Abstract
Coronavirus disease 2019 (COVID-19) is a debilitating viral infection and, to date, 628,903 people have died from it, numbers that cannot yet be compared to the 50 million who died in the 1918 flu pandemic. As COVID-19 became better understood, cardiovascular manifestations associated with it were identified. This led to a complete healthcare restructuring with virtual clinics and changes to the triaging of critically ill patients. There are a lot of questions over how COVID-19 affects patients with heart failure (HF) as this condition is a leading cause of cardiovascular death. This review describes the cardiovascular implications of COVID-19 and new practices surrounding the use of telehealth to follow up and triage patients with HF. Current practices supported by medical societies, the role of angiotensin-converting enzyme inhibitors and, finally, a brief note regarding the management of advanced HF patients will also be discussed.
Keywords: COVID-19, heart failure, viral infection, cardiovascular manifestations, telehealth
This review focuses on the implications of coronavirus disease 2019 (COVID-19) in the heart failure (HF) population. First of all, we will describe the cardiovascular implications of COVID-19 and the new practices surrounding the use of telehealth to follow up and triage patients with HF. We will then discuss the current practices supported by medical societies, the role of pharmacotherapy and, finally, a brief note regarding the management of patients with advanced HF (Figure 1).
Figure 1: Heart Failure Patients and Coronavirus Disease 2019.
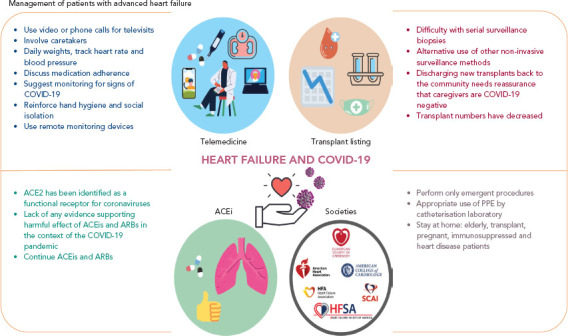
ACE2 = angiotensin-converting enzyme 2; ACEi = angiotensin-converting enzyme inhibitor; ARB = angiotensin 2 receptor blockers; COVID-19 = coronavius disease 2019; PPE = personal protective equipment.
COVID-19 and Cardiovascular Manifestations
COVID-19 is a debilitating viral infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and, to date, management is supportive, while off-label treatments are still under scrutiny and not yet supported by randomised controlled trials.[1] The symptoms of COVID-19 vary and may include cough, fever, shortness of breath, muscle aches, profound fatigue, dysgeusia, anosmia and diarrhoea.
COVID-19 can induce respiratory failure and subsequently acute respiratory distress syndrome (ARDS), which is the leading cause of mortality. The well-known cytokine storm is characterised by a hyperinflammatory syndrome resulting from a fulminant and often fatal hypercytokinaemia with multiorgan failure. Important features of the inflammatory response include unremitting haemophagocytic lymphohistiocytosis, pulmonary involvement (including ARDS) in approximately 50% of patients, increased interleukin (IL)-2, IL-7, granulocyte–colony-stimulating factor, interferon-gamma inducible protein 10, monocyte chemoattractant protein 1, macrophage inflammatory protein 1-alpha and tumour necrosis factor-alpha.[2,3]
Initial observations around COVID-19 were that it could cause organ failure. Approximately 85% of those infected are asymptomatic carriers, but a proportion will develop a severe condition and present to hospitals and some of them will require mechanical ventilation.[4,5] Initial data suggest that predisposing risk factors for COVID-19 mortality include cardiovascular comorbidities, such as hypertension and diabetes; however, the prevalence of HF in these patients is not well known. There is also little to no data on myocardial performance in hospitalised or non-hospitalised patients who acquired COVID-19. Reports indicate that some patients hospitalised with COVID have developed viral myocarditis and experienced thrombotic events and cardiac tamponade, but predisposing risk factors are unknown.[6,7,8]
Our knowledge of COVID-19 has progressed significantly in the last 3 months, initially from clinical cases and subsequently from large studies. Cardiology societies were the first to suggest protocols on how to visualise potential cardiac dysfunction and, importantly, on how to protect staff (Supplementary Tables 1 and 2).[9,10] The use of point-of-care ultrasound (POCUS) instead of a complete echocardiogram has also been suggested.[11]
Heart Failure Manifestation in COVID-19
There are reports describing the importance of endomyocardial biopsy and cardiac MRI in this population.[6,12]
Endomyocardial biopsy has identified diffuse T-lymphocytic inflammatory infiltrates (CD3+ >7/mm[2]) with huge interstitial oedema and limited foci of necrosis. No replacement fibrosis was detected, suggesting an acute inflammatory process.[11] There was also localisation of viral particles in the myocardium.[6]
Cardiac MRI has shown hypokinesis and diffuse myocardial oedema without evidence of late gadolinium enhancement.[12] Myocardial involvement and evidence of thrombosis have been recorded at autopsies but, because carrying these out poses risks to staff, hospital policies have restricted studies. There is a fine balance between scientific and clinical requirements and the occupational risk from exposure to SARS-CoV-2.
