Abstract
Background
Hallux rigidus, or first metatarsophalangeal joing arthritis, is a very common condition which causes pain and loss of motion in the joing which can be debilitating.
Methods
Patient reported outcome measures were utilised to study the difference in day to day functionality between two common surgical management options for hallux rigidus.
Results
55 Cartiva and 23 Cheilectomy patients were included in this study. The Manchester Oxford Foot and Ankle Questionnaire revealed statistically significant improvements in the cheilectomy patients when compared to Cartiva SCI.
Foot and Ankle Ability Measure found no statistical difference was found between the two surgical treatments.
Conclusion
Cheilectomy offers good post-operative functional and sporting outcomes after surgery for the management of hallux rigidus at 5 years.
Keywords: PROMs, Cartiva, Cheilectomy, Hallux rigidus
1. Introduction
First metatarsophalangeal joint (FMTPJ) arthritis or hallux rigidus is a common condition affecting those over fifty years old.1 This vital joint in the gait mechanism can support 119% of a person's body weight.2 The first metatarsal head carries more than 50% of body weight during the push-off phase of gait and is largely responsible for the propulsive power during gait.3 It has a dramatic role in sporting activity and in day to day functionality.
Osteophyte formation, sclerosis and subchondral cyst formation in the joint will result in reduced range of motion, stifness and pain.4 Pain is often at its most during maximal range of motion of the joint, during the lift off phase of gait, which impacts most physical activities that involve dorsiflexion of the joint.5 Also commonly found is a dorsal prominence on the joint due to formation of bone spurs which can rub on footwear causing inflammation leading to significant discomfort and pain.4
Hallux rigidus is normally be managed non-operatively with shoe and lifestyle modifications before surgery. Currently the accepted surgical management of this condition is divided into joint sparing (cheilectomy, excision and interpositional arthroplasty) and joint sacrificing (arthrodesis) techniques.6 Joint sparing techniques, such as cheilectomy and interpositional arthroplasty have traditionally been utilised in the management of mild to moderate arthritis.6 [Fig. 1, Fig. 2, Fig. 3, Fig. 4] These techniques are usually used in the management of earlier stages of hallux rigidus, to provide effective pain relief while preserving some degree of movement of the joint. This can be very attractive to younger, more active adults who participate regularly in sports and physical activities or may want to continue to wear heeled footwear. It also allows for a compartively shorter healing time and can be further revised to arthrodesis in the future if necessary.7
Fig. 1.
Pre-operative foot X-ray of Cartiva SCI patient with Hattrup and Johnson severe hallux rigidus.
Fig. 2.
Post-operative foot X-ray of Cartiva SCI patient showing implant arthroplasty in situ in first metatarsal with adequate joint spacing.
Fig. 3.
Pre-operative foot X-ray of Cheilectomy patient with Hattrup and Johnson severe hallux rigidus.
Fig. 4.
Post-operative lateral foot X-ray of Cheilectomy patient with good surgical outcome.
Interpositional arthroplasty allows the patient to retain movement in the FMTPJ and provides effective pain relief. The Cartiva Synthetic Cartilage Implant (SCI) is a recently launched 10 mm × 10 mm polyvinyl alcohol implant which has similar biomechanical properties as normal human cartilage.8 Research is limited so far on the efficacy of this implant. The industry-funded originator series- Cartiva Motion study -is a randomised trial which showed statistically significant improvements in pain reduction and function at two and five years.9 Other previous arthroplasty implants made of silicone, metal, ceramic and other materials, had high failure rates due to loosening, material failure and subsidence with many falling into disrepute.10 As of yet there are no studies comparing the Cartiva SCI to other implants such as the Hemicap. There are also no studies comparing Cartiva SCI with Chilectomy.
