Abstract
Background
Patient-reported outcome measures (PROMs) are increasingly being used in orthopedic surgery; however, there is significant variability and burden associated with their administration. The visual analog scale (VAS) may represent an efficient, single-question method to establish functional baselines in a domain-specific manner for glenohumeral arthritis.
Methods
Single-question VAS measures assessing function, strength, and pain as a percentage of normal were administered alongside legacy PROMs in patients with primary glenohumeral arthritis in a preoperative setting between October 2015 and March 2017. PROM performance was assessed using Spearman correlation coefficients. Both absolute and relative floor and ceiling effects were examined.
Results
A total of 70 patients (age 66.09 ± 9.84 years, body mass index 28.8 ± 9.77, 57.1% male, 54.2% right-sided) were included. The VAS Pain instrument (r = 0.45-0.64) outperformed the VAS Function (r = 0.23-0.62) and VAS Strength (r = 0.21-0.65) in correlation to preoperative PROMs. The performance of VAS Pain was comparable to American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES; r = 0.47-0.84). None of the VAS instruments in our study demonstrated preoperative floor effects (7.1%-8.6%) or ceiling effects (0.0%-4.3%). The most efficient instruments were Single-Assessment Numerical Evaluation (SANE; 0.87 ± 0.41 minutes), Patient-Reported Outcome Measurement Information System Upper Extremity Computer Adaptive Test (PROMIS UE CAT; 1.27 ± 1.30 minutes), and the triad of VAS measures (1.51 ± 1.61 minutes).
Conclusion
VAS Pain outperformed VAS Strength and Function relative to legacy PROMs, while performing comparable to ASES. None of the VAS measures were susceptible to significant floor or ceiling effects preoperatively. The VAS instruments along with SANE and PROMIS UE were the most time-efficient measures. VAS instruments may have a role in establishing preoperative baselines in those with glenohumeral arthritis in a simple, efficient, and adoptable manner.
Keywords: Visual analog scale, VAS, GHOA, glenohumeral osteoarthritis, sports medicine, outcome, patient-reported outcome measures, PROM
Value-based care initiatives have underlined the importance of promoting patient-centered care that emphasizes the quality of care delivered over volume.18,19 Patient-reported outcome measures (PROMs) have been particularly useful in quantifying patients' perceptions after surgical intervention based on specific health domains.19 The utility of PROMs cannot be underestimated, given broad applications from determining treatment efficacy to informing cost analyses.4,8,31,35, 36, 37,51 However, these instruments are not without important limitations, including financial and administrative burden3,17,37 and the need to validate performance (ie, correlations, floor and ceiling effects, and effect sizes) in a given population.9,44 Furthermore, various PROM designs are used for particular purposes, including mixed measures that combine patient and clinician input (ie, Constant-Murley score)40; health-related quality of life (HRQoL) measures to assess physical, mental, and social factors22,33; and disease-specific outcome measures assessing specific bodily regions or pathologies.46,47
When evaluating function and HRQoL in patients with glenohumeral osteoarthritis (GHOA), multiple PROMs have been validated for the purpose of establishing preoperative baselines and tracking longitudinal outcomes.27 Common function measures include the Western Ontario Osteoarthritis of the Shoulder index,30 American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES) score,25 the Single-Assessment Numerical Evaluation (SANE),24 and more recently, the Patient-Reported Outcome Measurement Information System (PROMIS) Upper Extremity (UE) and Physical Function instruments.14 Instruments used to evaluate HRQoL outcomes in those with GHOA include the the 12-Item Short Form Survey6 and EuroQol 5 Dimensions.6,14 The wide array of instruments available, each with its own unique psychometric properties, has created variability in the PROMs used to report outcomes after treatment for GHOA.32,48,49,59 Considered in the context of financial, administrative, and instrument-based limitations aforementioned, there is a specific need across orthopedic disciplines to adopt efficient, easily understandable instruments that display acceptable psychometric properties and may be administered in a variety of avenues (ie, paper, computer, cell phone messaging).10,42 Although the visual analog scale (VAS) is most commonly used to track pain,34,39 VAS measures represent single-question assessment tools that can assess specific outcome domains such as severity of disease symptoms,26 stress levels,16 and even HRQoL.54 However, limited research has examined the use of VAS measures in domains other than pain in orthopedic surgery.1,15,29
The purpose of this study is to define the preoperative performance of 3 VAS measures examining function, strength, and pain relative to legacy function PROMs in patients with GHOA. We hypothesize that (1) VAS Function and Strength measures will demonstrate greater correlative coefficients than VAS Pain with respect to legacy function PROMs; (2) VAS Function will have a comparable performance profile with respect to legacy PROM compared with ASES; (3) SANE will demonstrate the least average time to completion among PRO instruments, followed closely by the triad of VAS instruments; and (4) VAS instruments will demonstrate no significant absolute or relative floor or ceiling effects preoperatively.
