Abstract
Background and Aim:
An acute pain service (APS) has been running in our institute since April 2013 and is managed by the Department of Anesthesia and Intensive Care. However, it is not clear to what extent the patients feel benefited from the APS. The aim of the study was to compare the perception of postoperative pain management in patients receiving care under APS with those receiving routine postoperative pain relief following lower limb surgery.
Material and Methods:
This was a prospective, hospital-based, controlled non-randomized study. American Society of Anesthesiologists (ASA) grades I–III patients with age 18–75 years undergoing lower limb orthopedic surgery were prospectively recruited into APS (index group) or routine postoperative care (control group) (n = 55 each). Postoperatively, American Pain Society Patient Outcome Questionnaire-Revised (APS-POQ-R) and Short Form (SF-12) were used to evaluate the outcome of postoperative pain management at 24 h and health-related quality of life after 4 weeks respectively.
Results:
Both groups were comparable in terms of demographic data. Patients in the index group had statistically significant better perception of care than the control group. Index group scored significantly higher than control group on median patient satisfaction score (9; interquartile range [IQR] [7–10] vs. 5 [3–6]; P < 0.001). In index group, there was significant reduction of worst pain in first 24 h along with decreased frequency of severe pain.
Conclusion:
Implementation of acute pain service plays an important role in improving the quality of postoperative pain relief, perception of care, and patient satisfaction.
Keywords: Acute pain service, patient satisfaction, perception of care
Introduction
Pain has been considered as a silent epidemic. Since 2004, pain relief has been declared as one of the fundamental human rights with medical, ethical, and legal aspects.[1] Not only uncontrolled pain leads to poor functional outcome, it also causes increased readmissions with increased expense and further conversion to persistent chronic pain. Pavlin et al. showed that pain delayed recovery in 24% patients in ambulatory surgery.[2] Therefore, pain management is an important aspect of perioperative anesthesia care.
Despite substantial advancement and availability of drugs and regional techniques, surveys conclude that pain relief continues to be suboptimal.[3-5] A survey from USA concluded that approximately 86% of patients experienced postoperative pain with 76% patients having persistent pain even after discharge.[4] Similarly, in India, less than 30% patients received optimal postoperative pain relief.[5]
As a solution, evidence based acute pain service (APS) was introduced to manage postoperative pain.[6] It is a dedicated, round-the-clock service with quality assurance. APS has been running since April 2013 and is managed by the Department of Anesthesia and Intensive Care in our institute. However, it is not clear to what extent the patients feel benefited. Survey of patient satisfaction with pain management is also an important aspect of APS as per the American Pain Society in Quality Assurance standards for relief of acute- and cancer-related pain.[7] Thus, it was imperative to assess the postoperative pain perception, quality of care, and satisfaction of those patients receiving care under APS compared with those receiving routine postoperative care. Perception of care was defined as pain relief, participation in decisions, and satisfaction with pain treatment.[8]
The aim of the study was to compare the perception of postoperative pain management and health-related quality of life after orthopedic lower limb surgery using American Pain Society Patient Outcome Questionnaire-Revised (APS-POQ-R)[9] and Short Form Health Survey (SF-12), respectively in patients receiving care under APS with those receiving routine postoperative pain management.[10]
Material and Methods
A prospective, hospital-based controlled non-randomized study was conducted between August 2017 and March 2018 in a tertiary care teaching hospital in Chandigarh. After approval from the Institute Ethics Committee, 130 American Society of Anesthesiologists (ASA) grades I-III patients aged 18-75 years undergoing lower limb orthopedic surgery were prospectively recruited into two groups: Index and control group. Postoperative patients either received care under APS (index group) or routine postoperative care (control group). The group allocation was not random but was dependent on referral to APS. Referral was done preoperatively by the team of surgeon and anesthesiologist not involved in the study. Uncooperative, nonconsenting, and delirious patients were excluded from study. Patients with cognitive impairment, those suffering from other known painful conditions unrelated to the surgery, those with lack of access to a telephone or lack of basic verbal and language skills were also excluded. Patients were provided with a patient information sheet detailing the purpose of the study.
