Abstract
Objective
To study whether a high volume injection without corticosteroids improves clinical outcome in addition to usual care for adults with chronic midportion Achilles tendinopathy.
Design
Patient and assessor blinded, placebo controlled randomised clinical trial.
Setting
Sports medicine department of a large district general hospital, the Netherlands.
Participants
80 adults (aged 18-70 years) with clinically diagnosed chronic midportion Achilles tendinopathy and neovascularisation on ultrasonography. 39 were randomised to a high volume injection without corticosteroids and 41 to placebo.
Interventions
Participants were instructed to perform an exercise programme for 24 weeks (usual care) combined with one 50 mL high volume injection of saline and lidocaine (intervention group) or one 2 mL placebo injection of saline and lidocaine (placebo group) at baseline.
Main outcome measures
Primary outcome was pain and function assessed using the validated Victorian Institute of Sports Assessment-Achilles (VISA-A) questionnaire at 24 weeks (analysed using a generalised estimation equations model). Secondary outcomes were patient satisfaction, return to sport, degree of ultrasonographic Doppler flow, visual analogue scale on 10 hop test, power and flexibility of the gastrocnemius and soleus muscles, pain detect questionnaire for neuropathic pain, and pain coping inventory. Participants were evaluated at baseline and at 2, 6, 12, and 24 weeks.
Results
Only one participant (1%) was lost to follow-up. The estimated mean VISA-A score improved significantly, from 40.4 (95% confidence interval 32.0 to 48.7) at baseline to 59.1 (50.4 to 67.8) at 24 weeks in the high volume injection group and from 36.9 (27.1 to 46.8) to 58.5 (47.9 to 69.1) in the placebo group. The VISA-A score over time did not differ between the groups (adjusted between group difference at 24 weeks 0.5 points, 95% confidence interval −17.8 to 18.8). No significant between group differences were found for patient satisfaction (21/37 (57%) v 19/39 (49%) patients, P=0.50) and return to desired sport (15/29 (52%) v 19/31 (61%) patients active in sports, P=0.65) at 24 weeks. None of the other secondary outcomes differed between the two groups.
Conclusions
A high volume injection without corticosteroids in addition to usual care is not effective for symptom reduction in patients with chronic midportion Achilles tendinopathy. On the basis of our findings, we cannot recommend the use of a high volume injection in this patient group.
Trial registration
ClinicalTrials.gov NCT02996409
Introduction
Chronic disorders of the Achilles tendon (tendinopathy) are a common overuse injury seen in general practice, with an incidence rate of 2-3 per 1000 registered adult patients.1 Most (74%) of these patients have midportion Achilles tendinopathy.2 Runners are most at risk of developing symptoms, with a lifetime risk of 52%.3 The initial treatment of Achilles tendinopathy is exercise combined with load management.4 Despite initiation of treatments, two thirds of patients continue to have symptoms at one year follow-up.5 At 10 years follow-up, about a quarter of patients still have symptoms.5 6 About one third of these non-responders eventually require surgery.4 7 Therefore, effective conservative treatment options are necessary to improve the outcome of patients with chronic Achilles tendinopathy who fail to respond to initial exercise treatment.
The formation of blood vessels (neovascularisation) around and within the tendon is one of the features of chronic Achilles tendinopathy. Neovascularisation can be identified in 50-100% of patients with tendon symptoms using Doppler ultrasonography, compared with 0-30% in asymptomatic patients.8 9 10 11 12 The infiltration of nerve structures alongside this neovascularisation has been suggested to play a role in the chronicity of pain from Achilles tendinopathy.13 14 A large study showed an association between the degree of ultrasonographic Doppler flow and patient reported severity of symptoms.8
Consequently, treatments have been developed to target neovascularisation. A novel technique is high volume injection, in which a large amount of fluid is injected into the area surrounding the tendon with the aim of obliterating peritendinous and intratendinous neovascularisation from high mechanical pressure.14 Current debate is on the addition of corticosteroids to the injection mixture. Recent evidence shows that a high volume injection with corticosteroids is associated with superior short term improvement at 6-12 weeks compared with a high volume injection without corticosteroids, but intermediate term effects are similar.15 Several cohort studies and one small randomised controlled trial found that a high volume injection (both with and without corticosteroids) resulted in decreased pain and improved function in the short term (6-12 weeks).14 16 17 18 19 As a consequence, this treatment is increasingly being used in the clinical setting although its effectiveness has not been tested in a large well designed study. In this study, we compared the effect of a high volume injection without corticosteroids with a placebo injection (both combined with an exercise programme) on pain and functional outcome at 24 weeks in patients with chronic midportion Achilles tendinopathy.
Methods
Study design and participants
This study was conducted as a stratified, patient and assessor blinded, placebo controlled randomised clinical trial, with 1:1 allocation ratio, at the sports medicine department of a large district general hospital (Haaglanden Medical Centre, The Hague, Netherlands). The study was announced through letters to healthcare professionals, presentations at national conferences, and information on a national sports medicine platform. Potentially eligible participants were identified from referrals by healthcare providers and self-referrals, thereby comprising a mix of patients with and without primary care from healthcare providers. The coordinating researcher (AvdV) provided participants with detailed information on the study. Participants were screened for eligibility by telephone and online (using a pain map). A sports medicine physician (RvO) evaluated potentially eligible participants for inclusion at a booked appointment. Participants provided written informed consent before inclusion.
We included patients if they were aged 18-70 years, had a painful swelling of the Achilles tendon 2-7 cm proximal to the insertion on the calcaneus, had had symptoms for at least two months, had an unsatisfactory outcome after a six week exercise programme, and had detectable Doppler flow. When symptoms were bilateral, participants selected the most severely affected tendon for treatment. All the participants performed a minimum of six weeks of exercise treatment before inclusion.
