Abstract
Background
To address severe posterior subluxation associated with the Walch B2 glenoid deformity, the eccentricity of the prosthetic humeral head can be reversed, allowing the humerus to remain in a relatively posterior position while the prosthetic humeral head remains well-centered on the glenoid. This study describes the short-term outcomes after anatomic total shoulder arthroplasty (TSA) using this technique.
Methods
We retrospectively reviewed a consecutive series of patients with a B2 glenoid who underwent TSA with the prosthetic eccentric humeral head rotated anteriorly for excessive posterior subluxation noted intraoperatively. Medical records were reviewed for visual analog scale (VAS), American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES), and Simple Shoulder Test (SST) scores. Final radiographs were analyzed for instability, lesser tuberosity osteotomy healing, and glenoid loosening.
Results
Twenty patients were included with outcome scores at a mean of 48 months. Mean VAS (P < .0001), ASES (P < .0001), and SST (P < .0001) scores improved significantly. Using the Lazarus classification for glenoid loosening, 5 patients had grade 1 lucency and 2 had grade 2 lucency at a mean of 24 months' follow-up. The remaining 13 patients had no glenoid lucencies. Radiographic decentering was reduced from a mean of 9.9% ± 5.7% preoperatively to 0.5% ± 3.0% postoperatively (P < .001). There were no cases of lesser tuberosity repair failures or revision surgery.
Conclusion
TSA in patients with a B2 glenoid with a reversed, anterior-offset humeral head to address residual posterior subluxation resulted in excellent functional outcomes at short-term follow-up with improvement in humeral head centering. Early radiographic follow-up suggests low risks of progressive glenoid lucencies and component loosening.
Keywords: Shoulder arthroplasty, B2 glenoid, glenohumeral osteoarthritis, shoulder subluxation
Total shoulder arthroplasty has been shown to provide predictable pain relief and improvements in range of motion and function.2,3,15,16 However, in the setting of a biconcave glenoid wear pattern, classified by Walch as the “B2 glenoid,” outcomes have been shown to be less predictable.10,20 Glenoid loosening continues to be the most common cause of failure and indication for revision in total shoulder arthroplasty.1,6,7,21 Glenoid biconcavity, or a B2 glenoid in the Walch classification, has increasingly been recognized as a risk factor for accelerated glenoid loosening.19,21 This glenoid morphology is associated with posterior subluxation. Subluxation can persist postoperatively and is thought to be associated with postoperative instability, pain, and decreased implant survivorship.20 Complication rates have been high enough for some authors to suggest that reverse shoulder arthroplasty may be a more predictable option in patients with this wear pattern, especially in patients with more than 25° of glenoid retroversion and greater than 80% posterior humeral head subluxation.4,13,20 Recentering the humeral head and placement of a glenoid in near neutral version may lead to improved long-term outcomes of total shoulder arthroplasty in patients with a B2 glenoid.3
In the setting of a B2 glenoid, the dynamic forces that cause posterior subluxation continue to exist postoperatively despite shoulder arthroplasty. This persistent tendency for posterior subluxation leads to edge-loading and wear of the prosthetic glenoid. To address the natural tendency of the humeral head to translate posteriorly, the humeral head offset can be reversed to dial the maximum humeral head eccentricity anteriorly. This allows the humerus to remain posterior as a result of dynamic forces that persist after arthroplasty, whereas the articular portion of the implant remains centered on the glenoid (Fig. 1).
Figure 1.