All patients were recruited in APS after obtaining informed consent following referral. Demographics and clinical data were collected (age, gender, educational status, disease, type of surgery, type of anesthesia, and postoperative pain control measures). In the index group, protocol-driven multimodal analgesia was provided by trained pain nurse under supervision of anesthesiologist. Patients received either epidural infusions of local anesthetic or opioid mixtures, or intravenous opioid as patient-controlled analgesia (PCA) in addition to intravenous paracetamol and diclofenac unless contraindicated. The other elements of APS included 24 × 7 monitoring, pain documentation, pro-active approach, and pain rounds with a consultant. In the control group, pain management was supervised by the surgeon. Patients received medications mainly including paracetamol, diclofenac, ibuprofen, or tramadol, through oral and/or intravenous routes, but no epidural or PCA as in APS.
The primary outcome of the study was to compare the perception of postoperative pain management of the patients undergoing orthopedic lower limb surgery either receiving care under APS or routine postoperative pain management using APS-POQ-R.[9] The secondary outcomes of the study were to compare postoperative pain severity, adverse effects, interference to different activities, and health-related quality of life using APS-POQ-R and SF-12[10] respectively the two groups. Brief descriptions of these two key instruments are given below.
APS-POQ-R is a patient reported outcome questionnaire, developed by the American Pain Society for patient assessment of postoperative pain management. It has been universally accepted and used internationally by the PAIN OUT Project (www.pain-out.eu).[9] APS-POQ-R is composed of six subscales including pain severity, adverse effects, interference to different activities including sleep, emotional state, perception of care, and nonpharmacological therapies. It has 12 items, which are rated on 11-point continuous scale from 0 to 10 where 10 signifies the highest score. Frequency of pain and pain relief were measured on 11-point scale from 0% to 100%. Pain severity (two items) was measured using worst pain and frequency of pain in 24 h. Pain-related interference to activities (1 item) in bed like turning, repositioning, or out of bed like walking, sitting, standing, and sleep (difficulty falling or staying asleep) were observed. They were further categorized into: no interference (0), mild (1-3), moderate (4-6), and severe (7-10). Side effects (one item) include nausea, drowsiness, itching, and dizziness, whereas anxiety, depression, frightened, and helpless behavior were evaluated in emotional state.
SF-12 measures health-related quality of life with two domains of general physical and mental health status.[10] It consists of 12 items with eight health subdomains. General health is measured on a 5-level response scale: excellent (1), very good (2), good (3), fair (4), and poor (5). Physical functioning subdomain measures limitation in moderate and severe activities on 3 level response: “yes, limited a lot (1); yes, limited a little (2) and no, not limited at all (3).” Mental health (two items), vitality, and social functioning subdomain are measured on a 6-level response scale: all of the time (1), most of the time (2), good bit of the time (3), some of the time (4), a little of the time (5), and none of the time (6). Role functioning subdomain has physical and mental components with two items each. They are measured on 2-level response scale: yes (1) and no (2). Bodily pain subdomain is also measured on 5-level response scale: extremely (1), quite a bit (2), moderately (3), a little bit (4), and not at all (5).
Patients filled the APS-POQ-R at 24 h postoperatively either in English or Hindi. An investigator blinded to group allocation assessed their pain experience and also explained the meanings of items in forms in case of difficulty. This investigator was not involved in pain management of the patients. At 4 weeks, SF-12 form was filled telephonically by the blinded investigator not involved in group allocation. In order to decrease the bias, the data were interpreted by a third person (anesthesiologist) not involved in execution of the project.
Sample size calculation: The perception of postoperative pain management was the primary outcome variable in this study, which was measured by APS-POQ-R. The total score for perception of pain can range from 0 (worst perception) to maximum 120 (best possible perception). Assuming a median score of 60 for the index group, a large standard deviation of 25, it was calculated that 44 patients would be required in each group in order to detect a clinically meaningful 20% difference between the index group and control group on APS-POQ-R score, with power of 80% and alpha error of 5%. Allowing for 10% dropout and 10% oversampling, it was decided that 55 patients would be recruited in each group.
All statistical calculations was done using SPSS (Statistical Package for the Social Science) 21 version. Qualitative data were described in terms of frequencies (number of cases), relative frequencies (percentages), score distributions, median, and IQR. Quantitative data were expressed as mean ± standard deviation (±SD). Both the groups were compared in terms of frequencies and scores using chi squared test and Mann--Whitney U test, respectively. P values <0.05 were considered statistically significant.
Results
Patient characteristics: A total of 130 postoperative patients were recruited for the study and we lost 20 patients in follow-up. In both the groups, 55 patients were included. Both index and control group were comparable in terms of demographic and clinical data. Majority of patients were male and had completed middle or high school education in both groups [Table 1].