Given the above, COVID-19 seems to insult the cardiovascular system in multiple ways. HF triggered by respiratory failure is common, especially in patients with comorbidities. Viral myocarditis, thrombotic events, takotsubo myocarditis, complete heart block and tamponade have been reported as initial presentations of COVID-19.[7,12–15] Thrombotic events can include pulmonary embolism.[7]
In one of the first manuscripts on COVID-19 and cardiovascular effects, specifically myocardial injury, Rali et al. elegantly elaborated on the different manifestations of COVID-19, explaining the cytokine storm and the myocardial picture, as well as the thrombogenicity of the virus.[16]
As time allows bigger registries to be set up, we realised that impaired ventricular function as well as significant tricuspid regurgitation in patients with COVID-19 was associated with poor prognosis.[17] Lala et al. described the significant prevalence of myocardial injury in patients with COVID-19, despite low troponin levels.[18] Furthermore, they noted that, after adjusting for disease severity and relevant clinical factors, even small amounts of myocardial injury (e.g. troponin I 0.03–0.09 ng/ml; n=455; 16.6%) were significantly associated with death (adjusted HR 1.75; 95% CI [1.37–2.24]; p<0.001) while greater amounts (e.g. troponin I>0.09 ng/dl; n=530, 19.4%) were significantly associated with higher risk (adjusted HR 3.03; 95% CI [2.42–3.80]; p<0.001).[18]
Heart failure physicians have found themselves on the frontlines of this pandemic, as our patients are affected by this virus in novel ways and people with no cardiac history are developing a range of cardiac involvement. Specialists have been called upon to care for the influx of patients and radically modify well-established algorithms.
Value of Telemedicine in Heart Failure Patients Follow-up and Triage
Healthcare providers revisited disaster response policies for infectious disease outbreaks to incorporate telemedicine systems to address some of the unique challenges posed by COVID-19 (Figure 1).[19]
Within weeks, a few hospitals moved entirely into telehealth and, as a predicted second wave will affect the future of face-to-face visits, physicians indicate that telemedicine can and should be a future strategy for the majority of patients.
Telemedicine meets the needs of the majority of patients with HF, particularly those in rural or remote areas, those with limited mobility or financial or time constraints, and those with limited access to transportation.[20,21] These patients could remotely access services, seek expert advice and call nurses and specialists when needed – without the stress and opportunity cost of travel – and actively engage in and manage their care.[22]
Telemedicine in patients with HF may be challenging as those with New York Heart Association class II and III HF may need close follow-up. The priorities when managing these patients are following a healthy diet, measuring their weight daily and ensuring they are adhering to their medical management while at home. Most patients manage to weigh themselves daily and keep records of their blood pressure and heart rate. Furthermore, they are advised to have a low threshold for contacting the on-call physician, in case they experience shortness of breath or symptoms related to HF. HF specialist nurses coordinate with the physicians on risk stratification of patients and decide who will be followed up virtually. If a patient needs to be hospitalised, they are transferred to a COVID-19-negative ward with the highest level of precautions.