Patients were excluded if they had a history of an Achilles tendon rupture or surgery; were unable to perform the exercise programme, were engaged in concomitant treatment programmes, had sural nerve disease, had recent drug use (within two years) with putative effect on symptoms and tendon healing (quinolone antibiotics, corticosteroids), were suspected of having other musculoskeletal disorders clinically (insertional Achilles tendinopathy, plantar flexor tenosynovitis, peroneal subluxation, inflammatory internal disorders, or quinolone, corticosteroid, or statin induced tendinopathy), had a medical condition that would affect the safety of the participant when using the injection (eg, peripheral vascular disease, use of anticoagulant drugs, allergy for lidocaine), or were pregnant.
Procedures
One researcher (AvdV) prepared five 10 mL syringes (total volume 50 mL) for each patient. These syringes contained a mixture of 8 mL 0.9% sodium chloride solution (saline) and 2 mL 1% lidocaine (B Braun; Melsungen, Germany). Before and directly after injection, we used a Pro Focus Type 2202 (BK Medical; Herlev, Denmark) with a 5-12 MHz linear probe type 8811 to perform ultrasonography. The area of maximum Doppler flow was detected using power Doppler ultrasonography with predefined settings determined before the start of the study (mechanical index 1.28, thermal index 1.2, pulse repetition frequency 1.0 kHz, and gain 50%).20 We recorded the presence of intratendinous and peritendinous Doppler flow immediately after the injection. A blinded observer evaluated the presence of Doppler flow on these records to verify the success of the procedure after the trial had ended. These results had no consequences on the injection procedure—that is, no second injection was performed if Doppler flow was still present after the high volume injection. Complications and co-interventions were registered at each visit. All participants received daily compliance logs to complete for evaluation of adherence to the exercise programme. The participants were asked to upload these logs digitally every week. Reminders were sent to non-responders after five days.
Randomisation and masking
We used stratification for pre-injury activity level, since this could be a confounder for the primary outcome of pain and functional activity level using the Victorian Institute of Sports Assessment-Achilles (VISA-A) questionnaire.21 Stratification was conducted using the ankle activity score, which quantifies ankle related activity based on type and level of activities.22 Participants with an ankle activity score of 4 points or more were considered to be active and those with a score of 3 points or less were considered to be sedentary.23 Participants were randomised using a computer generated randomisation list (Microsoft Access; Redmond, WA). To ensure a balance between the number of participants in each treatment group, we performed block randomisation, with a variable block size of 4-10. To ensure blinding of the outcome assessor (AV), a secretary performed the randomisation who was independent of the researchers responsible for enrolment or the assessment of outcome measures. After randomisation, an unblinded sports medicine physician (RvO) who was not involved in the assessment of outcome measures carried out the allocated injection treatment. The participants were blinded to their assigned treatment, as they could not see the injection procedure. All the participants completed a short questionnaire immediately after the injection to check whether the blinding procedure was successful (which type of injection do you think you have received (high volume injection or placebo)?) and to assess the amount of pain (visual analogue scale 0-100, using a 100 mm line) during the procedure.
Interventions
High volume injection—Participants were placed in the prone position on the examination table with the affected ankle hanging over the edge. To ensure blinding, participants were asked not to turn their head during the injection procedure. The sports medicine physician inserted a 21 gauge and 40 mm long needle from the medial side of the ankle between the anterior aspect of the Achilles tendon and the anteriorly located Kager’s fat pad. The needle was attached to a connecting tube of 30 cm with Luer taper (Argon MC; Frisco, TX) to attach the syringes on the other side. The first syringe with the saline and lidocaine mixture (10 mL) was injected at the area of maximum Doppler flow. The following four syringes (10 mL each) were injected 1-2 cm proximal, distal, medial, and lateral, with coverage of the whole width of the tendon under real-time ultrasonography. The injection technique was identical to that described previously.14 Materials were stored in an opaque box to ensure blinding of the participants after the injection. The participants remained prone on the examination table for 5-7 minutes after the procedure.
Placebo injection—The placebo injection involved a similar technique, mixture, and duration as for the high volume injection. The only difference was the amount of injected fluid. Except for the third syringe, only 0.5 mL of each of the five syringes was injected at the different injection locations in the placebo group. The third syringe was attached to the connecting tube and the needle was localised at the injection site, but no fluid was injected. Therefore, 2 mL of the saline and lidocaine mixture was injected in total. To ensure blinding, the participants were unaware of the amount of injected fluid and type of procedure used for either treatment group. The participants were advised to refrain from strenuous walks and sports activities during the first 24 hours after the injection.
Exercise programme
The blinded outcome assessor (AV) instructed all the participants to perform a daily calf muscle exercise programme using detailed written information and videos. The exercise programme was based on an existing protocol, consisting of three consecutive phases: isometric exercises, concentric exercises, and eccentric exercises.24 25 The participants were asked to start the next phase if exercises could be performed for one week with acceptable symptoms (visual analogue scale score of ≤3/10 in activities and in daily life). If eccentric exercises could be performed without problems for at least one week, the participants continued with the return to sports module. This module consisted of four phases: simple plyometric exercises, fast plyometric exercises, a gradual increase in running, and interval training (if necessary for the type of sports). Web appendix 1 provides detailed information on the exercise programme and return to sport module.
All the participants were advised to refrain from weightbearing sporting activities for at least five weeks. The exercises and activities should be performed with only mild pain (maximum score of 3 on a scale from 0 to 10, with 0 indicating no pain and 10 maximum pain), and the participants were advised to decrease the activity level when the pain increased to more than 3 points during or after the activity or when morning stiffness increased one day after the activity compared with the previous days.24 The participants were then instructed to decrease their activity until symptoms had returned to an acceptable level. They were discouraged from using other treatments for their Achilles tendinopathy.