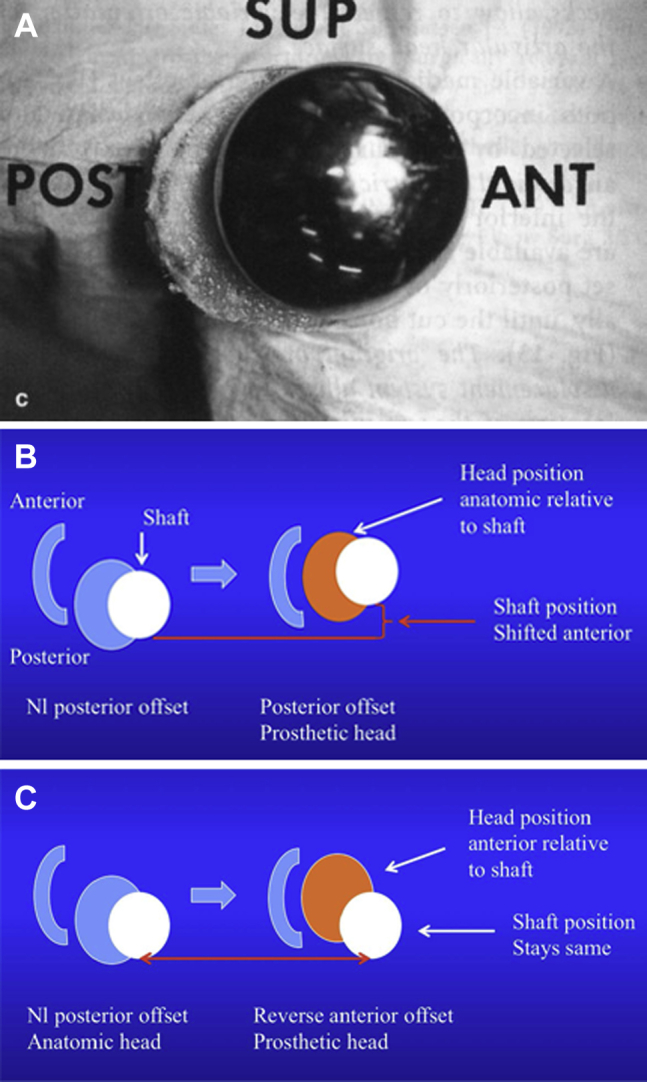
Demonstration of reverse offset of the humeral head. (A) Sawbones model. (B) Schematic of anatomic dialing of an eccentric head. The prosthetic glenoid is indicated by the C shape to the left. (C) Schematic demonstrating reverse offset dialing of an eccentric head allowing the humeral shaft to remain posterior.
A cadaveric model evaluating this technique has shown increased resistance to posterior humeral head translation and anteriorly directed joint contact pressures in shoulders with significant glenoid retroversion.11 Finite element analysis has demonstrated that anterior offset of the humeral head leads to significant increases in anterior-directed centering pressures of the humeral head on the glenoid component.12 Anterior humeral head offset has been described clinically to address intraoperative posterior humeral head subluxation in patients undergoing either hemiarthroplasty with a ream-and-run technique or total shoulder arthroplasty with good results in a small patient sample.9 The purpose of this study is to report the clinical and radiographic outcomes of anterior humeral head offset in patients undergoing total shoulder arthroplasty in the setting of preoperative posterior humeral head subluxation and a B2 glenoid deformity. Our hypothesis is that patients treated with an anterior-offset total shoulder arthroplasty have good clinical outcomes and a low rate of glenoid loosening, posterior subluxation, and need for revision surgery at short-term follow-up.
Materials and methods
After institutional review board approval, we performed a retrospective case series to identify patients who underwent a total shoulder arthroplasty between 2007 and 2014 using a departmental billing database (CPT code 23472). We included patients with a B2 glenoid deformity on preoperative imaging that were treated with an anatomic total shoulder arthroplasty with an anterior-offset humeral head.