Methods
Study design and cohort establishment
Our study case series was built using a prospectively maintained institutional registry (Outcome Based Electronic Research Database; Universal Research Solutions, Columbia, MO). Patient-reported outcome data was compiled between October 2015 and March 2017 using ICD-10 (International Classification of Diseases, Tenth Revision) codes signifying the diagnosis of primary GHOA (ie, M19.011, M19.012). Inclusion criteria included diagnosis of primary GHOA receiving total shoulder arthroplasty, full completion of preoperative PROMs, and no surgical history on the operative side. Exclusion criteria included those with surgical history on the operative shoulder or failure to complete any preoperative PROM (ie, <5% of patients failed to complete preoperative PROMs). Demographic variables collected comprised age, sex, and body mass index.
Patient-reported outcomes measures
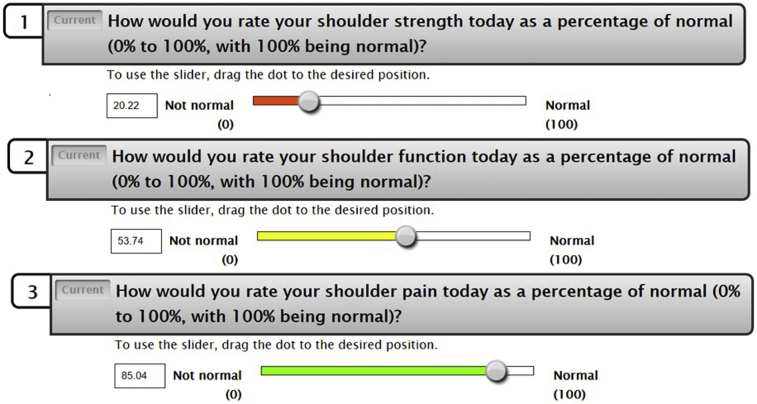
Legacy PROMs of interest examined in this study include the ASES score, Quick Disabilities of the Arm, Shoulder and Hand (qDASH) questionnaire, SANE, Constant-Murley score, and the PROMIS UE v2.0 Computer Adaptive Test. Three additional custom questionnaires were administered as single-question instruments, using an adapted version of the VAS in which different positions on the scale were color-coded to match the percentage of normal function, strength, and pain reported by patients (Fig. 1).
Figure 1.
Visual analog scale instruments for Strength, Function, and Pain. Pictured are examples of how each VAS instrument appears during computer adaptive testing, with a color scale correlating to the level of pain experienced helping the patient best estimate their strength, function, and pain, respectively. Each VAS instrument was completed in this order.
Statistical analysis
Statistical analysis consisted of 3 parts: time to completion, psychometrics, and floor and ceiling effects. Time-to-completion data were calculated using PROM start and completion time data recorded by our electronic registry. The PROMs were administered by trained research staff in the preoperative setting prior to surgery. Psychometric analysis used Spearman correlation coefficients to examine the strength of association between each individual VAS subscale and all legacy function PROMs included in this study. The performance of ASES relative to legacy function PROMs was also examined to provide a comparison point for each VAS instrument. Correlation coefficients were classified by the strength of association, with >0.8 equating to excellent, 0.71-0.8 equating to very good, 0.61-0.7 equating to good, 0.41-0.6 equating to fair, and 0.21-0.4 equating to poor.2,21 Absolute floor and ceiling effects were calculated by examining the percentage of respondents reporting achievement of the absolute lowest and highest scores. In the case that no one achieved absolute minimum or maximum score thresholds, relative floor and ceiling effects were calculated based on the minimum and maximum scores in the distribution. A percentage of ≥15% was designated as a significant floor or ceiling effect.2,14,45,50 A post hoc power analysis revealed a power of 0.74 assuming a medium effect size (0.3), a type I error rate of 5%, and a sample size of N=70 patients.
Results
A total of 70 patients (57.1% male, 54.2% right-handed) met criteria for appropriate inclusion in our study population. The average (±standard deviation) age in the study cohort was 66.09 ± 9.84 years, with average body mass index of 28.8 ± 9.77. Regarding time to completion, SANE demonstrated the shortest average completion time (0.87 ± 0.41 minutes), followed by the PROMIS UE CAT (1.27 ± 1.30 minutes) and the triad of custom VAS instruments (1.51 ± 1.61 minutes). The qDASH (2.82 ± 2.10 minutes) and Constant-Murley (3.55 ± 6.47 minutes) took the longest amount of time to complete, on average (Table I).
Table I.
