Abstract
Purpose
Os acromiale is a common entity in the middle-age group, in whom it is frequently associated with rotator cuff tears. However, it can be a cause of shoulder pain in the young athletes. We want to increase awareness of this pathology that may occultly affect the young athlete as well as to present the results of a perfusion-preserving arthrodesis.
Methods
Four consecutive young patients (17-21 years old) with a history of at least 6 months of unrecognized shoulder pain were surgically treated for os acromiale. Through a superior approach, stabilization of the neo-joint by means of cannulated screws and autogenic graft augmentation was performed.
Results
Union of the os acromiale was achieved in all the patients. They had an excellent functional outcome, reaching all the maximum Simple Shoulder Test (12) and Oxford shoulder Score (48) scores. All the patients were able to return to their previous sports level.
Conclusion
Awareness of the os acromiale in the young athlete, appropriate clinical examination, and image studies are crucial to confirm diagnosis. Surgical treatment aiming at fusion in situ has shown excellent result.
Keywords: Os acromiale, shoulder pain, overhead athlete, vascularity, arthrodesis
The os acromiale is an infrequent entity,12,14,17 related to rotator cuff tears5,10 and acromioclavicular (AC) joint arthritis9 in the middle aged. Sometimes it may affect the young and active individual and go unrecognized for a long time. It may present as unspecific subacromial pain.8,15
Normally the ossification centers complete their fusion by the age of 22-25 years and the bony bridging occurs from posterior to anterior.20 The reason for an eventual lack of fusion is possibly the mechanical strain on the developing acromion. During the perifusion phase, repetitive stress and strain or even a single traumatic event may stop the bridging process, resulting in a hypermobile joint.4 Striving at fusion of this diarthrodial joint has been proposed, with a variable success rate.3,8,13,16
The aim of this case series was to increase awareness of this pathology that may occultly affect the young athlete as well as to present the results of a perfusion-preserving arthrodesis.
Materials and methods
Between 2007 and 2017, 4 patients younger than 22 years underwent surgery for isolated unstable os acromiale (Table I).
Table I.
Pre- and postoperative data for the patients in our series
| Case | Age | Sex | Delay before diagnosis to surgery, mo | Mechanism | Stability OA | Screw stabilization | Postsurgical follow-up, mo | Preoperative SST | Postoperative SST | Preoperative OSS | Postoperative OSS |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 18 | M | 18 | Tennis overuse | Severe instability | Yes | 45 | 7 | 12 | 30 | 48 |
| 2 | 17 | F | 24 | Hockey repetitive trauma | Moderate unstable | No | 140 | 6 | 12 | 26 | 48 |
| 3 | 21 | M | 12 | Wrestling overload | Severe instability | Yes | 25 | 8 | 12 | 32 | 48 |
| 4 | 20 | M | 8 | Ski accident | Severe instability | Yes | 24 | 7 | 12 | 28 | 48 |
M, male; F, female; OA, os acromiale; SST, Shoulder Simple Test; OSS, Oxford Shoulder Score.
The first patient was an 18-year-old right-handed man evaluated at our office with right shoulder pain of 1.5 year's duration. He was a tennis player competing in the national league. The pain had started insidiously without any trauma while undergoing regular training and was more intense when hitting the forehand and serving. Two months after the initial onset of pain, he was referred to the orthopedic surgeon who examined him and asked for image studies. The simple shoulder radiographs were determined to be normal, and he was assigned to a physical therapy, including stretching, strengthening, cryotherapy, and anti-inflammatory drugs on demand. Following this treatment, however, he was unable to return to his previous level and compete in championships.