Cheilectomy is a procedure first described by Nilsonne in 1930.11 Following this, there have been many different techniques described in the literature which have been modified over the years, mostly based off the DuVries technique in 1959.12 Cheilectomy involves resection of osteophytes at the dorsal metatarsal. Although the amount of bone to resect is debatable, most authors put the figure at 20–30% of the dorsal metatarsal head.12 Ultimately, the goal is to provide pain relief and to restore FMTPJ motion. Several studies have shown good functional patient reported outcomes following cheilectomy for hallux rigidus.13 Cheilectomy also restores a good amount of movement at the FMTPJ, which is important to patients who engage in sports and physical activities. Progression of arthritis after chilectomy is possible in the residual joint and revision surgery may be indicated in due course.
Patient reported outcome measures (PROMs) are the best method of evaluating the efficacy of surgical outcomes.14 Validated outcome measures such as the Manchester Oxford Foot and Ankle questionnaire (MOXFQ) allow the success of foot and ankle surgical interventions to be determined.15 The Foot and Ankle Ability Measure (FAAM) sports subscale16,17 is a PROMs tool to assess sporting and physical ability post-operatively.
The aim of this prospective comparative case series study is to analyse the efficacy of the Cartiva SCI interpositional arthroplasty verus Cheilectomy in the treatment of hallux rigidus utilizing PROMs.
2. Methods
Adult patients over 18 years of age at a single centre with symptomatic hallux rigidus who underwent primary Cartiva SCI implant interpositional arthroplasty or cheilectomy surgery were identified. Patients with previous surgery to the first metatarsal, hallux valgus with underlying arthritis were excluded.
FMTPJ arthritis was graded utilizing the Hattrup and Johnson (HJ) classification.16 It grades FMTPJ arthritis radiographically from one to three with one being mild arthritis and three severe arthritis with the presence of osteophytes, loss of joint space and sclerosis of the joint.
The MOXFQ was utilised to evaluate patient-reported outcomes at a minimum of one year post-operatively. It is a 16-item Patient Reported Outcome measure developed for use in studies assessing outcome following foot and ankle corrective surgery. It assesses three domains; Walking/Standing (7 items), Pain (5 items), and Social Interaction (4 items). The raw scale scores or Index score are converted into a metric scale from 0 to 100, with 100 indicative of being the most severe.
The FAAM sports subscale was used to assess sporting ability outcomes at a minimum of one year post-operatively. It consists of 8 questions; each question is scored from 0 to 4, 0 being the worst (unable to do) and 4 the best (no difficulties doing). When the activity in question is limited by something other than the patient's foot and ankle, they are able to answer not applicable (N/A).
The Mann-Whitney U two-tailed test was used to identify statistically significant results between the two groups as determined by a p value of <0.05.
3. Results
There were 55 adult patients who underwent a Cartiva SCI and 23 adult patients who underwent Cheilectomy surgery available for review for this study.
The Cartiva group was divided into 14 male and 41 female patients, with 37 right feet and 18 left feet. Patients were followed up for an average of 21 months (SD ± 6.0). 14 patients suffered from HJ grade 2/moderate arthritis and 41 patients with HJ grade 3/severe arthritis (Table 1).
Table 1.
Patient demographics.
| Group | Number of Patients | Age/Mean (min, max) | Follow up months/Mean (min, max, SD) | Gender | Foot | Hattrup and Johnson Grade |
|---|---|---|---|---|---|---|
| Cartiva | 55 | 56 (30, 80) | 21 (12, 38, SD ± 6.0) | 14 Male 41 Female |
37 Right 18 Left |
HJ 2 = 14 HJ 3 = 41 |
| Cheilectomy | 23 | 58 (38, 79) | 69 (50, 90, SD ± 10.9) | 4 Male 19 Female |
12 Right 11 Left |
HJ 1 = 5 HJ 2 = 10 HJ 3 = 8 |
The Cheilectomy group was divided into 4 male and 19 female patients, with 12 right feet and 11 left feet. Patients were followed up for an average of 69 months (SD ± 10.9). 5 patients suffered from HJ grade 1/mild arthritis, 10 with HJ grade 2/moderate and 8 patients with HJ grade 3/severe arthritis (Table 1).
