ABSTRACT
Background
Antimicrobial resistance (AMR) is a major global public health issue. In India, access to medicines is poorly regulated and therefore antibiotics in dairy cattle are commonly used by farmers without consulting with veterinarians. This study was conducted to understand practices and knowledge related to antibiotic use and AMR among dairy farmers and veterinary professionals in selected urban and peri-urban areas of India.
Methods
A total of 28 focus group discussions with farmers and 53 interviews with veterinary professionals were carried out.
Results
Mastitiswas identified as the main animal health challenge. Antibiotic consultation behavior of farmers depended on the availability of veterinarians. Except in Bangalore, farmers were found to often treat animals on their own. They were found unaware of the concept of AMR, but knew the importance of vaccination. Veterinarians included in the study had a good understanding of antibiotics, AMR, and zoonotic diseases.
Conclusion
The knowledge level and practices observed in the study related to the use/abuse of antibiotics can potentially increase the risk of development of AMR and its transfer in the community. Our findings can help support AMR – mitigation efforts in the country, including the design of better policies on antibiotic use in dairy.
KEYWORDS: Antibiotics, antimicrobial resistance, dairy farmer, veterinary, animal health, zoonotic, qualitative, dairy production, knowledge, attitudes, practices
Background
Antimicrobial resistance (AMR) is an emerging public health issue globally, but the problem may even be more serious in developing countries like India. India has a high burden of infectious diseases and the uncontrolled access to medicines may lead to higher consumption and inappropriate use, and subsequently result in higher levels of resistance [1,2].
India leads in the global production of milk and milk products, and the country`s annual output of about 146 million ton accounts for 18.5% of the global output [3]. The increasing demand for milk and other animal-source foods has given rise to an increasing number of small-scale farms that operate on minimal input costs, often occupying less than 1 ha and utilizing family labor. Quality control is minimal, and the infrastructure is poor. In order to satisfy the increasing demand, the farmers often follow practices that may result in adverse public health impacts. One such practice is the non-therapeutic, irrational use of antibiotics in farm animals [3].
Antibiotics are widely used in milk-producing animals for both therapeutic and prophylactic purposes. Antimicrobial use may lead to the development of resistant bacteria, which may be transferred to humans through a number of pathways, including consumption of food, direct contact with food-producing animals, or through environmental spread including animal sewage and runoff water from agricultural sites [4]. In 2010, India was estimated to account for 3% of the global antibiotic consumption in food animal production, the fourth highest in the world [5].
Since the 1980s, studies in India have consistently shown that a large proportion of the tested milk samples contains antibiotic residues. Evidence on the drivers and determinants of antibiotic use in Indian dairy farms is lacking [3]. In addition, dairy farmers,’ paravets’ (frontline veterinary workers who hold a diploma in veterinary and animal husbandry and are primarily responsible for vaccination, artificial insemination, pregnancy diagnosis, minor treatments), and veterinarians’ knowledge on antibiotics and antimicrobial resistance has also not been studied. This study was conducted to try to understand practices and knowledge of dairy farmers, paravets and veterinarians on antibiotics use and AMR, and understand determinants of antibiotic use in dairy farms.
Methodology
Ethical permission
The study was approved by the Institutional Research Ethics Committee (IREC) at the International Livestock Research Institute (ILRI), ILRI-IREC 2018–25. All the participants (farmers, veterinarians, paravets) were informed about the study and consented to participate and for the data to be published. Verbal informed consent was obtained prior to the group discussions.
Study areas
The study was conducted in 2018, during the months of September and October, and covered urban and peri-urban areas of Guwahati (in Assam), Karnal (in Haryana), Bangalore (in Karnataka), and Kolkata (in West Bengal) (Figure 1). In each site, a total of eight villages (four urban and four rural) were included in the study. In Kolkata, four villages were selected (two rural and two urban). Villages in Karnal and Guwahati had randomly been selected to participate in previous studies [6,7]. In addition, two more regions Bangalore (Karnataka) and Kolkata (West Bengal) were added to increase number of states. Locations were not selected randomly. In Bangalore and Kolkata, a list of villages near the district headquarters was prepared; the ones to include in the study were randomly selected from this list. All the dairy farmers, veterinarians, and paravets in the study regions were included in the study and those consented to participate were a part of the discussions.
Figure 1.
