ABSTRACT
Background
Examine the ability of a dynamic scapular recognition exercise to improve scapular upward rotation and decrease shoulder pain and disability in patients with adhesive capsulitis of the shoulder.
Methods
A test-retest randomized controlled study design was used. A total of sixty-six patients with unilateral adhesive capsulitis were equally divided into two groups. The study group received a dynamic scapular recognition exercise using a wireless biofeedback system, while the control group received placebo treatment in the form of active range-of-motion (ROM) exercises of the sound upper limb. A digital inclinometer was used to measure the scapular upward rotation and ROM of the shoulder joint, and the Shoulder Pain and Disability Index (SPADI) was used to measure the shoulder pain and disability.
Results
Study results showed that after two weeks, there were statistically significant differences between the study and control groups in scapular upward rotation and shoulder flexion and abduction (P < .05) and nonsignificant differences in shoulder external rotation and SPADI (P > .05). After two and six months, there were statistically significant differences between study and control groups in scapular upward rotation; shoulder flexion, abduction and external rotation; and SPADI scores (P < .05).
Conclusion
This study showed that a dynamic scapular recognition exercise significantly improves scapular upward rotation and the ROM of shoulder flexion and abduction after two weeks. At two and six months, this exercise improves scapular upward rotation; ROM of shoulder flexion, abduction, and external rotation; and SPADI scores. These improvements persisted for six months after the performance of this exercise
KEYWORDS: Adhesive capsulitis, dynamic scapular recognition, scapular upward rotation, shoulder pain and disability
Introduction
Shoulder adhesive capsulitis is recognized as a common shoulder problem [1,2], and saffects approximately 2% to 5% of the general population, commonly between 40 and 60 years old [1]. Women are affected more often than men [1]. Recently, a meta-analysis by Zreik in 2016 in the United Kingdom showed that shoulder adhesive capsulitis is five times more common in people with diabetes than in those without diabetes and that its incidence in the former group is approximately 13.4% [3]. Shoulder problems are a challenge to any investigator because shoulder movements occur as a result of complex interactions between the scapular movements on the thorax, humeral head movement in the glenoid cavity and clavicle movement at the sternoclavicular and acromioclavicular joints [4]. One of the major issues in patients with shoulder adhesive capsulitis is the limitation of their ability to reach overhead, which impedes their work and activities of daily living, such as dressing and hair care [5].
Shoulder adhesive capsulitis causes alterations in the position of the scapula and movement sense (proprioception) [6,7]. It has been demonstrated that shoulder adhesive capsulitis is associated with an alteration in the scapular kinematics in the form of an increase in the scapular lateral rotation, which could be a compensatory mechanism for this limitation in the range of motion (ROM) of the glenohumeral joint [8]. Prolonged alteration in scapular kinematics causes further damage to the proprioception-related muscle mechanisms, which subsequently damages muscle spindles [9]. The muscle spindle is the main sensory unit for the sensation of joint position. Capsuloligamentous mechanoreceptors (Pacinian corpuscles, Ruffini endings, and Golgi endings remain inactive) also contribute to the sensation of joint position and are activated by the deformation of musculoskeletal tissues [10]. Most studies have demonstrated that activation of these receptors is most intense at the limits of the ROM, when both the muscle and the tendon are stretched [10,11]. These mechanoreceptors provide proprioceptive data in the form of sensory signals modulated by the activation of the peripheral mechanoreceptors in the muscles, joints, and skin. These peripheral mechanoreceptors provide the central nervous system with sensory information about joint position and movement to adjust motor action [12]. The inactivation of the scapular muscles in patients with adhesive capsulitis may be responsible for the decreased joint sense of the shoulder movements [13].
Research on the position and movement senses still has many unanswered questions, especially on rehabilitating the proprioception of the shoulder joint in patients with shoulder adhesive capsulitis [14]. Additionally, the relationship between the improvement of proprioception and the healing process of shoulder adhesive capsulitis is not fully known [15,16]. Yang et al. [15] showed that future research should emphasize joint position sense and the proprioceptive feedback mechanism for treating shoulder adhesive capsulitis.
However, Aman, Elangovan and Konczak [17] demonstrated that proprioceptive training incorporating both passive and ROM exercise improves both somatosensory and motor functions. Most studies on shoulder proprioception have focused more on the static joint position sense than on the dynamic movement sense [16,18,19]. To the best of our knowledge, no study has investigated the effect of improving awareness of scapular movements on shoulder pain, disability and ROM in patients with shoulder adhesive capsulitis. Thus, the aim of this study was to compare two groups to assess the effect of a dynamic scapular recognition exercise on scapular upward rotation, shoulder pain and disability in patients with shoulder adhesive capsulitis.
