Abstract
Objective:
Research Domain Criteria (RDoC) has posited a set of social dimensions that could be useful in identifying sources of individual variation in social impairments across neurodevelopmental disorders. The current investigation aimed to derive estimates of the RDoC social constructs from the Social Communication Questionnaire (SCQ) and examine whether RDoC social processes, as captured by the SCQ, are best represented by a dimensional, categorical or hybrid model.
Method:
Individual SCQ items from 4 databases were combined resulting in total N= 26,407 individuals (Mage= 8.13 years, SDage= 4.19; 69.1% male). The sample consisted of 60.0% of individuals with autism spectrum disorder (ASD), 6.8 % with a range of neurodevelopmental disorders and 33.2% of siblings of individuals with ASD.
Results:
Comparison of a range of factor solutions through the use of Exploratory Structural Equation Modelling and Confirmatory Factor Analysis indicated that a three-factor structure with separate Attachment and Affiliation, Production of Non-Facial and Facial communication factors provided excellent fit to the data (comparative fit index = .989, Tucker Lewis index = .984, root mean square error of approximation = .045) and robustness across clinical groups, age, sex and verbal status. Comparison between the best fitting factor analysis, latent class analysis and factor mixture analysis solutions demonstrated that the RDoC social processes domain is best represented as dimensional.
Conclusions:
Our findings show promise for capturing some of the important RDoC social constructs using the SCQ but also highlight crucial areas for the development of new, dedicated dimensional measures.
Keywords: Research Domain Criteria, Social Processes, Neurodevelopmental and Neuropsychiatric Disorders, Variable-Centered, Heterogeneity
Impaired ability to manage social interactions and successfully navigate the complexities of the social world represents an early emerging and cardinal feature of autism spectrum disorder (ASD). These impairments are also seen across a wide range of neurodevelopmental and neuropsychiatric disorders (Cotter et al., 2018; Happe & Frith, 2014). Irrespective of specific diagnostic status, social deficits are associated with a range of negative outcomes including poor quality of life and mental health, suboptimal educational and employment outcomes, as well as with strain on families and significant public health cost (Dickerson, 2015; Huber et al., 2018). Given the pervasive negative impact across all aspects of functioning of affected individuals, social deficits constitute an important intervention target. However, current diagnostic systems offer an imprecise characterization of social deficits, limiting their utility for etiologically-based research and stifling the development of individually tailored treatments and supports for affected individuals.
The Research Domain Criteria (RDoC) initiative advanced by the National Institute of Mental Health (NIMH) offers a promising framework for understanding variation in the social phenotypes. More specifically, RDoC defines a set of basic, distinctive processes subserved by a complex network of brain regions (Adolphs, 2009; van Overwalle, 2009) that underpin social functioning. RDoC social processes domain encompasses the following constructs: 1) Affiliation and attachment—the desire to engage in and maintain positive social interactions, 2) Social Communication—the capacity to perceive and communicate social and emotional information through both facial and non-facial expressions, 3) Perception and Understanding of Self— the ability to recognize one’s self as the agent of one’s actions (agency subconstruct) and the ability to make judgments about one’s traits, abilities, cognitive and emotional states (self-knowledge subcontract), and 4) Perception and Understanding of Self— the ability to perceive that an entity is an agent (animacy perception subconstruct), the ability to perceive and understand actions (action perception subconstruct) and the ability to perceive and interpret mental states (e.g. beliefs, desires, intentions and emotions) of others (understanding mental states subconstructs). Insight into the individual profile of strengths and weaknesses across noted processes can be used to identify sources of individual variation in social functioning irrespective of primary diagnosis, a necessary step towards the development of biologically- and etiologically-based treatments. However, given that the RDoC framework has been formalized only relatively recently and continues to be refined, measures for capturing proposed domains and constructs are still under development. This lack of dedicated measures represents a significant obstacle for the translation of this promising framework into research, and eventually, clinical practice. Therefore developing means for approximating relevant RDoC domains from the existing measures, even if somewhat suboptimal, can offer an important resource for initial testing of the explanatory power of this framework.
One of the most fundamental distinctions between the current diagnostic nosologies and the RDoC framework pertains to the categorical versus dimensional conceptualization of psychopathology. Unlike current diagnostic systems that are based on the categorical view which assumes qualitative differences between particular diagnostic categories, and between affected and non-affected individuals, RDoC is a fully dimensional framework based on the premise that psychopathology is a matter of degree rather than kind. Conceptualization of psychopathology influences both research and clinical practice in fundamental ways through assessment, research design and analysis, and etiology. A substantial body of evidence provides support for the dimensional nature of a wide range of psychopathologies (see Haslam et al., 2012 for an overview of taxometric and Krueger et al., 2018 for an overview of model-based research). However, to our knowledge, no studies to date have explored the nature of the RDoC social processes across normative and clinical populations.
