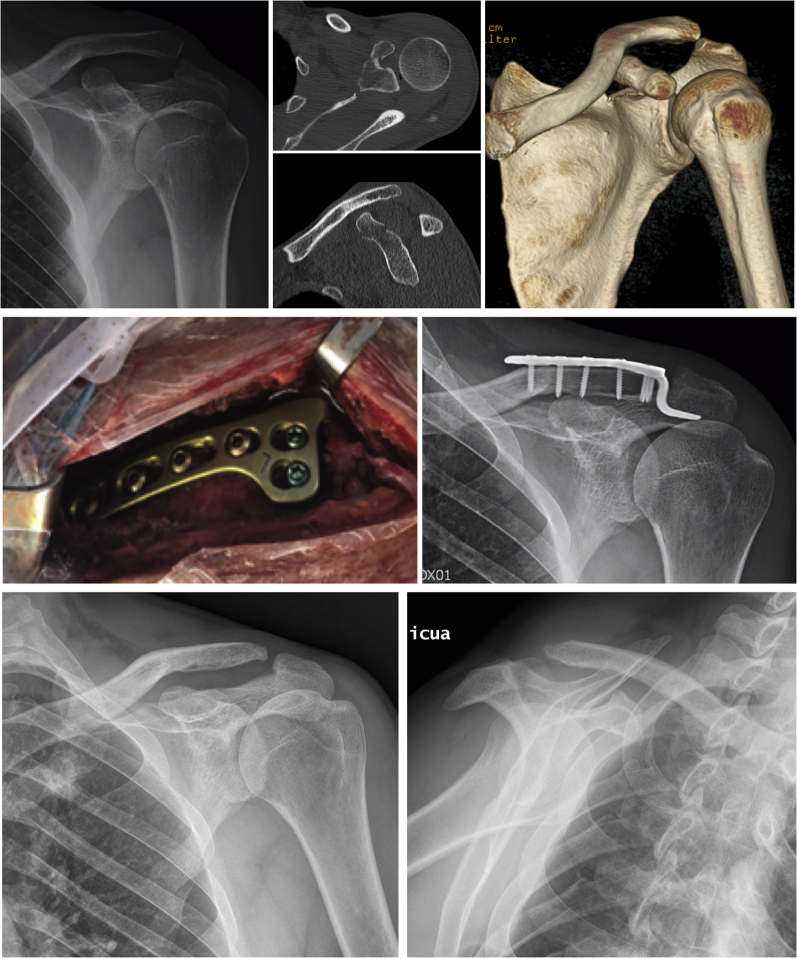
Figure 2.
Case 1: Shoulder AP radiograph, computed tomographic scan image, intraoperative view of a 6-hole clavicle hook plate, postoperative AP clavicle radiograph, and final result on an AP shoulder radiograph after removing the clavicle hook plate. AP, anteroposterior.
After AC reduction and fixation, an indirect reduction of the base of the coracoid process fracture was achieved, considering it unnecessary to perform any extra procedure on this fracture. The patient was immobilized in a sling in the immediate postoperative period. Two weeks after surgery, the patient began to perform passive exercises, and at 4 weeks active mobility in the supine position was permitted. At 3 months, signs of consolidation of the coracoid fracture in an anatomic position were observed. The clavicle hook plate was removed at 4 months. At 6 months, the patient had complete joint range of motion and had regained his previous activity level, with a Constant-Murley score of 97.5 and a Quick Disabilities of the Arm, Shoulder, and Hand questionnaire score of 0 (Table I).
Table I.
Characteristics of the cases presented
| Age, sex, and side | Mechanism | Rockwood AC joint dislocation classification | Ogawa coracoid fracture classification | AC joint dislocation treatment | Coracoid fracture treatment | CMS / DASH |
|
|---|---|---|---|---|---|---|---|
| Case 1 | 40, male, left | Bike fall while engaging in sport | III | I | ORIF with 3.5-mm LCP clavicle hook plate. A left, 6-hole, 18-mm hook and a right, 5-hole, 15-mm hook | Indirect reduction without fixation | 97.5 / 0 |
| Case 2 | 52, female, right | Fall while riding a bike | V | I | Indirect reduction without fixation | 93.5 / 2.3 |
AC, acromioclavicular; ORIF, open reduction and internal fixation; LCP, locking compression plate; CMS, Constant-Murley Score; DASH, Disabilities of the Arm, Shoulder, and Hand questionnaire.