Materials and methods
Design
A randomized controlled design was used in this study. All patients participated in this study after signing their informed consent for this study. This study was approved by the ethics committee of faculty of Physical Therapy, Beni-Suef University. Patients were recruited from April 2016 to December 2016. This study was prospectively registered with the registration number PACTR201602001463334 on 07/02/2016. The measurement of shoulder ROMs was applied to only three ROMs, namely, flexion, abduction and external rotation, because these shoulder ROMs are commonly affected in patients with shoulder adhesive capsulitis [6].
Sample size calculation
An a priori power test was used to calculate the sample size of this study. We used G*POWER software (ver. 3.1.9.2, Heinrich-Heine-University, Düsseldorf, Germany) to estimate the adequate sample size for the ANOVA test (repeated measures, within – between groups) using 2 groups, a significance level of 5%, a power level of 90%, two groups, five measurements and a medium effect size (dz = .25) [20]. The mean difference used in this study was 5 degrees of scapular upward rotation [21]. This mean difference was used to calculate the sample size because it was the main outcome measure of this study. Based on the aforementioned assumptions, the sample size needed for this study was 52 patients. We added 8 patients to compensate for dropout. A minimum power of 80% is acceptable in most studies [22].
Patients recruitment
All patients in this study were selected from the outpatient clinic of Faculty of Physical Therapy, Beni-Suef University. Because the main outcome measure was to improve the scapular upward rotation, the primary inclusion criterion was the inability of the patient to elevate the arm above 100 degrees in the plane of the scapula, as followed in the study of Teys et al [23]. Other inclusion criteria included unilateral shoulder adhesive capsulitis with these criteria, a limitation in both active and passive shoulder ROM and the presence of pain that interfered with performing activities of daily living [24]. The exclusion criteria included the presence of any shoulder condition that is a contraindication for exercising the shoulder joint, such as cancer, active infection, active inflammatory disease, recent dislocations, subluxations, surgery and fractures around the shoulder region [24]. Additionally, the patients were excluded if they had no signs of scapular dyskinesis. The Scapular Dyskinesis Test (SDT) was performed to confirm the presence of scapular dyskinesis [25]. This test was demonstrated by Tate et al [25,26] to be reliable and valid for measuring the degree of scapular dyskinesia.
Eighty patients were initially examined. Fifteen patients did not participate in this study. The excluded patients included ten patients (11.8%) who did not meet the selection criteria and four patients (5.9%) who participated only in the baseline assessment and did not continue the study. Ten patients did not meet the inclusion criteria because of new shoulder dislocations (4), subluxations (3), rheumatic disease (1), or shoulder surgery (2). Only sixty-six patients met these inclusion criteria. These candidates’ ages ranged from 40 to 60 years old. Only sixty patients completed the whole study, including the six-month follow-up. For reliable double blinding, two different licensed physical therapists who were blinded to the study procedures participated in this study. One of them performed the assessment, and the second performed the treatment. Patients were randomly assigned to 4 permuted blocks using computer software to balance the sample sizes among the two groups (study group and control group). The randomization was performed by a college staff member who was not involved in this study. A diagram of the patients’ flow through the study is shown in Figure 1.
Figure 1.
