Abstract
Objective: kinematic alignment technique has been recently described as a new surgical procedure able to restore the patient specific physiological knee alignment; furthermore, new prosthesis, as medial stabilized (MS) third generation TKA, were designed to better reproduce the anatomical shape of the knee. In this prospective study, the authors evaluated early clinical improvement and radiological outcomes of patients having pre-operative small coronal limb deformity underwent TKA using a surgical technique combining a “restricted kinematic alignment” with medial stabilized polyethylene insert.
Methods
Fifteen consecutive patients (8 female and 7 male) scheduled for a total knee replacement have been enrolled for this study and treated using a modern third generation knee implant with a medial congruent tibial polyethylene. Clinical improvements have been assessed pre-operatively and at 6 and 12 months Follow up (FU) using the Oxford knee Score (OKS)( Ishikawa et al., Jun. 2015) 12 the Knee Society Score (KSS)( Pinskerova and et al., Aug. 2004) 13 and Forgotten Joint Score (FJS) as patient reported outcomes measurement system (PROMs). A radiological evaluation was made by a single physician at 6 months.
Results
Average improvement in OKS was from 20.2 (SD 5.5) pre-operatively to 41.3 (SD 2.1) at the final FU. KSS pain/motion improved with a mean score from 40.1 (SD 4.0) pre-op to 89.1 (SD 6.3) while KSS function improved with an average score from 51.0 (SD 6.2) pre-op to 81.8 (SD 8.4) showing good to excellent results in all the knee treated. The mean FJS at 6 months follow up was 75.1 (SD 4.2) improving to 79.3 (SD 3.3) at one year FU. Post-operative XR showing an average varus Hip-Knee-Ankle (HKA) angle of 178.8° (range from 176° to 182°, SD 2,3°); We found no statistically significant difference between pre-operative and post-operative HKA (p < 0,05).
Conclusion
The current authors assumed appropriate to combine a modern TKA implant designed replicating the anatomical shape of the native knee with a surgical technique able to better reproduce the physiological, patient specific, knee biomechanics. Our findings suggest that combining MS implant with KA technique may results in better short-term functional results, helping the patient to “forget” their replaced joint and restoring their pre-arthritic quality of life.
Keywords: Total knee arthroplasty, TKA, Kinematic alignment, Restricted KA, Medial stabilized design, Knee
1. Introduction
Total knee arthroplasty (TKA) is a successful and safe surgical procedure able to restore function and relieve pain in knees affected by bi- or tricompartimental knee osteoarthritis.1
In the last years, advances have been made in primary TKA, however, numerous studies using historical TKA implant suggest that almost 20% of patients are not fully satisfied2 and, moreover, there is a large discordance between surgeon's and patient’ s perception of clinical results.3
One of the main challenges in the future of orthopedic surgery, along with a constant search for new advancements, will be wisely mix those innovations to enhance their single potential and definitively switch from a systematic to a patient specific approach that fulfils individual requests.
Knee surgeons should focus on modifiable factors that might affect overall satisfaction such as proper patient's selection, surgical technique and type of implants.4
A TKA aligned to the mechanical axis of the lower limb on the coronal plane following the guidelines of mechanical alignment (MA) technique has been the gold standard for several years.5 This method could be considered a “systematic approach” able to gain reproducible radiological results regardless of pre-arthritic axial deformities. Normally, this surgical technique was combined with classic cruciate retaining (CR) or posterior stabilized (PS) TKA designs2 which rarely reproduced the physiological “in vivo” knee kinematic.6
Recently, Howell et al. introduced the kinematic alignment (KA)method: a new surgical technique that focuses on restore physiological knee alignment in order to better reproduce the normal knee kinematic adopting a patient specific approach.7 Furthermore, new prosthesis, as medial stabilized (MS) third generation TKA, were designed to better reproduce the anatomical shape of the knee.8
However, following more cautious physicians, the current authors considered eligible for a KA method few selected patients with a small frontal limb deformity (≤5°) and opted for a compromise performing a TKA on patient having considerable coronal limb deformity or joint line obliquity.9 In these selected patients, the authors suggest combining a “restricted kinematic alignment” with medial stabilized design to re-establish the normal knee biomechanics.
Rationale combining a MS third generation prosthesis design with a KA technique is based on three significant principles driving the normal knee movement: axes of rotation, anatomy of the femoral condyle and femoral roll-back phenomenon.