Patients with HF are expected to:
Learn how to use their smartphone or computer to participate in telehealth video visits.
Keep track of missed visits and investigations, and work with caregivers to reschedule appointments once social distancing measures are relaxed.
Practise good hand hygiene and social distancing, and stay at home as much as possible.
Follow recommendations regarding the routine use of face masks.
Avoid unreliable information on social media but consult advice from healthcare organisations, such as the NHS or the Centers for Disease Control, and their government’s daily reports for recommendations to follow.
Access prescriptions.
During video visits, simple manoeuvres can help to guide the patient in physical examination. These include digital pressure on the calf to assess for signs of lower extremity oedema, and neck examination while sitting to evaluate jugular venous pressure.
HF services rely on remote haemodynamic monitoring with CardioMEMS (Abbott), watches to track heart rate and remote interrogation of ICDs to analyse the burden of ventricular tachycardia or impedance for volume status to ascertain if therapy needs to be adjusted. The goal is to avoid hospitalisation.
People who are elderly or not technologically savvy may have problems using telemedicine, so there is a need for a robust structure that can synchronise calls and provide technological support and scheduling. This also poses a challenge for patients, as they may have difficulty navigating the system and limited access to healthcare providers. The routine channels have changed and we are constantly adapting to try to ensure patient safety.
Despite the above difficulties and limitations, the use of telemedicine keeps growing and it is recognised that our lives as caregivers will change completely as we apply telehealth wherever we can and as much as possible.
Role of Heart Failure Societies
The Heart Failure Society of America (HFSA) and the Heart Failure Association of the European Society of Cardiology have ensured that HF patients are appropriately informed during the novel COVID-19 pandemic.[10,11]
The British Heart Foundation has identified extremely vulnerable groups who need to stay at home:[23]
Those who have had a transplant at any time, including a heart transplant.
Immunosuppressed patients, such as those with cancer receiving chemotherapy or extensive radiotherapy.[11]
Those who are pregnant and have significant heart disease – defined as any of the following: coronary heart disease, hypertrophic cardiomyopathy, hypertensive heart disease, pulmonary arterial hypertension, moderate or severe valvular heart disease, HF that affects left ventricular function, or significant congenital heart (cyanotic) disease.
People who are elderly.
At the moment, there is no evidence that virus can be transmitted to patients upon insertion of implanted devices, such as pacemakers and ICDs; and no evidence that it causes infective endocarditis in those with valvular heart disease.[11]
Angiotensin-converting Enzyme inhibitors, COVID-19 and Heart Failure Patients
Angiotensin-converting enzyme 2 (ACE2) is a cornerstone of the cardiovascular and immune systems.[24] ACE2 has been identified as a functional receptor for coronaviruses, including SARS-CoV, as well as SARS-CoV-2. SARS-CoV-2 infection is triggered when the spike protein of the virus binds to ACE2, which is highly expressed in the heart and lungs.[24] SARS-CoV-2 mainly invades alveolar epithelial cells, resulting in respiratory symptoms. These symptoms are more severe in patients with cardiovascular disease, which might be associated with increased secretion of ACE2 in these patients compared with healthy individuals.
ACE2 is a homologue of angiotensin-converting enzyme (ACE). ACE2 negatively regulates the renin-angiotensin system by converting angiotensin II to vasodilatory angiotensin 1–7, diminishing and opposing the vasoconstrictor effect of angiotensin II. ACE2, ACE, angiotensin II and other renin-angiotensin-aldosterone system (RAAS) interactions are complex and, at times, paradoxical. In experimental studies, both ACE inhibitors and angiotensin II receptor blockers (ARBs) have been shown to limit severe lung injury in certain viral pneumonias, and it has been speculated that these agents could be beneficial in COVID-19.[24]
The Council on Hypertension of the European Society of Cardiology has highlighted the lack of evidence supporting the harmful effects of ACE inhibitors and ARBs in the context of the pandemic COVID-19 outbreak.[25] The Council on Hypertension strongly recommends that physicians and patients should continue treatment with their usual antihypertensive therapy because there is no clinical or scientific evidence to suggest that treatment with ACE inhibitors or ARBs should be discontinued because of COVID-19 infection.