The second patient was a 17-year-old right-hand–dominant girl who presented in our office with left shoulder pain of 2 years’ duration. She was a hockey player on her regional competitive hockey team and she was a potential college scholarship athlete. No specific traumatic event was recalled with the progressive onset of symptoms. She reported that she had more pain when shooting from the left side and with minimal collisions during the game than at rest. Moreover, she felt pain when performing daily-life overhead activities or when sleeping on her left shoulder. Six weeks after the initial onset of pain, she visited her family doctor, who did not make a specific diagnosis, referring her to physiotherapy. After 2 months of physical therapy, cryotherapy, and rest, she resumed her sport activity and was involved again in competition. During the next few months, the shoulder pain increased in intensity until she was forced to stop all sport activity. Twenty-three months after the initial onset, the patient again visited the family doctor, who noted subacromial impingement signs and biceps tendinitis and referred her to us.
The third patient was a 21-year-old right-hand–dominant man who presented to our clinic with a 1-year history of left shoulder pain. He was a professional schwinger (a Swiss wrestling modality) ranked among the top 10 in the national league. He referred to multiple collisions and falls on both shoulders during routine fights, but he did not recall any of them as a pain trigger. He reported severe pain on the upper part of the left shoulder when wrestling the opponents. Two months after the onset of symptoms and before the end of the competitive season, he was forced to stop because of the severity of symptoms. The patient underwent physical therapy for 6 months, which failed to relieve shoulder pain when returning to training. After seeing the primary care physician, who examined him and observed the intense pain and mobility restriction, he was referred to our clinic.
The fourth patient was a 20-year-old right-hand–dominant man who showed up at our office after a history of 8 months' right shoulder pain. He was involved in overhead sports such as tennis and volleyball at a recreational level. The patient had first noticed discomfort in his right shoulder after a ski accident in which he fell on the same shoulder. Three days after the accident, he saw his primary care physician because of persistence of pain. After the examination, he obtained plain shoulder radiographs but they were unremarkable. The family doctor treated him with nonsteroidal anti-inflammatory drugs, cryotherapy, and rest. After 2 months, he began with his regular overhead sport activities but had increasing pain when hitting the ball in tennis, volleyball, and swimming, especially when crawling. The patient used cryotherapy after his workout, reporting temporary pain relief. Because the patient had prolonged pain of 8 months that impeded his daily-life activities, he sought a second opinion at our clinic.
All patients complained of subacromial “impingement-like” symptoms and had no previous surgeries. The physical examination revealed exacerbated pain with active flexion and abduction. The passive shoulder motions were symmetric without any loss of flexo-extension or rotations in the affected shoulders. Subacromial impingement maneuvers (Hawkins, Neer, and Yocum) were positive. Selective tenderness and discomfort occurred when strongly pressing over the acromio-acromial joint. Pressing down the acromion with a finger lead to visible and palpable motion at the site of the os acromiale (Video 1). Rotator cuff tests were consistently normal. Strength was reduced compared with the contralateral side. Neither the palpation of the acromioclavicular joint nor the cross-arm test was painful.
Imaging evaluation included anteroposterior, subacromial outlet, and axillary radiographs. Of these projections, the axillary was the most helpful to identify the os mesoacromiale in all cases (Fig. 1). A magnetic resonance imaging ruled out the presence of rotator cuff tears, SLAP lesions, or arthritic changes of the AC joint (Fig. 2). A further single-photon emission computed tomographic / computed tomographic scan (Fig. 3) confirmed that the nonunion had high metabolic activity.
Figure 1.
Axillary view radiograph of a left shoulder defines the neo-joint line (→) and the extension of the os mesoacromiale (- - - -).
Figure 2.
(Left) T1-weighted MRI coronal view of a left shoulder shows intact supraspinatus insertion. (Right) T1-weighted MRI axial view of a left shoulder shows the os mesoacromiale joint line (→) The adjacent acromioclavicular joint remains free of arthritic changes (- - - -). MRI, magnetic resonance imaging.