Historically, the trans-epicondylar axis (TEA) was identified as the landmark which better approximate the axis around which the tibia moves in space during flexion-extension of the knee but, concerns exist about accuracy of the TEA as a surrogate of the real transverse axis in the femur about which the tibia flexes and extends: this flexion-extension axis (FEA) has been extensively described by Howell10 and it is used as important reference following a KA technique to achieve a proper components alignment restoring the patient-specific femorotibial joint line orientation and native soft tissue balance.
FEA is reported as a line passing through the center of a circle fit to the articular surface of the femoral condyles from 10 to 160° of flexion confirming previous anatomical studies which reported evidence about a specific geometry with a single radius on the posterior part of the femoral condyles.11 In addition, greater femoral “roll-back” and more external rotation of the femoral component were observed with kinematically aligned TKA than mechanically aligned TKA reproducing a normal knee motion.12
The term “roll-back” describes a movement, driven by the tension in the cruciate ligaments, where a posterior translation of the lateral femoral condyle on the tibial plateau in observed during active and passive flexion of the normal knee, this movement is negligible on the medial femoral condyle. The knee rotation along an axis placed on the medial compartment is described as “medial-pivoting” and this phenomenon characterizes the normal knee biomechanics as confirmed by Pinskerova et al.13 which identified in the 2004 the point of closest approximation between the femoral and tibial subchondral plates and studied the movement of this contact points showing as the femur rotates externally around a medial center.
Modern MS TKA implants are designed trying to reproduce this normal kinematics of the knee miming the physiological “medial pivoting” pattern with a greater conformity on the medial compartment between tibial insert and femoral condyle and a less congruency on the lateral side.
A greater medial conformity is provided by a concave surface on the medial compartment of the tibial insert with an anterior lip that stabilizes the knee from full extension through deep flexion, in contrast, the lateral condyle is designed to move more freely along an arcuate path.8
The objective of this prospective study is to evaluate clinical improvement and radiological outcomes of patients at minimum 12 – mounts follow-up underwent TKA using a modern third generation knee implant with a medial congruent polyethylene insert combined with the kinematic alignment technique. The current authors assumed appropriate to combine a modern TKA implant designed replicating the anatomical shape of the native knee with a surgical technique able to better reproduce the physiological, patient specific, knee biomechanics.
2. Materials and methods
Fifteen consecutive patients (8 female and 7 male) scheduled for a total knee replacement have been enrolled for this study and treated using a modern third generation knee implant with a medial congruent tibial polyethylene (Persona system, Zimmer Biomet, Warsaw, USA). Implants was performed by the same surgeon between March and April 2019. The mean age of patients included was 73,5 years (from 65 to 80) with an average BMI of 30,7 kg/m2 (from a minimum of 21.5 kg/m2 to a maximum of 36.3 kg/m2).
A primary advanced knee osteoarthritis was the diagnosis in all patients. Exclusion criteria were knee osteoarthritis secondary to rheumatoid arthritis, valgus deformity, patients with previous major surgical treatments around the knee.