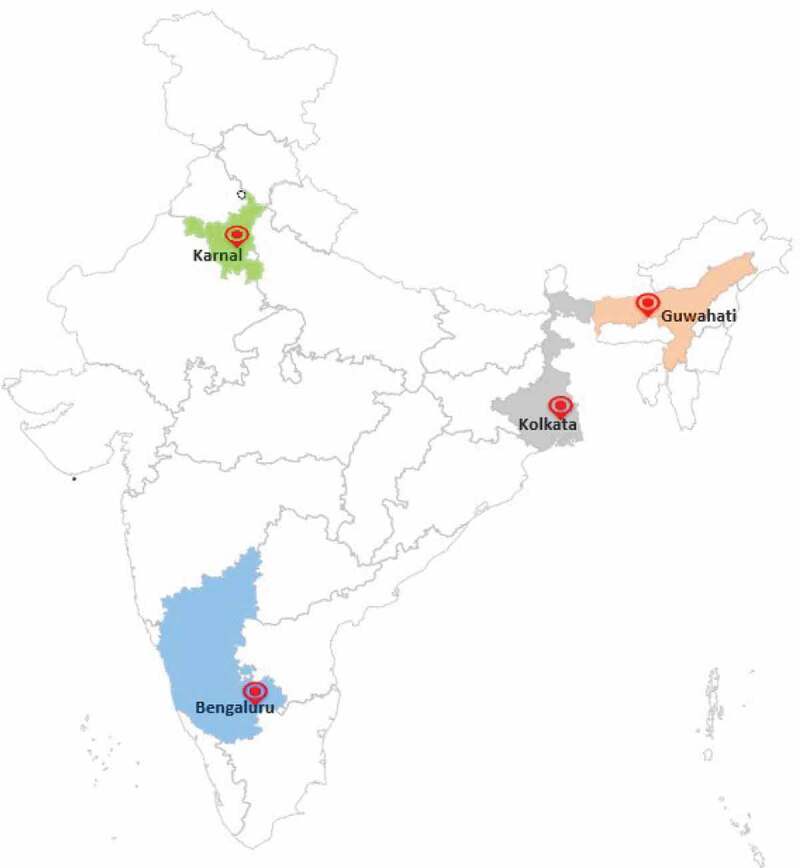
Showing the study sites.
Data collection
The study had two components, focus group discussions (FGD) with farmers and key informant interviews (KII) with animal health service providers (veterinarians and paravets). Study villages were identified as described above. For each site, we developed a schedule showing the dates when each village was to be visited. The schedule was communicated to veterinarians in charge of the villages, who, in turn, and through the paravets, arranged for a venue and consulted with the farmers to confirm their availability on the proposed dates. The local veterinary office also helped organize the village meetings, about 10–20 farmers were identified and invited to the meetings. Farmers needed to own at least one dairy animal (cow or buffalo) at the time of the study, to qualify as participants. FGD tool containing the key questions and probes (supplementary material 1) developed for the study was used to guide the discussions. All discussions were led by a moderator and were conducted in local languages: Assamese (in Guwahati), Hindi (in Karnal), Kannada (in Bangalore), and Bengali (in Kolkata). Sessions lasted for about 1–1.5 hours and were voice recorded. In addition, an assistant helped taking notes during the meetings. Similarly, KII tools containing the key questions and probes (supplementary material 2,3) were developed for the study to guide the interviews with veterinarians and paravets. We interviewed the veterinarians responsible for each village and 1–2 paravets.
The FGD guide was designed to capture data on animal health problems, the use of antibiotics, health consultation patterns, knowledge on zoonotic diseases, and disease control measures undertaken by farmers in the villages. The KIIs focused on disease control measures, their knowledge/practices on antibiotics and AMR, and zoonotic diseases that were thought to be frequent in the villages.
Data analysis
The audio recordings and field notes from FGDs and KIIs were translated and the resulting transcripts analyzed as described below:
Listing of codes: transcripts were read multiple times (by the first author) and this ensured a better understanding of the data. Participant response was enlisted, and codes generated for each of the responses. In the process, important statements, or quotes, with their references, were identified and extracted.
Categorization of codes: Codes with similar or comparable meanings were merged and placed under one category.
Generation of themes and sub-themes: The categories representing a similar idea came under one core-theme. Sub-themes were generated under each core theme. The responses were suitably placed for analysis under the core-themes and sub-themes.
Results
A total of 28 FGDs were conducted. In Karnal (Haryana) and Guwahati (Assam) participants were mostly men and only a few women, while in Bangalore (Karnataka) and Kolkata (West Bengal) almost an equivalent no. of men and women participated in the discussions. A total of 53 KII (including 29 (only men) with paravets and 24 with veterinarians (5 women and 19 men) ) were conducted across the four regions Table 1) describes no. of FGDs and KIIs conducted in each study region.
Table 1.
Description of the number of FGDs and KII`s conducted in Guwahati, Karnal, Bangalore, and Kolkata (September–October 2018).
| Study areas | FGDs with dairy farmers | KII |
|
|---|---|---|---|
| Veterinarians | Paravets | ||
| Guwahati | 8 | 7 | 9 |
| Karnal | 8 | 6 | 8 |
| Bangalore | 8 | 8 | 8 |
| Kolkata | 4 | 3 | 4 |
The results are summarized into five core themes (i.e. those that emerged from insights and perceptions of the stakeholders: farmers, veterinarians, and paravets) (Table 2).
Table 2.
Core themes and sub-themes.
| Core themes | Sub-themes |
|---|---|
| Animal health concerns |
|
| Veterinary consultation |
|
| Antibiotic use and knowledge on anti-microbial resistance |
|
| Zoonotic diseases |
|
| Vaccination |
|
CORE THEME 1: animal health concerns
Common issues and diseases
In all study areas, both farmers and field veterinarians identified mastitis as the main health problem in dairy animals. Foot and mouth disease (FMD) was also perceived to be common. Additional health issues observed by the veterinarians were; repeat breeding, abortion, metritis, dystocia, ruminal tympany (or bloat), milk fever (or hypocalcemia), diarrhea, hemorrhagic septicemia (HS), babesiosis, theileriosis, indigestion, allergies, and tick infestation.