Outcome measures
The primary outcome measure was the Dutch version of the VISA-A questionnaire.26 This validated and disease specific questionnaire quantifies pain and activity levels,27 with scores ranging from 0 to 100: 100 indicates no pain with full activity level, with the score decreasing with increasing severity of symptoms. Secondary outcomes were patient satisfaction, return to sport, degree of ultrasonographic Doppler flow, visual analogue scale on 10 hop test, power and flexibility of the gastrocnemius and soleus muscles, pain detect questionnaire, and pain coping inventory. Patient satisfaction was scored as moderate or poor or as excellent or good. Return to sport was scored as no return to the desired sport or return to the desired sport (regardless of reaching pre-injury level). All outcome measures were assessed at baseline (before intervention) and at 2, 6, 12, and 24 weeks.
Statistical analysis
Our sample size calculation showed that 40 participants were required in each group to detect a difference of 12 points on the VISA-A score (power 0.80, two sided significance level of 0.05, SD 18, and accounting for a 10% loss to follow-up).23 28 29 A researcher (AvdV) performed the statistical analyses under the supervision of a biomedical statistician (JW); both were blinded to the allocated treatment. Data were analysed on an intention-to-treat basis using SPSS 25.0.0.1 (SPSS, Chicago, IL). Normality of the data was checked visually with Q-Q plots and statistically using the Shapiro-Wilk test. Between group differences for the primary outcome were analysed using a generalised estimation equations model. To test whether the time course of the VISA-A score was different between groups we added the interaction term of treatment group×time point. Adjustments were made for the four predefined baseline variables of age, sex, body mass index, and duration of symptoms. Additionally, we adjusted for the stratification factor (ankle activity score).30 Outcomes of the generalised estimation equations model are presented as estimated means, unless otherwise stated. The same method was used to evaluate most of the secondary outcomes (see web appendix 2). A Fisher’s exact test was used to evaluate only patient satisfaction, return to sport, and the patient acceptable symptom scale. The outcomes to evaluate the success of the procedures were analysed using a Fisher’s exact test or χ2 test (categorical outcomes) or unpaired t test or Mann-Whitney U test (continuous outcomes). We considered differences of P<0.05 to be statistically significant. Missing data were not imputed, but we would have carried out sensitivity analyses if missing data exceeded 5%.
Patient and public involvement
Patients were not involved in defining the research question. Two patients participated in a pilot test round to evaluate the impact of the placebo and high volume injection procedure. Patients were not involved in other aspects of the study design. After completion of the trial, all trial participants were contacted to evaluate relevant outcome measures and the burden of participation to improve future trials. Five participants took part in a patient meeting to discuss these items. Study results will be disseminated to the trial participants by email or letter.
Results
From December 2016 to January 2019, 185 patients with posterior ankle pain were screened for eligibility. After exclusions 80 participants were included in the study and randomised to either a high volume injection without corticosteroids or a saline injection (placebo group). At the 24 week endpoint, only one participant was lost to follow-up (1%). Figure 1 shows the flow of participants through the trial. No differences in baseline characteristics were found between the groups, except for the presence of bilateral symptoms (table 1). A higher proportion of participants in the high volume injection group had bilateral symptoms (17/39 (44%) v 11/41 (27%)). An additional analysis using a generalised estimation equations model was done to correct for the variable unilateral or bilateral symptoms.
Fig 1.
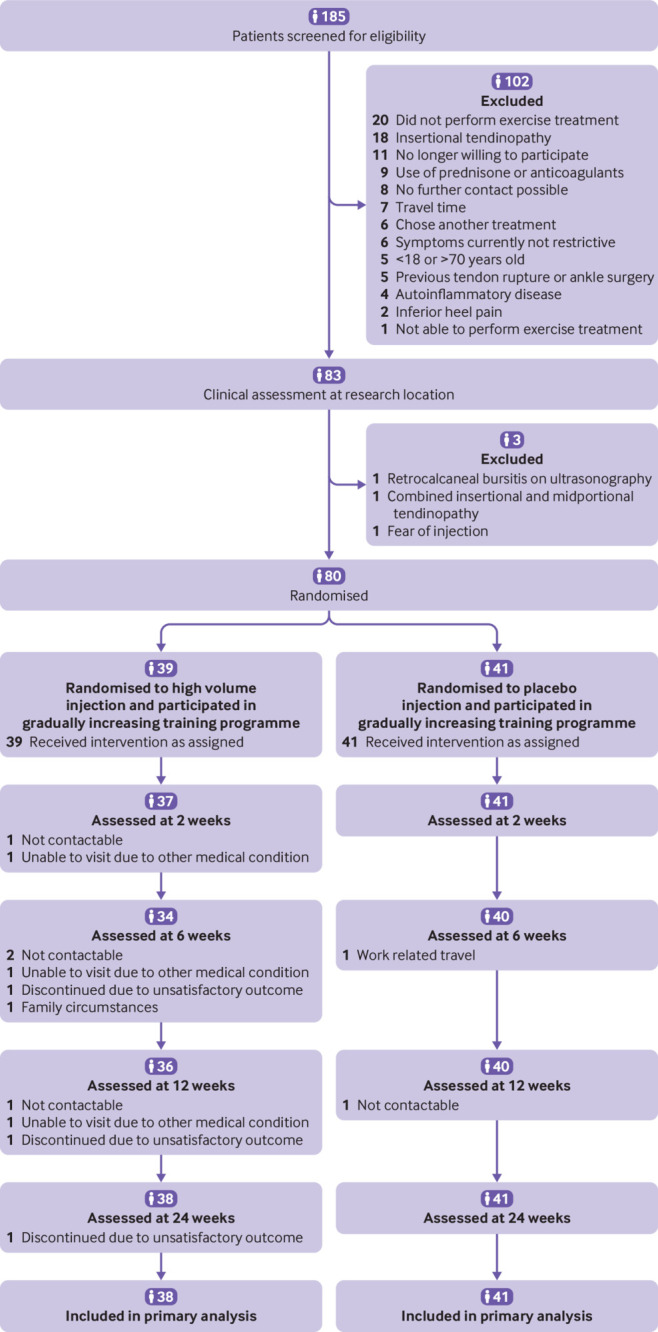
Flow of participants through study
Table 1.