To our knowledge, only one study to date has examined estimations of the RDoC social constructs from an existing measure. In a recent study, Uljarević et al. (2019) reported that the Social Responsiveness Scale (SRS-2; Constantino & Gruber, 2012) was able to capture the Attachment and Affiliation, Production of Facial and Non-facial Communication and the Mental State Understanding RDoC social constructs and subconstructs. However, despite promising findings, the SRS-2 RDoC coverage was limited given that the Production of Facial Communication construct was represented by only two items. Following the current recommendations by the NIMH (Cuthbert, 2015; National Advisory Mental Health Council Workgroup on Tasks and Measures for Research Domain Criteria, 2016), the current investigation sought to utilize a big data approach in order to test the ability of an existing and widely used measure, the Social Communication Questionnaire (SCQ; Rutter et al., 2003), to approximate proposed RDoC social process dimensions. The SCQ is a parent-report questionnaire originally developed as a screening measure of social interaction, communication, and restricted and repetitive behavior symptom domains consistent with Autism Spectrum Disorder (ASD). The original factor analysis of the SCQ derived the following 4 factors: Social Interaction (20 items), Communication (6 items), Abnormal Language (5 items) and Stereotyped Behavior (8 items) (Rutter et al., 2003). The original four-factor model explained 42.4% of the total variance, with Social Interaction, Communication, Abnormal Language and Stereotyped Behavior factors contributing 24.3%, 8.7%, 5% and 4.5 % of variance, respectively. Although developed in the context of ASD, and before the formalization of the RDoC framework, a range of SCQ social interaction and communication items bear strong conceptual resemblance to specific components of the RDoC social processes domain, most notably within the social motivation aspect of the Attachment and Affiliation (AA) construct, and Production of Facial (PFC) and Non-facial (PNFC) Communication subconstructs of the Social Communication construct. Therefore, this measure holds some promise for capturing some of the RDoC social constructs and subconstructs. In order to address the question of whether RDoC social processes are best represented by a dimensional, categorical or hybrid model we will compare the fit of their psychometric counterparts (factor analysis, latent class/profile analysis, and factor mixture modelling, respectively) to the existing data by employing analytical framework described by Clark et al. (2013). We employ the largest SCQ data set to date, comprised predominantly of a sample of children and adolescents with ASD, as well as a sample of non-affected siblings, and a non-ASD clinical sample. Mapping of this widely used screening instrument will provide the research and clinical community an alternative means of assessing key RDoC social constructs until more precise measures are developed that will enable a comprehensive and sensitive capturing of all social dimensions across clinical, at-risk and normative populations.
Methods
Participants
Data were obtained from four existing, publically available databases from the United States: the Healthy Brain Network (HBN; Alexander et al., 2017), the National Database for Autism Research (NDAR; https://ndar.nih.gov); the Simons Simplex Collection (SSC; Fischbach & Lord, 2010), and the Interactive Autism Research Database (IAN; http://iancommunity.org). Included datasets encompass individuals with autism spectrum disorder (HBN, NDAR, SSC, and IAN), unaffected siblings (SSC, IAN), and individuals with a range of clinical conditions (HBN, NDAR). This was a secondary data analysis of existing, publicly available databases, each of which encompassed a range of individual studies. Individual studies employed distinct recruitment and consenting process, inclusionary and exclusionary criteria, and incentivization approaches and strategies. All participants implicitly or explicitly consented for their anonymized data to be added to the database and publicly shared.
Only individuals with SCQ-Current version item level data, aged 18 years and younger, were included in the current investigation. No other exclusion criteria were applied. We have focused on childhood and adolescence given that majority of the disorders characterized by social impairments emerge during this period and due to the fact that majority of the development in the social domain occurs during this period.The final sample comprised N= 26,407 individuals (Mage= 8.13 years, SDage= 4.19, range: 2-18.9; 69.1% male, 30.9% female); 60.0% with a diagnosis of ASD (Mean SCQ total score= 22.56, SD= 6.66), 6.8 % with a range of other neurodevelopmental/neuropsychiatric disorders (Mean SCQ total score= 11.88, SD= 8.99) and 33.2% unaffected siblings of individuals with ASD (Mean SCQ total score= 3.98, SD= 5.16). Table 1 presents demographic and diagnostic characteristics separately for each of the databases.
Table 1.
Demographic Characteristics
| Study | |||||
|---|---|---|---|---|---|
| Whole Sample |
HBN (N= 1188) |
NDAR (N= 1576) |
SSC (N= 2180) |
IAN (N= 21463) |
|
| Mean age (SD), years | 8.13 (4.19) | 10.30 (3.35) | 5.60(3.75) | 8.82 (3.62) | 8.16 (4.21) |
| Male % | 69.1 | 64.5 | 75.5 | 68.7 | 68.9 |
| Diagnostic Group | |||||
| ASD % | 60.0 | 8.6 | 64.2 | 60.3 | 63.1 |
| Unaffected Sibling % | 33.2 | NA | NA | 39.7 | 36.8 |
| NDD/NPD %* | 6.8 | 91.4 | 35.8 | NA | 0.1 |
Note: ASD= Autism Spectrum Disorder; HBN= Healthy Brain Network; IAN= Interactive Autism Research Database; NDD/NPD= neuropsychiatric and neurodevelopmental disorders; SSC= Simons Simplex Collection.