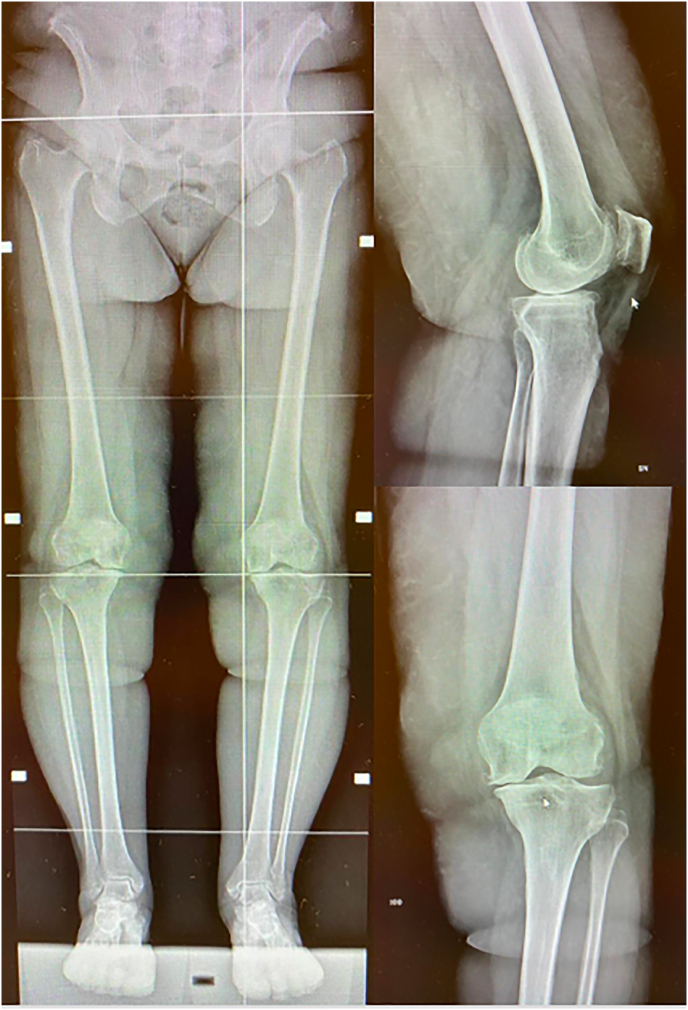
A standard anterior-posterior and lateral weight-bearing radiographs, a long-leg view of the lower extremities (Fig. 1) and a Marchant14 view of patellofemoral joint was performed in all patients preoperatively and at twelve months follow-up.
Fig. 1.
Pre-operative standard anterior-posterior and lateral weight-bearing radiographs and long-leg view of the lower extremities.
Intraoperatively, with the patient in supine position and spinal anesthesia, the surgical approach was performed thought a standard midline skin incision and a medial peri-patellar capsulotomy. Osteophytes were removed in order to restore ligament length motion and stability.15 Bone cuts were made according to the kinematic alignment surgical technique described by Howell16 using conventional instruments. The correct amount of bone and cartilage from the distal and posterior femur considering wear and saw blade thickness was removed to match femoral component size (9 mm). The intramedullary guide was not used and the location for the distal femoral cuts was selected manually placing the femoral guide on the lateral compartment and raising away from the medial according to the amount of wear which is typically 2 mm. An 8-mm distal resection on the unworn femoral condyle was performed according to the thickness of prosthesis components and measured with a caliper. On the worn side, 2 mm of cartilage loss have been considered in addition to amount of bone and saw blade kerf, so 6 mm was the amount of removed bone. Subsequently the femoral sizing guide was oriented with the conventional posterior reference and set at neutral rotation. The author made posterior femoral cuts with the same thickness as wear was negligible on the posterior femoral medial condyles in all cases enrolled.
The tibial resection was made checking the plane cut so that the worn side of the resected portion was thinner than the unworn compartment by the amount of wear with the slope determined neutral.
Extension and flexion gaps were assessed with FuZion TM tensor (Persona system, Zimmer Biomet, Warsaw, USA); the goal was to obtain a rectangular gap in extension and trapezoidal gap (more lateral laxity) in flexion according to KA alignment technique.
At this point, femoral and tibial components were fitted and the MC insert trial was used to evaluate the stability of the knee during all range of motion (ROM) with the patella reduced on the femoral groove. When a wide range of motion with a stable knee was restored the final MC tibial insert was introduced. Patella was replaced in all cases.