“Mastitis is the main problem. Udder becomes tight and warm to touch and blood comes out of teats on milking.”- (Dairy farmer, Guwahati)
“My animals frequently suffer from FMD. It occurs every year and I don’t know how to save my animals from it.”- (Dairy farmer, Bangalore)
Causes of disease
Poor hygiene was reported to be the one primarily responsible for disease occurrence. In Guwahati, farmers associated diseases to floods and changes in local weather, while in Karnal, farmers linked the disease to their failure to timely vaccinate animals against diseases (FMD, HS, Black quarter (BQ)), and also to the non-availability of proper feeds. One farmer was concerned about animals kept in enclosures. Flies (including mosquitoes) were a concern for farmers in Kolkata. Lack of proper feeding, poor ventilation in animal sheds, mineral deficiency, and presence of dogs and cats was the reasons given by farmers in Bangalore.
“When high milk producing cows lies down, teat opens due to pressure, so the bacteria enter through the pores in the teat causing infection.”- (Dairy farmer, Bangalore)
CORE THEME 2: veterinary consultation
Consultation behavior of the farmers
Consultation behavior was related to the availability of veterinarians (Table 4). In Karnal, farmers relied on private veterinarians to attend to their sick animals. The consultation fee of private veterinarians was perceived to be high. Farmers in Guwahati and Karnal reportedly used home remedies to treat sick animals or sometimes relied on old prescriptions to access medicines. Paravets and veterinarians were only called after the health problem persisted. In Kolkata, farmers relied either on homeopathic practitioners (or ‘quacks’) to have their animals treated or consulted local pharmacists for advice on the particular drugs they needed to buy, given the case description. Table 3 gives a description of various animal health seeking options by the dairy farmers and the legal standing on the use of the antibiotics.
Table 4.
Availability of veterinarians and consultation behavior according to dairy farmers in Karnal, Kolkata, Bangalore, and Guwahati (September–October 2018).
| Site | Access to veterinary services | Animal health seeking behavior of dairy farmers |
|---|---|---|
| Karnal | Low | Consult private veterinary practitioners (consultation fees of USD 3–13). Consult veterinarian on the phone if not able to come to farm. Use home remedies. |
| Kolkata | Low | Consult local pharmacists, or homeopathic practitioners, ‘quacks’. Consult veterinarians if available. Use home remedies. |
| Bangalore | High | Consult veterinarians from Karnataka milk federation (KMF) or state veterinarians. Use home remedies. |
| Guwahati | Low | Use ‘old prescriptions’; home remedies. Consult private veterinary practitioners. Consult paravet or veterinarian if problem persisted. Consult veterinarian on the phone if not able to come to farm. |
Table 3.
Animal health-seeking options by the dairy farmers in the study areas in India and the legal standing on the use of antibiotics.
| Source of treatment | Definition | Legal possibilities for each category of persons to prescribe antibiotics | Actual prescription made by each category of persons, regardless of legal constraints |
|---|---|---|---|
| Government veterinarian | University trained veterinarian working for state government. | Yes | Yes |
| Private veterinarian | University trained veterinarian not working for the government but runs his/her own private hospital. | Yes | Yes |
| Paravet | A frontline veterinary worker who holds a diploma in veterinary and animal husbandry | Yes, but are required to discuss the product and why they are prescribing it with the supervising veterinarian | Yes |
| Pharmacist | The shopkeeper running the pharmaceutical shop. | No | Yes |
| Quack/homeopathic practitioner | A non-veterinarian and untrained person treating sick animals | No | Yes |
| Dairy farmer | Dairy farmer keeping animals for milk production who sometime use old prescription to treat their animals. | No | Yes |
In Bangalore, the situation was completely different. Animal health services in the region were reported to be readily available, and farmers rarely treated the animals on their own. Veterinary services were received either from the Karnataka milk federation (KMF) or from the State Veterinary Department.
“I register a complaint to the secretary of KMF center and then doctor is called. Also, the cost of the treatment is charged as per the cooperative rate chart.”-(Dairy farmer, Bangalore)
Practices and responsibilities of veterinarians and paravets
Veterinarians interviewed in the study were largely responsible for the diagnosis and treatment of clinical cases, pregnancy diagnosis, and artificial insemination, for disease prevention, control, and provision of herd health services. Their years of experience and workload are given in Table 5.
Table 5.
Engagement of veterinarians in the delivery of animal health services, in Guwahati, Karnal, Bangalore, and Kolkata (September–October 2018).
| Study area | Number of years in veterinary practice | Number of veterinarians interviewed | Number of dairy animal cases reportedly handled in a week |
|---|---|---|---|
| Karnal | 10–30 years | 6 | 50–100 |
| Kolkata | 10–20 years | 3 | 25–30 |
| Bangalore | 15–30 years | 8 | 15–70 |
| Guwahati | 12–20 years | 7 | 50–100 |
They got referral cases from the paravets but were additionally also directly contacted by the farmers themselves, through telephone calls. In some cases, the farmers consult with the quacks before contacting the veterinarian as the quacks were readily available and farmers found it more convenient. In Bangalore, a system that allows farmers to register their animal health complaints at KMF was reported, the cases are addressed by the responsible veterinarian.
“Actually, it depends upon the farmers. Some well-educated, aware farmers come to me directly. But in some cases, farmers rely upon some so-called village doctors (‘quacks’) who practice without knowledge and prescribe veterinary medicines. After all these episodes of ‘quacks’, paravets; if their cow is not recovering then only, they come to me. “ – (Veterinarian, Guwahati)
Paravets interviewed in the study had also been in practice for a varying number of years (Table 6).
Table 6.
