Abstract
Background and Aims:
The role of cervical epidural analgesia in head and neck cancer surgery is not fully explored. The aim of this study was to evaluate cervical epidural analgesia in terms of opioid and anesthetic requirements and stress response in patients undergoing head and neck cancer surgery.
Material and Methods:
After institutional ethical committee approval and written informed consent, 30 patients undergoing elective head and neck cancer surgery were randomized into two groups: Group E (cervical epidural analgesia with general anesthesia), and group G (general anesthesia alone). In group E, an 18 gauge epidural catheter was placed at cervical (C) 6 – thoracic (T) 1 level. After test dose, a bolus of 10 ml of 0.2% ropivacaine was given followed by continuous infusion. Technique of general anesthesia and post-operative management was standardized in both the groups. Opioid and anesthetic drug requirement was observed. Blood glucose and serum cortisol levels were measured at baseline; post-incision and after surgery.
Results:
There was significant reduction in the requirement of morphine (P < 0.001), isoflurane (P = 0.004) and vecuronium (P = 0.001) in group E. Post-operative, blood glucose and serum cortisol levels were significantly reduced (P = 0.0153 and 0.0074, respectively). Early post-operative pain was reduced with the lesser requirement of post-operative morphine.
Conclusions:
The use of combined cervical epidural analgesia with general anesthesia reduces opioid, anesthetic drug requirement and stress response as compared to general anesthesia alone in patients undergoing head and neck cancer surgery.
Keywords: Anesthesia techniques, cancer surgery, cervical epidural, stress response
Introduction
General anesthesia is the technique of choice for head and neck cancer surgery. Regional anesthesia techniques for head and neck cancer surgery include the use of cervical epidural anesthesia as a sole technique[1,2,3] or cervical epidural analgesia for pain management.[4]
Recent studies indicate that the use of regional anesthesia techniques may benefit patients undergoing laryngeal and hypo-pharyngeal cancer surgery.[5] Proposed mechanisms include reduced anesthetic requirements and neuro-endocrine stress response.[6]
However, randomized trials evaluating the role of cervical epidural anesthesia/analgesia on opioid, anesthetic requirements and stress response in head and neck cancer surgery are lacking. Our hypothesis is that the use of cervical epidural analgesia may reduce opioid, anesthetic requirements and stress response in head and neck cancer surgery and these parameters were evaluated in this study.
Material and Methods
This study was approved by institutional ethics committee, and written informed consent was taken from all the patients.
This study included American Society of Anesthesiologist status I and II patients of either sex, aged between 18 and 65 years undergoing elective head and neck cancer surgery. Patients having infection at local site and coagulopathy were excluded from the study.
This was an open label study. Patients were allocated randomly into two groups of 15 patients each: Group E (received combined cervical epidural analgesia with general anesthesia), and group G (received general anesthesia alone). Method of randomization used was computer-generated random number sequence. Method of concealment used was sequentially numbered opaque envelopes.
All patients were pre-medicated with ranitidine 150 mg and alprazolam 0.25 mg the night before surgery and 2 h before surgery with sips of water. Inside the operation theatre, an intravenous line was secured and ringer lactate infusion was started. All patients were monitored with electrocardiogram, non-invasive blood pressure, oxygen saturation, end-tidal carbon dioxide (EtCO2), temperature, end-tidal isoflurane concentration analyzer and neuromuscular monitoring done using nerve stimulator.
In group E, cervical epidural catheter was inserted in an operating room. Cervical epidural was placed at C 6 – T1 level in a sitting position with neck flexion. Epidural space was identified by using the loss of resistance to air technique. Epidural catheter (18 G) was placed 3-4 cm into the epidural space. A test dose of 3 ml of 2% lignocaine with epinephrine (1:200,000) was given for confirmation. For analgesia, 10 ml of 0.2% ropivacaine was given as bolus dose followed by 0.2% ropivacaine infusion at a rate of 5 ml/h. After 10 min of injection of ropivacaine, general anesthesia was induced.
Patients in both the groups received general anesthesia using the same technique. Anesthesia was induced with morphine 0.1 mg kg-1 followed by propofol 1.5-2 mg kg-1 till the loss of verbal response. To facilitate naso-tracheal intubation, succinylcholine 1.5-2 mg kg-1 was given. Maintenance of anesthesia was done using nitrous oxide in oxygen and isoflurane (end tidal concentration 0.8-1.2%). For top-up doses of vecuronium, neuromuscular monitoring was done using train of four responses.