Table 1.
Demographic and clinical data
| Demographics | Index Group (n=55) | Control Group (n=55) | P | |
|---|---|---|---|---|
| Age | (yr) | 44.7±14.9 | 40.0±15.1 | 0.10 |
| Weight | (kg) | 69.0±12.2 | 63.8±9.8 | 0.07 |
| Gender | Male | 44 (80%) | 45 (81.8%) | 0.80 |
| Female | 11 (20%) | 10 (18.2%) | ||
| Educational status | Uneducated <5th class 5-10th class 10-12 class Graduation |
6 (10.9%) 15 (27.3%) 14 (25.5%) 14 (25.5%) 6 (10.9%) |
9 (16.4%) 8 (14.5%) 15 (27.3%) 14 (25.5%) 9 (16.4%) |
0.498 |
| Type of surgery | Tibia fracture Repair Femur fracture repair |
23 (41.8%) 32 (58.2%) |
24 (43.6%) 31 (56.4%) |
0.847 |
| Duration of surgery (h) | 3.4±0.6 | 3.4±0.9 | 0.713 | |
| Pain modalities | ||||
| Epidural - 50 (90.9%) Continuous - 35 (63.6%) PCA -15 (27.3%) IV-PCA - 5 (9.1%) |
IV-40 (72.7%) Oral -9 (16.4%) Oral + IV -6 (10.9%) |
|||
| Paracetamol -55 (100%) Diclofenac - 53 (94.5%) |
Paracetamol (O) - 3 (5.5%) Tramadol (I.V.) - 3 (5.5%) |
|||
| Paracetamol (I.V.) + Diclofenac (I.V.) - 37 (67.3%) Paracetamol (O) + Ibuprofen (O) - 6 (10.9%) Ibuprofen (O) + Tramadol (I.V.) - 4 (7.3%) Paracetamol (O) + Ibuprofen (I) + Tramadol (T) -2 (3.6%) |
||||
PCA– Patient controlled analgesia, IV-PCA - Intravenous patient controlled analgesia, O- oral, I.V.- Intravenous
Pain intensity was significantly higher in the control group with 47 (85%) patients having moderate to severe worst pain and 44 (80%) patients experiencing pain more than half of postoperative time. In contrast, only 21 patients (38%) receiving APS care (the index group) had moderate to severe worst pain, and only 5 (9%) patients had pain more than half of postoperative time.
In the index group, there was significant reduction of pain related interference in activities in and out of bed [Table 2]. In the index group, only three (5%) and two (4%) patients had severe anxiety and depression in postoperative period as compared to 23 (42%) and 14 (25%) patients in the control group, respectively. In the index group, there was significant reduction of pain-related incidence of nausea to 0% from nine patients (16%) in the control group.
Table 2.
Number of patients having pain-related interference to different activities
| Activities | None | Mild | Moderate | Severe | P | ||||
|---|---|---|---|---|---|---|---|---|---|
| I n (%) | C n (%) | I n (%) | C n (%) | I n (%) | C n (%) | I n (%) | C n (%) | ||
| Activities in bed | 1 (1.8) | 1 (1.8) | 25 (45.5) | 1 (1.8) | 25 (45.5) | 17 (30.9) | 4 (7.3) | 36 (65.5) | 0.001 |
| Activities out of bed | 2 (3.6) | 1 (1.8) | 20 (36.4) | 1 (1.8) | 13 (23.6) | 8 (14.5) | 20 (36.4) | 45 (81.8) | 0.001 |
| Staying sleep | 1 (1.8) | 1 (1.8) | 36 (65.5) | 24 (43.6) | 15 (27.3) | 10 (18.2) | 3 (5.5) | 20 (36.4) | 0.002 |
| Falling asleep | 9 (16.4) | 1 (1.8) | 27 (49.1) | 34 (61.8) | 12 (21.8) | 4 (7.3) | 7 (12.7) | 16 (29.1) | 0.003 |
n– number of patients; I– Index group; C– Control group; % - percentage of patients
Patients in the index group had significantly better perception of care than the control group [Table 3]. Majority of patients in the index group (n = 43; 78%) reported pain relief more than 60%, with ten patients (18%) having 100% pain relief, as compared to 15 (27%) and none in the control group respectively. [Figure 1] Majority of the patients in the index group (n = 44; 80%) were highly satisfied (score 7 or more) compared to a minority (n = 11; 20%) in the control group [Figure 2].