Baseline characteristics of adults with chronic midportion Achilles tendinopathy assigned to a high volume injection without corticosteroid or placebo injection. Values are numbers (percentages) unless stated otherwise
| Characteristics | High volume injection group (n=39) | Placebo injection group (n=41) |
|---|---|---|
| Mean (SD) age (years) | 46.9 (8.1) | 48.9 (9.9) |
| Men | 17 (44) | 22 (54) |
| Mean (SD) body mass index | 26.8 (5.7) | 27.6 (5.1) |
| Activity level*: | ||
| Active in sports | 31 (79) | 33 (80) |
| Sedentary | 8 (21) | 8 (20) |
| Participation in desired sport (total hours per week) | 3.9 (2.0) | 4.9 (3.6) |
| Affected side: | ||
| Unilateral, left/right | 11/11 (56) | 15/15 (73) |
| Bilateral | 17 (44) | 11 (27) |
| Median (interquartile range) duration of symptoms (weeks) | 64 (17-112) | 60 (14-107) |
| Mean (SD) VISA-A score | 44.4 (15.5) | 41.0 (16.0) |
| Interventions at study start: | ||
| None | 24 (62) | 19 (46) |
| Night splint | 1 (3) | 0 (0) |
| Foot orthoses | 10 (26) | 18 (44) |
| Pain killers | 1 (3) | 4 (10) |
| Others | 3 (8) | 1 (2) |
| Doppler flow: | ||
| Intratendinous | 33 (85) | 37 (90) |
| Peritendinous | 6 (15) | 4 (10) |
VISA-A=Victorian Institute of Sports Assessment-Achilles.
Determined using the ankle activity score. Participants who scored ≥4 points were considered to be active in sports (starting from physical work). Participants who scored ≤3 points were considered to be sedentary (cycling, equestrian, or less activity). Level of sport and sports participation is only presented for the active group.
Outcome measures
VISA-A score—In the high volume injection group the estimated mean VISA-A score improved from 40.4 (95% confidence interval 32.0 to 48.7) at baseline to 59.1 (50.4 to 67.8) at 24 weeks and in the placebo group from 36.9 (27.1 to 46.8) to 58.5 (47.9 to 69.1). The interaction term treatment group×time point was not statistically significant (P=0.42), meaning that the VISA-A score did not differ over time between the groups. The adjusted between group difference in VISA-A score at 24 weeks was 0.5 (95% confidence interval −17.8 to 18.8) in favour of the high volume injection group (table 2). Improvement in VISA-A score was not significant at two weeks for either group. VISA-A scores improved significantly in both groups at six weeks (P=0.05) and at 12 and 24 weeks (P<0.01). Figure 2 presents the raw changes in VISA-A scores. In the sensitivity analysis using the additional generalised estimation equations model to correct for unilateral or bilateral symptoms, the results for the primary outcome (interaction term treatment group×time point, P=0.44) remained unchanged.
Table 2.
Primary and secondary outcome measures in adults with chronic midportion Achilles tendinopathy assigned to a high volume injection without corticosteroid or placebo. Values are numbers (percentages) unless stated otherwise
| Outcome measures | High volume injection group (n=39) | Placebo injection group (n=41) | Adjusted between group difference |
|---|---|---|---|
| Primary outcome | |||
| Estimated mean (95% CI) VISA-A score at follow-up (weeks)*: | |||
| 2 | 41.4 (33.7 to 49.1) | 38.2 (28.3 to 48.1) | 3.2 (−11.2 to 17.5) |
| 6 | 43.3 (34.6 to 52.0) | 46.1 (35.7 to 56.6) | −2.8 (−18.9 to 13.3) |
| 12 | 50.9 (42.3 to 59.5) | 49.6 (39.3 to 60.0) | 1.3 (−14.7 to 17.3) |
| 24 | 59.1 (50.4 to 67.8) | 58.5 (47.9 to 69.1) | 0.5 (−17.8 to 18.8) |
| Secondary outcomes | |||
| Patient satisfaction†: | |||
| Moderate or poor | 16 (43) | 20 (51) | |
| Excellent or good | 21 (57) | 19 (49) | |
| Return to sport‡: | n=29 | n=31 | |
| No return to sport | 9 (31) | 7 (23) | |
| Returned to sport, but not to desired type | 5 (17) | 5 (16) | |
| Returned to desired sport, but not at pre-injury level | 11 (38) | 14 (45) | |
| Returned to desired sport at pre-injury level | 4 (14) | 5 (16) | |
VISA-A=Victorian Institute of Sports Assessment-Achilles.
Scores and adjusted between group differences were calculated using a generalised estimation equations model with adjustments for predefined baseline variables: age, sex, body mass index, duration of symptoms, and ankle activity score. Positive values favour the high volume injection group. No statistically significant differences were found between the treatment groups at any time point.
For analysis purposes, good or excellent patient satisfaction was dichotomised as “satisfied,” and a poor or moderate satisfaction as “dissatisfied.” Two patients in each group did not return the questionnaire in which patient satisfaction was assessed. No statistically significant differences were found between the treatment groups at 24 weeks (P=0.50).