Intra-operative, systolic blood pressure (SBP) and heart Rate (HR) >20% of the baseline was treated by morphine 3 mg intravenous (IV) bolus and/or increasing depth of anaesthesia (end tidal isoflurane concentration 1.5-2%).
Morphine, vecuronium and anesthetic agent requirements (end tidal isoflurane concentration) were noted.
If any of the patients developed bradycardia (HR <40 per min), injection atropine was used for treatment. In the case of hypotension (SBP <40% of baseline), fluid bolus was given. If necessary, mephentermine 3 mg bolus was given. Atropine and mephentermine requirement were noted.
A venous sample (5 ml) was taken for blood glucose measurements and serum cortisol levels at baseline, 30 min after incision, 60 min after surgery.
Fluid management was done as per standard protocol being followed for these procedures. Blood transfusion was given when blood loss exceeded the allowable blood loss for the particular patient.
Study lasted till 6 h post-operatively and during this period, patients were nursed in the high dependency unit. Vital signs (heart rate, blood pressure and respiratory rate) were monitored. Epidural infusion was discontinued in group E, and all patients received background morphine infusion at the rate 0.01 mg kg-1 h-1. All patients received IV paracetamol 1g at the end of surgery and thrice a day, thereafter. Patients were assessed for pain at 2, 4 and 6 h using a standard visual analogue scale (VAS). Morphine 3 mg IV bolus was given when VAS >3. Post-operative morphine requirement was recorded. Patient's were monitored for any sedation and/or respiratory depression.
Statistical analysis
Sample size calculation was based on morphine requirement in the two groups. In the pilot study, morphine requirement in the group G was found to be 7.6, and in the group E, it was 6.5 with a standard deviation of 0.95. By taking power at 85% and alpha error at 0.5, a sample size of 14 patients each was calculated.
To even out the sample size, 15 patients in each group were enrolled.Data were summarized as mean and standard deviation. T-test and Mann-Whitney test was used to analyse morphine, vecuronium and isoflurane requirement (Primary outcome). Blood glucose and serum cortisol levels (secondary outcomes) were analysed by two-way analysis of variance (ANOVA) test for repeated measures with post-hoc Bonferroni correction. Graph pad prism version 15 software was used to analyze the data.
Results
A total of 30 patients were enrolled for the study. Out of which, 15 patients in group G and 14 patients in group E completed study. One patient in group E could not complete the study due to failure to place epidural catheter. Type of surgery included oral, hypo-pharyngeal and laryngeal cancers. Patient characteristics are summarized in Table 1.
Table 1.
Patient characteristics, surgical and epidural data*
| Group G | Group E | |
|---|---|---|
| Age (yr) | 51.6±7.1 | 49.8±8.9 |
| Weight (kg) | 63.8±7.0 | 62.1±7.1 |
| Sex (M/F) | 10/5 | 9/5 |
| Oral/Hypopharyngeal/Laryngeal cancer | 4/9/2 | 5/8/1 |
| Duration of surgery (h) | 5.96±0.51 | 6.06±0.94 |
| Ropivacaine used (mg) | Not applicable | 87.13±9.28 |
*Data expressed as mean±SD and n. No significant difference observed between the two groups
There was significantly lower consumption of morphine (P < 0.0001), isoflurane (P = 0.004) and vecuronium (P = 0.001) in group E compared with the group G as shown in Table 2.
Table 2.
Opioid and anesthetic agent requirement data*
| Group G | Group E | Mean difference (95% CI) | P | |
|---|---|---|---|---|
| Morphine (mg) | 8.9±0.95 | 7.1±1.02 | 1.8 (-2.41 to 1.18) | <0.0001 |
| End-tidal Isoflurane (%) | 1.7±0.3 | 1.4±0.2 | 0.3 (-0.45 to 0.14) | 0.004 |
| Vecuronium (mg/h-1) | 2.9±0.79 | 1.4±0.48 | 1.5 (-1.90 to 1.09) | 0.001 |
*Data expressed as mean±SD
Mean dose of ropivacaine used in group E was found to be 87.13 ± 9.28 [Table 1].
No statistically significant difference was found in baseline and post-incision blood glucose levels. Post-operative glucose levels were found to be lower in group E [Figure 1].
Figure 1.