Preoperative PRO scores and time to completion
| PRO score | Time to completion, min | |
|---|---|---|
| ASES | 41.11 ± 16.42 | 2.69 ± 4.62 |
| qDASH | 49.40 ± 19.90 | 2.82 ± 2.10 |
| SANE | 27.40 ± 20.69 | 0.87 ± 0.41 |
| Constant-Murley | 13.58 ± 5.56 | 3.55 ± 6.47 |
| PROMIS UE CAT | 30.02 ± 6.61 | 1.27 ± 1.30 |
| VAS Strength | 25.54 ± 20.65 | 1.51 ± 1.61 |
| VAS Function | 25.48 ± 20.46 | |
| VAS Pain | 36.95 ± 29.79 |
PRO, patient-reported outcome; ASES, American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form; qDASH, Quick Disabilities of the Arm, Shoulder and Hand questionnaire; SANE, Single-Assessment Numerical Evaluation; PROMIS UE CAT, Patient-Reported Outcome Measurement Information System Upper Extremity Computer Adaptive Test; VAS, visual analog scale.
With respect to performance, both VAS Function (r = 0.23-0.62) and VAS Strength (r = 0.21-0.65) demonstrated poor to fair strengths of correlation with respect to legacy PROMs. The VAS Pain measure outperformed VAS Function and Strength by exhibiting fair to good correlations (r = 0.45-0.64). ASES demonstrated correlation coefficients ranging from fair to excellent in strength relative to legacies (r = 0.47-0.84). With respect to ASES, VAS Pain exhibited the strongest correlation coefficient (r = 0.60), whereas the weakest correlation coefficient was exhibited by VAS Strength (r = 0.21) (Table II). With respect to floor and ceiling effects, none of the VAS instruments demonstrated preoperative floor effects (7.1%-8.6%) or ceiling effects (0.0%-4.3%). The SANE instrument trended toward a preoperative relative floor effect (n=8, 11.4%) (Table III).
Table II.
Performance of the custom VAS Function relative to legacy instruments
| VAS Function | VAS Strength | VAS Pain | ASES | |
|---|---|---|---|---|
| VAS Function | ||||
| VAS Strength | 0.71 | |||
| VAS Pain | 0.41 | 0.42 | ||
| ASES | 0.42 | 0.21 | 0.60 | |
| qDASH | –0.50 | –0.34 | –0.64 | –0.84 |
| SANE | 0.62 | 0.65 | 0.58 | 0.47 |
| Constant-Murley | 0.25 | 0.26 | 0.45 | 0.69 |
| PROMIS UE | 0.23 | 0.38 | 0.48 | 0.56 |
VAS, visual analog scale; ASES, American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form; qDASH, Quick Disabilities of the Arm, Shoulder and Hand questionnaire; SANE, Single-Assessment Numerical Evaluation; PROMIS UE, Patient-Reported Outcome Measurement Information System Upper Extremity.
Table III.
Absolute and relative ceiling and floor effects
| PROM | Floor, n (%) | Ceiling, n (%) |
|---|---|---|
| VAS Function | 5 (7.1) | 0 (0.0) |
| VAS Strength | 6 (8.6) | 0 (0.0) |
| VAS Pain | 5 (7.1) | 3 (4.3) |
| PROMIS UE CAT | 1 (1.4) | 1 (1.4) |
| ASES | 2 (2.8) | 1 (1.4) |
| SANE | 8 (11.4) | 1 (1.4) |
| Constant-Murley | 4 (5.7) | 1 (1.4) |
| qDASH | 1 (1.4) | 1 (1.4) |
PROM, patient-reported outcome measure; VAS, visual analog scale; PROMIS UE CAT, Patient-Reported Outcome Measurement Information System Upper Extremity Computer Adaptive Test; ASES, American Shoulder and Elbow Surgeons score; SANE, Single-Assessment Numerical Evaluation; qDASH, Quick Disabilities of the Arm, Shoulder and Hand.
Italicized values represent relative ceiling effects in the scenario that absolute minimum or maximum values were not reported in the study population.
Discussion
The most important finding from this study is that the VAS Pain PROM outperformed VAS Strength and VAS Function in relation to legacy PROMs in patients receiving total shoulder arthroplasty with primary GHOA. However, considering that correlations between VAS and legacy PROMs ranged from fair to excellent, the following conclusions must be interpreted cautiously. The SANE, PROMIS UE CAT, and VAS instruments were the most efficient with respect to time to completion, and no PROM in the study demonstrated absolute or relative floor or ceiling effects. These results suggest that the VAS Pain PROM may be used to establish preoperative pain baselines in patients with primary GHOA.