All patients underwent primary anatomic total shoulder arthroplasty to surgically manage primary osteoarthritis using a deltopectoral approach. All glenoid deformities were managed using high-side (anterior) corrective reaming with a goal to ream to within approximately 10°-15° of normal anatomic glenoid version. Anterior reaming was not performed to the point of completely correcting glenoid version to the normal premorbid version as this would cause prohibitive bone loss and joint medialization. The premorbid glenoid version and humeral head posterior subluxation was assessed by the surgeon using preoperative radiographs and computed tomographic (CT) scans (when available). Preoperative imaging combined with intraoperative visualization guided the amount of anterior reaming needed to achieve the desired correction. Corrective reaming was performed until a minimum of adequate seating (estimated 80%) of the glenoid face was achieved. An in-line pegged polyethylene glenoid component (Zimmer, Warsaw, IN, USA) was implanted. All patients included in this study had the prosthetic humeral head placed using an anterior-offset technique to address excessive posterior humeral head subluxation noted intraoperatively. Posterior subluxation was considered excessive if the trial prosthetic humeral head translated >100% posteriorly and/or remained subluxated posteriorly more than 50% relative to the prosthetic glenoid with the shoulder resting in adduction and neutral rotation. This assessment was performed after the appropriate head size was determined and all soft tissue releases of the anterior and inferior capsule were performed along with osteophyte resection. Based on this intraoperative assessment, placement of an anterior-offset humeral head was performed in 32 of 114 patients with a B2 glenoid during the study period. The technique of reverse offset entailed dialing the eccentric humeral head from the normal posterior offset to an anterior-offset position while maintaining the appropriate head height to greater tuberosity relationship. This results in the prosthetic head overhanging anteriorly and may leave a small amount of uncovered humeral cut surface posteriorly. Uncovered posterior bone was left in place if it did not engage the glenoid while externally rotating up to 40° during trialing. By leaving the posterior bone to fill the posterior joint space, the posterior rotator cuff tissues and capsule would maintain their length-tension relationships that had developed over the long term. No concomitant rotator interval plication or posterior capsular plications were performed in any case. In all cases, the subscapularis was managed with a lesser tuberosity osteotomy. Repair of the lesser tuberosity was performed with heavy nonabsorbable suture around the stem and through lateral bone tunnels that cerclaged the lesser tuberosity fragment. The medial aspect of the lesser tuberosity was typically buttressed against the undersurface of the humeral head prosthesis.
We retrospectively reviewed medical records and collected preoperative visual analog scale for pain scores, American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form (ASES) scores, and Simple Shoulder Test scores. Patients were contacted and invited to return for clinical examination and radiographic follow-up. Images from a respective case are shown in Fig. 2. Three fellowship-trained shoulder surgeons reviewed the initial postoperative and most recent radiographs for glenoid lucencies according to the Lazarus classification. An average score was calculated and rounded to the nearest whole number. We considered the glenoid component to be radiographically loose if the Lazarus score was 4 or greater or there was gross subsidence of the glenoid component. Lesser tuberosity osteotomy healing was examined on both the anteroposterior and the axillary radiographs. We considered an osteotomy healed if there was bony union or if there was a visible gap measuring less than 2 mm without displacement of the tuberosity, indicating a fibrous union.
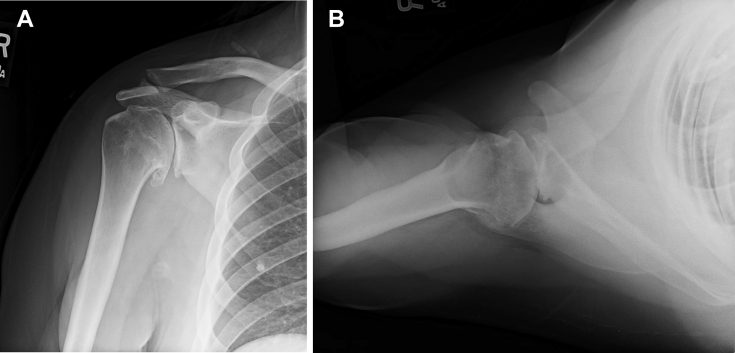
Figure 2.
Preoperative radiographs demonstrating primary glenohumeral osteoarthritis with a biconcave (B2) glenoid. (A) True anteroposterior view. (B) Axillary view.