Number represents the proportion of participants who were active in sports before the study start (n=31 in the high volume injection group and n=33 in the placebo injection group). Two patients in each group did not return the questionnaire in which return to sport was assessed. Return to sport was dichotomised as “no return to desired sport” (no return to sport or return to sport, but not in the desired sport) or “return to desired sport” (regardless reaching pre-injury level). No statistically significant differences were found between both treatment groups at 24 weeks (P=0.65).
Fig 2.
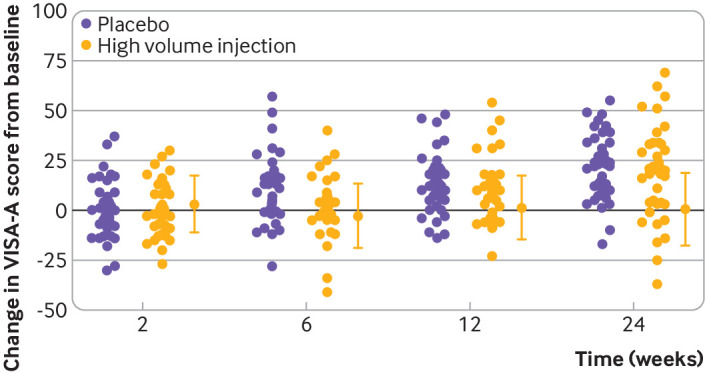
Between group differences in Victorian Institute of Sports Assessment-Achilles (VISA-A) score from baseline in participants treated with a high volume injection without corticosteroids or a placebo injection at 2, 6, 12, and 24 weeks. Whiskers represent 95% confidence intervals
Patient satisfaction—No significant difference was found in patient satisfaction between the treatment groups at 24 weeks (P=0.50). In the high volume injection group, 21/37 patients (57%) reported an excellent or good outcome compared with 19/39 (49%) in the placebo group.
Return to desired sport—No significant difference was found for return to the desired sport at 24 weeks (P=0.65). In the high volume injection group, 15/29 (52%) patients returned to their desired sport compared with 19/31 (61%) in the placebo group. Of these participants, only 4/29 (14%) returned to their pre-injury level in the high volume injection group and 5/31 (16%) in the placebo group.
Web appendix 2 shows the results of the other secondary outcome measures. No significant between group differences were found for any of these outcome measures.
Success of procedures
Success of injection procedure on Doppler flow—In participants with intratendinous Doppler flow before the injection procedure (n=33 in the high volume injection group and n=37 in the control group; table 1), Doppler flow was no longer detectable inside the Achilles tendon in 26/33 patients (79%) in the high volume injection group compared with 11/37 patients (30%) in the control group (P<0.001). The disappearance of Doppler flow after the high volume injection did not appear to influence the course of the VISA-A score over time compared with the presence of Doppler flow after the high volume injection (P=0.99), as explained in detail in web appendix 4.
Success of patient blinding—In the high volume injection group, 25/39 patients (64%) correctly thought they had received the high volume injection. In the placebo group, 22/41 patients (54%) correctly thought they had received the placebo injection (P=0.36).
Complications and pain during injection procedure—No complications (infections, haematomas, or tendon ruptures) were reported during the study period. The median pain score (visual analogue scale score 0-10) during the injection procedure was 6.0 (interquartile range 5.0-8.0) for the high volume injection group and 5.0 (2.0-7.0) for the placebo group (P=0.10).
Adherence—80% of participants (1536 out of 1920 questionnaires) completed the weekly online questionnaires to evaluate adherence to exercise treatment. The median percentage of performed exercises (compared with the amount of prescribed exercises) was 76% (interquartile range 46-100%) in the high volume injection group and 72% (43-100%) in the placebo group (P=0.17).
Co-interventions—The use of 12 co-interventions (eg, foot orthoses, manual treatment, and sports massage) was reported in 12 patients (31%) in the high volume intervention group compared with nine co-interventions in six patients (15%) in the placebo group (P=0.30).
Discussion
In our patient and assessor blinded, placebo controlled randomised clinical trial we found that a high volume injection without corticosteroids has no added value to an exercise programme in patients with chronic midportion Achilles tendinopathy. We found no differences in patient reported outcomes between the high volume injection and a placebo injection. Also, no between group differences were found in any of the secondary outcome measures, indicating that a high volume injection does not have mechanistic effects.