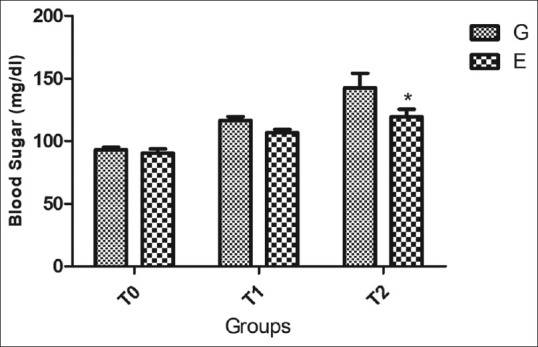
Blood sugar levels measured at three different time points (T0 – baseline, T1 – 30 minutes after incision, T2 – 60 min after surgery). Difference found to be significant at T2 (*P = 0.015)
No statistically significant difference was found in baseline and post-incision serum cortisol levels. Post-operative serum cortisol levels were found to be lower in group E [Figure 2].
Figure 2.
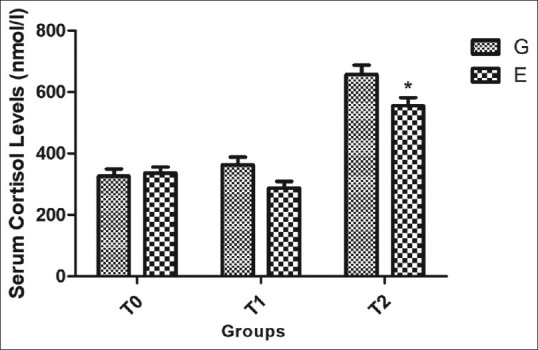
Serum cortisol levels measured at three different time points (T0 – baseline, T1 – 30 min after incision, T2 – 60 min after surgery). Difference found to be significant at T2 (*P = 0.0074)
Mean VAS scores were found to be 2.84, 2.94, 2.7 (group E) vs. 3.58, 3.32, 3.12 (group G) at 2, 4 and 6 hpost-operatively. Difference was found to be statistically significant at 2 h (P = 0.004). Post-operative morphine IV bolus requirement was found to be significantly lower in group E [Figure 3].
Figure 3.
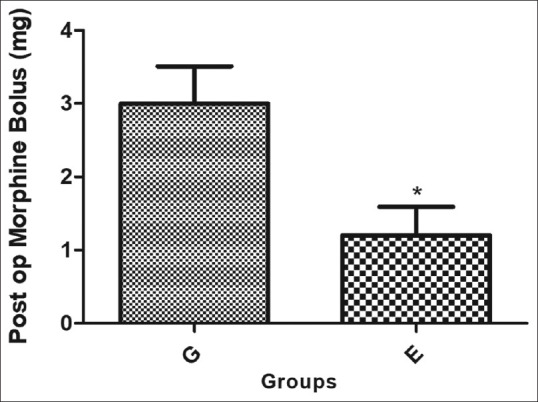
Post-operative morphine requirement (*P value 0.01)
No statistically significant difference was observed in the hemodynamic parameters. In group E, incidence of bradycardia was 6.6%. Hypotension at induction was seen in 13.3%. of the patients.
Discussion
Promising effects of regional anesthesia techniques in cancer surgery have revived interest in cervical epidural anesthesia and analgesia techniques for head and neck cancer patients. Use of regional anesthesia techniques as a part of balanced anesthesia may help to counteract immunosuppressive effects of pain and neuro-endocrine stress response.[7]
Our study compares combined cervical epidural analgesia and general anesthesia with general anesthesia alone in patients undergoing head and neck cancer surgery.
Our study demonstrates that the use of cervical epidural analgesia reduces morphine, isoflurane and vecuronium requirements. Stress response in terms of blood glucose and serum cortisol levels was seen to be less in the immediate post-operative period. Early post-operative pain is reduced with the lesser requirement of post-operative morphine.
The combined use of cervical epidural and general anesthesia in the carcinoma of neck has been studied and results show that it helps to stabilize hemodynamics during cervical surgery.[8]
Results of our study are comparable to previous studies that demonstrate reduced neuro-endocrine stress response with the use of thoracic epidural techniques in patient undergoing major abdominal surgeries. Use of thoracic epidural led to reduced consumption of opioids, inhalational agent along with inhibition of stress response (blood glucose and serum cortisol levels) in the peri-operative period.[9,10,11]
Effect of cervical epidural anesthesia on stress response was evaluated by Nakamura et al. in patients undergoing upper arm surgeries. There was incomplete abolition of stress response with cervical epidural anesthesia in terms of blood glucose levels and insulin secretion.[12]
In our study, we used ropivacaine as the local anesthetic as it produces less intense motor block as compared to bupivacaine. Lower concentration of ropivacaine (0.2%) was used as intended for analgesia purposes.