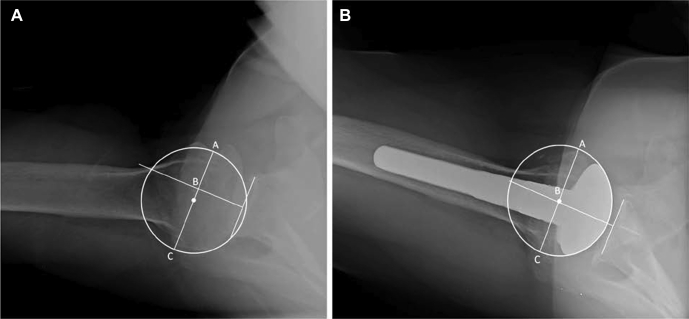
Preoperative and postoperative final follow-up radiographs were analyzed to determine the extent of posterior subluxation or “decentering” of the humeral head relative to the glenoid face on axillary radiographs. This method of determining humeral head centering has been previously described.9 This method describes the amount of decentering as a percentage of the humeral head that is subluxated from a perpendicular line that bisects a line drawn from the anterior to the posterior glenoid face. A perfectly centered humeral head would yield a value of 50%. An example of this measurement technique is shown in Fig. 3. Preoperative and postoperative final follow-up radiographs were analyzed for centering by 2 fellowship-trained shoulder surgeons.
Figure 3.
A line is drawn from the anterior rim of the glenoid to the posterior rim. A perpendicular line is drawn bisecting the glenoid line. A circle is drawn and fit to the humeral head. A line (AC) is drawn as a diameter through the circle and parallel to the glenoid line. Point B is the intersection of line AC and the perpendicular bisector of the glenoid line. The ratio lines BC/AC in a centered humeral head is 0.5. The percent decentering was calculated as (BC/AC − 0.5) × 100%. In this example, there is 12% posterior decentering preoperatively (A). Postoperatively (B), with placement of the eccentricity of the humeral head prosthesis anteriorly, there is <0.2% decentering.
Two-tailed Student t tests were used to compare means of continuous variables. A P value of .05 was set as significant. Chi-square or Fisher exact test was used to compare dichotomous outcome variables. All statistical analysis was done using SPSS software (IBM, Armonk, NY, USA).
Results
Thirty-two patients underwent a total shoulder arthroplasty with an anterior-offset humeral head to treat primary osteoarthritis with a B2 glenoid and posterior subluxation. Eleven patients were unable to be contacted, and 3 patients declined to participate in the study. Thus, 20 patients met our inclusion criteria and had clinical outcome scores at an average of 49 months postoperatively (28-78 months).
There were 16 male and 4 female patients with an average age of 61.7 years (range 43-81 years). Preoperative, postoperative, and change in outcome scores are shown in Table I. Mean visual analog scale scores improved from 7.5 ± 1.4 preoperatively to 1.0 ± 1.7 postoperatively (P < .0001). ASES score improved from 32.7 ± 13.6 to 86.2 ± 16.5 (P < .0001), and the Simple Shoulder Test improved from 4.9 ± 2.6 to 9.8 ± 1.7 (P < .0001). Using previously established minimum clinically important differences, 19/20 patients (95%) had a clinically significant change in the visual analog scale for pain score and ASES score, whereas 18/20 (90%) achieved a minimum clinically significant improvement in the Simple Shoulder Test score.17
Table I.
Summary of operations
| Variable | Preoperative |
Postoperative |
Change |
|||
|---|---|---|---|---|---|---|
| Mean (SD) | Range | Mean (SD) | Range | Mean (SD) | Range | |
| SST | 4.9 (2.6) | 0-9 | 9.8 (1.7) | 6-12 | 5.1 (2.6) | 1-12 |
| VAS-pain | 7.5 (1.4) | 5-10 | 1.0 (1.7) | 0-6 | −6.1 (2.1) | −10 to −1.0 |
| ASES | 32.7 (13.6) | 6.7-53.3 | 86.2 (16.5) | 38.3-100 | 53.5 (18.3) | 13.3-93.3 |
SST, Simple Shoulder Test; VAS-pain, visual analog scale for pain; ASES, American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form; SD, standard deviation.