Engagement of paravets in the delivery of animal health services, in Guwahati, Karnal, Bangalore, and Kolkata (September–October 2018).
| Study area | Number of years in veterinary practice | Number of paravets interviewed | Number of dairy animal cases reportedly handled in a week |
|---|---|---|---|
| Karnal | 10–15 years, 30–35 years | 8 | 100–300 (animal treatment as well as vaccination, artificial insemination) |
| Kolkata | 1–5 years | 4 | 50–100 (animal treatment as well as vaccination and artificial insemination) |
| Bangalore | 10–15 years | 8 | 100–200 (just vaccination and artificial insemination. The paravets were not involved in treatment) |
| Guwahati | 30–35 years | 9 | 30–40 (animal treatment as well as vaccination, artificial insemination) |
In most cases, they were called by farmers when there was a case to be attended, which included animal treatments, except in Bangalore where paravets only handled vaccination and artificial insemination cases, and neither treated nor prescribed any medicines.
CORE THEME 3: antibiotic use and knowledge on antimicrobial resistance
Practices of farmers related to medicines
Farmers in Guwahati and Karnal were not familiar with the names of allopathic (or modern) medicines. They administered these to their animals, as injectables, tablets, and powder medicines. The administration was based on the prescription given either by the veterinarian or the local pharmacist. Some of them, particularly in Guwahati, used old prescriptions, to not only know which medicines to buy but also to determine the dosage they needed to give. In Kolkata, farmers accessed allopathic medicines through local pharmacies. They, in most cases, explained the symptoms they had observed to the pharmacists who would in turn recommend and sell the medicines they considered appropriate. In Bangalore, animal treatment was only done by the village veterinarian. Non-prescribed use in Bangalore was rare among the farmers, they only gave what had been prescribed by their veterinarians.
“I am a dairy farmer and it’s been 10–15 years in this field so first I treat my animals by giving antibiotics but if the problem persists then only, I call the doctor.”- (Dairy farmer, Karnal)
The use of home remedies (or traditional medicines) to manage animal diseases was reported in all areas. This included the use of jaggery (a coarse, dark brown sugar made in India by evaporation of the sap of palm trees), betel leaves (heart-shaped leaves of an evergreen vine (Piper betle) of South and Southeast Asia), and mustard oil.
In most cases, farmers were not aware of health risks, either those associated with the use of medicines in the treatment of animal diseases or the presence of antibiotic residues in the milk and failure to observe drug withdrawal periods. Administering medicines to dairy cows was perceived by the farmers to have negative effects on both production (reduced milk yield) and quality (bad smell of milk). Some farmers in Karnal and Bangalore were aware of the health effects associated with the presence of antibiotic residues in milk but believed that boiling made the milk safe to drink. A few farmers (almost in all the groups at each study site) knew about drug withdrawal periods, but they still used milk from animals on antibiotic treatment as they could not afford to waste it. Notably, farmers in Kolkata did not consume milk from animals on antibiotic treatment but instead sold the milk to be consumed by others in the community. Farmers in all the study regions only discarded milk if they observed a change in its color, consistency, and smell.
“Yes, there must be risk of using medicines in food animals. Doctors tell us not to consume milk while the cow is on treatment, but we still drink milk as we have no other alternative. “- (Dairy farmer, Guwahati)
Antibiotic use by the veterinarians, paravets and understanding on anti-microbial resistance
The type of antibiotic prescribed by veterinarians depended on the severity of the case presented. Veterinarians in Guwahati reportedly prescribed antibiotics only in severe cases, and only when they were needed. Some of them sent samples for laboratory testing before prescribing any antibiotic.
‘I prescribe antibiotics after seeing the severity of a case. Now suppose a prolonged case of bacterial infection has reached to my door, initially instead of giving an antibiotic, i see the normal supportive treatment line, if not i go for certain tests like pus, culture sensitivity of the localize tissue and antibiotics are injected for 3–5 days after the sensitivity tests are performed/checked.’ – (Veterinarian, Guwahati).
The most common antibiotics prescribed by the veterinarians across all four study sites included gentamycin, oxytetracycline, penicillin, dicrysticin, amoxicillin, ampicillin, ceftriaxone, tazobactam, enrofloxacin, cephalosporins. Given that only a few of the antibiotics were available through the government supply chain, farmers mostly received a prescription from government veterinarians but had to buy prescribed medicines from nearby pharmacies. Where the drugs were available in government veterinary hospitals, farmers did not have to pay for the medication.
Veterinarians were well versed with the topic of antimicrobial resistance and according to them, it is the farmers, ‘quacks’, and paravets who are responsible for the problem, as they often fail to consult with professionals before using antibiotics.
“Equally all are responsible and mostly “quacks” play an important role in this. Farmers are impatient and look for quick results.” – (Veterinarian, Guwahati)
The paravets defined antibiotics as the medicines that kill pathogens and prevent diseases in animals and humans. In Guwahati, paravets relied on drug marketing agents to know about the effectiveness of a particular antibiotic.
“Sorry directly I can’t say what antibiotics are? The medical representative tells us about particular antibiotics giving good response in particular conditions.”- Paravet (Guwahati)
Almost all the paravets prescribed antibiotics in the field very often, except in Bangalore where they are only allowed to prescribe herbal medicines available at their local KMF. A considerable proportion of the paravets (8 of the 29) reported that antibiotics should be administered to all sick animals. In Kolkata, paravets always discussed the case presented with the available veterinarian before prescribing antibiotics.