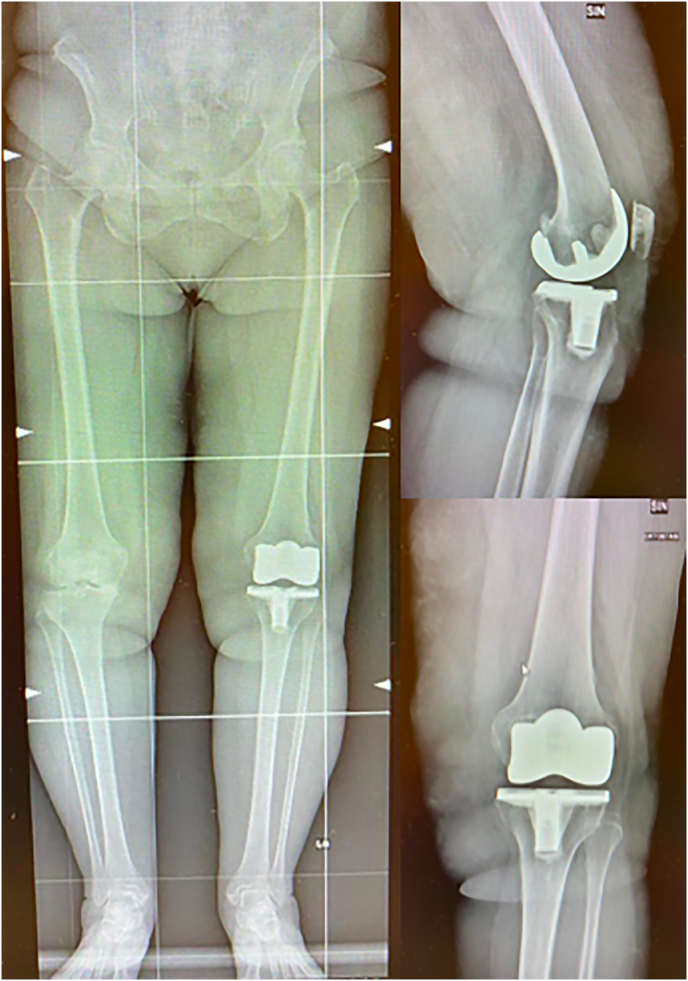
All patients followed a standard postoperative rehabilitation protocol including weight bearing as tolerated with crutches on post-operative day one and clinical improvements have been assessed pre-operatively at 6 and 12 months Follow up (FU) using the Oxford knee Score (OKS)12 the Knee Society Score (KSS)13 and Forgotten Joint Score (FJS)34 as patient reported outcomes measurement system (PROMs). A radiological evaluation was made by a single physician at 6 months (Fig. 2).
Fig. 2.
Post-operative standard anterior-posterior and lateral weight-bearing radiographs and long-leg view of the lower extremities.
3. Results
All patients were available for clinical and radiological evaluation at one year follow-up.
Average improvement in OKS was from 20.2 (SD 5.5) pre-operatively to 41.3 (SD 2.1) at the final FU. KSS pain/motion improved with a mean score from 40.1 (SD 4.0) pre-op to 89.1 (SD 6.3) while KSS function improved with an average score from 51.0 (SD 6.2) pre-op to 81.8 (SD 8.4) showing good to excellent results in all the knee treated. The mean FJS at 6 months follow up was 75.1 (SD 4.2) improving to 79.3 (SD 3.3) at one year FU (Table 1). Evaluating the maximum ROM at the final FU the average maximum active movement was 123° (SD 5.3) and none of the patients needing for a revision surgery or manipulation under anesthesia. No complications were observed at the final follow-up as septic or aseptic loosening or vascular or neurological injury.
Table 1.
Pre-operative values and early clinical results at 6 and 12 mounts follow-up.
| PRE-OPERATIVE (SD) | 6-MONTH FU (SD) | 12-MONTH FU (SD) | |
|---|---|---|---|
| OKS | 20.2 (5.5) | 40.3 (SD 3.1) | 41.3 (2.1) |
| FJS | 75.1 (4.2) | 79.3 (3.3) | |
| KSS PAIN/MOTION | 40.1 (4.0) | 87.1 (7.0) | 89.1 (6.3) |
| KSS FUNCTION | 51.0 (6.2) | 79.4 (9.3) | 81.8 (8.4) |
Post-operative XR showing an average varus Hip-Knee-Ankle (HKA) angle of 178.8° (range from 176° to 182°, SD 2,3°); We found no statistically significant difference between pre-operative and post-operative HKA (p < 0,05). No radiolucent lines were found in anterior-posterior and lateral view, none of the components was found to be radiologically loose. The patellofemoral view showed a correct position of the patellar articular surface on the femoral groove.
4. Discussion
In the early 1970s, when TKA was first introduced, available instrument precision was poor and implant failures were frequent.17 There were many difficulties to overcome, including implant fixation, joint instability, size match, and polyethylene wear. No wonder that the focus was primarily on implant survivorship, rather than reproducing normal knee function.18 To achieve this goals TKAs were implanted through mechanical alignment technique by performing a neutral femoral and tibial cut with fixed femoral rotation to create equal flexion and extension gaps using posterior stabilized (PS), cruciate retaining (CR) or mobile bearing (MB) implants.