Preoperative and postoperative radiographs were reviewed in all cases. Preoperative CT scans were available in 15 cases. Mean preoperative glenoid version measured on available CT scans was 31° ± 8°. Mean preoperative posterior subluxation was 71% ± 10%. Final radiographs were obtained at a mean of 24 months. Radiographic analysis demonstrated no cases of postoperative instability. Using the Lazarus classification, initial postoperative radiographs demonstrated excellent initial cement technique, with 15 patients having no evidence of radiolucent lines and 5 with grade 1 radiolucent lines around the pegs. On final follow-up radiographs, 5 patients had grade 1 lucencies and 2 had grade 2 lucencies around the glenoid pegs. The remaining 13 patients had no glenoid lucencies (Table II). Comparing subjects individually, 4 had progression of radiolucent lines of 1 grade and zero subjects had progression of 2 grades or more. No patients had radiographic evidence of glenoid loosening or subsidence. There were no cases of lesser tuberosity repair failures. No patients had subjective complaints of instability, and there were no revision surgeries at final follow-up. Radiographic decentering was reduced from a mean of 9.9% ± 5.7% preoperatively to 0.5% ± 3.0% postoperatively (P < .001). Preoperatively, 18/20 (90%) were decentered 5% or greater. Postroperatively, zero shoulders were posteriorly decentered greater than 5%. Postoperative radiographs after utilizing this technique are shown in Fig. 4.
Table II.
Glenoid radiolucency measurements
| Lazarus grade | First postoperative radiograph, mean (SD) | Final radiograph, mean (SD) |
|---|---|---|
| Grade 0 | 15 | 13 |
| Grade 1 | 5 | 5 |
| Grade 2 | 0 | 2 |
| Grade 3 | 0 | 0 |
| Grade 4 | 0 | 0 |
| Grade 5 | 0 | 0 |
SD, standard deviation.
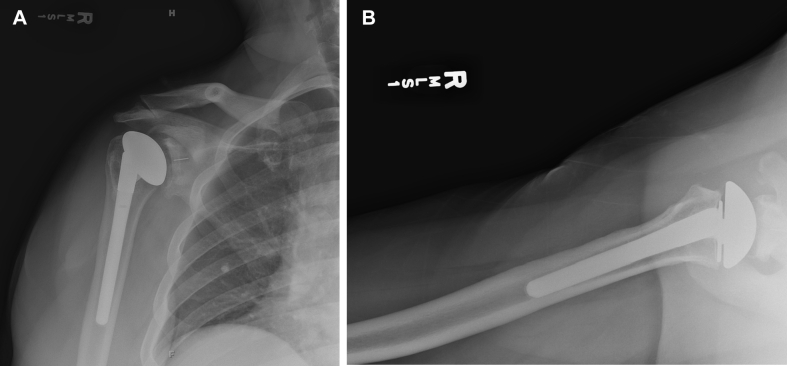
Figure 4.
Final postoperative radiographs showing concentric glenohumeral prosthetic alignment with a reverse offset humeral head and a healed lesser tuberosity osteotomy. (A) True anteroposterior view. (B) Axillary view.
Discussion
This retrospective study reports the short-term clinical and radiographic results of total shoulder arthroplasty with an anterior-offset humeral head to address persistent intraoperative posterior subluxation in total shoulder arthroplasty patients with a B2 glenoid. In this study, 95% of patients had a clinically significant improvement in pain and function as measured with the ASES score. In addition, the rate of progressive glenoid radiolucencies was low, no patients had evidence of early glenoid loosening, and there were no postoperative complications such as instability or nonunion or displacement of the lesser tuberosity osteotomy fragment. We believe this technique of partial glenoid version correction combined with anterior “reverse” offset of the humeral head prosthesis to represent a viable option for select B2 arthritic shoulders.
Recent biomechanical data have demonstrated increased resistance to posterior humeral head translation and improved joint contact pressures in shoulders with significant glenoid retroversion treated with an anterior-offset technique.11 Finite element analysis has confirmed an anterior shift in the center of pressure with an anterior-offset humeral head in the setting of increased glenoid retroversion.12 Hsu et al9 have reported good outcomes for a series of 33 patients undergoing either total shoulder arthroplasty or hemiarthroplasty who required an anterior-offset humeral head technique to correct intraoperative posterior humeral head subluxation. To our knowledge, this is the first case series to report on this technique in the clinical setting for patients undergoing total shoulder arthroplasty exclusively for glenohumeral arthritis with B2 glenoid deformities.