Measures
The Social Communication Questionnaire (SCQ; Rutter et al., 2003) is a 40-item parent-report questionnaire designed to index the severity of impairments in social, communication and repetitive behavior domains seen in ASD. The SCQ has Lifetime and Current versions. The SCQ-Current was used in this paper. Each item is scored using the dichotomous response format, with a value of one indicating the presence of atypicality and a value of zero the absence of atypicality. The first item is not scored but determines whether the individual is verbal or not. For verbal children, the range of possible scores is between zero and thirty-nine, and for nonverbal children between zero and thirty-three (omitting six questions focused on abnormal language use). The SCQ provides total score, as well as scores for the Abnormal Language (example item “Does she/he ever use odd phrases or say the same thing over and over in almost exactly the same way”), Social Interaction (example item “Does she/he smile back if someone smiles at her/him”), Communication (example item “Does she/he nod her/his head to indicate yes”) and Stereotyped Behavior (example item “Does she/he ever seem to be unusually interested in the sight, feel, sound, taste, or smell of things or people”) subscales. In the original study, Berument et al. (1999) reported 15 to be an optimal cut-off score for differentiating between individuals with and without autism (sensitivity= .85 and specificity= .75) and between individuals with autism from individuals with intellectual disability but without autism (sensitivity= .96 and specificity= .67). However, subsequent studies suggested 11 as a more sensitive cut-off score that improves discriminant validity (Allen et al., 2007; Corselo et al., 2007; Lee et al., 2007; Snow & Lecavalier, 2008).Data Analysis
The total sample created by merging the four datasets (N=26,407) was randomly split into two subsamples (Sample 1 N= 13,282; Sample 2 N= 13,125) with a comparable distribution of ASD, other clinical conditions, and siblings. All analyses described below were first conducted in Sample 1 and then replicated in Sample 2 to ensure the robustness and replicability of the findings. SCQ items were conceptually mapped onto the overarching RDoC social constructs of Attachment and Affiliation and Social Communication, as well as onto the more fine-grained social communication constructs (Production of Facial and Non-Facial Communication subconstructs within the Social Communication construct). Mapping of the items was based on the definitions for each of the construct and subconstructs provided by the NIMH (Social Processes Workshop, 2012; National Advisory Mental Health Council Workgroup on Tasks and Measures for Research Domain Criteria, 2016). Only social interaction and communication items from the SCQ were considered. Items assessing restricted and repetitive behaviors and structural aspects of language were not considered. Given the emphasis of the RDoC on assessing constructs that are basic rather than encompassing several different processes, items that sampled behaviors that could result from several distinct processes were excluded. Initial mapping of the items onto RDoC social constructs was done by the first author. Following the initial mapping agreement on each item was reached with the third and last author. The ability of the SCQ to depict a distinct RDoC social construct was examined through a factor analytic framework. The question of whether a dimensional, categorical or hybrid model provides the best explanation for RDoC social processes (as measured by the SCQ) was explored through comparison between the best-fitting factor analytic (representing a dimensional model), latent class (representing a categorical model), and factor mixture modeling (representing a hybrid model). These analyses were conducted using MPLUS 8.0 (Muthen & Muthen, 1998-2015). In order to explore age and gender effects on the identified RDoC social factors, factor scores were regressed on age and gender in unaffected sibling, ASD and non-ASD clinical samples. Regression models were run in SPSS (Version 24; IBM Corp. 2016) and performed with 5000 resamples bootstrapping to provide more robust standard error estimates (Efron & Tibshirani, 1993).
Factor Analysis:
The following factor solutions were tested (i) a unidimensional model, where 19 SCQ items load onto the general social processes factor; (ii) a two-factor model where SCQ items were conceptually mapped onto the overarching Attachment and Affiliation (AA) and Social Communication (SC) RDoC social sub-constructs; (iii) a three-factor model where AA mapping was retained, and items previously mapped onto the SC factor were reassigned onto the Production of Facial (PFC) and Non-facial (PNFC) RDoC social sub-constructs. In addition, the best fitting model was further compared with the previous factor SCQ structure (Rutter et al., 2003). These alternative models were tested using Confirmatory Factor Analysis (CFA) and Exploratory Structural Equation Modelling (ESEM). The CFA that has been traditionally used to validate the construct and measurement structure relies on the independent factor model which allows items to load only onto the hypothesized factors while setting the loading as zero onto other factors. This assumption is not always realistic in psychology and psychiatry research and often leads to poor fit when items exhibit even minimal loading onto non-hypothesized factors (Marsh et al., 2014). Unlike CFA, ESEM (Asparouhov & Muthén, 2009; Marsh et al., 2014) allows items to load onto non-hypothesized factors. Model fit was evaluated using the following fit indices: the Comparative Fit Index (CFI), the Tucker-Lewis Index (TLI), the Root Mean Square Error of Approximation (RMSEA), and the Standardized Root Mean Square Residual (SRMR). The following cut-offs were applied: (i) CFI and TLI values > .90 indicating adequate and > .95 excellent fit; (ii) RMSEA and SRMR values of < .08 indicating adequate and < .06 excellent fit, with RMSEA 90% confidence intervals required not to cross the .08 boundary and the close fit test to have a p value > .05.
Latent Class Analysis (LCA):
LCA was run using individual item level data to estimate one to eight class solutions. The Bayesian Information Criterion (BIC) and Bootstrap Likelihood Ratio Test (BLRT) are considered the most reliable information criteria and the most reliable likelihood-based statistics, respectively when comparing different class solutions (Nyland et al., 2007). However, given that the decision of an optimal number of classes to be retained in LCA models is often complex, the Akaïke Information Criterion (AIC), the sample-size Adjusted BIC (ABIC) and entropy (higher values indicating fewer classification errors) were considered. Importantly, it has been demonstrated that in large sample datasets both information criteria and likelihood-based statistics suggest improvements for additional profiles without ever reaching a minimum. In those cases, it has been suggested that plotting the information criteria and examining the presence of elbows can serve as a useful guide in selecting the optimal number of classes (Morin et al., 2011).
Factor Mixture Modelling (FMM):
FMM represents a combination of factor analysis and LCA, therefore combining both categorical and dimensional features in data modeling (Lubke & Muthén, 2005). More specifically, FMM allows variation in the continuous latent variables (factors) within the identified classes. The approach taken here pre-specifies the number of factors based on the CFA and ESEM conducted in the first step and varies the number of classes broadly guided by the number of classes identified in the LCA. The most optimal solution will be determined based on the above-described information criteria, particularly BIC (lower values representing a more optimal solution).
Comparison between dimensional, categorical and hybrid models of the social processes will be conducted by comparing the BIC information criteria between the best factor analysis, LCA and FMM solutions.