However, recent studies have shown that the MA technique frequently results in significant anatomical modifications with a wide range of complex collateral ligament imbalances, which are not correctable by collateral ligament release.19 Therefore, it is unsurprising that this scenario may results in an unnatural gait20 and consequently in residual patients’ dissatisfaction.
Kinematic alignment technique was introduced as a possible solution. The KA purpose is to restore the pre-arthritic patient's constitutional knee alignment through a pure bone resection procedure with only exceptional ligament release, which has been shown to reliably position knee components.21 This technique allows the surgeon to align the implant in respect of three axis of rotation the natural knee moves through: the transverse axis in the femur about which the tibia flexes and extends, the transverse axis in the femur about which the patella flexes and extends and the longitudinal axis in which the tibia internally-externally rotates on the femur. Each axis is parallel or perpendicular to the natural joint line between the femur and tibia throughout the motion.16
This change of perspective clearly induced many surgeons to worry about leaving the prosthesis with some degree of varus or valgus. Despite KA tries to restore the 3D anatomy of the knee,18 malalignment can increase the risk of implant failure and varus alignment could be associated with decreased patient satisfaction. Keeping in mind these uncertainties and proceeding in a cautious manner due to our preliminary experience approaching KA; the current authors restricted their indication for patients with a small constitutional frontal limb deformity (≤5°) and a frontal joint line obliquity with less than 5° considered as a safe alignment zone.
In the literature, results on KA are encouraging: three RCTs22,23,24 and five meta-analyses25,7,26,31,32 have reported better early to long term clinical results with KA compared to MA TKAs.27 Although reported clinical outcomes of KA TKA are independent to the patient's anatomy reported in the published studies, it must be said that currently there are no clear evidence that all patients are suitable for kinematic alignment, especially those who have severe valgus, varus alignment or joint line obliquity.9 In our series, and this is one of the limits of our study, post-operative XR showed an average varus HKA of 178.8° (range from 176° to 182°, SD 2,3°) with no statistically significant difference with pre-operative HKA assessment. In this situation KA and “restricted KA” overlap: our present and future data won't help in management of severe coronal deformity.
Focusing on knee kinematic a recent gait analysis20 that compares CR KA and MA TKA with healthy controls, reported no significant differences between KA TKA end healthy control for sagittal plane range of motion, maximum flexion and abduction/adduction curves resulting in a well oriented joint line. This optimal orientation obtained on the sagittal and coronal plane are remarked by other studies focusing on patellar kinematic, better restored in the KA technique.29,30 Interestingly, these kinematic differences translated to a significantly better clinical outcome in the KA group.
On the other hand, they20 demonstrated a statistically significant difference in the axial plane motion of the gait cycle between KA TKR and healthy control. Focusing on this point, research by Pinskerova et al.13 has influenced our understanding of femoral condyle motion relative to the tibial surface throughout flexion in the axial plane. Now we know that the medial condyle works as a pivot, whereas the lateral condyle translates backwards by rolling and sliding about 20 mm, from 0° to 120°, resulting in the so called femoral “rollback” motion with flexion. This movement points out a significant difference from classic TKAs, which were designed before this knowledge of femoral kinematics was acquired. PS and CR designs showed a “paradoxical” anterior translation of both condyles in most cases, while mobile bearing designs have a central pivot point.18
Modern medial pivot (MP) TKA implants are designed trying to overcome this problem reproducing the physiological “medial pivoting” pattern with a greater conformity on the medial compartment and a less congruency on the lateral side. This design may be promising to help the KA TKR to freely reproduce the physiological knee motion on the transverse axes of rotation.
Results of MP TKR are variable and mainly focused on mechanical alignment technique. This implant seems to better reproduce healthy knee motion scoring higher results on the FJS,31 reducing the so called “mid flexion instability”32 and resulting in similar to better clinical outcomes when compared to PS and CR implants.8,33
In this paper, we combined a medial pivot third generation prosthesis design with a kinematic alignment technique in order to enhance their single potential: an implant designed to mimic the anatomical shape and motion of the native knee housed in a surgical technique able to better reproduce the physiological, patient specific, knee biomechanics.