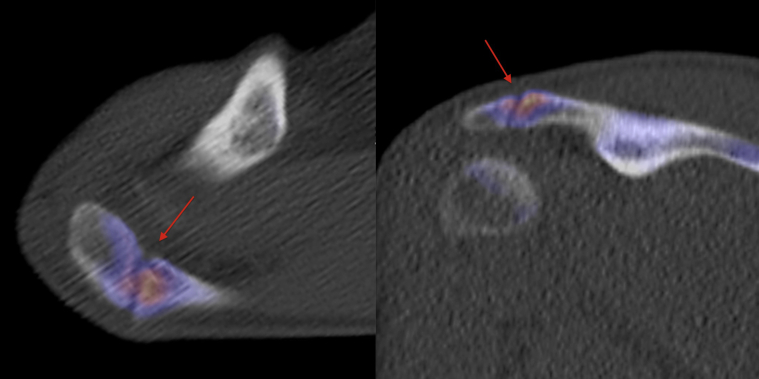
Figure 3.
SPECT/CT axial (left) and coronal (right) reveals increased activity at the unfused mesoacromion, indicating ongoing osteoblastic activity likely from a painful os acromiale. SPECT, single-photon emission CT; CT, computed tomography.
All patients underwent a course of conservative treatment, which included nonsteroidal anti-inflammatory drugs and physiotherapy, for at least 6 months. The purpose of the surgery was to obtain fusion of the acromion by resecting the joint, interposing an autogenic graft and stabilizing with screws. The patients were operated under general anesthesia in beach chair position using a superior approach.10 The dissection preserved the anterior deltoid and, thus, the vascular supply coming from the acromial branch of the thoracoacromial artery. The interacromial articulation was approached, performing minimal resection of 3 mm of the bone ends using a burr. About 80% of the “joint” was resected while preserving the inferior, medial, and lateral rims of the joint. The remaining 20% of the articular surfaces prevented shortening and malalignment of the acromion. The acromioclavicular joint was left intact. Autologous cancellous bone graft was harvested from the ipsilateral iliac crest and used to fill the defect. Finally, the os acromiale was stabilized using 2 fully threaded cannulated 3.5-mm screws introduced from the posterior acromial margin. The screws were inserted without compression to avoid shortening. In one patient, stability was considered sufficient to obtain healing of the bone graft and therefore no screws were used. Additional decortication of the bone ends and closure of the periosteum was done.
Postoperatively the patients were immobilized with a simple sling for 6 weeks. Within this time, free passive range of motion was allowed. In a second phase from week 7-12, active mobilization without load was allowed.
The patients were reviewed at 6 weeks, 12 weeks, and at 2 or more years postoperatively. At the last follow-up, analysis included clinical examination, the Oxford Shoulder Score, and the Simple Shoulder Test.2,7 Radiographic assessments using a modified axillary radiographic view were done to confirm fusion. The radiographic studies were independently assessed by 2 surgeons.
Results
The mean follow-up time at the final revision was 58 months (24, 26, 44, and 140 months, respectively, for each of the patients).
Patient 1 started shoulder-strengthening exercises 12 weeks after surgery and returned to training in the tennis court 5 months after surgery. Seventh months postoperatively he was able to play pain-free. At that time, he was allowed to participate in tennis competition without limitations, reaching the same preoperative level.
Twelve weeks after surgery, patient 2 was allowed to run and do static bicycling. At the fourth month, she was allowed to join her hockey training, progressively using her affected arm. Six months after the surgery, she was completely asymptomatic and returned to competition at the same level.
Patient 3 had complete range of motion 12 weeks after the surgery but was not allowed to return to Schwingen progressively until the seventh month. Because of the heavy load of the shoulder and violent falls during the combats, we adopted a more conservative attitude. He returned to competition 9 months postoperatively and won the national championship 15 months after the surgery.
Patient 4 was asymptomatic to perform daily living activities 3 months after the surgery. He started progressively swimming 4 months after the surgery, but was not allowed to return to overhead sports until the sixth month and reached the full level of sport activity at the 8-month mark. He asked for removal of a disturbing screw head on the posterior margin of the acromion 18 months after the index procedure.
On the radiologic studies, the os acromiale union was obtained in all patients (Fig. 4). The blinded radiologic union assessment by the 2 surgeons was always concordant. The mean functional score improved from 7 to 12 on the Simple Shoulder Test and from 29 to 48 on the Oxford shoulder Score.
Figure 4.