Similarly, a joint HFSA, America College of Cardiology (ACC) and American Heart Association statement said there were no experimental or clinical data demonstrating beneficial or adverse outcomes with background use of ACE inhibitors, ARBs or other RAAS antagonists among COVID-19 patients with a history of cardiovascular disease treated with such agents.[26–28]
In addition, Vaduganathan et al. suggest withdrawing RAAS inhibitors may be harmful in certain high-risk patients with known or suspected COVID-19, and RAAS inhibitors may have a beneficial effect in patients with HF.[29]
Further evidence was provided in a retrospective cohort study of 4,480 patients with COVID-19, which showed that use of ACE inhibitors/ARBs was not significantly associated with COVID-19 diagnosis among patients with hypertension or with mortality or severe disease in patients diagnosed with COVID-19.[28]
Advanced Heart Failure: Durable Left Ventricular Assist Devices and Transplant Patients
Patients with a left ventricular assist device (LVAD) or who have had a heart transplant are a particularly challenging group to manage in the current pandemic.[29–33]
Patients with LVADs require frequent monitoring of anticoagulation levels, which requires blood draws in the laboratory or home monitoring if the person can do this. Additionally, the LVAD needs to be interrogated for any alarms and sometimes its speed may need to be adjusted, which cannot be done remotely. Furthermore, early in the postoperative period, LVAD patients may require in-person visits for assessment of surgical sites and echocardiograms to adjust pump speeds.[30] Early clinical case reports have highlighted how LVAD patients respond to the cytokine storm of COVID-19.[34,35]
Transplant patients pose other issues. Early in the postoperative period, patients undergo frequent routine endomyocardial biopsies and right heart catheterisations for surveillance for any signs of graft rejection. As many as 10 biopsies may be carried out in the first 6 months after a transplant, assuming a smooth postoperative course.
At the beginning of the pandemic, the ACC’s Interventional Council and the Society for Cardiovascular Angiography and Interventions suspended elective procedures in catheterisation laboratories to preserve resources and prevent patients being exposed to the hospital environment where COVID-19 may be more prevalent.[36] That said, the definition of elective requires clinical judgement as, in some cases, deferring a procedure may have deleterious effects, such as in the case of allograft rejection. Some institutions have adopted a very early transition to non-invasive surveillance of rejection using AlloMap (CareDx) and Allosure (CareDx) to minimise patient exposure to a hospital setting, which require just a blood draw.
It is also unclear how immunosuppression therapy plays a role in transplant patients’ vulnerability to COVID-19. If they do become infected, ideal immunosuppression management is not clear. Some have advocated reducing immunosuppression to allow the body to tackle the virus. Later in the course of the disease, it is believed that hyperactive immune responses are responsible for deleterious effects leading to ARDS, cardiac injury, cytokine release syndrome and multiorgan failure.[37,38] Ongoing trials are evaluating the effects of immunosuppression to improve outcomes for these patients.
In the US, at the first peak of the pandemic on 22 March 2020, the number of inactivations reached 85% in the transplant list.[32] By 21 June 2020, most of the patients had been reactivated and only 4–9% remain inactive due to COVID-19.
The Aftermath
We need to bear in mind that current clinical cases refer to hospitalised patients and a significant percentage of patients may exhibit mild symptoms and stay at home as per governmental recommendations. These patients may experience cardiovascular manifestations related to COVID-19 that may present later once the COVID-19 pandemic subsides. The other wave of admissions or complications that we will probably see are patients who stayed home with missed MIs, and those with a worsening HF functional class or underdiagnosed atrial or ventricular arrhythmias.