Case 2
A 52-year-old woman who had a fall while riding a bicycle was diagnosed with a Rockwood type V AC dislocation and an Ogawa type I coracoid process fracture. Analogous to the former case, the AC dislocation was openly reduced and synthesized with a 5-hole, 15-mm clavicle hook plate, achieving an indirect reduction of the coracoid fracture that was left without additional fixation (Fig. 3). The postoperative course was similar to the patient in case 1, with full joint range of motion and activity level recovery before 7 months, with a Constant-Murley score of 93.5 and a Quick Disabilities of the Arm, Shoulder, and Hand questionnaire score of 2.3.
Figure 3.
Case 2: Shoulder AP preoperative radiograph, postoperative AP clavicle radiograph showing the fixation with a hook plate, and final result on an AP shoulder radiograph after removing the clavicle hook plate. AP, anteroposterior.
Discussion
The 2 cases we describe coincide with most available in the literature with regard to epidemiologic data, injury mechanism and classification, clinical symptoms, and diagnosis. In line with the literature, both cases occurred in the context of high-energy trauma: a fall from a bicycle. In addition, as reported in the first case, it is not uncommon for a fracture of the coracoid process to go unnoticed on a simple radiograph because of the overlap of bone structures2,15 and a high clinical suspicion is required. When a grade III AC dislocation is observed in simple radiography, it is important to determine if the CC space is altered,1 and if it is maintained, we should seek for an associated coracoid fracture. Even so, performing a computed tomographic scan may be necessary for a definitive diagnosis and assessment of associated lesions.
According to Ogawa et al,21 coracoid process fractures can be classified into 2 types with respect to their location in relation to the CC ligaments, with type I fractures being proximal to the insertion of CC ligaments and type II fractures, distal. Type I would be more unstable and require an open reduction and internal fixation; type II could be caused by contractions of the coracobrachialis muscle, the short head of the biceps, or the pectoralis minor and is usually managed conservatively. On the other hand, AC dislocations can be classified into 6 types following Rockwood classification26: type I and II are frequently treated conservatively; type III can be debatable; and type IV, V, and VI require surgical management. The association of AC dislocation and coracoid process fracture simulates a complete disruption of the AC and CC ligaments,13 which would bear resemblance to a type III AC injury or more.
With regard to the treatment, we must take into account that the SSSC is considered the most important element in the suspension function of the upper limb, as the AC joint together with the CC ligaments is responsible for transmitting the forces and weight of the upper limb across the clavicle and to the thorax. Also, both the AC joint and the CC ligaments direct the movement of the clavicle and scapula during shoulder motion and act as a fulcrum to lift the arm above the head.17,26 A good understanding of the biomechanics of the SSSC can help illustrate why a complete interruption of the AC joint associated with an injury at another point of the ring detaches the upper extremity from the axial skeleton.
Although good results have been described in this type of combined injuries with either conservative4,23,28 or surgical treatment, the complex SSSC anatomic and biomechanical relationships lead to consider the injuries occurring at 2 points of the ring as potentially unstable lesions, especially when they involve a large displacement. That is the reason why so many authors tend to opt for surgical stabilization. Some authors advocate for the fixation of a single point whereas others advise addressing both injured sites, performing a fixation of the coracoid fracture and the AC dislocation5,11,12,15,20 to achieve both horizontal and vertical stability.19 Among the authors who opt for the surgical fixation of a single point of the ring, the procedures described consist in fixation of the coracoid process with a screw,3,13 whereas others perform fixation of the AC dislocation using Kirschner wires2,14 or through a Dewar-Barrington procedure, only described by Ishizuki et al.10
In both of our cases, we decided to perform an open reduction and internal fixation of the AC dislocation using a rigid system such as the hook plate, thereby achieving an indirect reduction of the coracoid process fracture, leading to additional stabilization.24 By fixing one of the injuries, we managed to transform an unstable injury into a stable one. Besides, we consider that if when fixing one of the injuries we acquire an indirect reduction of the other, it becomes no longer necessary to perform any supplementary surgical procedure because the fracture will in all probably consolidate in the appropriate position. However, in cases where a reduction of the coracoid fracture is not achieved after reducing AC dislocation or in cases in which the fracture extends to the glenoid, it would be necessary to perform a reduction and added fixation of the coracoid fracture.
The benefits of deciding on this procedure are that, on the one hand, we manage to treat the 2 injuries simultaneously by acting directly on only one of them. On the other hand, with this method, we avoid approaching the coracoid fracture straight on, which becomes advantageous because the main neurovascular structures of the upper limb are very close to its medial area,18 and it is recommended to always perform the approaches lateral to the coracoid process. The potential disadvantages of using a clavicular hook plate are shoulder pain, osteolysis, and the need for a second surgery for implant removal.6,16 Some authors have described minimally invasive techniques for the placement of percutaneous screws as a method of fixation of the coracoid process3,13 that allow, as in our cases, to treat both lesions by fixing only one of them, as an add-on, avoiding the drawbacks of the open approach for coracoid fracture repair and those related to the use of a hook plate.