Clinical implications
These findings are important and clinically relevant, as high volume injections have become increasingly popular after several non-blinded case series and one cohort study showed an improvement in pain during activities at intermediate term follow-up (30-52 weeks).14 18 31 These findings exceeded the improvement known from eccentric exercises.24 32 33 34 As previous high volume injection studies were only performed in non-responders to eccentric training, this treatment gained even more attention. Surprisingly, large improvements (38 points on the VISA-A score) after a high volume injection were already seen in the short term (three weeks).17 This indicates a rapid decrease in symptoms of Achilles tendinopathy when a high volume injection is given. A recent blinded randomised controlled trial with a small sample size (n=19 in each treatment group) confirmed these findings, in which patient reported outcomes improved significantly more in the high volume injection group at the six week follow-up compared with the placebo group. This improvement had slightly decreased at the 24 week follow-up. Improvement in VISA-A score was lower than expected in the placebo group at 24 weeks, thereby raising the possibility of unsuccessful blinding of the participants.16 23 35 36 In our large study, we did not find any beneficial effect of the high volume injection in either the short term (2 or 6 weeks) or the intermediate term (12 or 24 weeks). An important difference between our study and previous studies investigating high volume injections, is that we did not use corticosteroids in the injection mixture. The hypothesis is that the saline solution in the injection mechanically damages the neovascularisation and its adjacent nerves.14 Corticosteroids are discouraged as treatment for tendinopathies owing to detrimental long term effects and the risk of ruptures to the Achilles tendon.37 38 39 Therefore, we decided not to include corticosteroids in the injection mixture. This could explain the difference in outcomes between our study and previous studies. We hypothesise that a high volume injection does not have a mechanical pain reducing effect but that the short term improvement as seen in previous studies might have been related to the corticosteroids. The previous randomised controlled trial evaluating the high volume injection supports this hypothesis, since short term outcome exceeded the long term outcome. This is a typical course after treatment with a corticosteroid injection.40 In studies that did not use corticosteroids in the injection mixture, comparable results to ours were seen at 12-24 weeks.15 19 31 The clinical improvement in symptoms of Achilles tendinopathy for both treatment arms in our study is similar to that reported in a recent meta-analysis evaluating the effectiveness of treatment using heavy load eccentric calf muscle exercise, and in a comparable population included at our research centre in which standalone exercise treatment was provided.28 41 The difference in the form of exercise programmes is not likely to have influenced the results, because no evidence suggests that one form of exercise training is superior to another.42 Improvement could additionally be explained by the placebo effect, patient education, load management, and the clinical course of the disorder. Our findings indicate that an exercise programme, patient education, and load management are still beneficial in patients with no previous improvement during calf muscle exercise training. We would therefore advice all patients to continue an exercise programme as the basis of their treatment.
Strengths and limitations of this study
The strength of our study is that we performed this randomised clinical trial according to the current consolidated standards of reporting trials (CONSORT) guideline. The patients, outcome assessor, and statistician were all blinded to the intervention, and only one participant was lost to follow-up. Despite our robust research design, our study also has some methodological limitations. Firstly, it was not feasible to blind the doctor who performed the injection procedure at baseline. As this doctor was not involved in the treatment allocation (randomisation), follow-up of participants, or data analysis, this probably did not influence study outcomes. Secondly, the lack of a group that only performed an exercise programme (without injection) might be regarded as limitation. We do not know whether the improvement of symptoms over time in both groups is a consequence of the exercise programme, a promoted healing response after the injection procedure, a placebo effect from the injection procedure, or represents the clinical course of Achilles tendinopathy. Thirdly, a high volume injection is a technically demanding and specific procedure. A single sports medicine doctor with extensive experience in injection procedures performed the interventions. Test sessions were carried out before the start of the study according to instructions provided by experts in high volume injections.14 Intratendinous Doppler flow disappeared in 79% of the patients in the high volume injection group compared with 30% in the placebo group, indicating success with the high volume injection.
Conclusion
In patients with a chronic midportion Achilles tendinopathy, a high volume injection without corticosteroids did not result in a beneficial effect in addition to an exercise programme. On the basis of these findings, we cannot recommend the use of a high volume injection in this patient group.
What is already known on this topic
Achilles tendinopathy is common and symptoms are often chronic
About 25-50% of patients show no improvement one year after conservative interventions
Neovascularisation, along with nerve infiltration, is one of the features in chronic symptoms; a high volume injection has been developed to obliterate these structures and is gaining popularity, yet robustly designed studies are lacking
What this study adds
A high volume injection without corticosteroids in patients with chronic midportion Achilles tendinopathy results in an initial decreased ultrasonographic Doppler flow
The high volume injection was not effective in reducing symptoms
Acknowledgments
We thank Eline van Es (Department of Orthopaedic Surgery, Erasmus MC University Medical Centre, Rotterdam, Netherlands) for the design and evaluation of the allocation sequence; Willemien Rebel-Wolterbeek and Monique de Kroes-Groeneveld (Department of Sports Medicine, Haaglanden Medical Centre, The Hague, Netherlands) for randomisation of the participants; the patients for their participation; and the healthcare providers who referred patients to our study.
Web extra.
Extra material supplied by authors
Supplementary information: additional material
Contributors: AvdV, JV, JW, PvV, RdV, RvO, and SBZ desiged the study. AvdV and RvO collected the data. AvdV, JW, and RdV analysed and interpreted the data. AvdV and RdV drafted the manuscript. RdV is the study guarantor. All authors reviewed the final manuscript and agreed to be accountable for all aspects of the work and approved the final manuscript for submission. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This study was supported by the Dutch Arthritis Association and the Anna Foundation. Both are non-commercial organisations and were not involved in the design, analysis, and content of this publication.
Competing interest: All authors have completed the ICMJE uniform disclosure form at http://www.icmje.org/coi_disclosure.pdf and declare: support from the Dutch Arthritis Association and the Anna Foundation; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: The study protocol was approved by the local medical ethics committee of South-west Holland, Netherlands (MEC 14-100).
Data sharing: Data supporting the study findings are available from the corresponding author on reasonable request.
The manuscript’s guarantor (RdV) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned have been explained.