There are numerous efforts around the world to gather and report findings regarding COVID-19 and cardiovascular involvement, such as the CAPACITY-COVID registry.[36] We may need to rely on follow-up to see what the cardiovascular consequences, thrombotic concerns and possible lung impairment are for those who survive COVID-19.
Most importantly, healthcare systems are now prepared for the second wave of the pandemic, the extent of which of course we cannot predict.[37] However we are now prepared to protect our patients with HF as much as possible.
Supplementary materials
References
- 1.Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020;323:1824–36. doi: 10.1001/jama.2020.6019. [DOI] [PubMed] [Google Scholar]
- 2.Mehta P, McAuley DF, Brown M et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–4. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bai Y, Yao L, Wei T et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323:1406–7. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Day M. Covid-19: four fifths of cases are asymptomatic, China figures indicate. BMJ. 2020;369:m1375. doi: 10.1136/bmj.m1375. [DOI] [PubMed] [Google Scholar]
- 6.Tavazzi G, Pellegrini C, Maurelli M et al. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail. 2020;22:911–5. doi: 10.1002/ejhf.1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ullah W, Saeed R, Sarwar U et al. COVID-19 complicated by acute pulmonary embolism and right-sided heart failure. JACC Case Rep. 2020;2:1379–82. doi: 10.1016/j.jaccas.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Driggin E, Madhavan MV, Bikdeli B et al. Cardiovascular considerations for patients, health care workers, and health systems during the coronavirus disease 2019 (COVID-19) pandemic. J Am Coll Cardiol. 2020;5:2352–71. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Skulstad H, Cosyns B, Popescu BA et al. COVID-19 pandemic and cardiac imaging: EACVI recommendations on precautions, indications, prioritization, and protection for patients and healthcare personnel. Eur Heart J Cardiovasc Imaging. 2020;21:592–8. doi: 10.1093/ehjci/jeaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.British Society of Echocardiography. Clinical guidance regarding provision of echocardiography during the COVID-19 pandemic. 2020. https://bsecho.org/covid19 (accessed 24 July 2020)
- 11.Cheung JC, Lam KN. POCUS in COVID-19: pearls and pitfalls. Lancet Respir Med. 2020;8:e34. doi: 10.1016/S2213-2600(20)30166-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garot J, Amour J, Pezel T et al. SARS-CoV-2 fulminant myocarditis. JACC Case Rep. 2020;2:1342–6. doi: 10.1016/j.jaccas.2020.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Minhas AS, Scheel P, Garibaldi B et al. Takotsubo syndrome in the setting of COVID-19 infection. JACC Case Rep. 2020;2:1321–5. doi: 10.1016/j.jaccas.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kochav SM, Coromilas E, Nalbandian A et al. Cardiac arrhythmias in COVID-19 infection. Circ Arrhythm Electrophysiol. 2020;13:e008719. doi: 10.1161/CIRCEP.120.008719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dabbagh MF, Aurora L, D’Souza P et al. Cardiac tamponade secondary to COVID-19. JACC Case Rep. 2020;2:1326–30. doi: 10.1016/j.jaccas.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rali AS, Ranka S, Shah Z, Sauer AJ. Mechanisms of myocardial injury in coronavirus disease 2019. Card Fail Rev. 2020;6:e15. doi: 10.15420/cfr.2020.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rath D, Petersen-Uribe Á, Avdiu A Impaired cardiac function is associated with mortality in patients with acute COVID-19 infection. Clin Res Cardiol. 2020. epub ahead of press. [DOI] [PMC free article] [PubMed]
- 18.Lala A, Johnson KW, Januzzi JL Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol. 2020. epub ahead of press. [DOI] [PMC free article] [PubMed]