Although there are no established postoperative rehabilitation protocols, it is important to understand the type of fixation used. In our cases, the use of a rigid AC fixation as achieved with the hook plate gives us enough confidence to let the patient begin passive joint exercises after 2 weeks. However, it is important in these cases to limit the abduction and forward elevation to 90º, because of the increasing participation of the AC joint together with the clavicle and scapula in shoulder movement at this point.27 After 4 weeks, active exercises in supine position are allowed, in addition to periscapular muscle activation exercises. Exercises performed in a closed kinetic chain with support of the upper limb are more protective of the joint and activate the muscles to a lesser degree than those performed with the limb free.29
In conclusion, according to our review workup, these are the first cases report describing the combination of an AC joint dislocation associated with a coracoid process fracture that was treated by the mere fixation of the AC dislocation using a rigid system such as the hook plate. The radiologic and functional results achieved in our patients are very satisfactory and allowed early mobilization and rehabilitation. This, together with our understanding of the complex injuries that affect the SSSC and their consequences, leads us to consider it as an appropriate treatment option for these combined injuries.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgments
Informed written consent was obtained from the patients for publication. This study has been conducted according to the principles of the Declaration of Helsinki.
Footnotes
Institutional review board approval was not required for this case report
References
- 1.Bearden J.M., Hughston J.C., Whatley G.S. Acromioclavicular dislocation: method of treatment. J Sports Med. 1973;1:5–17. doi: 10.1177/036354657300100401. [DOI] [PubMed] [Google Scholar]
- 2.Bernard T.N., Jr., Brunet M.E., Haddad R.J., Jr. Fractured coracoid process in acromioclavicular dislocations. Report of four cases and review of the literature. Clin Orthop Relat Res. 1983:227–232. [PubMed] [Google Scholar]
- 3.Bhatia D.N. Orthogonal biplanar fluoroscopy-guided percutaneous fixation of a coracoid base fracture associated with acromioclavicular joint dislocation. Tech Hand Up Extrem Surg. 2012;16:56–59. doi: 10.1097/BTH.0b013e31823e2172. [DOI] [PubMed] [Google Scholar]
- 4.DiPaola M., Marchetto P. Coracoid process fracture with acromioclavicular joint separation in an American football player: a case report and literature review. Am J Orthop (Belle Mead NJ) 2009;38:37–39. [discussion 40] [PubMed] [Google Scholar]
- 5.Duan X., Zhang H., Zhang H., Wang Z. Treatment of coracoid process fractures associated with acromioclavicular dislocation using clavicular hook plate and coracoid screws. J Shoulder Elbow Surg. 2010;19:e22–e25. doi: 10.1016/j.jse.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 6.Eschler A., Gradl G., Gierer P., Mittlmeier T., Beck M. Hook plate fixation for acromioclavicular joint separations restores coracoclavicular distance more accurately than PDS augmentation, however presents with a high rate of acromial osteolysis. Arch Orthop Trauma Surg. 2012;132:33–39. doi: 10.1007/s00402-011-1399-x. [DOI] [PubMed] [Google Scholar]
- 7.Eyres K.S., Brooks A., Stanley D. Fractures of the coracoid process. J Bone Joint Surg Br. 1995;77:425–428. [PubMed] [Google Scholar]
- 8.Goss T.P. Double disruptions of the superior shoulder suspensory complex. J Orthop Trauma. 1993;7:99–106. doi: 10.1097/00005131-199304000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Goss T.P. Scapular fractures and dislocations: diagnosis and treatment. J Am Acad Orthop Surg. 1995;3:22–33. doi: 10.5435/00124635-199501000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Ishizuki M., Yamaura I., Isobe Y., Furuya K., Tanabe K., Nagatsuka Y. Avulsion fracture of the superior border of the scapula. Report of five cases. J Bone Joint Surg Am. 1981;63:820–822. [PubMed] [Google Scholar]