Effects of bupivacaine and ropivacaine have been compared in patients undergoing modified radical mastectomy under cervical epidural anesthesia. Authors concluded that ropivacaine is a safer option in view of less motor blockade and less effect on respiratory parameters.[13] Use of 0.2% ropivacaine has been found to be very effective in continuous thoracic epidural anesthesia in patients undergoing modified radical mastectomy for breast cancer.[14]
A bolus of 10 ml of ropivacaine was given based on previous reports that show that a volume of 10 ml of ropivacaine through cervical epidural at C 6-7 level achieves block at C2-T10 levels.[15]
Hong et al. studied effects of local anesthetics and opioids in cervical epidural anesthesia. They observed that combining local anesthetics and fentanyl can produce hemodynamic and ventilatory side effects. Hence, the use of epidural opioids was avoided in our study.[16]
In our study, both the groups received IV morphine and IV paracetamol for post-operative analgesia. Post-operative VAS score was found to be reduced at 2 h with reduced post-operative morphine requirement in group E.
In a previous study, authors demonstrate better analgesia at rest (reduced VAS score) in the first 6 h after surgery with administration of fentanyl using cervical epidural route as compared to IV route in patients undergoing pharyngolaryngeal surgery. Total fentanyl dose requirement was found to be similar in both the groups.[6]
Lower post-operative morphine requirement observed in our study may be due to use of multi-modal analgesia (epidural analgesia, opioids and paracetamol) in the epidural group. Epidural use was pre-emptive and was not continued in the post-operative period.
Above findings of our study match with the results of a study by Amiri et al. suggesting that the use of multi-modal analgesic technique using combination of drugs reduce post-operative pain scores and opioid consumption in patients undergoing radical neck dissection.[17]
In the cervical epidural with general anesthesia group (group E), one patient developed bradycardia, which responded to atropine and two patients developed hypotension at induction which responded to fluid boluses. There were no other side effects associated with the use of cervical epidural.
Previous studies using cervical epidural anesthesia for neck and arm surgery show that the incidence of hypotension and bradycardia is 20-30% and is easily treatable.[18]
Anesthestic dose of local anesthetics is associated with motor block of upper extremities with decrease in ventilatory parameters in the post-operative period. This decrease is proportionate to concentration of local anesthetic used.[19,20]
In our study, although we did not measure ventilatory parameters, they are unlikely to be affected as only lower concentration of local anesthetic intended for analgesia was used, no opioids were added and epidural infusion of ropivacaine was discontinued in the post-operative period.
Limitations of our study include small sample size, titration of anesthetic drugs was based on hemodynamic parameters (non-invasive blood pressure and heart rate) and observer bias cannot be ruled out as blinding was not possible in this study. Also, epidural use was limited to intra-operative period and no follow up was done for cancer recurrence or metastasis.
Conclusion
The use of combined cervical epidural analgesia with general anaesthesia reduces opioid, anesthetic drug requirement and stress response as compared to general anesthesia alone in patients undergoing head and neck cancer surgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We thank Dr Sudhir Bahadur (Professor and ex-head of Department of ENT, Hamdard Institute of Medical Sciences and Research, New Delhi, India) for his valuable guidance.
References
- 1.Cata JP, Zafereo M, Villarreal J, Unruh BD, Truong A, Truong DT, et al. Intraoperative opioids use for laryngeal squamous cell carcinoma surgery and recurrence: A retrospective study. J Clin Anaesth. 2015;27:672–9. doi: 10.1016/j.jclinane.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 2.Merquiol F, Montelimard AS, Nourissat A, Molliex S, Zufferey PJ. Cervical epidural anaesthesia is associated with increased cancer-free survival in laryngeal and hypo pharyngeal cancer surgery: A retrospective propensity-matched analysis. Reg Anesth Pain Med. 2013;38:398–402. doi: 10.1097/AAP.0b013e31829cc3fb. [DOI] [PubMed] [Google Scholar]