“It depends upon the case. I never prescribe an antibiotic by myself. If the animal is ill, I note down the symptoms and consult the veterinarian of the block hospital. She prescribes and then, i direct the owner.”- Paravet (Kolkata)
The common antibiotics prescribed by paravets in the study sites included enrofloxacin, gentamicin, oxytetracycline, ceftriaxone (also combined with tazobactam), and penicillin/streptomycin combinations. Some paravets sold the drugs on credit while others did not. In some areas, the paravets relied on the government supply system to get the drugs and only bought from private pharmacies if a particular medicine was unavailable. In Guwahati, paravets purchased antibiotics from private pharmacies.
Most paravets were familiar with the concept of antimicrobial resistance (except in Bangalore where they were found to have no idea of the concept). According to the paravets, antibiotics stop working if they are continuously used in animals, if the dosage is altered, and if the prescribed course is not completed. The paravets in Kolkata also linked antimicrobial resistance to the consumption of meat contaminated with resistant microbes. They were aware of the health impacts associated with antibiotic use in animals. As per the paravets in Karnal, lower doses of antibiotics reduced the risk of AMR. According to the paravets, farmers and ‘quacks’ are the ones primarily responsible for the increasing resistance levels.
CORE THEME 4: zoonotic diseases
Knowledge and perception of the farmers on zoonotic diseases
Some farmers in each group knew that diseases might occur in humans through contact with sick animals but most could not name any. Rabies, tuberculosis, and brucellosis were given as examples of such diseases. Farmers in Bangalore, despite the good veterinary practice provision, were also found not to be aware of zoonotic diseases.
“I know … my cow once suffered from TB and I referred to the veterinarian. He himself told me that I shouldn’t go near to cattle often and should not drink its milk as this disease may get spread to man and also don’t sell or give this milk to others.”- (Dairy farmer, Guwahati)
Farmers in Karnal did not take any precautions when handling sick animals. Those in Guwahati washed their hands after touching sick animals. Washing of hands after touching sick animals and regular cleaning of animal sheds was reported by farmers in Bangalore. In Kolkata, sick animals were isolated from healthy ones and fed separately. Abortion in cattle was a problem but none of the farmer groups knew its cause. Whenever there was an abortion case, the fetus was wrapped, put in a jute bag, and disposed of, either by burying or throwing it in a pond, and sometimes left in an isolated place.
Knowledge and perception of the veterinarians and paravets on zoonotic diseases
Rabies, leptospirosis, tuberculosis, brucellosis, and Japanese encephalitis were the main zoonotic diseases frequently observed by veterinarians. The diagnosis was either symptomatic or laboratory-confirmed. Veterinarians in the study reported wearing gloves, masks and washed their hands properly after handling sick animals. They also provided advice on simple measures that farmers needed to observe while handling sick animals. Although they sensitized farmers about the proper disposal of aborted fetuses, they were concerned that the farmers were not paying attention to the messages provided.
All the paravets were aware of infection spread from animals to humans. They were conversant with a number of zoonotic diseases including brucellosis, rabies, tuberculosis, and bird flu. Some also mentioned anthrax. They wore gloves and washed hands when handling sick animals. Those in Guwahati complained of non-availability of gloves in the government hospitals. The paravets always informed the farmers on the importance of disease control measures including quarantine and hand washing. They handled cases of animal abortions in the villages. Brucellosis was identified as one of the causes of abortion, and whenever there was abortion, farmers were advised not to touch aborted fetuses with bare hands and were asked to bury them at an appropriate depth on the ground.
“I always tell them to separate the healthy animals from sick animals. Not to mix fodder of sick and healthy animals and wash hands after touching the sick animals.”- Paravet (Bangalore)
CORE THEME 5: vaccination
Vaccination activities and perspective of the farmers
In all regions, farmers were found to be aware of the value of vaccination and presented their animals to be vaccinated. Vaccination was mostly done by the paravets. In Guwahati and Kolkata, farmers called paravets whenever they had animals to be vaccinated and were required to pay for the services. Unlike in Karnal and Bangalore where the Government Veterinary Department organized campaigns and vaccinated animals for free. None of the farmer groups in Guwahati, Kolkata talked about government-organized vaccination campaigns.
“Vaccination protects my cow from diseases. It is very important.”-(Farmer, Guwahati)
There was also a mention of the ‘homeopathic vaccine’ by two of the farmer groups in Kolkata. It was given by local quacks, but none of those interviewed could provide details about the product. Farmers had to pay quacks for this ‘homeopathic vaccine.’