Table 3.
Comparison of the groups in terms of APS-POQ-R
| APS-POQ-R | Index Group (n=55) median (IQR) | Control Group (n=55) median (IQR) | P |
|---|---|---|---|
| Worst pain in 24 h | 6 (3-8) | 8 (7-10) | P<0.001 |
| Frequency of severe pain in 24 h | 20% (10-40) | 70% (60-80) | P<0.001 |
| Mood and emotions Anxious Depression Frightened Helpless |
1 (0-2) 1 (0-2) 1 (0-2) 1 (0-4) |
6 (3-7) 4 (2-7) 3 (1-6) 6 (2-7) |
P<0.001 P<0.001 P<0.001 P<0.001 |
| Side effects Nausea Drowsiness Itching Dizziness |
0 (0-1) 0 (0-1) 0 (0-1) 0 (0-1) |
1 (0-6) 0 (0-4) 0 (0-1) 0 (0-3) |
0.0036 0.146 0.103 0.146 |
| Pain relief in 24 h | 8 (7-9) | 4 (3-6) | P<0.001 |
| Participation in decisions | 6 (3-9) | 3 (1-8) | 0.016 |
| Satisfaction | 9 (7-10) | 5 (3-6) | P<0.001 |
Figure 1.
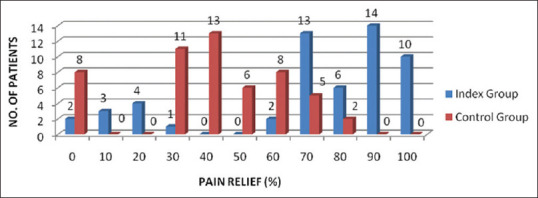
Comparison of both groups in terms of pain relief (%)
Figure 2.
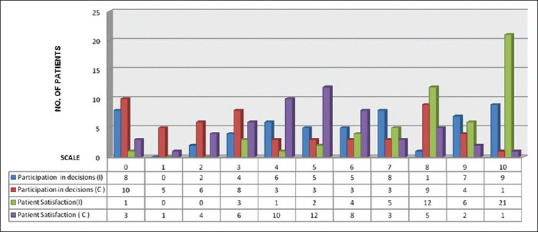
Comparison of participation in decisions and patient satisfaction
Majority of patients (n = 41; 74.54%) participated in decisions (score >3) about pain relief in the index group compared to 26 patients (47.27%) in the control group [Figure 2]. Only 23 patients (41.81%) received information about pain-treated options in the control group as compared to 46 (83.63%) in the index group. Majority of patients (n = 38; 69.09%) found the information provided very helpful (score >6) in the index group compared to only 7 (12.72%) in the control group.
There was no statistical difference in quality of life in both groups at one month postoperatively. However, in the index group, after APS care, more patients significantly felt that moderate activities were not limited after 1 month postoperatively (P = 0.009) [Table 4].
Table 4.
Comparison of the groups in terms of SF-12
| SF-12 | Index Group (n=55) n (%) | Control Group (n=55) n (%) | P | ||
|---|---|---|---|---|---|
| Subdomain | Item | Score level | |||
| General health* | Health | 1 | 8 (1.5%) | 16 (29.1%) | 0.05 |
| 2 | 14 (25.5%) | 10 (18.2%) | |||
| 3 | 21 (38.2%) | 11 (20%) | |||
| 4 | 12 (21.8%) | 16 (29.1%) | |||
| 5 | 0 (0%) | 2 (3.6%) | |||
| Physical functioning* | Limitation of moderate activities | 1 | 18 (32.7%) | 34 (61.8%) | 0.009 |
| 2 | 22 (40%) | 13 (23.6%) | |||
| 3 | 15 (27.3%) | 8 (14.5%) | |||
| Limitation of climbing several flights | 1 | 28 (50.9%) | 38 (69.1%) | 0.1 | |
| 2 | 14 (25.5%) | 9 (16.4%) | |||
| 3 | 13 (23.6%) | 8 (14.5%) | |||
| Role functioning (physical)* | Regular activities - accomplished less | 1 | 31 (56.4%) | 31 (56.4%) | 1 |
| 2 | 24 (43.6%) | 24 (43.6%) | |||
| Limitation of regular activities due to physical health | 1 | 23 (41.8%) | 31 (56.4%) | 0.12 | |
| 2 | 32 (58.2%) | 24 (43.6%) | |||
| Role functioning (mental)** | Due to emotional problems - Accomplished less | 1 | 27 (49.1%) | 32 (58.2%) | 0.54 |
| 2 | 28 (50.9%) | 23 (41.8%) | |||
| Limitation of work due to emotional problem | 1 | 24 (43.6%) | 28 (50.9%) | 0.44 | |