Posterior glenoid erosion is postulated to be a progressive process, with every degree of glenoid retroversion resulting in a 0.5-mm posterior shift of the humeral head and a resultant 0.5° shift of the force vector posterior from the center of the glenoid.14 Over time, the soft tissues about the shoulder adapt to the posterior position of the proximal humerus, and these forces can be difficult to overcome with corrective reaming or augmented components that realign the humerus anteriorly. In fact, Kim et al11 postulated that correcting the humeral position may escalate the posterior pull of the soft tissues. Anteriorly offsetting the humeral head allows the head center to have congruent alignment to the glenoid center while allowing the proximal humerus to remain in a relatively posterior position, thus mitigating the adaptive posterior pull of the soft tissues. If the proximal humerus is maintained in a posterior position, the muscle forces across the shoulder have a more anteromedial vector that may contribute to congruent glenoid loading and improved joint stability. One concern with this technique is the anterior overhang of the humeral head over which the subscapularis tendon must drape. There were no complications with the subscapularis repair in our study as all of the lesser tuberosity osteotomies healed. However, theoretically, this technique may present a challenge in the setting of a subscapularis peel or tenotomy due to the anterior overhang of the prosthesis.
Historically, B2 glenoid deformity is associated with increased failure rates of total shoulder arthroplasty.10 Eccentric loading of the glenoid in these shoulders can result in early prosthetic loosening, which combined with persistent posterior humeral head subluxation may result in an increased risk for early revision surgery. Walch et al20 showed that good clinical results in patients with a B2 glenoid can be obtained; however, increasing complication rates are seen with greater degrees of glenoid retroversion and posterior subluxation. In their study, patients with more than 30° of retroversion had a 62% complication rate, and 73% of the complications occurred in the group of patients with a neoglenoid retroversion greater than 27°. In that series, 20.6% of glenoid components were radiographically loose at a mean of 77 months. In the present study, we had no shoulders with radiographic loosening of the glenoid component, although these results are early and not directly comparable to those published by Walch et al. Our initial postoperative radiolucencies scores demonstrated that good cement mantles were obtained at the time of surgery (no instances of grade 2 or higher radiolucencies). At short-term follow-up, 2 of 20 (16%) shoulders demonstrated grade 2 radiolucencies, with no instances of radiographic loosening. The rate of progression of radiolucencies seen in the present study is comparable to those of a general osteoarthritis population at short-term follow-up.5,18 Further studies are warranted to examine the durability of these implants over time.
Our study has several limitations inherent to its retrospective design; however, the clinical results of this technique are promising. Despite exhaustive attempts to contact patients, we were unable to recruit 37% of eligible subjects. We do feel that our study is representative of the entire cohort given the observed severity of preoperative radiographic findings and feel; therefore, that selection bias is limited. Also, although this is the largest clinical cohort of patients treated with this technique, our study is underpowered to evaluate specific factors that may affect glenoid loosening. All patients in our cohort had a standard cylindrical diaphyseal stemmed humeral implant. It is possible that eccentric forces on the humeral implant from a nonanatomic, anteriorly offset humeral head prosthesis could cause loosening of short-stem or stemless implants. The use of advanced imaging studies (CT scan and magnetic resonance imaging) preoperatively was not controlled. For this reason, we were not able to precisely define the severity of preoperative glenoid retroversion deformities within this cohort; thus we cannot conclude that this surgical technique is applicable to all severities of B2 deformities seen in osteoarthritic shoulders. All shoulders demonstrated gross recentering of the head relative to the glenoid, and there were no instances of posterior subluxation seen clinically. We were able to demonstrate this recentering by measuring centeredness on axillary radiographs using a previously validated method.9 However, given the lack of postoperative CT scans and preoperative CT scans in some cases, we quantified head position using radiographs only. Thus, precision in quantifying pre- and postoperative posterior humeral head subluxation is limited as has been previously shown in a prior study.8 Our study only analyzed patients with a stemmed implant. We cannot comment on the potential alteration of forces affecting humeral fixation that may affect short-stem or stemless humeral implants. Finally, our findings are short-term, and the durability of this technique will require long-term follow-up studies.