Vaccination activities and perspective of veterinarians and paravets
Vaccination was done for FMD, BQ, and HS. The vaccines were received through the government supply system and farmers were not required to pay anything, except presenting the animals for vaccination, either in the hospital or in camps organized by the veterinary department. All paravets in the study sites had participated in the vaccination exercises. In addition to FMD, BQ, and HS vaccination, animals in Bangalore were also vaccinated against brucellosis. On disease control and farmer perception regarding vaccination, a veterinarian in Guwahati said:
“They are very much aware. They have learnt from their mistakes. Previously they have lost many animals, so now they have realized, and this is good for us and for farmers too. Still some farmers come and remind us about the schedule. “ – (Veterinarian, Guwahati)
Discussion
Dairy farming is an important source of income for farmers in India. Mastitis was found to be a significant problem in all the study areas, similar to the findings of other studies in the country [8,9]. Verma and co-workers [10] isolated pathogens from 71 (83.5%) milk samples collected in and around Meerut region, and according to the authors, failure of growth in 16.5% of the samples was due to the presence of antimicrobial residues in the milk. More recent studies have shown that the most common indication for using antibiotics in dairy cattle is mastitis, and the preferred antibiotics include beta-lactams and streptomycin [11]. The importance of mastitis highlighted by the dairy farmers of this study indicates its significance as a driver in our study for antibiotic use. In India, there is a lack of veterinary ability to cultivate bacteria in clinical cases of mastitis, as well as to decide antibiotic susceptibility. Therefore, the use of antibiotics for treatment is not guided by this. The veterinarians interviewed in this study did not have access to laboratory facilities.
Irrational use of antibiotics in dairy systems is aggravated by a number of factors, including; poor knowledge and misconceptions about antibiotics, easy access to antibiotics, limited field supervision, possibly due to inadequate veterinary coverage, and practices such as old prescriptions used to purchase drugs, and consultation with non-veterinarians [12]. However, the lack of trained veterinarians and inadequate delivery of animal health services appeared to be the major drive in our study. Similar results were reported in the study by Chauhan et al. [3], conducted in Guwahati, Ludhiana, and Bangalore. The lack of trained veterinarians in the field and the neglect of the veterinary department was also highlighted by Sasidhar in 2002 [13].
The dairy farmers in all the study regions except Bangalore rely upon ‘quacks’ and paravets and only consult with qualified veterinarians after the animals have failed to respond to prior treatments. Similar practices were reported by Chauhan et al. [3], where due to the acute shortage of professionals, farmers tended to consult either the informal prescribers or the veterinary field assistants. This implies that, by the time a farmer reaches the veterinarian, he/she has already spent time and money trying out other alternatives. A case study on the preference of service providers for the veterinary service [14] conducted in Maharashtra found that farmers would not consult a ‘quack’ or try to treat the animals on their own if veterinary services were readily available. Farmers with high literacy levels were found to always approach qualified veterinary practitioners [14].
Farmers were found to be unaware of the words ‘antibiotic’ and ‘antimicrobial resistance.’ A qualitative study similar to our study done in Guwahati, Ludhiana, and Bangalore showed the same results [3]. As per our results, most of the farmers could not differentiate between antibiotics and non-antibiotic allopathic medicines and relied upon the old prescriptions or the pharmacist of a local pharmacy to figure out the names and dosage of the medicines. The results are also similar to a study in the eastern Haryana region which revealed cases of over-the-counter antibiotic sales (either without a prescription or by reusing old prescriptions) and farmers who were unaware of the harmful effects of certain types of antibiotics [12].
None of the interviewed paravets could clearly define antibiotics or antimicrobial resistance, although they seemed aware of the reasons why antibiotics could stop working and the concept of antibiotic resistance. Only a few of them consulted the veterinarian before prescribing an antibiotic. Veterinarians interviewed in the study demonstrated good knowledge of antibiotic resistance; similar findings were reported in a cross-sectional study conducted in Haryana by Parkunan et al. [15]. The study found the majority of veterinarians to be aware of fundamental clinical aspects of AMR, i.e., the general causes and transmission of resistance, response during treatment failure, and safe disposal of hospital waste.
Both the veterinarians and the paravets interviewed in the current study had good knowledge of the zoonotic diseases, and most observed the precautions while handling sick animals, unlike the farmers who were less aware and in most of the areas took no precautions while handling sick animals. Poor knowledge relating to zoonotic pathogens has been reported in other countries. In Tajikistan, the majority of livestock keepers (85%) were not aware of brucellosis and were thus at a higher risk of being infected with the disease [16].
Vaccination has the potential to reduce antimicrobial use by reducing illness. Almost all the farmers in the four regions reported that they vaccinated their animals and knew the value of disease control and prevention. Farmers in Haryana and Punjab (61.4%; n = 360) perceived vaccination to be profitable [17]. The Haryana and Punjab study also showed that farmers had their livestock vaccinated only when a veterinarian or paravet visited their village under government schemes such as the control programs for FMD and brucellosis.
Limitations of the study
This was a qualitative study conducted only in a few villages of Guwahati, Karnal, Bangalore, and Kolkata regions and neither represents the situation in the entire country nor the entire regions. India is a large country and the findings of this study are not representative of the entire country. Despite the limited coverage, the study has provided key data on knowledge and perceptions of various stakeholders on antibiotics and their use and gave a snapshot of animal health practices that are common across the four regions. The FGDs with farmers and KIIs with the veterinarians, paravets were conducted in local languages and then translated to English. A possible bias is related to the fact that participants may not answer truthfully resulting in responses that may not reflect the actual situation in the population. For example, veterinarians knowing about the importance of prudent antibiotic use may be prone to say how they should use it, and not what they actually practice. Similarly, farmers may be more prone to report complaints on veterinary services, and not always want to report positive experiences or problems that arise as a consequence of their own faults (and may instead find it easy to blame veterinarians and paravets).