| 2 | 31 (56.4%) | 27 (49.1%) | |||
| Bodily pain* | Pain interference to normal work | 1 | 15 (27.3%) | 13 (23.6%) | 0.56 |
| 2 | 7 (12.7%) | 10 (18.2%) | |||
| 3 | 14 (25.5%) | 8 (14.5%) | |||
| 4 | 11 (20%) | 13 (23.6%) | |||
| 5 | 8 (14.5%) | 11 (20%) | |||
| Vitality** | Lot of energy | 1 | 10 (18.2%) | 5 (9.1%) | 0.052 |
| 2 | 13 (23.6%) | 20 (36.4%) | |||
| 3 | 15 (27.3%) | 6 (10.9%) | |||
| 4 | 10 (18.2%) | 9 (16.4%) | |||
| 5 | 5 (9.1%) | 13 (23.6%) | |||
| 6 | 2 (3.6%) | 2 (3.6%) | |||
| Mental health** | Calm and peaceful | 1 | 11 (20%) | 5 (9.1%) | 0.120 |
| 2 | 10 (18.2%) | 16 (29.1%) | |||
| 3 | 15 (27.3%) | 8 (14.5%) | |||
| 4 | 9 (16.4%) | 9 (16.4%) | |||
| 5 | 10 (18.2%) | 15 (27.3%) | |||
| 6 | 0 (0%) | 2 (3.6%) | |||
| Downhearted and blue | 1 | 1 (1.8%) | 1 (1.8%) | 0.144 | |
| 2 3 4 |
8 (14.6%) 7 (12.7%) 14 (25.5%) |
20 (36.4%) 6 (10.9%) 8 (14.6%) |
|||
| 5 | 12 (21.8%) | 11 (20%) | |||
| 6 | 13 (23.6%) | 9 (16.4%) | |||
| Social functioning** | Physical health or emotional problem interference to social activities | 1 2 3 4 5 6 |
0 (0%) 9 (16.4%) 16 (29.1%) 8 (14.5%) 7 (12.7%) 15 (27.3%) |
2 (3.6%) 14 (25.5%) 8 (14.5%) 9 (16.4%) 12 (21.8%) 10 (18.2%) |
0.155 |
*- Physical component, ** - Mental component
In the index group, battery operated infusion pumps were used and no incidence of infusion pump failure was recorded.
Discussion
APS aims at regular detailed assessment of patient's pain mainly postoperative pain, pain management delivery using defined protocols, and different modalities. It also includes monitoring at regular intervals by trained personnel and documentation of records. Patients are also informed regarding pain, treatment modalities, and their side effects.[6] It started in the USA and then in Germany to every major hospital in UK. Moreover, provision of APS has become a prerequisite for accreditation for training by the Royal College of Anesthetists UK, Australian, and New Zealand College of Anesthetists.[11,12] At present, more than 95% of the hospitals have an APS in developed countries.[12]
However, the situation in developing countries is very different. After 3 decades, APS is still in an evolving stage in India. In 2015, a survey found that anesthesiologists were involved in managing postoperative pain in only 45% hospitals and there were only 68 APS centers. Out of 68 APS centers, 19 were thriving and 24 were struggling for their existence. The survey also concluded that administrative issues were considered as a major barrier in APS.[13] Despite APS, 60% respondents complained of moderate to severe pain in a survey.[14]
Therefore, regular surveys, quality assurance studies, and audits are required to evaluate the performance of APS; otherwise economic burden and administrative issues can threaten the existence of APS. Clinical audit is the backbone of good governance and aims to take a stock of the actual situation as it is at present.