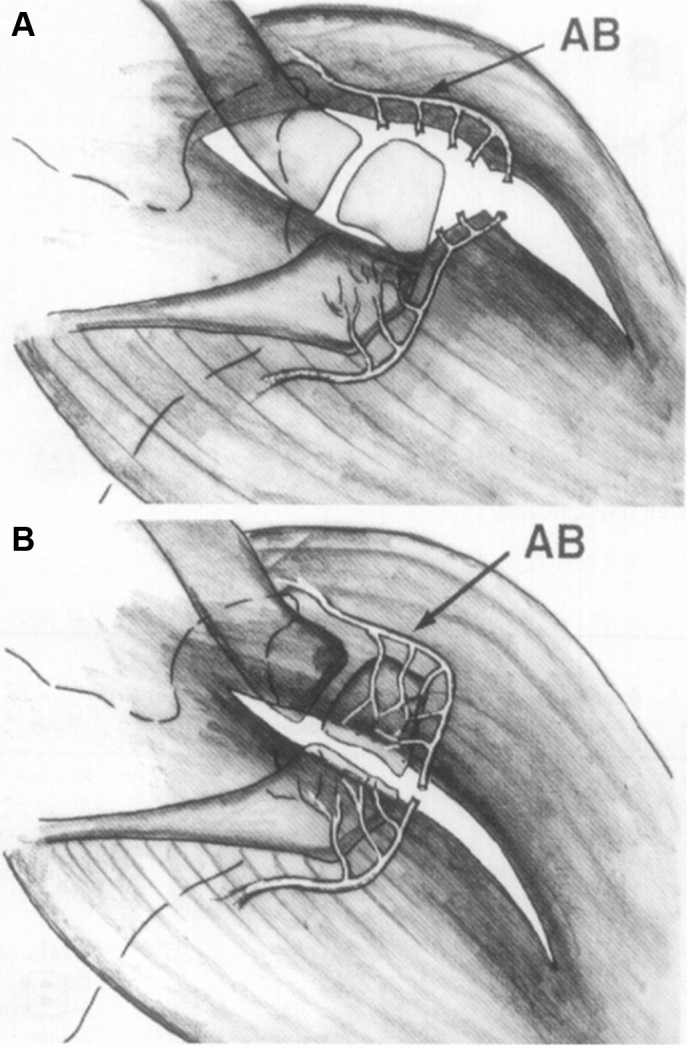
(A) Anterior approach: acromial terminal branches (AB) of the thoracoacromial artery are disrupted. (B) Superior approach: terminal branches of the thoracoacromial artery remain intact. Acromial epiphysis remains vital and maintains full healing potential.
Discussion
Shoulder symptoms in the presence of an os acromiale represent a particular challenge. Generally os acromiale are discovered when investigating rotator cuff lesions in middle-aged patients. Occasionally, unfused acromial apophyses become symptomatic early in adult life, long before the rotator cuff fails. It seems that sport-associated overuse might destabilize a previously asymptomatic os acromiale.
The authors have previously presented the results of os acromiale associated to rotator cuff tear, comparing the classic deltoid-off approach to the transacromial approach.10 This report focused on 4 cases in which an unstable os acromiale was the isolated source of shoulder pain. Other causes like AC joint pathology, subacromial impingement, or rotator cuff lesions were ruled out clinically and radiologically. Single-photon emission computed tomography / computed tomography was particularly useful to confirm the diagnosis.1
Several surgical techniques have been described to stabilize the os acromiale using screws, wire cerclage, or a combination of both.4,6,11,18 Most of them describe a complete resection of the neo-joint, applying compression to the fragments and thereby shortening the acromion length. We have chosen an open procedure aiming at a fusion in situ, thus avoiding shortening and angulation. Preservation of perfusion, stable fixation, and bone graft are the hallmarks of the procedure.
Although the type of fixation is considered the most important aspect for os acromiale healing, promotion of biological healing was even more crucial for us. We can argue in this respect that 1 of the cases from our series got the os acromiale consolidated without the necessity of screws, with excellent long-term results. In this specific case with mild os acromiale instability and inherent favorable biology due to the early age, decortication, periosteum restoration, and graft filling were sufficient for the consolidation.