The results are promising, we reported an improvement in OKS from 20.2 (SD 5.5) pre-operatively to 41.3 (SD 2.1) at the final FU. KSS pain/motion improved with an average score from 40.1 (SD 4.0) pre-op to 89.1 (SD 6.3) while mean KSS function improved from 51.0 (SD 6.2) pre-op to 81.8 (SD 8.4) showing good to excellent result in all the knee treated. Those results are consistent with major meta-analysis on KA in literature.7,23,25,28,30 The mean FJS at 6 months FU was 75.1 (SD 4.2) improving to 79.3 (SD 3.3) at one year FU: this result highlights a slightly faster recovery from surgery when compared to other studies in literature.32
To our knowledge there is only one paper that investigates association of KA technique and MP TKR and our results are consistent with it. French SR et al.35 compared KA MP with KA CR TKA at one year follow up: patients who underwent the MP-TKA scored significantly better on the FJS and the quality of life subscale of the KOOS and KOOS-12 than those who underwent a CR-TKA.
Our findings associated to the previously reported evidences suggest that at short-term follow-up, the MP TKA associated with a restricted KA technique is likely to allow a patient to “forget” that a joint has been replaced and restore their quality of life. This is of special importance in a background where the demand for primary TKA is expected to increase the most in young active patients.36
This study has some limitations. First, this is a prospective study enrolling a limited number of patients with no control group; second, the FU is short and limited to 12 months. More cases and a long-term FU might be necessary to confirm the value of this new design and eventual clinical improvements. Third, our preliminary clinical results should be confirmed with more objective methods: measurements using fluoroscopic evaluations, or a gait analysis study might be more appropriate to better support our preliminary clinical results.
5. Conclusions
Our findings suggest that combining MS implant with KA technique may results in better short-term functional results, helping the patient to “forget” their replaced joint and restoring their pre-arthritic quality of life. The authors know that we are far from a perfect TKA but we truly believe that a wise combination of recent available technology and surgical technique side by side with a constant advancement in TKA designs may lead to strong clinical improvements.
References
- 1.Gademan M.G.J., Hofstede S.N., Vliet Vlieland T.P.M., Nelissen R.G.H.H., Marang-van de Mheen P.J. Indication criteria for total hip or knee arthroplasty in osteoarthritis: a state-of-the-science overview. BMC Muscoskel Disord. Dec. 2016;17(1):463. doi: 10.1186/s12891-016-1325-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Risitano S., Indelli P.F. “Is ‘symmetric’ gap balancing still the gold standard in primary total knee arthroplasty? Ann Transl Med. 2017;5(16) doi: 10.21037/atm.2017.06.18. AME Publishing Company. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bourne R.B., Chesworth B.M., Davis A.M., Mahomed N.N., Charron K.D.J. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi Y.-J., Ra H.J. Patient satisfaction after total knee arthroplasty. Knee Surg Relat Res. Mar. 2016;28(1):1–15. doi: 10.5792/ksrr.2016.28.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schiraldi M., Bonzanini G., Chirillo D., de Tullio V. Mechanical and kinematic alignment in total knee arthroplasty. Ann Transl Med. 01-Apr-2016;4(7) doi: 10.21037/atm.2016.03.31. AME Publishing Company. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Indelli P.F., Risitano S., Hall K.E., Leonardi E., Migliore E. “Effect of polyethylene conformity on total knee arthroplasty early clinical outcomes,” Knee Surgery. Sport Traumatol Arthrosc. Apr. 2019;27(4):1028–1034. doi: 10.1007/s00167-018-5170-5. [DOI] [PubMed] [Google Scholar]