Results
SCQ RDoC Factor Analysis:
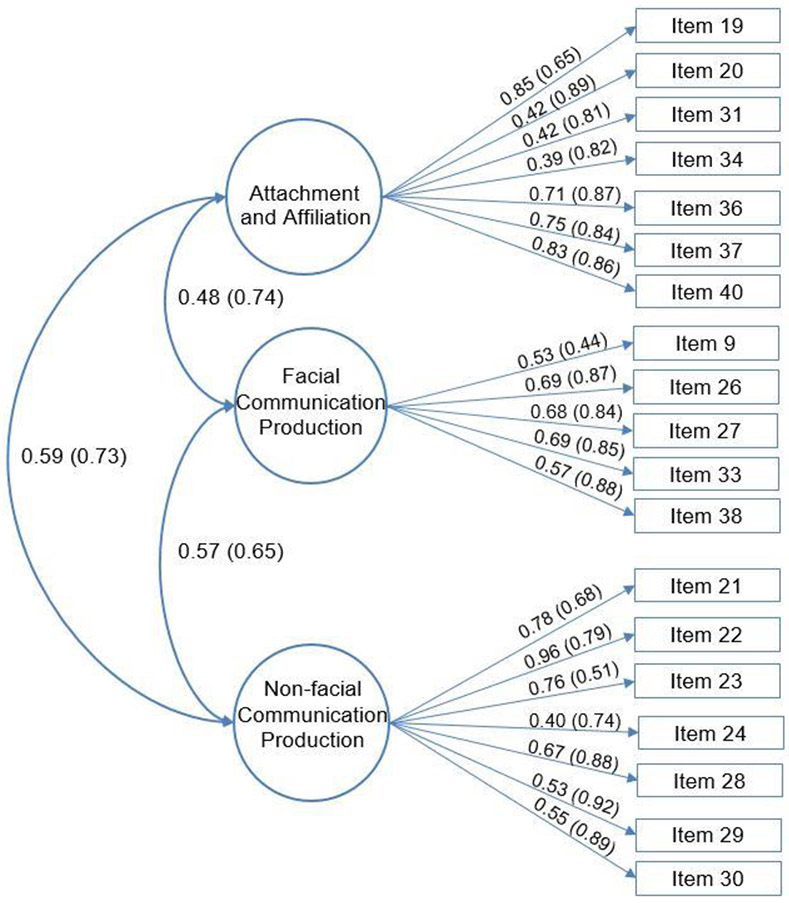
In order to evaluate the ability of SCQ to depict distinct RDoC social constructs we have utilized the CFA and ESEM approaches. Factor analysis represents a psychometric counterpart of the dimensional model of a particular trait/collection of traits. The CFA and ESEM models for both Samples 1 and 2 are presented in Table 2. The unidimensional model had unsatisfactory fit across both samples. ESEM and CFA for both two-factor (consisting of attachment and affiliation [AA] and social communication [SC] factors), and three-factor (comprising AA, production of non-facial [PNFC] and facial [PFC] communication) RDoC solutions showed excellent fit. The increase from two to three-factors was associated with a > .01 increase in CFI and TLI values across both samples and the RMSEA close fit test was not significant, suggesting that the three-factor solution was superior to the two-factor model. This three-factor RDoC solution demonstrated superior fit across all indices when compared to the previously reported SCQ factor structure (Rutter et al., 2003). Given that the focus of our investigation was on the social processing domain, we have evaluated the fit of the original Social Interaction and Communication SCQ factors. As expected, the ESEM framework indicated a more optimal fit and significantly lower factor correlations than CFA (See Figure 1 for ESEM and CFA for the whole sample). Given that large correlations between AA, PFC and PNFC suggested potential existence of an underlying general social processes factor, bi-factor modeling was used to model the potential presence of a general social factor, in addition to the presence of specific AA, PFC and PNFC factors. As can be seen from Table 2, the bi-factor model did not result in significant improvement of the model fit over the correlated three-factor solution (CFI and TLI increase < .01). Figure 1 shows factor loading for ESEM and CFA for the whole sample. Stability of the derived three-factor solution was further confirmed across (i) diagnostic group (unaffected siblings, non-ASD clinical and ASD subsamples); (ii) sex; (iii) age (the sample was divided into children aged 2-6, 7-12 and 13-18 years); and (iv) verbal level (the clinical subsample—ASD and non-ASD—was divided into verbal and non-verbal groups based on SCQ item one). Table 2 shows fit indices across the tested models. The three-factor solution showed excellent fit across typical and atypical development, age, sex and verbal status (all CFI ≥ .966, all TLI ≥ .950, all RMSEA ≤ .046, all SRMR ≤ .039) and items loadings onto AA, PNFC and PFC factors were comparable and significant across tested subgroups.
Table 2.
Summary of Goodness of Fit Statistics for the Tested Factor Analysis Models
| Model | χ2 | CFI | TLI | RMSEA (90%CI) | SRMR | |
|---|---|---|---|---|---|---|
| ESEM Unidimensional | Sample 1 | 11257.761** | .896 | .883 | .074** (.073; .075) | .042 |
| Sample 2 | 11445.913** | .895 | .882 | .075** (.074; .076) | .043 | |
| ESEM 2-Factor | Sample 1 | 5006.317** | .983 | .978 | .052** (.051; .053) | .036 |
| Sample 2 | 5025.603** | .983 | .979 | .052** (.051; .054) | .036 | |
| CFA 2-Factor | Sample 1 | 8970.420** | .969 | .965 | .066** (.065; 067) | .053 |
| Sample 2 | 9217.169** | .969 | .965 | .067** (.066; 068) | .054 | |
| ESEM 3-Factor | Sample 1 | 3287.610** | .989 | .984 | .045 (.044; .046) | .028 |
| Sample 2 | 3278.077** | .989 | .984 | .045 (.044; .046) | .027 | |
| Whole Sample | 6477.613** | .989 | .984 | .045 (.044; .046) | .037 | |
| ASD Sample | 3797.688** | .973 | .960 | .044 (.043; .045) | .035 | |
| Unaffected Siblings | 770.965** | .990 | .985 | .025 (.024; .027) | .028 | |
| Non-ASD Clinical Sample | 396.094** | .997 | .996 | .038 (.034; 042) | .024 | |
| Female Sex/Gender | 1728.446** | .994 | .991 | .041 (.039; .043) | .023 | |
| Male Sex/Gender | 4652.722** | .985 | .978 | .046 (.045; .047) | .030 | |
| Age Group 1*** | 2456.331** | .989 | .984 | .041 (.039; .042) | .026 | |
| Age Group 2*** | 1957.350** | .993 | .985 | .040 (.039; .042) | .025 | |
| Age Group 3*** | 748.154** | .996 | .994 | .036 (.033; .038) | .021 | |
| No Functional Language | 978.637** | .966 | .950 | .044 (.042; .047) | .039 | |
| Functional Language | 3515.676** | .976 | .964 | .045 (.044; .047) | .036 | |
| CFA 3-Factor | Sample 1 | 6252.670** | .979 | .976 | .055** (.054; .056) | .044 |