Dissemination to participants and related patient and public communities: Study outcomes will be disseminated to the trial participants by email or letter. An easily understandable summary will be made available to patients and the public on a national online sports medicine platform (www.sportzorg.nl) and in English on the university repository (www.erasmusmc.nl/en/research/projects). We also intend to disseminate the results using social media and media outreach.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. de Jonge S, van den Berg C, de Vos RJ, et al. Incidence of midportion Achilles tendinopathy in the general population. Br J Sports Med 2011;45:1026-8. 10.1136/bjsports-2011-090342 [DOI] [PubMed] [Google Scholar]
- 2. Kvist M. Achilles tendon injuries in athletes. Ann Chir Gynaecol 1991;80:188-201. [PubMed] [Google Scholar]
- 3. Kujala UM, Sarna S, Kaprio J. Cumulative incidence of achilles tendon rupture and tendinopathy in male former elite athletes. Clin J Sport Med 2005;15:133-5. 10.1097/01.jsm.0000165347.55638.23 [DOI] [PubMed] [Google Scholar]
- 4. Alfredson H. Chronic midportion Achilles tendinopathy: an update on research and treatment. Clin Sports Med 2003;22:727-41. 10.1016/S0278-5919(03)00010-3 [DOI] [PubMed] [Google Scholar]
- 5.Lagas IF. Veldhoven PLJv, Weir A, et al. A quarter of patients with midportion Achilles tendinopathy has persisting symptoms after 10 years: a prospective cohort study. VSG Conference. Ermelo, the Netherlands, 2019. [Google Scholar]
- 6. Johannsen F, Jensen S, Wetke E. 10-year follow-up after standardised treatment for Achilles tendinopathy. BMJ Open Sport Exerc Med 2018;4:e000415. 10.1136/bmjsem-2018-000415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maffulli N, Sharma P, Luscombe KL. Achilles tendinopathy: aetiology and management. J R Soc Med 2004;97:472-6. 10.1177/0141076809701004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. De Jonge S, Warnaars JL, De Vos RJ, et al. Relationship between neovascularization and clinical severity in Achilles tendinopathy in 556 paired measurements. Scand J Med Sci Sports 2014;24:773-8. 10.1111/sms.12072 [DOI] [PubMed] [Google Scholar]
- 9. de Vos RJ, Weir A, Cobben LP, Tol JL. The value of power Doppler ultrasonography in Achilles tendinopathy: a prospective study. Am J Sports Med 2007;35:1696-701. 10.1177/0363546507303116 [DOI] [PubMed] [Google Scholar]
- 10. Zanetti M, Metzdorf A, Kundert HP, et al. Achilles tendons: clinical relevance of neovascularization diagnosed with power Doppler US. Radiology 2003;227:556-60. 10.1148/radiol.2272012069 [DOI] [PubMed] [Google Scholar]
- 11. Peers KH, Brys PP, Lysens RJ. Correlation between power Doppler ultrasonography and clinical severity in Achilles tendinopathy. Int Orthop 2003;27:180-3. 10.1007/s00264-002-0426-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Leung JL, Griffith JF. Sonography of chronic Achilles tendinopathy: a case-control study. J Clin Ultrasound 2008;36:27-32. 10.1002/jcu.20388 [DOI] [PubMed] [Google Scholar]
- 13. Ohberg L, Lorentzon R, Alfredson H. Neovascularisation in Achilles tendons with painful tendinosis but not in normal tendons: an ultrasonographic investigation. Knee Surg Sports Traumatol Arthrosc 2001;9:233-8. 10.1007/s001670000189 [DOI] [PubMed] [Google Scholar]
- 14. Chan O, O’Dowd D, Padhiar N, et al. High volume image guided injections in chronic Achilles tendinopathy. Disabil Rehabil 2008;30:1697-708. 10.1080/09638280701788225 [DOI] [PubMed] [Google Scholar]
- 15. Boesen AP, Langberg H, Hansen R, Malliaras P, Boesen MI. High volume injection with and without corticosteroid in chronic midportion achilles tendinopathy. Scand J Med Sci Sports 2019;29:1223-31. 10.1111/sms.13450 [DOI] [PubMed] [Google Scholar]
- 16. Boesen AP, Hansen R, Boesen MI, Malliaras P, Langberg H. Effect of High-Volume Injection, Platelet-Rich Plasma, and Sham Treatment in Chronic Midportion Achilles Tendinopathy: A Randomized Double-Blinded Prospective Study. Am J Sports Med 2017;45:2034-43. 10.1177/0363546517702862 [DOI] [PubMed] [Google Scholar]
- 17. Humphrey J, Chan O, Crisp T, et al. The short-term effects of high volume image guided injections in resistant non-insertional Achilles tendinopathy. J Sci Med Sport 2010;13:295-8. 10.1016/j.jsams.2009.09.007 [DOI] [PubMed] [Google Scholar]
- 18. Maffulli N, Spiezia F, Longo UG, Denaro V, Maffulli GD. High volume image guided injections for the management of chronic tendinopathy of the main body of the Achilles tendon. Phys Ther Sport 2013;14:163-7. 10.1016/j.ptsp.2012.07.002 [DOI] [PubMed] [Google Scholar]
- 19. Wheeler PC, Tattersall C. Novel Interventions for Recalcitrant Achilles Tendinopathy: Benefits Seen Following High-Volume Image-Guided Injection or Extracorporeal Shockwave Therapy-A Prospective Cohort Study. Clin J Sport Med 2020;30:14-9. [DOI] [PubMed] [Google Scholar]
- 20. Yang X, Pugh ND, Coleman DP, Nokes LD. Are Doppler studies a useful method of assessing neovascularization in human Achilles tendinopathy? A systematic review and suggestions for optimizing machine settings. J Med Eng Technol 2010;34:365-72. 10.3109/03091902.2010.497892 [DOI] [PubMed] [Google Scholar]
- 21. Sayana MK, Maffulli N. Eccentric calf muscle training in non-athletic patients with Achilles tendinopathy. J Sci Med Sport 2007;10:52-8. 10.1016/j.jsams.2006.05.008 [DOI] [PubMed] [Google Scholar]