- 11.Jettoo P., de Kiewiet G., England S. Base of coracoid process fracture with acromioclavicular dislocation in a child. J Orthop Surg Res. 2010;5:77. doi: 10.1186/1749-799X-5-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kawasaki Y., Hirano T., Miyatake K., Fujii K., Takeda Y. Safety screw fixation technique in a case of coracoid base fracture with acromioclavicular dislocation and coracoid base cross-sectional size data from a computed axial tomography study. Arch Orthop Trauma Surg. 2014;134:913–918. doi: 10.1007/s00402-014-1995-7. [DOI] [PubMed] [Google Scholar]
- 13.Kim K.C., Rhee K.J., Shin H.D., Kim D.K., Shin H.S. Displaced fracture of the coracoid process associated with acromio-clavicular dislocation: a two-bird-one-stone solution. J Trauma. 2009;67:403–405. doi: 10.1097/TA.0b013e3181ac8ef1. [DOI] [PubMed] [Google Scholar]
- 14.Kose O., Canbora K., Guler F., Kilicaslan O.F., May H. Acromioclavicular dislocation associated with coracoid process fracture: report of two cases and review of the literature. Case Rep Orthop. 2015;2015:858969. doi: 10.1155/2015/858969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li J., Sun W., Li G.D., Li Q., Cai Z.D. Fracture of the coracoid process associated with acromioclavicular dislocation: a case report. Orthop Surg. 2010;2:165–167. doi: 10.1111/j.1757-7861.2010.00080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lopiz Y., Checa P., García-Fernández C., Valle J., Vega M.L., Marco F. Complications with the clavicle hook plate after fixation of Neer type II clavicle fractures. Int Orthop. 2019;43:1701–1708. doi: 10.1007/s00264-018-4108-3. [DOI] [PubMed] [Google Scholar]
- 17.Ludewing P.M., Phadke V., Braman J.P. Motion of the shoulder complex during multiplanar humeral elevation. J Bone Joint Surg Am. 2009;91:378–389. doi: 10.2106/JBJS.G.01483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matsen F.A., 3rd, Lippitt S.B., DeBartolo S.E. Saunders; Philadelphia, PA: 2004. Shoulder surgery: principles and procedures; p. 663. [Google Scholar]
- 19.Metwaly R.G., Edres K. Biplanar fixation of acromio-clavicular joint dislocation associated with coracoid process fracture: case report. Trauma Case Rep. 2018;15:4–7. doi: 10.1016/j.tcr.2018.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Naik M., Tripathy S.K., Goyal S., Rao S.K. Combined acromioclavicular joint dislocation and coracoid avulsion in an adult. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2014-208563. bcr2014208563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ogawa K., Yoshida A., Takahashi M., Ui M. Fractures of the coracoid process. J Bone Joint Surg Br. 1997;79:17–19. doi: 10.1302/0301-620x.79b1.6912. [DOI] [PubMed] [Google Scholar]
- 22.Oh W., Jeon I.H., Kyung S., Park C., Kim T., Ihn C. The treatment of double disruption of the superior shoulder suspensory complex. Int Orthop. 2002;26:145–149. doi: 10.1007/s00264-001-0325-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pedersen V., Prall W.C., Ockert B., Haasters F. Non-operative treatment of a fracture to the coracoid process with acromioclavicular dislocation in an adolescent. Orthop Rev (Pavia) 2014;6:5499. doi: 10.4081/or.2014.5499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Phadnis J., Bain G.I., Bak K. Pathoanatomy of Acromioclavicular Joint Instability. In: Bain G.I., Itoi E., Di Giacomo G., Sugaya H., editors. Normal and pathological anatomy of the shoulder. Springer; Berlin: 2015. [Google Scholar]
- 25.Protass J.J., Stampfli F.V., Osmer J.C. Coracoid process fracture diagnosis in acromioclavicular separation. Radiology. 1975;116:61–64. doi: 10.1148/116.1.61. [DOI] [PubMed] [Google Scholar]
- 26.Rockwood C.A. Injuries to the acromioclavicular joint. In: Saunders W., editor. Fractures in adults. 4th ed. Lippincott Williams & Wilkins; Philadelphia, PA: 1996. pp. 1341–1413. [Google Scholar]
- 27.Stucken C., Cohen S.B. Management of acromioclavicular joint injuries. Orthop Clin North Am. 2015;46:57–66. doi: 10.1016/j.ocl.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 28.Thomas K., Ng V.Y., Bishop J. Nonoperative management of a sagittal coracoid fracture with a concomitant acromioclavicular joint separation. Int J Shoulder Surg. 2010;4:44–47. doi: 10.4103/0973-6042.70823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wise M.B., Uhl T.L., Mattacola C.G., Nitz A.J., Kibler W.B. The effect of limb support on muscle activation during shoulder exercises. J Shoulder Elbow Surg. 2004;13:614–620. doi: 10.1016/S1058274604001375. [DOI] [PubMed] [Google Scholar]