| Sample 2 | 6444.218** | .978 | .975 | .056** (.055; .058) | .045 | |
| ESEM 3-Factor Bi-factor | Sample 1 | 2219.278** | .993 | 988 | .040 (.038; .041) | .022 |
| Sample 2 | 2112.161** | .993 | .988 | .039 (.037; .040) | .021 | |
| ESEM Original SCQ | Sample 1 | 13909.576** | .970 | .964 | .061** (.060; .062) | .051 |
| Sample 2 | 13301.103** | .971 | .966 | .060** (.059; .061) | .050 | |
| CFA Original SCQ | Sample 1 | 21912.657** | .952 | .948 | .074** (.073; .075) | .067 |
| Sample 2 | 22150.090** | .951 | .947 | .075** (.074; .076) | .068 |
Note:
p< .01;
p< .001;
Group 1: 2-6, Group 2: 7-12, Group 3: 13-18 years; CFA: Confirmatory Factor; CFI: Comparative Fit Index; ESEM: Exploratory Structural Equation Modelling; RMSEA= Root Mean Square Error of Approximation; SRMR= Standardized Root Mean Square Residual; TLI= Tucker-Lewis Index.
Figure 1.
Exploratory Structural Equation Modelling and Confirmatory Factor Analysis correlated 3-factor solution. Solid lines represent factor loadings and curved lines represent the correlation among factors. Factor loadings and factor correlations for the Confirmatory Factor Analysis are presented in brackets.
Latent Class Analysis (LCA):
LCA was used to identify subgroups of individuals that share distinct pattern of strengths and weaknesses across different social traits and behaviors as indexed by the individual SCQ items. LCA represents psychometric counterpart of the categorical model of a particular trait/collection of traits. Table 3 provides a full summary of information criteria and likelihood-based statistics for LCA models one to eight for both samples one and two. AIC, BIC and ABIC were reduced, with each additional profile added, and with BLRT remaining significant. Plotting BIC for both samples one and two indicated leveling after the third latent class (Supplementary Figure 1). All classes had high entropy values. Both three- and four class solutions resulted in classes (subgroups) that were only distinguished by severity rather than by the specific symptom endorsement profile. Therefore, given that addition of the fourth class did not provide additional explanatory value, and that the reductions in BIC value were small after the 3rd class, the three-class solution was chosen as optimal. Identified classes were characterized as high, moderate and low severity. High severity class consisted of 92.5% of individuals with ASD, 2.2% of unaffected siblings and 5.3% of individuals with NDD/NPD; moderate severity class consisted of 59% of individuals with ASD, 30.8% of individuals with NDD/NPD and 10.2% of unaffected siblings; low severity class consisted of 76.6% of unaffected siblings, 16.6% of individuals with ASD and 6.8% of individuals with NDD/NPD.
Table 3.
Fit Indices from Latent Class Analysis models
| Model | AIC | BIC | ABIC | Entropy | BLRT p |
|---|---|---|---|---|---|
| Sample 1 | |||||
| 1 Class | 336325.185 | 336467.784 | 336407.403 | - | - |
| 2 Classes | 262178.180 | 262470.882 | 262346.944 | .939 | <.001 |
| 3 Classes | 250257.680 | 250700.485 | 250512.989 | .887 | <.001 |
| 4 Classes | 247509.351 | 248102.259 | 247851.205 | .831 | <.001 |
| 5 Classes | 245251.689 | 245994.701 | 245680.088 | .839 | <.001 |
| 6 Classes | 243755.064 | 244648.180 | 244270.009 | .812 | <.001 |
| 7 Classes | 243084.054 | 244127.273 | 243685.544 | .806 | <.001 |
| 8 Classes | 242555.667 | 243748.989 | 243243.703 | .791 | <.001 |
| Sample 2 | |||||
| 1 Classes | 332328.215 | 332470.601 | 332410.221 | - | - |
| 2 Classes | 258542.113 | 258834.379 | 258710.441 | .937 | <.001 |
| 3 Classes | 246327.849 | 246769.996 | 246582.499 | .888 | <.001 |
| 4 Classes | 243284.961 | 243876.988 | 243625.933 | .877 | <.001 |
| 5 Classes | 240861.001 | 241602.908 | 241288.296 | .843 | <.001 |
| 6 Classes | 239470.375 | 240362.163 | 239983.993 | .816 | <.001 |
| 7 Classes | 238738.465 | 239780.133 | 239338.404 | .812 | <.001 |
| 8 Classes | 238204.466 | 239396.014 | 238890.728 | .782 | <.001 |
| Factor Mixture Analysis | |||||
| Sample 1 | |||||
| 3-factor 1-class | 253086.174 | 253536.484 | 253345.810 | - | - |
| 3-factor 2-class | 253088.174 | 253545.990 | 253352.137 | .714 | > .05 |
| Sample 2 | |||||
| 3-factor 1-class | 248179.750 | 248629.391 | 248438.717 | - | - |
| 3-factor 2-class | 248181.750 | 248638.885 | 248445.033 | .938 | > .05 |
Note: AIC = Akaïke Information Criterion; BIC = Bayesian Information Criterion; BLRT = Bootstrap Likelihood Ratio Test; ABIC = sample-size Adjusted BIC.