- 3.Patel MG, Swadia VN. Cervical epidural anaesthesia for various neck surgeries. J Anaesthesiol Clin Pharmacol. 2009;25:297–30. [Google Scholar]
- 4.Wittich DJ, Jr, Berny JJ, Davis RK. Cervical epidural anesthesia for head and neck surgery. Laryngoscope. 1984;94:615–9. [PubMed] [Google Scholar]
- 5.Mulimani SM, Talikoti DG. Cervical epidural analgesia in a case of oral cancer undergoing reconstructive surgery. Indian J Anaesth. 2011;55:528–9. doi: 10.4103/0019-5049.89897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roussier M, Mahul P, Pascal J, Baylot D, Prades JM, Auboyer C, et al. Patient-controlled cervical epidural fentanyl compared with patient-controlled iv fentanyl for pain after pharyngolaryngeal surgery. Br J Anaesth. 2006;96:492–6. doi: 10.1093/bja/ael025. [DOI] [PubMed] [Google Scholar]
- 7.Sekandarzad MW, van Zundert AAJ, Lirk PB, Doornebal CW, Hollmann MW. Perioperative anaesthesia care and tumour progression. Anesth Analg. 2017;124:1697–708. doi: 10.1213/ANE.0000000000001652. [DOI] [PubMed] [Google Scholar]
- 8.Arakawa M, Amemiya N, Nagai K, Kato S, Goto F. Effects of epidural analgesia combined with general anesthesia on hemodynamics during neck surgery. Masui. 1993;42:1464–9. [PubMed] [Google Scholar]
- 9.Ahlers O, Nachtigall I, Lenze J, Goldmann A, Schulte E, Höhne C, et al. Intraoperative thoracic epidural anaesthesia attenuates stress-induced immunosuppression in patients undergoing major abdominal surgery. Br J Anaesth. 2008;101:781–7. doi: 10.1093/bja/aen287. [DOI] [PubMed] [Google Scholar]
- 10.Atia AM, Abdel-Rahman KA. Combined thoracic epidural with general anaesthesia vs. general anaesthesia alone for major abdominal surgery: Anaesthetic requirements and stress response. J Anesth Clin Res. 2016;7:616. [Google Scholar]
- 11.Fant F, Tina E, Sandblom D, Andersson SO, Magnuson A, Hultgren-Hörnkvist E, et al. Thoracic epidural analgesia inhibits the neuro-hormonal but not the acute inflammatory stress response after radical retropubic prostatectomy. Br J Anaesth. 2013;110:747–57. doi: 10.1093/bja/aes491. [DOI] [PubMed] [Google Scholar]
- 12.Nakamura S, Shigemastu A. Influence of cervical epidural anaesthesia on glucose disappearance and insulin secretion. Masui. 1981;30:967–72. [PubMed] [Google Scholar]
- 13.Kulkarni K, Namazi IJ, Deshpande S, Goel R. Cervical epidural anaesthesia with ropivacaine for modified radical mastectomy. Kathmandu Univ Med J. 2013;11:126–31. doi: 10.3126/kumj.v11i2.12487. [DOI] [PubMed] [Google Scholar]
- 14.Doss NW, Ipe J, Crimi T, Rajpal S, Cohen S, Fogler RJ, et al. Continuous thoracic epidural anaesthesia with 0.2% Ropivacaine versus general anaesthesia for perioperative management of modified radical mastectomy. Anesth Analg. 2001;92:1552–7. doi: 10.1097/00000539-200106000-00041. [DOI] [PubMed] [Google Scholar]
- 15.Michalek P, David I, Adamec M, Janousek L. Cervical epidural anesthesia for combined neck and upper extremity procedure: A pilot study. Anesth Analg. 2004;99:1833–6. doi: 10.1213/01.ANE.0000137397.68815.7B. [DOI] [PubMed] [Google Scholar]
- 16.Hong JG, Lee C, Park CH, Kim WT. Bupivacaine versus bupivacaine fentanyl for cervical epidural anesthesia. Korean J Anesthesiol. 1997;32:44–50. [Google Scholar]
- 17.Amiri HR, Mirzaei M, Beig Mohammadi MT, Tavakoli F. Multi-modal pre-emptive analgesia with pregabalin, acetaminophen, naproxen, and dextromethorphan in radical neck dissection surgery: A randomized clinical trial. Anesth Pain Med. 2016;6:e33526. doi: 10.5812/aapm.33526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agarwal M, Kang LS. Cervical epidural analgesia for neck arm and upper thoracic surgery. J Anaesthesiol Clin Pharmacol. 2010;26:189–92. [Google Scholar]
- 19.Capdevila X, Biboulet P, Rubenovitch J, Serre-Cousine O, Peray P, Deschodt J, et al. The effects of cervical epidural anaesthesia with bupivacaine on pulmonary function in conscious patients. Anesth Analg. 1998;86:1033–8. doi: 10.1097/00000539-199805000-00024. [DOI] [PubMed] [Google Scholar]
- 20.Jain G, Bansal P, Garg GL, Singh DK, Yadav G. Comparison of three different formulations of local anaesthetics for cervical epidural anaesthesia during thyroid surgery. Indian J Anaesth. 2012;23:7–10. doi: 10.4103/0019-5049.96306. [DOI] [PMC free article] [PubMed] [Google Scholar]