Numerous PROMs have been validated in patients with primary GHOA, including ASES, SANE, the Constant-Murley score, and the Western Ontario Osteoarthritis of the Shoulder index.44 However, as new PROMs continue to be developed (eg, PROMIS), it is increasingly important to administer simple, efficient instruments that are also appropriately discriminative of outcomes.37 VAS instruments are the existing gold standard in the evaluation of pain,7,23,28,38,58 and instrument-based advantages in efficiency and simplicity have led researchers to examine VAS instruments in functional disability,1 hand function and grip,15,29 and general health status and monitoring of symptoms.13,26 The current study suggests that in those with GHOA, the VAS Pain measure outperforms the VAS Function and VAS Strength measures relative to legacy instruments. Furthermore, by using all 3 instruments, function-based outcomes can also be reported in a domain-specific manner noting the relative improvements of pain interference, strength improvement, and general functional changes to overall improvement.11,12,37,55
In a fashion similar to the development of new PROMs, the administration of PROMs is undergoing rapid evolution as outcomes initiatives are increasingly being implemented at orthopedic care centers.41,43,57 Previous literature has suggested that theoretically the optimal PROM is one single domain-specific question, with appropriate outcome discrimination, and without significant floor or ceiling effects.5 Question burden is an important consideration given previous work demonstrating significant impact on follow-up rates, as well as the speed and accuracy with which patients complete instruments.5,20,53 The time-to-completion data from the current study demonstrates that SANE, the PROMIS UE CAT, and triad of VAS measures are the quickest to complete, with Constant-Murley, qDASH, and ASES each requiring an average time to completion exceeding 2 minutes 30 seconds. Thus, the VAS measures used in this study represent an important example in which the SANE score can be administered and reported in a domain-specific manner without significantly increasing the time (ie, <45 seconds) or questions (ie, 2 additional).
With respect to the floor and ceiling effect analysis, the VAS instruments used in this study were not found to demonstrate any relative or absolute floor or ceiling effects. However, the current study was limited specifically to preoperative data, and it remains uncertain if any floor or ceiling effects would occur postoperatively in this patient population. With respect to legacy PROMs, previous research has demonstrated that the GHOA population is not particularly susceptible to floor and ceiling effects.27,52 Nonetheless, SANE scores trended toward a relative floor effect (11.8%), with previous research demonstrating a significant ceiling effect postoperatively in those with GHOA.46,56 Our work aligns well with that of Dowdle et al14 in that legacy instruments and the PROMIS PF CAT were devoid of floor and ceiling effects in those with primary GHOA.
Limitations
Our study is not without important limitations, which all readers should consider. First, we are unable to assess the effect of questionnaire fatigue on patient response speeds and response rates. Based on the electronic registry used in this study, participants answered standardized, predetermined sets of questionnaires in a nonrandomized fashion. That is, every person initiated the questionnaire set with the ASES and VAS questionnaires and ended with 12-item Short Form Survey and the Veterans RAND 12-Item Health Survey instruments. Theoretically, this may have led to “hasty completion,” which has previously been linked to a predisposition toward floor effects on the PROMIS Depression CAT.20 Additionally, generalizability of our study results is most applicable to other patient populations receiving total shoulder arthroplasty with primary GHOA. Lastly, because ICD-10 codes were used, there may be a degree of diagnostic variability with respect to the population of patients included. Two ICD-10 codes were used—M19.011 and M19.012—but confounding by other conditions (ie, acromioclavicular joint arthritis) must be considered.
Conclusion
VAS Pain outperformed VAS Strength and Function relative to legacy PROMs, while performing comparable to ASES. None of the VAS measures were susceptible to significant floor or ceiling effects preoperatively. The VAS instruments along with SANE and PROMIS UE were the most time-efficient measures. VAS instruments may have a role in establishing preoperative baselines in those with glenohumeral arthritis in a simple, efficient, and adoptable manner.
Disclaimer
Jorge Chahla reports other relationship: unpaid consultant for Arthrex, Inc., CONMED Linvatec, and Smith & Nephew.
Brian Forsythe reports personal fees from Elsevier, Arthrex, Inc., Jace Medical, and Stryker and grants from Smith & Nephew and Ossur, outside the submitted work.
Brian Cole reports other from Aesculap/B.Braun, American Journal of Orthopaedics, and American Journal of Sports Medicine; grants, personal fees, nonfinancial support, and other from Arthrex, Inc.; other from Arthroscopy Association of North America, Athletico, Cartilage, Elsevier Publishing, International Cartilage Repair Society, Journal of Shoulder and Elbow Surgery, Journal of the American Academy of Orthopaedic Surgeons, JRF Ortho, National Institutes of Health (NIAMS & NICHD), Operative Techniques in Sports Medicine, and Ossio; personal fees and other from Regentis; other from Smith & Nephew; and personal fees and other from Zimmer, outside the submitted work.