Factor Mixture Modelling (FMM):
FMM was used to model underlying structure of social domain by allowing the structure to be both categorical and dimensional. Table 3 provides a summary of information criteria and likelihood-based statistics for FMM models. In both samples 1 and 2, the addition of the second class resulted in the increase of BIC values and did not result in a significant improvement (as indicated by the BLRT p value > .05). Increase in the BIC and lack of significant BLRT both indicate that K is preferable to K+1 solution, we did not run additional models.
Comparison between dimensional, categorical and hybrid models of social processing domain:
In order to determine whether the social processing domain is best conceptualized as dimensional, categorical, we have conducted a comparison of BIC across the best fitting dimensional model (ESEM correlated three-factor model), categorical model (3 class LCA model), and FMA model (3-factor 1 class). Comparison indicated superior fit of the dimensional model across both samples (Sample 1: 246105.14 vs 250700.485 vs 253536.48; Sample 2: 241778.91 vs 246769.99 vs 248629.39).
Age and gender effects on the identified RDoC social factors:
Table 4 shows the effects of age and gender across typically developing, ASD and non-ASD clinical groups. In the ASD sample, older age was associated with more severe AA, PNFC and PFC scores, and male gender with more severe AA scores. Conversely, in the non-ASD clinical sample, younger age was associated with more severe AA, PNFC and PFC scores. In a sample of unaffected siblings, more severe AA and PFC scores were associated with younger and older age, respectively. Male sex was associated with more severe AA scores in the ASD group; however, no significant effects for sex were observed in the other two groups. While there were no significant sex effects on either PNFC or PFC scores in the ASD and non-ASD clinical samples, female gender was associated with lower PFC and PNFC scores in the unaffected sibling sample.
Table 4.
Relationship between RDoC SCQ Social Constructs with Age and Gender
| β | SE | t | p | BCa 95% CI | |||
|---|---|---|---|---|---|---|---|
| AA | ASD | CA | .108 | .004 | 13.908 | <.001 | .048; .064 |
| Sex | −.020 | .042 | −2.592 | .01 | −.193; −.027 | ||
| Other Clinical | CA | −.327 | .013 | −13.99 | <.001 | −.214; −.162 | |
| Sex | .008 | .116 | .350 | .726 | −.186; .267 | ||
| Unaffected Siblings | CA | −.139 | .003 | −12.557 | <.001 | −.047; −.034 | |
| Sex | −.086 | .029 | −7.763 | .609 | −.281; −.167 | ||
| PNFC | ASD | CA | .114 | .004 | 14.698 | <.001 | .053; .069 |
| Sex | .014 | .044 | 1.799 | .072 | −.007; .164 | ||
| Other Clinical | CA | −.188 | .013 | −7.791 | <.001 | −.124; −.074 | |
| Sex | −.032 | .109 | −1.324 | .186 | −.359; .070 | ||
| Unaffected Siblings | CA | .011 | .003 | 1.015 | .310 | −.003; .009 | |
| Sex | −.056 | .026 | −4.948 | <.001 | −.181; −.078 | ||
| PFC | ASD | CA | .147 | .003 | 19.064 | <.001 | .051; .063 |
| Sex | .011 | .031 | 1.441 | .150 | −.016; .107 | ||
| Other Clinical | CA | −.408 | .010 | −18.09 | <.001 | −.206; −.166 | |
| Sex | −.019 | .088 | −.832 | .406 | −.247; .100 | ||
| Unaffected Siblings | CA | .050 | .002 | 4.447 | <.001 | .005; .013 | |
| Sex | −.042 | .018 | −3.723 | <.001 | −.101; −.031 |
Note: AA= Attachment and Affiliation; CA= Chronological Age; PNFC= Production of Non-Facial Communication; PFC= Production of Facial Communication.
Discussion
The primary aim of the current study was to apply advanced variable-centered analyses to the largest SCQ sample to date, mainly comprising individuals with ASD, but also their unaffected siblings and individuals with other clinical conditions, in order to explore the utility of the Social Communication Questionnaire (SCQ) as a potentially useful instrument for capturing certain constructs within the RDoC social processes domain. Systematic comparison between a unidimensional, two-factor RDoC model with Attachment and Affiliation (AA) and Social Communication factors, and a 3-factor RDoC model with AA, Production of Facial (PFC) and Non-Facial (PNFC) factors showed that the three-factor RDoC model had superior fit across all fit indices, for both initial and replication subsamples, both when using CFA and ESEM frameworks. Strong correlations among the identified AA, PFC, and PNFC factors suggested the possibility of the presence of a general, overarching social processes factor, akin to the general intelligence factor or general psychopathology factor (Caspi et al., 2014). However, bi-factor modeling with a general social factor and specific AA, PFC and PNFC factors did not show improvements over the correlated three-factor solution, suggesting the latter as the most optimal solution. This was most likely due to the fact that ESEM approach allows items to load onto both hypothesized and non-hypothesized factors (Marsh et al., 2014), therefore, the addition of general factor does not result in a significant improvement over the correlated factor solution. Further analyses confirmed the robustness of the three-factor model across typical and atypical development, age, sex and verbal.
A secondary aim of the current investigation was to test whether dimensional, categorical or hybrid models provide the best explanation of the RDoC social processes as measured by the SCQ. Findings from the current investigation suggest that the dimensional model showed superior performance over the categorical and hybrid models. This conclusion is in line with the most comprehensive review of the taxometric research to date (Hasslam et al., 2012). Interestingly, results from the current analyses do not align with previous studies (Frazier et al., 2010; 2012; James et al., 2016) which suggested that ASD might form a qualitative category distinct from normative behaviors and traits. However, while noted studies relied on a general student sample, and ASD and unaffected sibling samples from a single database, our sample was an order of magnitude larger comprising individuals with ASD, their siblings and non-ASD clinical group, therefore providing wider variation/behavioral range. The influence of sampling on the findings is further underscored by a very recent study by Kim et al. (2018) which, contrary to studies by James et al. and Frazier et al., concluded that the dimensional framework provides the best conceptualization of ASD traits in a sample comprising individuals with ASD and other clinical conditions. Finally, unlike previous studies, the focus of the present investigation was specifically on addressing the question of whether the social processing domain, as described by the RDoC framework, should be conceptualized as dimensional. Therefore, we did not include other behavioral types, and further work with similar sample sizes as used here is needed to further inform the debate on the categorical versus dimensional nature of psychopathology.