- 19.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382:1679–81. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 20.Poppas A, Rumsfeld JS, Wessler JD. Telehealth is having a moment: will it last? J Am Coll Cardiol. 2020;75:2989–91. doi: 10.1016/j.jacc.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.D’Amario D, Canonico F, Rodolico D et al. Telemedicine, artificial intelligence and humanisation of clinical pathways in heart failure management: back to the future and beyond. Card Fail Rev. 2020;6:e16. doi: 10.15420/cfr.2019.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ayebare RR, Flick R, Okware S et al. Adoption of COVID-19 triage strategies for low-income settings. Lancet Respir Med. 2020;8:e22. doi: 10.1016/S2213-2600(20)30114-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.British Heart Foundation. Coronavirus: what it means for you if you have heart or circulatory disease. Heart Matters 21 July 2020. https://www.bhf.org.uk/informationsupport/heart-matters-magazine/news/coronavirus-and-your-health (accessed 27 July 2020)
- 24.Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259–60. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.European Society of Cardiology. Position statement of the ESC Council on Hypertension on ACE-inhibitors and angiotensin receptor blockers. 2020. https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang (accessed 7 July 2020)
- 26.Heart Failure Society of America, American College of Cardiology and American Heart Association. HFSA/ACC/AHA statement addresses concerns re: using RAAS antagonists in COVID-19. 2020. https://www.acc.org/latest-in-cardiology/articles/2020/03/17/08/59/hfsa-acc-aha-statement-addresses-concerns-re-using-raas-antagonists-in-covid-19 (accessed 7 July 2020)
- 27.Patel AB, Verma A. COVID-19 and angiotensin-converting enzyme inhibitors and angiotensin receptor blockers: what is the evidence? JAMA. 2020. epub ahead of press. [DOI] [PubMed]
- 28.Fosbøl EL, Butt JH, Østergaard L et al. Association of angiotensin-converting enzyme inhibitor or angiotensin receptor blocker use with COVID-19 diagnosis and mortality. JAMA. 2020;324:168–77. doi: 10.1001/jama.2020.11301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vaduganathan M, Vardeny O, Michel T et al. Renin-angiotensin-aldosterone system inhibitors in patients with Covid-19. N Engl J Med. 2020;382:1653–9. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li F, Cai J, Dong N. First cases of COVID-19 in heart transplantation from China. J Heart Lung Transplant. 2020;39:496–7. doi: 10.1016/j.healun.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Imamura T. Therapeutic strategy for patients with coronavirus disease 2019 during left ventricular assist device supports. J Card Fail. 2020;26:479. doi: 10.1016/j.cardfail.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Latif F, Farr MA, Clerkin KJ Characteristics and outcomes of recipients of heart transplant with coronavirus disease 2019. JAMA Cardiol. 2020. epub ahead of press. [DOI] [PMC free article] [PubMed]
- 33.American Heart Association. Organ transplants make a turnaround from COVID-19 decline. 18 June 2020. https://www.heart.org/en/news/2020/06/18/organ-transplants-make-a-turnaround-from-covid-19-decline (accessed 7 July 2020)
- 34.Mahmood K, Rashed ER, Oliveros E et al. Predisposition or protection?: COVID-19 in a patient on LVAD support with HIV/AIDS. JACC Case Rep. 2020;2:1337–41. doi: 10.1016/j.jaccas.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chau VQ, Oliveros E, Mahmood K et al. The imperfect cytokine storm: severe COVID-19 with ARDS in patient on durable LVAD support. JACC Case Rep. 2020;2:1315–20. doi: 10.1016/j.jaccas.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Welt FGP, Shah PB, Aronow HD et al. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from the ACC’s Interventional Council and SCAI. J Am Coll Cardiol. 2020;75:2372–5. doi: 10.1016/j.jacc.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Linschoten M, Asselbergs FW. CAPACITY-COVID: a European registry to determine the role of cardiovascular disease in the COVID-19 pandemic. Eur Heart J. 2020;41:1795–6. doi: 10.1093/eurheartj/ehaa280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Argulian E. Anticipating the ‘second wave’ of health care strain in the COVID-19 pandemic. JACC Case Rep. 2020;2:845–6. doi: 10.1016/j.jaccas.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