- 7.Lee Y.S., Howell S.M., Won Y.Y. “Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty,” Knee Surgery. Sport Traumatol Arthrosc. Nov. 2017;25(11):3467–3479. doi: 10.1007/s00167-017-4558-y. [DOI] [PubMed] [Google Scholar]
- 8.Sabatini L., Risitano S., Parisi G. Medial pivot in total knee arthroplasty: literature review and our first experience. Clin Med Insights Arthritis Musculoskelet Disord. 01-Jan-2018;11 doi: 10.1177/1179544117751431. SAGE Publications Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rivière C., Iranpour F., Auvinet E. Alignment options for total knee arthroplasty: a systematic review. Orthop Traumatol Surg Res. 2017 Nov;103(7):1047–1056. doi: 10.1016/j.otsr.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 10.Howell S.M., Kuznik K., Hull M.L., Siston R.A. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics. Sep. 2008;31(9):857–864. doi: 10.3928/01477447-20080901-15. [DOI] [PubMed] [Google Scholar]
- 11.Matsuda S., Matsuda H., Miyagi T., Sasaki K., Iwamoto Y., Miura H. Femoral condyle geometry in the normal and varus knee. Clin Orthop Relat Res. 1998;349:183–188. doi: 10.1097/00003086-199804000-00022. [DOI] [PubMed] [Google Scholar]
- 12.Ishikawa M., Kuriyama S., Ito H., Furu M., Nakamura S., Matsuda S. Kinematic alignment produces near-normal knee motion but increases contact stress after total knee arthroplasty: a case study on a single implant design. Knee. Jun. 2015;22(3):206–212. doi: 10.1016/j.knee.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 13.Pinskerova V., Johal P., Nakagawa S. Does the femur roll-back with flexion? J Bone Jt Surg Ser B. Aug. 2004;86(6):925–931. doi: 10.1302/0301-620x.86b6.14589. [DOI] [PubMed] [Google Scholar]
- 14.Merchant AC C.C., Mercer R.L., Jacobsen R.H. Roentgenographic analysis of patellofemoral congruence. J Bone Jt Surg Am. 1974;56:1391–1396. [PubMed] [Google Scholar]
- 15.Indelli P.F., Graceffa A., Baldini A., Payne B., Pipino G., Marcucci M. 2015. Clinical Study Relationship between Tibial Baseplate Design and Rotational Alignment Landmarks in Primary Total Knee Arthroplasty. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Howell M.M., Hull S.M., ML Kinematic alignment in total knee arthroplasty. Insa Scott Surg Knee. 2012:1255–1268. [Google Scholar]
- 17.Robinson R.P. “The early innovators of today's resurfacing condylar knees. J Arthroplasty. 2005;20(SUPPL. 1):2–26. doi: 10.1016/j.arth.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Vendittoli P.A., Blakeney W. Redefining knee replacement. J Orthop Traumatol: Surg Res. 01-Nov-2017;103(7):977–979. doi: 10.1016/j.otsr.2017.09.003. Elsevier Masson SAS. [DOI] [PubMed] [Google Scholar]
- 19.Gu Y., Roth J.D., Howell S.M., Hull M.L. How frequently do four methods for mechanically aligning a total knee arthroplasty cause collateral ligament imbalance and change alignment from normal in white patients? AAOS exhibit selection. J Bone Jt Surg Am. Jun. 2014;96(12) doi: 10.2106/JBJS.M.00306. e101(1) [DOI] [PubMed] [Google Scholar]
- 20.Blakeney W., Clément J., Desmeules F., Hagemeister N., Rivière C., Vendittoli P.A. “Kinematic alignment in total knee arthroplasty better reproduces normal gait than mechanical alignment,” Knee Surgery. Sport Traumatol Arthrosc. May 2019;27(5):1410–1417. doi: 10.1007/s00167-018-5174-1. [DOI] [PubMed] [Google Scholar]
- 21.Rivière C., Iranpour F., Harris S. The kinematic alignment technique for TKA reliably aligns the femoral component with the cylindrical axis. Orthop Traumatol Surg Res. Nov. 2017;103(7):1069–1073. doi: 10.1016/j.otsr.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 22.Calliess T., Bauer K., Stukenborg-Colsman C., Windhagen H., Budde S., Ettinger M. “PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study,” Knee Surgery. Sport Traumatol Arthrosc. Jun. 2017;25(6):1743–1748. doi: 10.1007/s00167-016-4136-8. [DOI] [PubMed] [Google Scholar]
- 23.Dossett K.B., HG, Estrada N.A., Swartz G.J., LeFevre G.W. A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results - PubMed. Bone Joint J. 2014;96-B(7):907–913. doi: 10.1302/0301-620x.96b7.32812. [DOI] [PubMed] [Google Scholar]