The key element for successful consolidation of the os acromiale is preservation of acromial perfusion (Fig. 4). Through the superior approach, that does not require deltoid detachment and the vascular supply to the unfused epiphysis can be maintained. We also consider that placement of screws from the posterior margin of the acromion has less postoperative screw disturbance (Fig. 5). In addition, the risk of potential damage to the acromial branch when inserting the screws from the anterior is diminished.
Figure 5.
Axillary view radiograph of a left shoulder showing successful surgical fusion of mesoacromiale using 2 retrograde screws (3.5-mm). The acromion maintains its preoperative length and the acromioclavicular joint remains intact.
We also want to note that when the acromioclavicular joint is not affected, avoiding shortening of the acromion during surgery is paramount to preserve AC joint biomechanics.19 With this intention, we preserved cortices during resection and did not apply compression with the screws. Maintaining acromial length has an additional benefit by keeping the tension of the coracoacromial ligament. Otherwise, this ligament would behave as a bowstring pulling the tip of the acromion downward and causing impingement.
In conclusion, os acromiale may be a cause of otherwise unexplained shoulder pain in the young athlete. Adequate study of this entity with the appropriate clinical examination and image studies is crucial to confirm diagnosis. Surgical treatment aiming at fusion in situ has shown excellent results.
Disclaimer
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Acknowledgments
The authors would like to acknowledge Isabel Räschle for her translation skills to communicate and collect data from patients.
Footnotes
This study was approved by the Bern Cantonal Commission of Ethics (no. Req-2019-01140). Ethics approval was obtained to evaluate postoperative results, and the patients signed the informed consent form to be part of the research.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jseint.2020.02.008.
Supplementary Material
A left shoulder is examined with the examiner standing behind the patient. Although the right hand identifies the neo-joint with the index finger, the left hand lies on the anterior and posterior margins of the acromion, pressing the os acromiale downward, showing pathologic motion.
References
- 1.Al-faham Z., Jolepalem P. Use of SPECT/CT with 99mTc-MDP bone scintigraphy to diagnose symptomatic os acromiale. J Nucl Med Technol. 2015;43:236–237. doi: 10.2967/jnmt.114.150102. [DOI] [PubMed] [Google Scholar]
- 2.Angst F., Schwyzer H.-K., Aeschlimann A., Simmen B.R., Goldhahn J. Measures of adult shoulder function: Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) and its short version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and Elbow Surgeons (ASES) Society standardized shoulder assessment form, Constant (Murley) Score (CS), Simple Shoulder Test (SST), Oxford Shoulder Score (OSS), Shoulder Disability Questionnaire (SDQ), and Western Ontario Shoulder Instability Index (WOSI) Arthritis Care Res. 2011;63(Suppl 11):S174–S188. doi: 10.1002/acr.20630. [DOI] [PubMed] [Google Scholar]
- 3.Atoun E., van Tongel A., Narvani A., Rath E., Sforza G., Levy O. Arthroscopically assisted internal fixation of the symptomatic unstable os acromiale with absorbable screws. J Shoulder Elbow Surg. 2012;21:1740–1745. doi: 10.1016/j.jse.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 4.Barbier O., Block D., Dezaly C., Sirveaux F., Mole D. Os acromiale, a cause of shoulder pain, not to be overlooked. Orthop Traumatol Surg Res. 2013;99:465–472. doi: 10.1016/j.otsr.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 5.Boehm T.D., Matzer M., Brazda D., Gohlke F.E. Os acromiale associated with tear of the rotator cuff treated operatively. Review of 33 patients. J Bone Joint Surg Br. 2003;85:545–549. doi: 10.1302/0301-620x.85b4.13634. [DOI] [PubMed] [Google Scholar]