Nikhil Verma reports personal fees and nonfinancial support from Arthrex, Inc.; nonfinancial support and other from Arthroscopy; personal fees from DJ Orthopaedics and Orthospace; and nonfinancial support and other from Vindico Medical-Orthopedics Hyperguide, outside the submitted work; in addition, Dr. Verma has a patent Smith & Nephew–Instrumentation with royalties paid to Smith & Nephew; and American Orthopaedic Society for Sports Medicine, American Shoulder and Elbow Surgeons, and Arthroscopy Association of North America: board or committee member; Cymedica: stock or stock options; Journal of Knee Surgery: editorial or governing board; Minivasive: paid consultant, stock or stock options; Omeros: stock or stock options; and SLACK Incorporated: editorial or governing board.
The other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
Institutional review board approval was received from Rush University Medical Center (no. 19022301).
References
- 1.Anagnostis C., Mayer T.G., Gatchel R.J., Proctor T.J. The million visual analog scale: its utility for predicting tertiary rehabilitation outcomes. Spine (Phila Pa 1976) 2003;28:1051–1060. doi: 10.1097/01.BRS.0000061989.94487. 9B. [DOI] [PubMed] [Google Scholar]
- 2.Anthony C.A., Glass N.A., Hancock K., Bollier M., Wolf B.R., Hettrich C.M. Performance of PROMIS instruments in patients with shoulder instability. Am J Sports Med. 2017;45:449–453. doi: 10.1177/0363546516668304. [DOI] [PubMed] [Google Scholar]
- 3.Ayers D.C., Zheng H., Franklin P.D. Integrating patient-reported outcomes into orthopaedic clinical practice: proof of concept from FORCE-TJR. Clin Orthop Relat Res. 2013;471:3419–3425. doi: 10.1007/s11999-013-3143-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baumhauer J.F., Bozic K.J. Value-based healthcare: patient-reported outcomes in clinical decision making. Clin Orthop Relat Res. 2016;474:1375–1378. doi: 10.1007/s11999-016-4813-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beach W.R. Editorial commentary: Patient Reported Outcomes Measurement Information System (PROMIS) may be our promise for the future. Arthroscopy. 2017;33:1775–1776. doi: 10.1016/j.arthro.2017.07.015. [DOI] [PubMed] [Google Scholar]
- 6.Brownson P., Donaldson O., Fox M., Rees J.L., Rangan A., Jaggi A. BESS/BOA patient care pathways: traumatic anterior shoulder instability. Shoulder Elbow. 2015;7:214–226. doi: 10.1177/1758573215585656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cancienne J., Kunze K.N., Beck E.C., Chahla J., Suppauksorn S., Nho S.J. Influence of cigarette smoking at the time of surgery on postoperative outcomes in patients with femoroacetabular impingement: a matched-pair cohort analysis. Am J Sports Med. 2019;47:1138–1144. doi: 10.1177/0363546519832545. [DOI] [PubMed] [Google Scholar]
- 8.Carr A.J. Evidence-based orthopaedic surgery: what type of research will best improve clinical practice? J Bone Joint Surg Br. 2005;87:1593–1594. doi: 10.1302/0301-620X.87B12.17085. [DOI] [PubMed] [Google Scholar]
- 9.Chen R.E., Papuga M.O., Nicandri G.T., Miller R.J., Voloshin I. Preoperative Patient-Reported Outcomes Measurement Information System (PROMIS) scores predict postoperative outcome in total shoulder arthroplasty patients. J Shoulder Elbow Surg. 2019;28:547–554. doi: 10.1016/j.jse.2018.08.040. [DOI] [PubMed] [Google Scholar]
- 10.Christie A., Dagfinrud H., Dale O., Schulz T., Hagen K.B. Collection of patient-reported outcomes;--text messages on mobile phones provide valid scores and high response rates. BMC Med Res Methodol. 2014;14:52. doi: 10.1186/1471-2288-14-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deshpande P.R., Rajan S., Sudeepthi B.L., Abdul Nazir C.P. Patient-reported outcomes: a new era in clinical research. Perspect Clin Res. 2011;2:137–144. doi: 10.4103/2229-3485.86879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.DeVine J., Norvell D.C., Ecker E., Fourney D.R., Vaccaro A., Wang J. Evaluating the correlation and responsiveness of patient-reported pain with function and quality-of-life outcomes after spine surgery. Spine (Phila Pa 1976) 2011;36:S69–S74. doi: 10.1097/BRS.0b013e31822ef6de. [DOI] [PubMed] [Google Scholar]