Conclusion
The current study reveals that the farmers have poor knowledge about antibiotics, and they are largely unaware of the concept of antimicrobial resistance. Only a few of them are aware of zoonotic diseases and no one takes any precautions while handling sick animals. Due to the lack of adequate veterinary services and the high cost of treatment, dairy farmers treat animals on their own by using old prescriptions. Some of them also consult ‘quacks’ for treatment or ask the local pharmacist for medicines. The veterinarians, on the other hand, are well-informed and claimed to use antibiotics judiciously. However, most of the paravets did not consult the veterinarian before prescribing antibiotics.
The study identifies several factors that determine the use of antibiotics in smallholder dairy farms. However, lack of proper veterinary services with limited outreach activities and readily available veterinarians was frequently reported by the farmers, and thus seems the major issue that is leading to the inadequate use of antibiotics by the farmers, together with the ready availability of antibiotics and low knowledge. The situation was much better in Bangalore, where the veterinary services were available, the paravets rarely prescribed any antibiotics and the dairy farmers did not treat the animals on their own. Therefore, strengthening of veterinary human resources is the need of the hour. Other interventions such as community awareness programs related to antibiotics, antibiotic resistance, and zoonotic diseases are also required to increase the awareness level and address various issues. Proper legislation must be framed to limit over the counter sales of antibiotics without a veterinary prescription from a veterinarian. This will not only limit the invariable use of antibiotics by the farmers, paravets and pharmacists but will greatly address the issue of anti-microbial resistance due to the use of antibiotics in the animals.
Supplementary Material
Acknowledgments
This project was supported by the ICAR-ILRI collaboration funds and the CGIAR Research Program Agriculture for Nutrition and Health. The authors would like to thank the donors to the CGIAR system for their support. We would like to acknowledge support from farmers, veterinarians, and paravets engaged in the study, and that from the data collection teams at ILRI Guwahati, NDRI Karnal, NIVEDI Bangalore, and IVRI Kolkata. We are grateful to Dr HR Rahman for his support in the course of the project implementation. We are thankful to the Director and scientists, ICAR-NIVEDI, Bangalore for their support.
Biographies
Garima Sharma is a PhD student under the Department of Medical Biochemistry and Microbiology, Uppsala University, Sweden. She is a PhD fellow with Department of Biosciences at International Livestock Research Institute (ILRI). She holds a graduate degree in Veterinary Medicine and a post graduate degree in Public Health. She is working with Animal and Human Health (AHH) Programme of ILRI where her research focuses mainly on antimicrobial resistance and zoonotic diseases. Email: G.Sharma@cgiar.org, drgarima111@gmail.com
Florence Mutua is a Scientist working for International Livestock Research Institute (ILRI) and based in Dar es Salaam, Tanzania. She has a postgraduate training in Veterinary Epidemiology and has participated in several livestock projects in East Africa. Her current research focuses on Animal Health and Food safety. Email: F.Mutua@cgiar.org
Ram Pratim Deka is a PhD student under the Department of Clinical Sciences at Swedish University of Agricultural Sciences (SLU), Sweden. He is also working under the Animal and Human Health (AHH) Programme of the International Livestock Research Institute (ILRI) where his research focuses upon foodborne and zoonotic diseases. Email: R.Deka@cgiar.org
Rajeshwari Shome is a Principal Scientist at ICAR-National Institute of Veterinary Epidemiology and Disease Informatics, Government of India. She has extensive experience of conducting laboratory studies on brucellosis, pasteurellosis, coxiellosis and antimicrobial resistance (AMR). Email: rajeswarishome@gmail.com
Samiran Bandyopadhyay is a senior scientist at ICAR- Indian Veterinary Research Institute, Eastern Regional Station, Kolkata. He is involved in research on the emergence of antimicrobial resistance (AMR) in livestock from Eastern and North-eastern India. He is also the coordinator of ICAR- Indian Network for Fishery and Animals Antimicrobial Resistance (INFAAR) for animal science institutes. He authored more than 100 research papers in reputed national and international journals and a book “Antimicrobial Resistance in Agriculture: Perspective, Policy and Mitigation” published by Elsevier. Email: samiranvet@gmail.com
Bibek R Shome is a Principal Scientist at ICAR-National Institute of Veterinary Epidemiology and Disease Informatics, Government of India. He has specialization in microbiology with broader knowledge on infectious diseases of livestock, outbreak investigation, molecular epidemiology, nucleic acid based diagnostic assays with special experience on Antimicrobial resistance (AMR). Email: brshome@gmail.com
Naresh Goyal Kumar is a Principal Scientist at Dairy Microbiology Division Of National Dairy Research Institute (NDRI), Karnal, Haryana. He is currently working upon development of Biosensors for monitoring food safety, quality assurance in dairy industry and has developed technologies for rapid detection of antibiotics, pesticides and contaminants in milk. He established National Referral Centre on milk quality and safety at ICAR-NDRI under NAIP World Bank funded project with BSL-3 facility. Email: nkg6825@gmail.com
