Clinical manifestations of COVID-19 may range from asymptomatic to severe interstitial pneumonia with acute respiratory distress syndrome (ARDS) and death. COVID-19 mortality rates vary greatly [1] and the most reliable assessment of mortality comes from patients admitted due to severe cases of pneumonia [2].
At San Raffaele Hospital in Milano, Italy, we managed the COVID-19 outbreak with dynamic reorganization, and an increase in bed capacity. From 25 February until 13 May 2020, 950 consecutive adults were admitted, 68% were male and the mean age was 65 years (Table 1). Intensive Care Unit (ICU) beds raised progressively up to 56 beds with a proportion of 17% (range 10–20%) of the entire bed capacity.
Table 1.
COVID-19 patients characteristic and logistic model for mortality.
| COVID-19 patients characteristic | First quartile | Second quartile | Third quartile | Fourth quartile |
|---|---|---|---|---|
| Number of patients | 284 | 445 | 167 | 54 |
| Age, mean ± SD | 66 ± 14 | 64 ± 14 | 65 ± 17 | 65 ± 18 |
| Male, n (%) | 213(75%) | 300 (67%) | 100 (60%) | 35 (65%) |
| ICU, n (%) | 48 (17%) | 61 (14%) | 16 (10%) | 4 (7.4%) |
| Age for ICU patients, mean ± SD | 60 ± 12 | 62 ± 9 | 60 ± 11 | 66 ± 19 |
| Hospital stay over all, median (IQR) | 14 (8–25) | 14 (7–26) | 13 (7–27) | 17 (8–24) |
| Hospital stay for survivors, median (IQR) | 15 (8–28) | 15 (8–27) | 14.5 (7–29) | 17 (8–23) |
| Hospital stay for dead patients, median (IQR) | 12 (7–22) | 10 (5–20) | 13 (5–22) | 24 (24–24) |
| First data quartile | 25/02/2020 | 16/03/2020 | 05/04/2020 | 24/04/2020 |
| Last data quartile |
15/03/2020 |
04/04/2020 |
23/04/2020 |
13/05/2020 |
| Logistic model for mortality |
Odds Ratio |
P value |
95% Confidence Interval |
|
| Age | 0.99 | <0.0001 | 0.99 | 0.99 |
| Based on first quartile (ref) | ||||
| Quartile 2 | 0.33 | <0.0001 | 0.24 | 0.46 |
| Quartile 3 | 0.39 | <0.0001 | 0.25 | 0.61 |
| Quartile 4 | 0.03 | 0.001 | 0.004 | 0.22 |
Here, we report the mortality rates across time for COVID-19 patients admitted at our institution. Patients are divided into temporal quartiles of 20 days each. Date of last follow-up was 12 June 2020. Minimum follow-up of the last patients hospitalized was 30 days. A total of 129/950 (14%) patients required ICU. Of the 950 patients, 30-day mortality was 164/950 (17%), with a dramatic drop in the mortality rate after the first time quartile, decreasing from 24% to 2% (Figure 1). Age and time of admission were independent predictors of hospital mortality in the multivariate model (Table 1).
Figure 1.
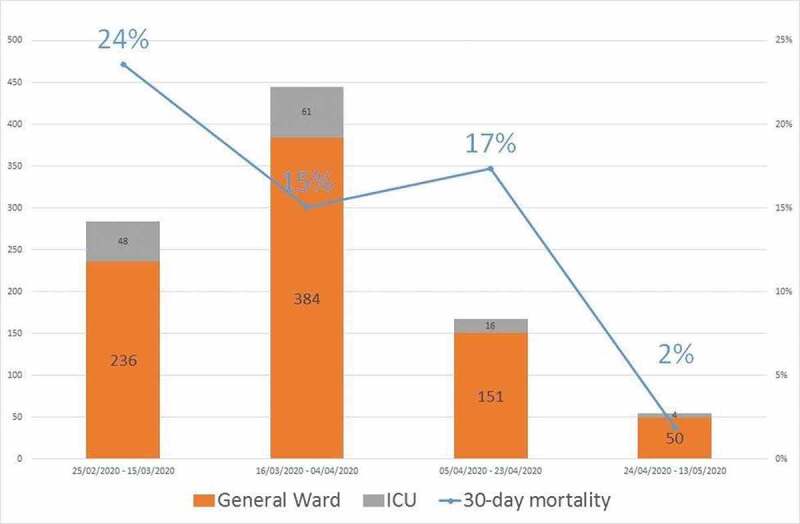
COVID-19 patients admitted in general wards and ICU per temporal quartiles and mortality rates.
There are a number of possible reasons that may explain these findings. In our institution, the proportion of patients requiring ICU decreased over time from 17% to 7%, without significant changes in patients’ age, suggesting a decreased severity of clinical presentation and progression. Understanding the pathophysiology of the disease [3], improving patients’ management and treatments [4] targeted to specific pathways of hyper-inflammation and microvascular thrombosis associated with COVID-19 may have contributed to a reduction of mortality. The establishment of the national Italian lockdown from 9 March has been a cornerstone for limiting the SARS-CoV-2 spread, as well as the large use of respiratory protective devices and other measures of social distancing. Additionally, the co-infection of respiratory pathogens (i.e. seasonal influenza viruses) might have decreased, and this factor could have had an impact on disease severity.
Recent findings [5] highlight the possible correlation between the pollutant emissions and region-specific climatic features in the areas mostly impacted by the COVID-19 outbreaks. A concomitant reduction of air pollution could be associated with a further decrease in factors associated with morbidity. Finally, the tracking of virus population diversity in time through SARS-CoV-2 [6] mutations could potentially establish a correlation of viral fitness and eventually viral attenuation with observed clinical outcomes. Our observation of a current reduction in the mortality of COVID-19 may contribute to the planning of social and economic measures during the post-pandemic phase.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020. April 22;323(20):2052–2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Ciceri F, Castagna A, Rovere-Querini P, et al. Early predictors of clinical outcomes of COVID-19 outbreak in Milan, Italy. Clin Immunol. 2020;217:108509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Ciceri F, Beretta L, Scandroglio AM, et al. Microvascular COVID-19 lung vessels obstructive thromboinflammatory syndrome (MicroCLOTS): an atypical acute respiratory distress syndrome working hypothesis. Crit Care Resusc. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Sanders JM, Monogue ML, Jodlowski TZ, et al. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020. April 13. DOI: 10.1001/jama.2020.6019. [DOI] [PubMed] [Google Scholar]
- [5].Frontera A, Martin C, Vlachos K, et al. Regional air pollution persistence links to COVID-19 infection zoning. J Infect. 2020. April 10;30173-0(20):S0163–4453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]