- 13.Di Martino A., Tentoni F., Di Matteo B., Cavicchioli A., Lo Presti M., Filardo G. Early viscosupplementation after anterior cruciate ligament reconstruction: a randomized controlled trial. Am J Sports Med. 2016;44:2572–2578. doi: 10.1177/0363546516654909. [DOI] [PubMed] [Google Scholar]
- 14.Dowdle S.B., Glass N., Anthony C.A., Hettrich C.M. Use of PROMIS for patients undergoing primary total shoulder arthroplasty. Orthop J Sports Med. 2017;5 doi: 10.1177/2325967117726044. 2325967117726044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Downie W.W., Leatham P.A., Rhind V.M., Pickup M.E., Wright V. The visual analogue scale in the assessment of grip strength. Ann Rheum Dis. 1978;37:382–384. doi: 10.1136/ard.37.4.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dutheil F., Pereira B., Moustafa F., Naughton G., Lesage F.X., Lambert C. At-risk and intervention thresholds of occupational stress using a visual analogue scale. PLoS One. 2017;12:e0178948. doi: 10.1371/journal.pone.0178948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fung C.H., Hays R.D. Prospects and challenges in using patient-reported outcomes in clinical practice. Qual Life Res. 2008;17:1297–1302. doi: 10.1007/s11136-008-9379-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldman A.H., Kates S. Pay-for-performance in orthopedics: how we got here and where we are going. Curr Rev Musculoskelet Med. 2017;10:212–217. doi: 10.1007/s12178-017-9404-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MOTION Group Patient-reported outcomes in orthopaedics. J Bone Joint Surg. 2018;100:436–442. doi: 10.2106/JBJS.17.00608. [DOI] [PubMed] [Google Scholar]
- 20.Guattery J.M., Dardas A.Z., Kelly M., Chamberlain A., McAndrew C., Calfee R.P. Floor effect of PROMIS depression CAT associated with hasty completion in orthopaedic surgery patients. Clin Orthop Relat Res. 2018;476:696–703. doi: 10.1007/s11999.0000000000000076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hancock K.J., Glass N., Anthony C.A., Hettrich C.M., Albright J., Amendola A. Performance of PROMIS for healthy patients undergoing meniscal surgery. J Bone Joint Surg Am. 2017;99:954–958. doi: 10.2106/JBJS.16.00848. [DOI] [PubMed] [Google Scholar]
- 22.Jackowski D., Guyatt G. A guide to health measurement. Clin Orthop Relat Res. 2003;413:80–89. doi: 10.1097/01.blo.0000079771.06654.13. [DOI] [PubMed] [Google Scholar]
- 23.Karaaslan F., Karaoglu S., Yurdakul E. Reducing intra-articular hemarthrosis after arthroscopic anterior cruciate ligament reconstruction by the administration of intravenous tranexamic acid: a prospective, randomized controlled trial. Am J Sports Med. 2015;43:2720–2726. doi: 10.1177/0363546515599629. [DOI] [PubMed] [Google Scholar]
- 24.Kerr B.J., McCarty E.C. Outcome of arthroscopic debridement is worse for patients with glenohumeral arthritis of both sides of the joint. Clin Orthop Relat Res. 2008;466:634–638. doi: 10.1007/s11999-007-0088-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kirkley A., Griffin S., Dainty K. Scoring systems for the functional assessment of the shoulder. Arthroscopy. 2003;19:1109–1120. doi: 10.1016/j.arthro.2003.10.030. [DOI] [PubMed] [Google Scholar]
- 26.Klimek L., Bergmann K.C., Biedermann T., Bousquet J., Hellings P., Jung K. Visual analogue scales (VAS): Measuring instruments for the documentation of symptoms and therapy monitoring in cases of allergic rhinitis in everyday health care: Position Paper of the German Society of Allergology (AeDA) and the German Society of Allergy and Clinical Immunology (DGAKI), ENT Section, in collaboration with the working group on Clinical Immunology, Allergology and Environmental Medicine of the German Society of Otorhinolaryngology, Head and Neck Surgery (DGHNOKHC) Allergo J Int. 2017;26:16–24. doi: 10.1007/s40629-016-0006-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kocher M.S., Horan M.P., Briggs K.K., Richardson T.R., O'Holleran J., Hawkins R.J. Reliability, validity, and responsiveness of the American Shoulder and Elbow Surgeons subjective shoulder scale in patients with shoulder instability, rotator cuff disease, and glenohumeral arthritis. J Bone Joint Surg Am. 2005;87:2006–2011. doi: 10.2106/JBJS.C.01624. [DOI] [PubMed] [Google Scholar]
- 28.Krishnamoorthy V.P., Kunze K.N., Beck E.C., Cancienne J.M., O'Keefe L.S., Ayeni O.R. Radiographic prevalence of symphysis pubis abnormalities and clinical outcomes in patients with femoroacetabular impingement syndrome. Am J Sports Med. 2019;47:1467–1472. doi: 10.1177/0363546519837203. [DOI] [PubMed] [Google Scholar]