Conclusions
In this small retrospective series, total shoulder arthroplasty with partial glenoid version correction and the use of a reversed, anterior-offset humeral head to address residual posterior subluxation in patients with a B2 glenoid deformity resulted in excellent functional outcomes at short-term follow-up with improvement in humeral head centering. Early radiographic follow-up suggests low risks of progressive glenoid lucencies and component loosening.
Acknowledgments
The authors thank Georgia Stobbs-Cucchi, Lauren Bayens, and Karen Holtman for their assistance in the data collection for this study, and Carrie Heineman for her assistance in the manuscript submission.
Disclaimer
Aaron M. Chamberlain receives research support from Zimmer Biomet, Inc., and is a consultant for Arthrex, Wright Medical, and DePuy Synthes.
Jay D. Keener receives research support from Zimmer, Inc.; is a consultant for Arthrex and Imascap; receives royalities from Shoulder Innovations and Wright Medical; and was funded by a National Institute of Health Grant.
The other authors, their immediate families, and any research foundations with which they are affiliated have not received any financial payments or other benefits from any commercial entity related to the subject of this article.
Footnotes
The Washington University in St. Louis Institutional Review Board approved this work (IRB 201409158).
References
- 1.Bonnevialle N., Melis B., Neyton L., Favard L., Molé D., Walch G. Aseptic glenoid loosening or failure in total shoulder arthroplasty: revision with glenoid reimplantation. J Shoulder Elbow Surg. 2013;22:745–751. doi: 10.1016/j.jse.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 2.Bülhoff M., Sattler P., Bruckner T., Loew M., Zeifang F., Raiss P. Do patients return to sports and work after total shoulder replacement surgery? Am J Sports Med. 2015;43:423–427. doi: 10.1177/0363546514557940. [DOI] [PubMed] [Google Scholar]
- 3.Chin P.C., Hachadorian M.E., Pulido P.A., Munro M.L., Meric G., Hoenecke H.R. Outcomes of anatomic shoulder arthroplasty in primary osteoarthritis in type B glenoids. J Shoulder Elbow Surg. 2015;24:1888–1893. doi: 10.1016/j.jse.2015.05.052. [DOI] [PubMed] [Google Scholar]
- 4.Denard P.J., Walch G. Current concepts in the surgical management of primary glenohumeral arthritis with a biconcave glenoid. J Shoulder Elbow Surg. 2013;22:1589–1598. doi: 10.1016/j.jse.2013.06.017. [DOI] [PubMed] [Google Scholar]
- 5.Edwards T.B., Labriola J.E., Stanley R.J., O'Connor D.P., Elkousy H.A., Gartsman G.M. Radiographic comparison of pegged and keeled glenoid components using modern cementing techniques: a prospective randomized study. J Shoulder Elbow Surg. 2010;19:251–257. doi: 10.1016/j.jse.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 6.Farron A., Terrier A., Büchler P. Risks of loosening of a prosthetic glenoid implanted in retroversion. J Shoulder Elbow Surg. 2006;15:521–526. doi: 10.1016/j.jse.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Ho J.C., Sabesan V.J., Iannotti J.P. Glenoid component retroversion is associated with osteolysis. J Bone Joint Surg Am. 2013;95:e82. doi: 10.2106/JBJS.L.00336. [DOI] [PubMed] [Google Scholar]
- 8.Ho J.C., Youderian A., Davidson I.U., Bryan J., Iannotti J.P. Accuracy and reliability of postoperative radiographic measurements of glenoid anatomy and relationships in patients with total shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22:1068–1077. doi: 10.1016/j.jse.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 9.Hsu J.E., Gee A.O., Lucas R.M., Somerson J.S., Warme W.J., Matsen F.A., 3rd Management of intraoperative posterior decentering in shoulder arthroplasty using anteriorly eccentric humeral head components. J Shoulder Elbow Surg. 2016;25:1980–1988. doi: 10.1016/j.jse.2016.02.027. [DOI] [PubMed] [Google Scholar]