To the best of our knowledge, only two centers in India including Tata Memorial Cancer Institute, Mumbai and Indian Spinal Injury Centre, New Delhi have published study about the performance of APS centers, but none using APS-POQ-R and SF-12.[13,15]
We used the instruments APS-POQ-R and SF-12 to evaluate the performance of our APS as these scales objectively measure six aspects of pain management and eight subdomains of physical and mental health, respectively. They are validated internationally, easy to administer, take a short time to complete, and comprehensively capture the variables relevant to patient perception of care, various aspects of pain control, patient satisfaction, and quality of life.[8,9,10,16]
Therefore, in this study, we compared patients' perception of care and health-related quality of life in orthopedic patients experiencing postoperative acute noncancer pain undergoing either APS care or routine care using APS-POQ-R and SF-12. We chose orthopedic surgery patients because studies demonstrate that 40%-70% of such patients experience moderate and severe postoperative pain.[17,18]
Patients' perception of care is a vital criterion and relevant outcome measure of pain management for healthcare institutions.[17] In our study, the index group scored significantly higher than control group on perception of care including pain relief, patient satisfaction score and participation in decisions. Miaskowski et al. also demonstrated that significant percentage of patients was more satisfied with APS care as compared to control group.[19] Ready also reported higher satisfaction rate of 89% with rating 8 or more with APS care in their large study of 6790 patients.[20] Our results are also supported by observations of Govind et al. and Farooq et al.[15,21] Patients' participation in decision making regarding pain management also leads to better pain relief and improve their satisfaction.[22] In our study, majority of patients (69%) found the information very helpful.
The worst pain level and time in severe pain are very important predictor of patient outcome.[8] In our study, in index group, there was significant reduction of worst pain in first 24 h (median 6; IQR 3-8) along with decreased frequency of severe pain (median 2; IQR 1-4; P < 0.001). Similarly, Miaskowski et al. also observed that patients experienced lesser worst pain with APS care.[19] Our results are favorable as compared to an Indian and UK survey of 14 hospitals in which 60% patients reported moderate to severe pain at 24 h.[14,23] Gould et al. also demonstrated that after APS care, there was significant reduction of resting Visual Analog Scale(VAS) from 45 (34-53) to 16 (10-20), during movement from 78 (66-80) to 46 (38-48) and during deep inspiration from 64 (48-78) to 46 (38-48).[24] Other studies also concluded that there was reduction in patients experiencing moderate to severe pain, which varied from 0% to 8--27% during rest and from 16% to 64% during activity.[25]
In the index group, there was also significant reduction of pain related interference with various activities including sleep, emotions, and decreased incidence of nausea. Our results are similar to study by Miaskowski et al., in which there was lesser frequency of nausea in hospitals with APS.[19]
According to a survey in the UK, overnight cover was only provided by 15% hospitals with only 29% hospitals with weekend cover and in Germany, only 45% hospitals fulfills the minimum quality criteria.[23,26,27] As per a survey in the United States, only 55% hospitals had written protocol.[28] In India, a survey found that 60% APS centers do not take regular postoperative rounds for assessment of pain and 50% centers do not have any written protocol. Only three have night APS services.[13] According to another multicentric survey in India, only two centers had APS according to set criteria.[29] In contrast, in our institute, we have a written protocol and minimum four rounds are taken by anesthesia residents with round-the-clock service including overnight and weekends. Written protocol is important so as to ensure uniformity and proper assessment of patients. APS of our institute is in congruence with the recommendations laid by faculty of pain medicine of the UK.[30]
Different APS models have been described. They include anesthesiologist-based, resident-based, and nurse-based models.[31] In our hospital, resident and APS nurse under supervision of consultant anesthesiologist-based model is being adopted.
With the availability of ultrasound, peripheral nerve stimulator, or loss of resistance techniques, various nerve plexuses involving upper and lower limbs, fascial plane blocks including the transversus abdominis plane, erector spinae, rectus sheath, and pectoral nerve blocks are widely used for pain management.[32] However, the question that whether the epidural analgesia can be replaced by other regional analgesic techniques is still unanswered.[12] In contrast, Govind et al. concluded that introduction of regional techniques either continuous or single shot in APS played a major role in improving the pain scores of the patient.[15] A good regional anesthesia service can be crucial to any APS as it provides timely application of appropriate pain relieving methods, which improves the overall postoperative pain management and patient's hospital experience.
The limitations in our study include lack of randomized allocation of patients to the two groups, relatively small sample size, inclusion of only orthopedic population, use of Hindi translated versions of APS-POQ-R and SF-12 in patients who did not understand English, and possible recall bias. The hurdles faced in implementing the APS, patient barriers to receive pain medications and timely delivery of intervention were not evaluated in this study.