- 22. Halasi T, Kynsburg A, Tállay A, Berkes I. Development of a new activity score for the evaluation of ankle instability. Am J Sports Med 2004;32:899-908. 10.1177/0363546503262181 [DOI] [PubMed] [Google Scholar]
- 23. de Vos RJ, Weir A, van Schie HT, et al. Platelet-rich plasma injection for chronic Achilles tendinopathy: a randomized controlled trial. JAMA 2010;303:144-9. 10.1001/jama.2009.1986 [DOI] [PubMed] [Google Scholar]
- 24. Silbernagel KG, Thomeé R, Eriksson BI, Karlsson J. Continued sports activity, using a pain-monitoring model, during rehabilitation in patients with Achilles tendinopathy: a randomized controlled study. Am J Sports Med 2007;35:897-906. 10.1177/0363546506298279 [DOI] [PubMed] [Google Scholar]
- 25. Silbernagel KG, Thomeé R, Thomeé P, Karlsson J. Eccentric overload training for patients with chronic Achilles tendon pain--a randomised controlled study with reliability testing of the evaluation methods. Scand J Med Sci Sports 2001;11:197-206. 10.1034/j.1600-0838.2001.110402.x [DOI] [PubMed] [Google Scholar]
- 26. Sierevelt I, van Sterkenburg M, Tol H, van Dalen B, van Dijk N, Haverkamp D. Dutch version of the Victorian Institute of Sports Assessment-Achilles questionnaire for Achilles tendinopathy: Reliability, validity and applicability to non-athletes. World J Orthop 2018;9:1-6. 10.5312/wjo.v9.i1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Robinson JM, Cook JL, Purdam C, et al. Victorian Institute Of Sport Tendon Study Group The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. Br J Sports Med 2001;35:335-41. 10.1136/bjsm.35.5.335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. de Vos RJ, Weir A, Visser RJ, de Winter T, Tol JL. The additional value of a night splint to eccentric exercises in chronic midportion Achilles tendinopathy: a randomised controlled trial. Br J Sports Med 2007;41:e5. 10.1136/bjsm.2006.032532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brant R. Inference for Means: Comparing Two Independent Samples. https://www.stat.ubc.ca/~rollin/stats/ssize/n2.html.
- 30. Kahan BC, Morris TP. Reporting and analysis of trials using stratified randomisation in leading medical journals: review and reanalysis. BMJ 2012;345:e5840. 10.1136/bmj.e5840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wheeler PC, Mahadevan D, Bhatt R, Bhatia M. A Comparison of Two Different High-Volume Image-Guided Injection Procedures for Patients With Chronic Noninsertional Achilles Tendinopathy: A Pragmatic Retrospective Cohort Study. J Foot Ankle Surg 2016;55:976-9. 10.1053/j.jfas.2016.04.017 [DOI] [PubMed] [Google Scholar]
- 32. Beyer R, Kongsgaard M, Hougs Kjær B, Øhlenschlæger T, Kjær M, Magnusson SP. Heavy Slow Resistance Versus Eccentric Training as Treatment for Achilles Tendinopathy: A Randomized Controlled Trial. Am J Sports Med 2015;43:1704-11. 10.1177/0363546515584760 [DOI] [PubMed] [Google Scholar]
- 33. de Jonge S, de Vos RJ, Van Schie HT, Verhaar JA, Weir A, Tol JL. One-year follow-up of a randomised controlled trial on added splinting to eccentric exercises in chronic midportion Achilles tendinopathy. Br J Sports Med 2010;44:673-7. 10.1136/bjsm.2008.052142 [DOI] [PubMed] [Google Scholar]
- 34. Yelland MJ, Sweeting KR, Lyftogt JA, Ng SK, Scuffham PA, Evans KA. Prolotherapy injections and eccentric loading exercises for painful Achilles tendinosis: a randomised trial. Br J Sports Med 2011;45:421-8. 10.1136/bjsm.2009.057968 [DOI] [PubMed] [Google Scholar]
- 35. Tumilty S, McDonough S, Hurley DA, Baxter GD. Clinical effectiveness of low-level laser therapy as an adjunct to eccentric exercise for the treatment of Achilles’ tendinopathy: a randomized controlled trial. Arch Phys Med Rehabil 2012;93:733-9. 10.1016/j.apmr.2011.08.049 [DOI] [PubMed] [Google Scholar]
- 36. Brown R, Orchard J, Kinchington M, Hooper A, Nalder G. Aprotinin in the management of Achilles tendinopathy: a randomised controlled trial. Br J Sports Med 2006;40:275-9. 10.1136/bjsm.2005.021931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Newnham DM, Douglas JG, Legge JS, Friend JA. Achilles tendon rupture: an underrated complication of corticosteroid treatment. Thorax 1991;46:853-4. 10.1136/thx.46.11.853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Vallone G, Vittorio T. Complete Achilles tendon rupture after local infiltration of corticosteroids in the treatment of deep retrocalcaneal bursitis. J Ultrasound 2014;17:165-7. 10.1007/s40477-014-0066-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Coombes BK, Bisset L, Brooks P, Khan A, Vicenzino B. Effect of corticosteroid injection, physiotherapy, or both on clinical outcomes in patients with unilateral lateral epicondylalgia: a randomized controlled trial. JAMA 2013;309:461-9. 10.1001/jama.2013.129 [DOI] [PubMed] [Google Scholar]
- 40. Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet 2010;376:1751-67. 10.1016/S0140-6736(10)61160-9 [DOI] [PubMed] [Google Scholar]
- 41. Murphy MC, Travers MJ, Chivers P, et al. Efficacy of heavy eccentric calf training for treating mid-portion Achilles tendinopathy: a systematic review and meta-analysis. Br J Sports Med 2019;53:1070-7. 10.1136/bjsports-2018-099934 [DOI] [PubMed] [Google Scholar]
- 42. Wilson F, Walshe M, O’Dwyer T, Bennett K, Mockler D, Bleakley C. Exercise, orthoses and splinting for treating Achilles tendinopathy: a systematic review with meta-analysis. Br J Sports Med 2018;52:1564-74. 10.1136/bjsports-2017-098913 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information: additional material