Derived AA, PNFC and PFC factors showed a distinct pattern of associations with chronological age and gender, and some of these effects were moderated based on clinical status. There was a contrasting relationship between age and distinct social factors in ASD and unaffected sibling samples. More specifically, while older age was associated with more problems in affiliation and attachment, facial communication, and non-facial communication in the ASD group, the opposite was the case in unaffected siblings. General literature strongly suggests that in normative development, all aspects of social functioning become progressively more advanced and sophisticated over time, which is in line with our findings in unaffected siblings. Conversely, social deficits in ASD either persist or become progressively more pronounced over time without the early interventions. However, given the cross-sectional nature of the data reported here, inferences about development are necessarily tenuous. In addition, given the dichotomous scoring of the SCQ, and the fact that items were developed in the context of ASD, items might not be sensitive enough to pick up more subtle and more complex symptom expressions seen beyond neurodevelopmental disorders. Therefore, detailed longitudinal explorations of these phenomena measured concurrently by SCQ and other instruments, across both normative and atypical development, and how they mutually interact across sensitive developmental periods in order to produce distinct clinical presentations, is needed in order to further clarify findings reported here. Consistent with the previous literature on social motivation in ASD (Sedgewick et al., 2016) we found that female gender was associated with less severe SCQ AA scores. However, consistent with the suggestions that in ASD differential effects of gender on social functioning are either not present, or even reversed in some cases (Frazier et al., 2014), we found no significant effects of gender on the PFC and PNFC scores in the ASD sample.
The current investigation has important research and clinical implications. The analyses demonstrated that the model mapping 19 SCQ items onto RDoC AA, PFC and PNFC constructs provided an excellent fit to the data. At this time, there is a lack of comprehensive measurement tools specifically designed to depict all proposed social RDoC dimensions and constructs, which has significantly stifled testing and refinement of this promising framework and its adoption in research and clinical practice. Given that the SCQ is a widely used screening instrument and is available in a range of existing datasets, newly constructed SCQ RDoC subscales offer a valuable resource for both research and clinical communities. If replicated, our findings that social processes are best conceptualized as dimensional, suggest that it is more fruitful for future instruments to be optimized for gradation rather than purely for classification, and that rather than adopting case-control designs, it is more optimal to sample individuals with a specific distribution of the trait/behavior of interest, irrespective of the primary diagnosis.
Limitations and future directions
Several notable limitations need to be considered when interpreting findings from the current study. The four datasets used in the current investigation encompassed individuals with ASD, their unaffected siblings, and individuals with a range of neurodevelopmental and neuropsychiatric disorders, therefore affording a sample size an order of magnitude larger than samples used in previous investigations as well as a wide distribution of the social domain item scores. However, our sample was nevertheless heavily skewed towards the ASD population, and although findings are generalizable across the autism spectrum, it will be of crucial importance for future studies to replicate current findings in samples which include more balanced distribution of different clinical disorders characterized by social impairments. In addition, the possibility of rating bias in unaffected siblings of children with ASD needs to be taken into account when interpreting findings reported here. However, it is important to highlight that our investigation focused on the factor analysis and has demonstrated excellent fit of the derived factors across both ASD sample and the sample of their unaffected siblings. Although the 3-factor RDoC SCQ structure was replicated across the verbal and non-verbal clinical subgroups it will be important for future research to provide further evidence of external validity by incorporating dedicated dimensional measures of psychopathology and cognitive functioning. As noted, the SCQ provides a relatively wide sampling of different social behaviors, which as we have demonstrated, reliably depict three distinct RDoC constructs. Nevertheless, the SCQ was designed in the context of ASD and is limited in terms of sampling particular social dimensions described by the RDoC framework. For example, the attachment and affiliation dimension is only represented by items relating to the social motivation aspect of this dimension, and the production of non-facial communication subconstruct does not provide an in-depth depiction of all important behavioral indicators. In addition, the SCQ does not sample the reception of facial and non-facial communication nor the understanding of mental states. Therefore, it is important for future investigations to supplement the use of the SCQ with measures that depict these noted dimensions. The purpose of this study was not to arrive at the best fitting general SCQ factor solution. Therefore, alternative factor structures, especially in relation to the structure of ASD, are possible. Rather, our focus was to evaluate the ability of selected SCQ items to approximate RDoC social sub-constructs and we believe that the resultant excellent statistical fit suggests that the item mapping was adequate and our goal was achieved. Finally, given that the current investigation focused on the subjective report unit of analysis, it will be important for future studies to include performance-based assessments of different social dimensions as well as neuroimaging and genetic information.
Conclusions
Our findings demonstrate the utility of the SCQ, a well-established and widely used subjective report measure, as a useful tool for capturing the RDoC social constructs of attachment and affiliation, and production of facial and non-facial communication. In addition to providing a means for initial testing of the explanatory power of the RDoC framework, the current investigation highlights crucial areas for development of novel, dedicated, comprehensive measures of social processing.
Supplementary Material
Acknowledgments
Funding details: The study was supported by grant R03MH111846-01 (Hardan & Jo) by the National Institute of Mental Health.
Footnotes
Conflicts of Interest: None.