Despite these limitations, we believe that our results justify the efforts and resources associated with the establishment and running of APS in our institute. Patients actually perceive the care they receive from APS as a satisfying experience as compared with control group. We recommend that to further improve the pain scores and satisfaction, recent regional techniques may also be included in APS along with central neuraxial techniques. There is also a need to increase the awareness about APS and different pain modalities among residents, surgical team, patients, and nursing staff.
Conclusion
Implementation of APS plays an important role in improving the quality of postoperative pain relief, perception of care, and patient satisfaction, thereby increasing the healthcare standards. Later studies with a randomized controlled design, larger sample size, and using a more detailed questionnaire can further add to the value of this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lippe PM, Brook C, David J, Crossno R, Gitlow S. The first national pain medicine summit - Final summary report. Pain Med. 2010;11:1447–68. doi: 10.1111/j.1526-4637.2010.00961.x. [DOI] [PubMed] [Google Scholar]
- 2.Pavlin DJ, Chen C, Penaloza DA, Polissar NL, Buckley FP. Pain as a factor complicating recovery and discharge after ambulatory surgery. Anesth Analg. 2002;95:627–34. doi: 10.1097/00000539-200209000-00025. [DOI] [PubMed] [Google Scholar]
- 3.Benhamou D, Berti M, Brodner G, DeAndres J, Draisci G, Moreno-Azzcoita M, et al. Postoperative analgesic therapy observational survey (PATHOS): A practice pattern study in 7 Central/Southern European countries. Pain. 2008;136:134–41. doi: 10.1016/j.pain.2007.06.028. [DOI] [PubMed] [Google Scholar]
- 4.Gan TJ, Habib AS, Miller TE, White W, Apfelbaum JL. Incidence, patient satisfaction, and perceptions of post-surgical pain: Results from a US national survey. Current Med Res Opin. 2014;30:149–60. doi: 10.1185/03007995.2013.860019. [DOI] [PubMed] [Google Scholar]
- 5.Vijayan R. Managing Acute Pain in Developing World Pain Clinical Updates. Seattle: IASP Press; 2011. [Google Scholar]
- 6.Kishore K, Agarwal A, Gaur A. Acute pain service. Saudi J Anaesth. 2011;5:123–4. doi: 10.4103/1658-354X.82777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bond MR, Charlton GE, Wolff C. Proceeding of the Sixth World Congress on Pain. New York: Elsevier; 1992. American Pain Society quality assurance standards for relief of acute pain and cancer pain; pp. 185–9. [Google Scholar]
- 8.Wang H, Sherwood G, Gong ZY, Liu HP. Psychometric evaluation of the revised American pain society patient outcome questionnaire (APS-POQ-R) in postoperative patients. FAM. 2013;20:285–91. [Google Scholar]
- 9.Gordon DB, Polomano RC, Pellino TA, Turk DC, McCracken LM, Sherwood G, et al. Revised American pain society patient outcome questionnaire (APS-POQ-R) for quality improvement of pain management in hospitalized adults: Preliminary psychometric evaluation. J Pain. 2010;11:1172–86. doi: 10.1016/j.jpain.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 10.Stewart A, Ware JE. Measuring functioning and well-being The Medical Outcomes Study Approach. Durham NC: Duke University Press; 1992. [Google Scholar]
- 11.Smith G, Power I, Cousins MJ. Acute pain: Is there scientific evidence on which to base treatment [editorial]? Br J Anaesth. 1999;82:817–9. doi: 10.1093/bja/82.6.817. [DOI] [PubMed] [Google Scholar]
- 12.Jain PN. Acute pain service: Round the clock vigilance. Indian J Anaesth. 2018;62:491–2. doi: 10.4103/ija.IJA_471_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain PN, Bakshi SG, Thota RS. Acute pain services in India: A glimpse of the current scenario. J Anesthesiol Clin Phamacol. 2015;31:554–5. doi: 10.4103/0970-9185.169088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jain PN, Myatra SN, Kakade AC, Sareen R. An evaluation of postoperative analgesia in acute pain service in an Indian cancer hospital (a preliminary experience of patient satisfaction survey) Acute Pain. 2008;10:9–14. [Google Scholar]