The Cartiva group had a MOXFQ Index score of 27. The MOXFQ Domain scores demonstrated a Walking/Standing score of 29 points, Pain score of 28 points and a Social Interaction score of 24 points (Fig. 5).
Fig. 5.
Manchester Foot and Ankle Questionnaire (MOXFQ) scores for Cartiva and Cheilectomy.
The Cheilectomy group had a MOXFQ Index score of 14. The MOXFQ Domain scores demonstrated a Walking/Standing score of 7 points, Pain score of 27 points and a Social Interaction score of 8 points (Fig. 5).
There were statistically significant differences between the two groups (p > 0.05). The significant differences were notes in MOXFQ Index scores p = 0.01, Walking/Standing p = 0.0005 and Social Interaction p = 0.003 (Table 2).
Table 2.
Manchester Oxford Foot and Ankle questionnaire (MOXFQ) scores.
| Pain | Walking/Standing | Social Interaction | MOXFQ Index | |
|---|---|---|---|---|
| Cartiva SCI | 27.52 | 28.76 | 23.88 | 27.00 |
| Cheilectomy | 27.17 | 6.83 | 8.15 | 14.13 |
| Mann-Whitney p-value | 0.6818 | 0.00054 | 0.00308 | 0.01242 |
Pain outcome scores however was not significant (p = 0.7).
There were no differences when matching for age; <55 years old (p = 0.67) and >55 years old (p = 0.73) or for sex; male (p = 0.75) and female (p = 0.61). No statistical significant differences were shown when matching for severity of arthritis across all 3 HJ grades (p > 0.05).
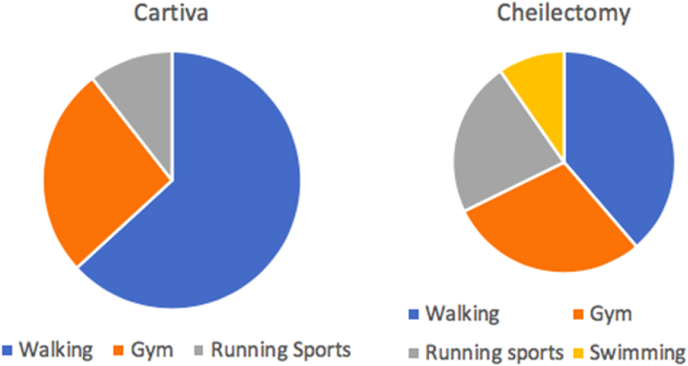
In both groups a small percentage of patients do not routinely participate in sporting activities and were therefore excluded from the FAAM sports assessment. In the Cartiva group 30 patients were included. These patients participate in Walking (19), Gym (8) and Running sports (3) (Fig. 6). In the Cheilectomy group 19 patients were included. These patients participate in Walking (8), Gym (6), Running sports (4) and Swimming (1) (Fig. 6).
Fig. 6.
Sporting activities for the Cartiva and Cheilectomy groups.
Mean post-operative FAAM Sports scores were 74.9% for Cartiva and 82.7% for Cheilectomy. Mann-Whitney U testing revealed no statistically significant difference between Cartiva and Cheilectomy (p = 0.11).
Recovery and return to function times were comparable with no statistical difference. No peripoerative complications, or revision surgery was required for any of the patients. Patient satisfaction with both techniques was high.
4. Discussion
The data from this study would seem to support that for mild to moderate stages of osteoarthritis (OA), the functional outcomes of Cheilectomy are better, even at longer follow-up times.
Comparing the functional outcomes for both procedures, Cheilectomy demonstrated significant improvement across all domains except for pain which was similar to Cartiva SCI. No patients in this group has required a revision surgery or fusion during the period of available follow up. These results suggest that cheilectomy is a viable long term option for mild to moderate hallux rigidus and that the Cartiva SCI in these patients may not offer any additional advantage.
A Chilecetomy is considered as a technically simpler and cheaper surgical procedure.