References
- Adolphs R The social brain: neural basis of social knowledge. (2009). Annual Review of Psychology, 60, 693–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander LM, Escalera J, Ai L, Andreotti C, Febre K, Mangone A, et al. (2017). An open resource for transdiagnostic research in pediatric mental health and learning disorders. Scientific Data, 4, 170181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asparouhov T, & Muthén B (2009). Exploratory structural equation modeling. Structural Equation Modeling, 16, 397–438. [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor SJ, Harrington H, Israel S, et al. The p Factor: One General Psychopathology Factor in the Structure of Psychiatric Disorders? Clinical Psychological Science, 2(2), 119–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark SL, Muthén B, Kapiro J, D’Onofrio BM, Viekn R, & Rose RJ (2013). Models and Strategies for Factor Mixture Analysis: An Example Concerning the Structure Underlying Psychological Disorders. Structural Equation Modelling, 20(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotter J, Granger K, Backx R, Hobbs M, Looi CY, & Barnett JH (2018). Social cognitive dysfunction as a clinical marker: A systematic review of meta-analyses across 30 clinical conditions. Neuroscience and Biobehavioral Reviews, 84, 92–99. [DOI] [PubMed] [Google Scholar]
- Constantino JN, Gruber CP (2012). Social responsive scale manual (2nd ed., SRS-2). Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Cuthbert BN. Research Domain Criteria: toward future psychiatric nosologies. (2015). Dialogues in Clinical Neuroscience, 17(1), 89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson BC (2015). Dysfunction of social cognition and behavior. Continuum (Minneap Minn), 21(3), 660–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Efron B, & Tibshirani R (1993). An introduction to the bootstrap. Boca Raton, FL: Chapman & Hall/CRC. [Google Scholar]
- Fischbach GD, & Lord C (2010). The Simons Simplex Collection: a resource for identification of autism genetic risk factors. Neuron, 68(2), 192–5. [DOI] [PubMed] [Google Scholar]
- Frazier TW, Youngstrom EA, Sinclair L, Kubu CS, Law P, Rezai A, et al. (2010). Autism spectrum disorders as a qualitatively distinct category from typical behavior in a large, clinically ascertained sample. Assessment 17(3), 308–320. [DOI] [PubMed] [Google Scholar]
- Frazier TW, Youngstrom EA, Speer L, et al. (2012). Validation of proposed DSM-5 criteria for autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 51, 28–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier TW, Ratliff KR, Gruber C, Zhang Y, Law PA, & Constantino JN (2014). Confirmatory factor analytic structure and measurement invariance of quantitative autistic traits measured by the Social Responsiveness Scale-2. Autism, 18(1), 31–44. [DOI] [PubMed] [Google Scholar]
- Happe F, & Frith U (2014). Annual research review: towards a developmental neuroscience of atypical social cognition. Journal of Child Psychology and Psychiatry, 55(6), 553–77. [DOI] [PubMed] [Google Scholar]
- Hasslam N, Holland E, & Kuppens P (2012). Categories versus dimensions in personality and psychopathology: a quantitative review of taxometric research. Psychological Medicine, 42(5), 903–20. [DOI] [PubMed] [Google Scholar]
- Huber L, Plötner M, & Schmitz J (2018). Social competence and psychopathology in early childhood: a systematic review. European Child & Adolescent Psychiatry. [DOI] [PubMed] [Google Scholar]
- James RJE, Dubey I, Smith D, Ropar D, & Tunney RJ The Latent Structure of Autistic Traits: A Taxometric, Latent Class and Latent Profile Analysis of the Adult Autism Spectrum Quotient. Journal of Autism and Developmental Disorders, 46(12), 3712–3778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, Keifer C, Rodriguez-Seijas C, Eaton N, Lerner M, & Gadow K (2018). Quantifying the Optimal Structure of the Autism Phenotype: A Comprehensive Comparison of Dimensional, Categorical, and Hybrid Models. Journal of the American Academy of Child and Adolescent Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Kotov R, Watson D, Forbes MK, Eaton NR, Ruggero CJ, et al. (2018). Progress in achieving quantitative classification of psychopathology. World Psychiatry, 17(3), 282–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubke GH, & Muthén BO (2005). Investigating population heterogeneity with factor mixture models. Psychological Methods 10, 21–39. [DOI] [PubMed] [Google Scholar]
- Marsh HW, Morin AJS, Parker P, & Kaur G (2014). Exploratory structural equation modeling: an integration of the best features of exploratory and confirmatory factor analysis. Annual Review of Clinical Psychology, 10, 85–110. [DOI] [PubMed] [Google Scholar]
- Morin AJS, Morizot J, Boudrias JS, & Madore I (2011). A multifoci person-centered perspective on workplace affective commitment: A latent profile/factor mixture analysis. Organizational Research Methods, 14, 58–90. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 5th ed. Los Angeles, CA: Muthén & Muthén; 2007. [Google Scholar]
- National Advisory Mental Health Council Workgroup on Tasks and Measures for Research Domain Criteria. Behavioral Assessment Methods for RDoC Constructs. Bethesda, MD; 2016. [Google Scholar]
- Nylund KL, Asparouhov T, Muthén B (2007). Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Structural Equation Modeling, 14(4), 535–569 [Google Scholar]
- Rutter M, Bailey A, & Lord C (2003). Social Communication Questionnaire (SCQ). Los Angeles: Western Psychological Services. [Google Scholar]
- Sedgewick F, Hill V, Yates R, et al. (2016). Gender Differences in the Social Motivation and Friendship Experiences of Autistic and Non-autistic Adolescents. Journal of Autism and Developmental Disorders, 46, 1297–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uljarević M, Frazier TW, Phillips JM, Jo B, Littlefield S, & Hardan AY (2019). Mapping the Research Domain Criteria Social Processes Constructs to the Social Responsiveness Scale. Journal of American Academy of Child and Adolescent Psychiatry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Overwalle F (2009). Social cognition and the brain: a meta-analysis. Human Brain Mapping, 30(3), 829–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.