- 15.Govind P, Bhakta P, Dureja GP, Gupta A, Venkataraju A. Acute pain service: The journey in a developing country setting. Acta Anaesthesiol Scand. 2015;59:98–106. doi: 10.1111/aas.12434. [DOI] [PubMed] [Google Scholar]
- 16.Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: Results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:1171–8. doi: 10.1016/s0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 17.Ramia E, Nasser S, Salameh P, Saad AH. Patient perception of acute pain management: Data from three tertiary care hospitals. Pain Res Manag. 2017;2017 doi: 10.1155/2017/7459360. Article ID 7459360, 12 pages doi: 101155/2017/7459360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sommer M, De Rijke JM, Kleef VM. The prevalence of postoperative pain in a sample of 1490 surgical inpatients. Eur J Anaesthesiol. 2008;25:267–74. doi: 10.1017/S0265021507003031. [DOI] [PubMed] [Google Scholar]
- 19.Miaskowski C, Crews J, Ready LB. Anaesthesia based pain services improve the quality of postoperative pain management. Pain. 1999;80:23–9. doi: 10.1016/s0304-3959(98)00192-4. [DOI] [PubMed] [Google Scholar]
- 20.Ready LB. Acute pain: Lessons learned from 25000 patients. Reg Anesth Pain Med. 1999;11:583–9. doi: 10.1016/s1098-7339(99)90038-x. [DOI] [PubMed] [Google Scholar]
- 21.Farooq F, Khan R, Ahmed A. Assessment of patient satisfaction with acute pain management service: Monitoring quality of care in clinical setting. Indian J Anaesth. 2016;60:248–52. doi: 10.4103/0019-5049.179450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zoega S, Sveinsdottir H, Sigurdsson GH, Aspeund T, Ward SE, Gunnarsdottir S. Quality pain management in the hospital setting from patients perspective. Pain Pract. 2015;15:236–46. doi: 10.1111/papr.12166. [DOI] [PubMed] [Google Scholar]
- 23.Moss E, Taverner T, Norton P, Lesser P, Cole P. A survey of postoperative pain management in fourteen hospitals in the UK. Acute Pain. 2005;7:12–20. [Google Scholar]
- 24.Gould TH, Upton PM, Collins P. A survey of the intended management of acute postoperative pain by newly qualified doctors in south west region of England in August 1992. Anaesthesia. 1994;49:807–10. doi: 10.1111/j.1365-2044.1994.tb04459.x. [DOI] [PubMed] [Google Scholar]
- 25.Werner MU, Soholm L, Nielsen PR. Does an acute pain service improve postoperative outcome? Anesth Analg. 2002;95:1361–72. doi: 10.1097/00000539-200211000-00049. [DOI] [PubMed] [Google Scholar]
- 26.Rockett M, Vanstone R, Chand J, Waeland D. A survey of acute pain services in the UK. Anaesthesia. 2017;72:1237–42. doi: 10.1111/anae.14007. [DOI] [PubMed] [Google Scholar]
- 27.Erlenwein J, Koschwitz R, Pauli-Magnus D, Quintel M, Meißner W, Petzke F, et al. Afollow-up on Acute Pain Services in Germany compared to international survey data. Eur J Pain. 2016;12:874–83. doi: 10.1002/ejp.812. [DOI] [PubMed] [Google Scholar]
- 28.Nasir D, Howard JE, Joshi GP, Hill GE. A survey of acute pain service structure and function in United States hospitals? Pain Res Treat. 2011;2011:934932. doi: 10.1155/2011/934932. doi: 10.1155/2011/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khatib SK, Razvi SS, Kulkarni SS, Parab S. A multicentre survey of the current acute post-operative pain management practices in tertiary care teaching hospitals in Maharashtra. Indian J Anaesth. 2017;61:215–24. doi: 10.4103/ija.IJA_506_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rcoa.ac.uk. Core standards for pain management in UK.[online] [Last accessed on 2018 Dec 07]. Available from: http://www.rcoa.ac.uk/system/files/FPM-CSPMS-UK2015.pdf .
- 31.Borracci T, Prencipe D, Masotti A, Nella A, Tuccinardi G, Margiacchi L, et al. The experience of setting up a resident-managed Acute Pain Service: A descriptive study. BMC Anesthesiol. 2016;16:14. doi: 10.1186/s12871-016-0179-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wahal C, Kumar A, Pyati S. Advances in regional anaesthesia: A review of current practice, newer techniques and outcomes. Indian J Anaesth. 2018;62:94–102. doi: 10.4103/ija.IJA_433_17. [DOI] [PMC free article] [PubMed] [Google Scholar]