- 6.Campbell P.T., Nizlan N.M., Skirving A.P. Arthroscopic excision of os acromiale: effects on deltoid function and strength. Orthopedics. 2012;35:e1601–e1605. doi: 10.3928/01477447-20121023-16. [DOI] [PubMed] [Google Scholar]
- 7.Dawson J., Rogers K., Fitzpatrick R., Carr A. The Oxford Shoulder Score revisited. Arch Orthop Trauma Surg. 2009;129:119–123. doi: 10.1007/s00402-007-0549-7. [DOI] [PubMed] [Google Scholar]
- 8.Demetracopoulos C.A., Kapadia N.S., Herickhoff P.K., Cosgarea A.J., McFarland E.G. Surgical stabilization of os acromiale in a fast-pitch softball pitcher. Am J Sports Med. 2006;34:1855–1859. doi: 10.1177/0363546506288305. [DOI] [PubMed] [Google Scholar]
- 9.Gordon B.H., Chew F.S. Isolated acromioclavicular joint pathology in the symptomatic shoulder on magnetic resonance imaging: a pictorial essay. J Comput Assist Tomogr. 2004;28:215–222. doi: 10.1097/00004728-200403000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Hertel R., Windisch W., Schuster A., Ballmer F.T. Transacromial approach to obtain fusion of unstable os acromiale. J Shoulder Elbow Surg. 1998;7:606–609. doi: 10.1016/s1058-2746(98)90008-8. [DOI] [PubMed] [Google Scholar]
- 11.Johnston P.S., Paxton E.S., Gordon V., Kraeutler M.J., Abboud J.A., Williams G.R. Os acromiale: a review and an introduction of a new surgical technique for management. Orthop Clin North Am. 2013;44:635–644. doi: 10.1016/j.ocl.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 12.Kumar J., Park W.H., Kim S.H., Lee H.I., Yoo J.C. The prevalence of os acromiale in Korean patients visiting shoulder clinic. Clin Orthop Surg. 2013;5:202–208. doi: 10.4055/cios.2013.5.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lebus G.F., Fritz E.M., Hussain Z.B., Pogorzelski J., Millett P.J. Operative treatment of symptomatic meso-type os acromiale. Arthrosc Tech. 2017;6:e1093–e1099. doi: 10.1016/j.eats.2017.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nicholson G.P., Goodman D.A., Flatow E.L., Bigliani L.U. The acromion: morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg. 1996;5:1–11. doi: 10.1016/s1058-2746(96)80024-3. [DOI] [PubMed] [Google Scholar]
- 15.Pagnani M.J., Mathis C.E., Solman C.G. Painful os acromiale (or unfused acromial apophysis) in athletes. J Shoulder Elbow Surg. 2006;15:432–435. doi: 10.1016/j.jse.2005.09.019. [DOI] [PubMed] [Google Scholar]
- 16.Peckett W.R.C., Gunther S.B., Harper G.D., Hughes J.S., Sonnabend D.H. Internal fixation of symptomatic os acromiale: a series of twenty-six cases. J Shoulder Elbow Surg. 2004;13:381–385. doi: 10.1016/j.jse.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 17.Sammarco V.J. Os acromiale: frequency, anatomy, and clinical implications. J Bone Joint Surg Am. 2000;82:394–400. doi: 10.2106/00004623-200003000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Stetson W.B., McIntyre J.A., Mazza G.R. Arthroscopic excision of a symptomatic meso-acromiale. Arthrosc Tech. 2017;6:e189–e194. doi: 10.1016/j.eats.2016.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tauber M. Diseases of the acromioclavicular jointOrthopade. 2016;45:555–568. doi: 10.1007/s00132-016-3269-2. [in German]. https://doi.org/10.1007/s00132-016-3269-2. [DOI] [PubMed] [Google Scholar]
- 20.Yammine K. The prevalence of os acromiale: a systematic review and meta-analysis. Clin Anat. 2014;27:610–621. doi: 10.1002/ca.22343. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A left shoulder is examined with the examiner standing behind the patient. Although the right hand identifies the neo-joint with the index finger, the left hand lies on the anterior and posterior margins of the acromion, pressing the os acromiale downward, showing pathologic motion.