The early results for the Cartiva SCI form our cohort of patients are as expected from previous studies.9 The Cartiva motion study quotes FAAM sports score of 79.5 at 2 years which is comparable to our result of 74.9.9
In the case of Cheilectomy, there are other studies with long follow-up times which have shown similar results to our study.18,19 In these previous studies the post-operative MOXFQ Index scores ranged from 9.5 to 30.5 with follow-up times between 2 and 4 years.
When matching for ages or sex in our 2 cohorts of patients, there were no differences between the groups. The stage of arthritis was however more severe in the Cartiva group. It should be noted that 74% of the Cartiva group were HJ 3, while only 35% of the Cheilectomy group were HJ 3. We know that these patients will have poorer functional outcomes and therefore score less that HJ 1 or 2 patients. However, in terms of high impact sporting activities both groups scored equally highly with the majority of patients being able to participate in the sports of their choice.
Our outcome data supports the fact that Cartiva SCI can offer the same pain relief and a similar functional outcomes to Chilectomy across all grades of Hallux MTPJ arthritis. Cartiva SCI may also have a greater role in the more severe grades of FMTPJ OA.
We feel that the improved MOXFQ in Chilectomy patients with regards to walking/standing and social interaction could be due to the better range of movement in dorsofelexion a Chilectomy may offer in comparison to Cartiva SCI. No individual assesment of ROM was carried out as a part of this review.
This is the first comparative series from the same center compacting outcomes following Cartiva SCI and Chilectomy, demonstrating equivalent functional outcomes. This would suggest that longer follow up is required to study both the survivability, as well as the superiority of the implant and supports the efficacy of cheilectomy.
In our centre, Cartiva arthroplasty has become the first line treatment option for patients with hallux rigidus, the primary indication for cheilectomy is for dorsal impingement. We aim to explore the results of this study in more detail in future publications.
5. Limitations
This is a level 2 comparative study comparing two surgical management techniques for hallux rigidus. No pre-operative scores were taken so we cannot compare the relative improvements after surgery. The two groups were operated on by the same three surgeons at the same center which reduces bias between the two. Patients were not randomised or blinded, patients were assigned to either group based on patient and surgeon preference. Follow-up times vary between the two groups as the individual studies for each surgical technique took place at different time points. Larger cohort sizes are necessary, however this would likely require a multi-centre study to obtain a sufficient number of patients.
6. Conclusion
Cheilectomy offers good post-operative functional and sporting outcomes after surgery for the management of hallux rigidus at 5 years.
Cartiva SCI does not offer any advantage in the management of hallux rigidus in comparison with chielectomy.
More research with larger cohorts, across multiple centres by non-industry sponsored researchers is indicated in the future.
Funding received
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
None of the authors have conflicts of interest to disclose.
Contributor Information
Bernardo Brandao, Email: b.brandao@nhs.net.
Angus Hall, Email: angus.hall1@nhs.net.
Ahmed Aljawadi, Email: ahmed.aljawadi@doctors.org.uk.
Anna Fox, Email: anna.fox@mft.nhs.uk.
Anand Pillai, Email: anandpillai@nhs.net.