- 29.Limaye V., Frankham A., Disney A., Pile K. Evaluation of hand function in patients undergoing long term haemodialysis. Ann Rheum Dis. 2001;60:278–280. doi: 10.1136/ard.60.3.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lo I.K., Griffin S., Kirkley A. The development of a disease-specific quality of life measurement tool for osteoarthritis of the shoulder: the Western Ontario Osteoarthritis of the Shoulder (WOOS) index. Osteoarthritis Cartilage. 2001;9:771–778. doi: 10.1053/joca.2001.0474. [DOI] [PubMed] [Google Scholar]
- 31.Makhni E.C., Swart E., Steinhaus M.E., Mather R.C., 3rd, Levine W.N., Bach B.R., Jr Cost-effectiveness of reverse total shoulder arthroplasty versus arthroscopic rotator cuff repair for symptomatic large and massive rotator cuff tears. Arthroscopy. 2016;32:1771–1780. doi: 10.1016/j.arthro.2016.01.063. [DOI] [PubMed] [Google Scholar]
- 32.Mitchell J.J., Horan M.P., Greenspoon J.A., Menge T.J., Tahal D.S., Millett P.J. Survivorship and patient-reported outcomes after comprehensive arthroscopic management of glenohumeral osteoarthritis: minimum 5-year follow-up. Am J Sports Med. 2016;44:3206–3213. doi: 10.1177/0363546516656372. [DOI] [PubMed] [Google Scholar]
- 33.Muragundi P., Tumkur A., Shetty R., Naik A. Health-related quality of life measurement. J Young Pharm. 2012;4:54. doi: 10.4103/0975-1483.93568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Namdari S., Nicholson T., Abboud J., Lazarus M., Steinberg D., Williams G. Randomized controlled trial of interscalene block compared with injectable liposomal bupivacaine in shoulder arthroplasty. J Bone Joint Surg Am. 2017;99:550–556. doi: 10.2106/JBJS.16.00296. [DOI] [PubMed] [Google Scholar]
- 35.Nwachukwu B.U., Chang B., Adjei J., Schairer W.W., Ranawat A.S., Kelly B.T. Time required to achieve minimal clinically important difference and substantial clinical benefit after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2018;46:2601–2606. doi: 10.1177/0363546518786480. [DOI] [PubMed] [Google Scholar]
- 36.Nwachukwu B.U., Chang B., Voleti P.B., Berkanish P., Cohn M.R., Altchek D.W. Preoperative short form health survey score is predictive of return to play and minimal clinically important difference at a minimum 2-year follow-up after anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:2784–2790. doi: 10.1177/0363546517714472. [DOI] [PubMed] [Google Scholar]
- 37.Nwachukwu B.U., Hamid K.S., Bozic K.J. Measuring value in orthopaedic surgery. JBJS Rev. 2013;1 doi: 10.2106/JBJS.RVW.M.00067. [DOI] [PubMed] [Google Scholar]
- 38.Oka K., Tanaka H., Okada K., Sahara W., Myoui A., Yamada T. Three-dimensional corrective osteotomy for malunited fractures of the upper extremity using patient-matched instruments: a prospective, multicenter, open-label, single-arm trial. J Bone Joint Surg Am. 2019;101:710–721. doi: 10.2106/JBJS.18.00765. [DOI] [PubMed] [Google Scholar]
- 39.Okoroha K.R., Lynch J.R., Keller R.A., Korona J., Amato C., Rill B. Liposomal bupivacaine versus interscalene nerve block for pain control after shoulder arthroplasty: a prospective randomized trial. J Shoulder Elbow Surg. 2016;25:1742–1748. doi: 10.1016/j.jse.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 40.Poolman R.W., Swiontkowski M.F., Fairbank J.C., Schemitsch E.H., Sprague S., de Vet H.C. Outcome instruments: rationale for their use. J Bone Joint Surg Am. 2009;91(Suppl 3):41–49. doi: 10.2106/JBJS.H.01551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pulido P.A., Hardwick M.E., Sandwell J.C., Colwell C.W., Jr. Developing and implementing an orthopaedic outcomes program: a step-by-step guide. Orthop Nurs. 2008;27:94–100. doi: 10.1097/01.NOR.0000315621.21267.a6. quiz 101-102. [DOI] [PubMed] [Google Scholar]
- 42.Roberts N., Bradley B., Williams D. Use of SMS and tablet computer improves the electronic collection of elective orthopaedic patient reported outcome measures. Ann R Coll Surg Engl. 2014;96:348–351. doi: 10.1308/003588414X13946184900769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rothrock N.E., Bass M., Blumenthal A., Gershon R.C., Hanson B., Joeris A. AO patient outcomes center: design, implementation, and evaluation of a software application for the collection of patient-reported outcome measures in orthopedic outpatient clinics. JMIR Form Res. 2019;3:e10880. doi: 10.2196/10880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sciascia A.D., Morris B.J., Jacobs C.A., Edwards T.B. Responsiveness and internal validity of common patient-reported outcome measures following total shoulder arthroplasty. Orthopedics. 2017;40:e513–e519. doi: 10.3928/01477447-20170327-02. [DOI] [PubMed] [Google Scholar]