- 24.Matsumoto T., Takayama K., Ishida K., Hayashi S., Hashimoto S., Kuroda R. Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Jt J. May 2017;99B(5):640–646. doi: 10.1302/0301-620X.99B5.BJJ-2016-0688.R2. [DOI] [PubMed] [Google Scholar]
- 25.Courtney P.M., Lee G.C. Early outcomes of kinematic alignment in primary total knee arthroplasty: a meta-analysis of the literature. J Arthroplasty. 01-Jun-2017;32(6):2028–2032. doi: 10.1016/j.arth.2017.02.041. Churchill Livingstone Inc. e1. [DOI] [PubMed] [Google Scholar]
- 26.Li Y., Wang S., Wang Y., Yang M. Does kinematic alignment improve short-term functional outcomes after total knee arthroplasty compared with mechanical alignment? A systematic review and meta-analysis. J Knee Surg. 01-Jan-2018;31(1):78–86. doi: 10.1055/s-0037-1602136. Georg Thieme Verlag. [DOI] [PubMed] [Google Scholar]
- 27.Takahashi T., Ansari J., Pandit H.G. Kinematically aligned total knee arthroplasty or mechanically aligned total knee arthroplasty. J Knee Surg. Nov. 2018;31(10):999–1006. doi: 10.1055/s-0038-1632378. [DOI] [PubMed] [Google Scholar]
- 28.Yoon J.R., Han S.B., Jee M.K., Shin Y.S. Comparison of kinematic and mechanical alignment techniques in primary total knee arthroplasty. Medicine (United States) Sep. 2017;96(39) doi: 10.1097/MD.0000000000008157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Keshmiri A., Maderbacher G., Baier C., Benditz A., Grifka J., Greimel F. “Kinematic alignment in total knee arthroplasty leads to a better restoration of patellar kinematics compared to mechanic alignment,” Knee Surgery. Sport Traumatol Arthrosc. May 2019;27(5):1529–1534. doi: 10.1007/s00167-018-5284-9. [DOI] [PubMed] [Google Scholar]
- 30.Lozano R., Campanelli V., Howell S., Hull M. “Kinematic alignment more closely restores the groove location and the sulcus angle of the native trochlea than mechanical alignment: implications for prosthetic design,” Knee Surgery. Sport Traumatol Arthrosc. May 2019;27(5):1504–1513. doi: 10.1007/s00167-018-5220-z. [DOI] [PubMed] [Google Scholar]
- 31.Samy D.A., Wolfstadt J.I., Vaidee I., Backstein D.J. A retrospective comparison of a medial pivot and posterior-stabilized total knee arthroplasty with respect to patient-reported and radiographic outcomes. J Arthroplasty. May 2018;33(5):1379–1383. doi: 10.1016/j.arth.2017.11.049. [DOI] [PubMed] [Google Scholar]
- 32.Tsubosaka M., Ishida K., Kodato K. “Mid-flexion stability in the anteroposterior plane is achieved with a medial congruent insert in cruciate-retaining total knee arthroplasty for varus osteoarthritis,” Knee Surgery. Sport Traumatol Arthrosc. Mar. 2020:1–7. doi: 10.1007/s00167-020-05927-4. [DOI] [PubMed] [Google Scholar]
- 33.Nishio Y., Onodera T., Kasahara Y., Takahashi D., Iwasaki N., Majima T. Intraoperative medial pivot affects deep knee flexion angle and patient-reported outcomes after total knee arthroplasty. J Arthroplasty. 2014;29(4):702–706. doi: 10.1016/j.arth.2013.06.035. [DOI] [PubMed] [Google Scholar]
- 34.Carlson V.R., Post Z.D., Orozco F.R., Davis D.M., Lutz R.W., Ong A.C. When does the knee feel normal again: a cross-sectional study assessing the forgotten joint score in patients after total knee arthroplasty. J Arthroplasty. Mar. 2018;33(3):700–703. doi: 10.1016/j.arth.2017.09.063. [DOI] [PubMed] [Google Scholar]
- 35.French S.R., Munir S., Brighton R. A single surgeon series comparing the outcomes of a cruciate retaining and medially stabilized total knee arthroplasty using kinematic alignment principles. J Arthroplasty. Feb. 2020;35(2):422–428. doi: 10.1016/j.arth.2019.09.021. [DOI] [PubMed] [Google Scholar]
- 36.Niki Y., Nagura T., Kobayashi S., Udagawa K., Harato K. Who will benefit from kinematically aligned total knee arthroplasty? Perspectives on patient-reported outcome measures. J Arthroplasty. Feb. 2020;35(2):438–442. doi: 10.1016/j.arth.2019.09.035. e2. [DOI] [PubMed] [Google Scholar]