Delia Grace is the professor for Food Safety System at the Natural Resources Institute, University of Greenwich, UK and the contributing scientist at Animal and Human Health (AHH) Programme of International Livestock Research Institute (ILRI). She has been a lead researcher in food safety in informal markets for several decades. She has led or contributed to evidence synthesis and investment advise for World Bank, DFID, USAID, ACIAR, BMGF, FAO, OIE, WHO, AU-IBAR, OECD and others. She has an extensive experience in leading several projects related to foodborne and zoonotic diseases. Email: d.grace@cgiar.org
Tushar Kumar Dey is a PhD student under the Department of Medical Biochemistry and Microbiology at Uppsala University, Sweden. He is a PhD fellow at International Livestock Research Institute (ILRI) and is working with Animal and Human Health (AHH) Programme at ILRI. He is also attached to ICAR- National Institute of Veterinary Epidemiology and Disease Informatics, Government of India. His work is related to assessment of AMR burden in poultry sector of India. He has experience on basic, molecular studies and bioinformatics analysis of AMR mediated microbes. He also holds experience in field survey, data collection, sample collection and analysis with respect to AMR studies. Email: tusharkrde@gmail.com
Nimita Venugopal is a project assistant at ICAR-National Institute of Veterinary Epidemiology and Disease Informatics, where she is working to obtain her PhD and has experience on molecular studies related to E.coli and Staphylococci mediated AMR in bovimes. Email: nimitacv@gmail.com
Swati Sahay is a project assistant at ICAR-National Institute of Veterinary Epidemiology and Disease Informatics, where she is working to obtain her PhD. She has experience in studies related to bovine respiratory diseases and conducting laboratory diagnostic experiments on brucellosis and coxiellosis. Email: simi17ko1@gmail.com
Johanna F. Lindahl is working as a senior scientist at Animal and Human Health (AHH) Programme of Interantional Livestock Research Institute (ILRI) and adjunct at Swedish University of Agricultural Sciences as well as Uppsala University, Sweden. She is leading projects related to food safety, vector-borne diseases, emerging infectious diseases and zoonotic diseases in developing countries, mainly East Africa, South and South east Asia. Email: j.lindahl@cgiar.org
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1]. Kumar S, Aditham C, Harish B, et al. Antimicrobial resistance in India: A review. J Nat Sci Biol Med. 2013;4(2):279–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2]. Kakkar M, Walia K, Vong S, et al. Antibiotic resistance and its containment in India. BMJ. 2017;358:25–30. [DOI] [PubMed] [Google Scholar]
- [3]. Chauhan AS, George MS, Chatterjee P, et al. The social biography of antibiotic use in smallholder dairy farms in India. Antimicrob Resist Infect Control. 2018. May;7(1). DOI: 10.1186/s13756-018-0354-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Ayukekbong JA, Ntemgwa M, Atabe AN.. The threat of antimicrobial resistance in developing countries: causes and control strategies. Antimicrob Resist Infect Control. 2017. May 15;6(1). BioMed Central Ltd. DOI: 10.1186/s13756-017-0208-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5]. Van Boeckel TP, Brower C, Gilbert M, et al. Global trends in antimicrobial use in food animals. Proc Natl Acad Sci U S A. 2015. May;112(18):5649–5654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Lindahl JF, Goyal Kumar N, Deka RP, et al. Serological evidence of Brucella infections in dairy cattle in Haryana, India. Infect Ecol Epidemiol. 2018. Jan;8(1): 1555445.do [Google Scholar]
- [7]. Shome R, Deka RP, Sahay S, et al. Seroprevalence of hemorrhagic septicemia in dairy cows in Assam, India. Infect Ecol Epidemiol. 2019. Jan;9(1):1604064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8]. Bisla RS, singh H, Bhanot V, et al. Retrospective study on prevalence and antibiogram of mastitis in cows and buffaloes of Eastern Haryana. 2011. [cited 2019 Oct 29 ]. Available from: https://www.arccjournals.com/journal/indian-journal-of-animal-research/ARCC436 [Google Scholar]
- [9]. Sinha MK, Thombare NN, Mondal B. Subclinical mastitis in dairy animals: incidence, economics, and predisposing factors. Sci World J. 2014;2014. DOI: 10.1155/2014/523984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10]. Verma H, Rawat S, Sharma N, et al. Prevalence, bacterial etiology and antibiotic susceptibility pattern of bovine mastitis in Meerut. J Entomol Zool Stud. 2018;6(1):706–709. [Google Scholar]
- [11]. World Health Organization, Ministry of Health and Family Welfare Government of India . Antimicrobial resistance and its containment in India. 2016. Available from: origin.searo.who.int/india/topics/antimicrobialresistance/amr_containment.pdf. [Google Scholar]
- [12]. Kumar V, Gupta J. Prevailing practices in the use of antibiotics by dairy farmers in Eastern Haryana region of India. Vet World. 2018. Mar;11(3):274–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13]. Sasidhar PVK. Revitalizing veterinary and animal science education for the future in India — issues and approaches. J Agric Educ Ext. 2002. Oct;8(3):139–149. [Google Scholar]
- [14]. Mirajkar PP, Kumar S, Singh YP. Preference of service providers for the veterinary service-a case study of Sangli District of Maharastra state, India. 2011.
- [15]. Thulasiraman Parkunan MA, Sukumar B, Chera JS, et al. Antibiotic resistance: A cross-sectional study on knowledge, attitude, and practices among veterinarians of Haryana state in India. Vet World. 2019;12(2):258–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16]. Lindahl E, Sattorov N, Boqvist S, et al. A study of knowledge, attitudes and practices relating to brucellosis among small-scale dairy farmers in an urban and peri-urban area of Tajikistan. PLoS One. 2015. Feb;10(2). DOI: 10.1371/journal.pone.0117318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17]. Rathod P, Chander M, Bangar Y. Livestock vaccination in India: an analysis of theory and practice among multiple stakeholders. Rev Sci Tech Off Int Epiz. 2016;35(3):729–739. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