- 45.Selim A.J., Rogers W., Qian S.X., Brazier J., Kazis L.E. A preference-based measure of health: the VR-6D derived from the Veterans RAND 12-Item Health Survey. Qual Life Res. 2011;20:1337–1347. doi: 10.1007/s11136-011-9866-y. [DOI] [PubMed] [Google Scholar]
- 46.Smith M.V., Calfee R.P., Baumgarten K.M., Brophy R.H., Wright R.W. Upper extremity-specific measures of disability and outcomes in orthopaedic surgery. J Bone Joint Surg Am. 2012;94:277–285. doi: 10.2106/JBJS.J.01744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smith M.V., Klein S.E., Clohisy J.C., Baca G.R., Brophy R.H., Wright R.W. Lower extremity-specific measures of disability and outcomes in orthopaedic surgery. J Bone Joint Surg Am. 2012;94:468–477. doi: 10.2106/JBJS.J.01822. [DOI] [PubMed] [Google Scholar]
- 48.Somerson J.S., Neradilek M.B., Service B.C., Hsu J.E., Russ S.M., Matsen F.A., 3rd Clinical and radiographic outcomes of the ream-and-run procedure for primary glenohumeral arthritis. J Bone Joint Surg Am. 2017;99:1291–1304. doi: 10.2106/JBJS.16.01201. [DOI] [PubMed] [Google Scholar]
- 49.Steen B.M., Cabezas A.F., Santoni B.G., Hussey M.M., Cusick M.C., Kumar A.G. Outcome and value of reverse shoulder arthroplasty for treatment of glenohumeral osteoarthritis: a matched cohort. J Shoulder Elbow Surg. 2015;24:1433–1441. doi: 10.1016/j.jse.2015.01.005. [DOI] [PubMed] [Google Scholar]
- 50.Terwee C.B., Bot S.D., de Boer M.R., van der Windt D.A., Knol D.L., Dekker J. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60:34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 51.Teusink M.J., Virani N.A., Polikandriotis J.A., Frankle M.A. Cost analysis in shoulder arthroplasty surgery. Adv Orthop. 2012;2012:692869. doi: 10.1155/2012/692869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thigpen C.A., Shanley E., Momaya A.M., Kissenberth M.J., Tolan S.J., Tokish J.M. Validity and responsiveness of the single alpha-numeric evaluation for shoulder patients. Am J Sports Med. 2018;46:3480–3485. doi: 10.1177/0363546518807924. [DOI] [PubMed] [Google Scholar]
- 53.Vega J.F., Jacobs C.A., Strnad G.J., Farrow L., Jones M.H., Miniaci A. Prospective evaluation of the patient acceptable symptom state to identify clinically successful anterior cruciate ligament reconstruction. Am J Sports Med. 2019;47:1159–1167. doi: 10.1177/0363546519831008. [DOI] [PubMed] [Google Scholar]
- 54.Wehby G.L., Naderi H., Robbins J.M., Ansley T.N., Damiano P.C. Comparing the visual analogue scale and the Pediatric Quality of Life Inventory for measuring health-related quality of life in children with oral clefts. Int J Environ Res Public Health. 2014;11:4280–4291. doi: 10.3390/ijerph110404280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Weldring T., Smith S.M. Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs) Health Serv Insights. 2013;6:61–68. doi: 10.4137/HSI.S11093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Williams G.N., Gangel T.J., Arciero R.A., Uhorchak J.M., Taylor D.C. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med. 1999;27:214–221. doi: 10.1177/03635465990270021701. [DOI] [PubMed] [Google Scholar]
- 57.Wixted J.J., Grover N.K., Anderson F.A., Jr., Fitzgerald R.H., Jr. Clinical outcomes in orthopaedic surgery. The collaborative efforts of orthopaedic surgeons with industry. Bull Hosp Jt Dis. 1999;58:161–165. [PubMed] [Google Scholar]
- 58.Yim J.H., Seon J.K., Song E.K., Choi J.I., Kim M.C., Lee K.B. A comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am J Sports Med. 2013;41:1565–1570. doi: 10.1177/0363546513488518. [DOI] [PubMed] [Google Scholar]
- 59.Zhang B., Thayaparan A., Horner N., Bedi A., Alolabi B., Khan M. Outcomes of hyaluronic acid injections for glenohumeral osteoarthritis: a systematic review and meta-analysis. J Shoulder Elbow Surg. 2019;28:596–606. doi: 10.1016/j.jse.2018.09.011. [DOI] [PubMed] [Google Scholar]