- 10.Iannotti J.P., Norris T.R., Levine W., Barrett W., Franklin J., Kelly I. Influence of preoperative factors on outcome of shoulder arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 2003;85:251–258. doi: 10.1016/s1058-2746(97)70052-1. [DOI] [PubMed] [Google Scholar]
- 11.Kim H.M.M., Chacon A.C., Andrews S.H., Roush E.P., Cho E., Conaway W.K. Biomechanical benefits of anterior offsetting of humeral head component in posteriorly unstable total shoulder arthroplasty: a cadaveric study. J Orthop Res. 2016;34:666–674. doi: 10.1002/jor.23048. [DOI] [PubMed] [Google Scholar]
- 12.Lewis G.S., Conaway W.K., Wee H., Kim H.M. Effects of anterior offsetting of humeral head component in posteriorly unstable total shoulder arthroplasty: finite element modeling of cadaver specimens. J Biomech. 2017;53:78–83. doi: 10.1016/j.jbiomech.2017.01.010. [DOI] [PubMed] [Google Scholar]
- 13.Mizuno N.M., Denard P.J.M., Raiss P.M., Walch G.M. Reverse total shoulder arthroplasty for primary glenohumeral osteoarthritis in patients with a biconcave glenoid. J Bone Joint Surg Am. 2013;95:1297–1304. doi: 10.2106/JBJS.ST.M.00048. [DOI] [PubMed] [Google Scholar]
- 14.Nyffeler R.W., Sheikh R., Atkinson T.S., Jacob H.A.C., Favre P., Gerber C. Effects of glenoid component version on humeral head displacement and joint reaction forces: an experimental study. J Shoulder Elbow Surg. 2006;15:625–629. doi: 10.1016/j.jse.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 15.Raiss P., Bruckner T., Rickert M., Walch G. Longitudinal observational study of total shoulder replacement with cement. J Bone Joint Surg Am. 2014;96:198–205. doi: 10.2106/JBJS.M.00079. [DOI] [PubMed] [Google Scholar]
- 16.Raiss P., Schmitt M., Bruckner T., Kasten P., Pape G., Loew M. Results of cemented total shoulder replacement with a minimum follow-up of ten years. J Bone Joint Surg Am. 2012;94 doi: 10.2106/JBJS.K.00580. e1711-10. [DOI] [PubMed] [Google Scholar]
- 17.Tashjian R.Z., Hung M., Keener J.D., Bowen R.C., McAllister J., Chen W. Determining the minimal clinically important difference for the American Shoulder and Elbow Surgeons score, Simple Shoulder Test, and visual analog scale (VAS) measuring pain after shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26:144–148. doi: 10.1016/j.jse.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 18.Throckmorton T.W., Zarkadas P.C., Sperling J.W., Cofield R.H. Pegged versus keeled glenoid components in total shoulder arthroplasty. J Shoulder Elbow Surg. 2010;19:726–733. doi: 10.1016/j.jse.2009.10.018. [DOI] [PubMed] [Google Scholar]
- 19.Walch G., Badet R., Boulahia A., Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty. 1999;14:756–760. doi: 10.1016/s0883-5403(99)90232-2. [DOI] [PubMed] [Google Scholar]
- 20.Walch G., Moraga C., Young A., Castellanos-Rosas J. Results of anatomic nonconstrained prosthesis in primary osteoarthritis with biconcave glenoid. J Shoulder Elbow Surg. 2012;21:1526–1533. doi: 10.1016/j.jse.2011.11.030. [DOI] [PubMed] [Google Scholar]
- 21.Walch G., Young A.A., Boileau P., Loew M., Gazielly D., Molé D. Patterns of loosening of polyethylene keeled glenoid components after shoulder arthroplasty for primary osteoarthritis: results of a multicenter study with more than five years of follow-up. J Bone Joint Surg. 2012;94:145–150. doi: 10.2106/JBJS.J.00699. [DOI] [PubMed] [Google Scholar]