References
- 1.Gould N., Schneider W., Ashikaga T. Epidemiological survey of foot problems in the continental United States: 1978-1979. Foot Ankle. 1980;1(1):8–10. doi: 10.1177/107110078000100104. [DOI] [PubMed] [Google Scholar]
- 2.Jacob H.A. Forces acting in the forefoot during normal gait— an estimate. Clin Biomech. 2001;16(9):783–792. doi: 10.1016/s0268-0033(01)00070-5. [DOI] [PubMed] [Google Scholar]
- 3.Beertema W., Draijer W.F., van Os J.J., Pilot P. A retrospective analysis of surgical treatment in patients with symptomatic hallux rigidus: long-term follow-up. J Foot Ankle Surg. 2006 Jul-Aug;45(4):244–251. doi: 10.1053/j.jfas.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 4.Hamid K.S., Parekh S.G. Clinical presentation and management of hallux rigidus. Foot Ankle Clin. 2015 Sep;20(3):391–399. doi: 10.1016/j.fcl.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 5.DeFrino P.F., Brodsky J.W., Pollo F.E., Crenshaw S.J., Beischer A.D. First metatarsophalangeal arthrodesis: a clinical, pedobarographic and gait analysis studyFoot Ankle. Bar Int. 2002;23:496–502. doi: 10.1177/107110070202300605. [DOI] [PubMed] [Google Scholar]
- 6.Galois L., Hemmer J., Ray V. Eur J Orthop Surg Traumatol. 2019 doi: 10.1007/s00590-019-02528-x. [DOI] [PubMed] [Google Scholar]
- 7.Peace R.A., Hamilton G.A. End-stage hallux rigidus: cheilectomy, implant or arthrodesis? Clin Podiatr Med Surg. 2012;29:341–353. doi: 10.1016/j.cpm.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Baker M.I., Walsh S.P., Schwartz Z., Boyan B.D. A review of polyvinyl alcohol and its uses in cartilage and orthopedic applications. J Biomed Mater Res B Appl Biomater. 2012 Jul;100(5):1451–1457. doi: 10.1002/jbm.b.32694. [DOI] [PubMed] [Google Scholar]
- 9.Baumhauer J.F., Singh D., Glazebrook M. Prospective, randomized, multi-centered clinical trial assessing safety and efficacy of a synthetic cartilage implant versus first metatarsophalangeal arthrodesis in advanced hallux rigidus. Foot Ankle Int. 2016;37(5):457–469. doi: 10.1177/1071100716635560. [DOI] [PubMed] [Google Scholar]
- 10.Gross C.E., Hsu A.R., Lin J., Holmes G.B., Lee S. Revision MTP arthrodesis for failed MTP arthroplasty. Foot Ankle Spec. 2013;6(6):471–478. doi: 10.1177/1938640013502725. [DOI] [PubMed] [Google Scholar]
- 11.Nilsonne H. Hallux rigidus and its treatment. Acta Orthop Scand. 1930;1:295–302. [Google Scholar]
- 12.DuVries H.L. Mosby; St Louis (MO): 1959. Surgery of the Foot. [Google Scholar]
- 13.Smith S.M., Coleman S.C., Bacon S.A., Polo F.E., Brodsky J.W. Improved ankle push-off power following cheilectomy for hallux rigidus: a prospective gait analysis study. Foot Ankle Int. 2012 Jun;33(6):457–461. doi: 10.3113/FAI.2012.0457. [DOI] [PubMed] [Google Scholar]
- 14.Dawson J., Coffey J., Doll H. A patient-based questionnaire to assess outcomes of foot surgery: validation in the context of surgery for hallux valgus. Qual Life Res. 2006 Sep;15(7):1211–1222. doi: 10.1007/s11136-006-0061-5. [DOI] [PubMed] [Google Scholar]
- 15.Dawson J., Boller I., Doll H. The MOXFQ patient-reported questionnaire: assessment of data quality, reliability and validity in relation to foot and ankle surgery. Foot. 2011;21:92–102. doi: 10.1016/j.foot.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 16.Martin R.L., Irrgang J.J., Burdett R.G., Conti S.F., Van Swearingen J.M. Evidence of the validity of the foot and ankle ability measure (FAAM) Foot Ankle Int. 2005 Nov;26(11):968–983. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 17.Hattrup S.J., Johnson K.A. Subjective results of hallux rigidus following treatment with cheilectomy. Clin Orthop Relat Res. 1988;226:182–191. [PubMed] [Google Scholar]
- 18.Harrison T., Fawzy E., Dinah F., Palmer S. Prospective assessment of dorsal cheilectomy for hallux rigidus using a patient-reported outcome score. J Foot Ankle Surg. 2010;49:232–237. doi: 10.1053/j.jfas.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 19.Teoh, Kar Hao. Foot & Ankle International, U.S. National Library of Medicine; Feb. 2019. Clinical Outcomes Following Minimally Invasive Dorsal Cheilectomy for Hallux Rigidus.www.ncbi.nlm.nih.gov/pubmed/30282465 [DOI] [PubMed] [Google Scholar]