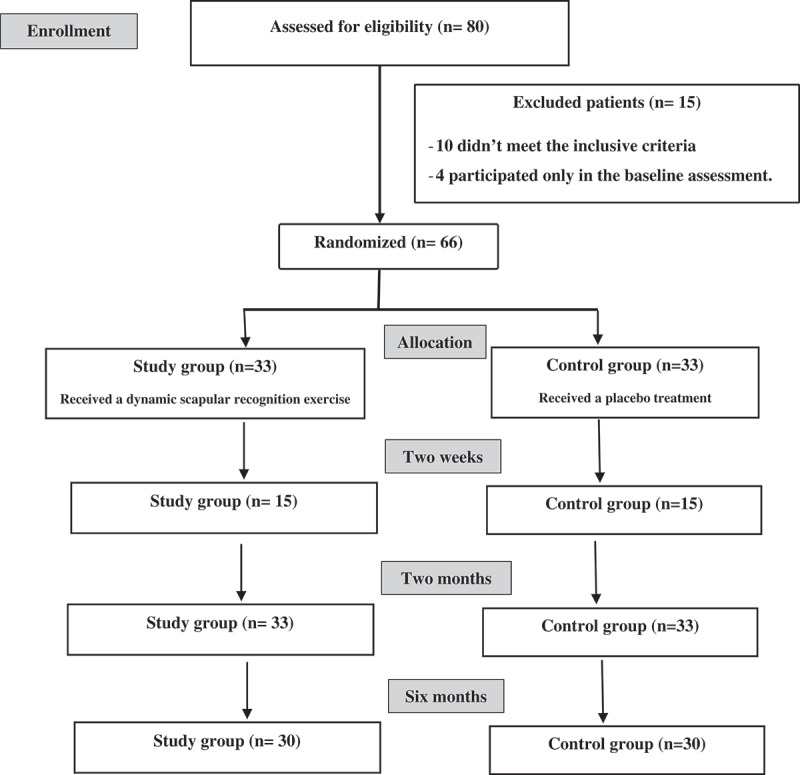
Patients flow chart.
Evaluative procedures
The primary outcome measure was scapular upward rotation, while the secondary outcome measures were the ROMs of shoulder flexion, abduction and external rotation as well as SPADI scores.
Scapular upward rotation
The measurement of scapular upward rotation was accomplished using a digital inclinometer (The Saunders Group, Chaska, MN, USA). Digital inclinometers are demonstrated to be a reliable tool for the measurement of scapular upward rotation [27,28]. The measurement was performed by following the same protocol used in the study of Wassinger et al [29]. The measurement was performed while the arm was at 80 degrees of shoulder abduction. The upward rotation of the scapula was measured in relation to the horizontal line by manually aligning the inclinometer’s base along the lateral and medial aspects of the spine of the scapula.
Shoulder pain and disability index (SPADI)
The SPADI is demonstrated to be a validated and reliable measure of shoulder pain and disability [30]. The SPADI was explained in detail to patients before the measurement was conducted. The patients were instructed to characterize the extent of their shoulder problems in the preceding week by marking one number on a scale from zero (no pain or disability) to ten (maximum pain and disability) for each item [31]. The results from each subscale were summed and converted to a score out of 100. Means were taken for these two subscales of the SPADI to give a total score out of 100. The higher the final score, the greater the shoulder pain, impairment or disability [32].
Shoulder ROM
Measurements for the shoulder ROMs were performed during flexion, abduction and external rotation. These measurements were performed by the same digital inclinometer used in the measurement of the upward rotation of the scapula. Digital inclinometers are demonstrated to be a reliable tool for the measurement of shoulder ROM. For accurate measurements, this inclinometer was calibrated to zero degree before each measurement. The measurement of the shoulder ROM was performed as described by Clarkson [33]. These guidelines have been established in the literature to have satisfactory intrarater reliability, with intraclass correlation coefficients (ICCs) of ≥0.85 [34].
For the ROMs of shoulder flexion and abduction, the digital inclinometer was positioned on the distal part of the upper arm proximal to the elbow joint and distal to the glenohumeral joint. The patient was positioned in an upright seated position in a high-backed chair. To prevent trunk compensation, a cloth gait belt was secured around the patient’s waist (at the umbilicus level) and back of the chair. The patient was asked to actively raise the tested arm raised in a firm sagittal plane with the palm facing down. Measurements of ROMs were recorded at the end of the available active ROM(34).
For the ROM of external rotation, the digital inclinometer was positioned on the distal forearm almost proximal to the wrist joint. The patient was positioned in the supine lying position with hips and knees flexed to nearly 45 degrees. The tested arm was placed on the table with both shoulder abduction and elbow flexed to a right angle, and the wrist joint was placed in neutral. To ensure neutral horizontal positioning, a roll was positioned under the humerus to place the humerus at the same level as the acromion(34). The patients was asked to rotate his or her arm externally by moving the forearm upward.
Treatment procedures
The physical therapy programmes for the two groups were equal in duration (40 min, 3 sessions/week for two months). Both the control and study groups received hot packs for 20 min and scapular mobilization for 5 min. In addition to hot packs and scapular mobilization, the control group performed a placebo active shoulder exercise with the uninvolved shoulder for 15 min. These active ROM exercises were performed in both the flexion and abduction directions for 20 repetitions/set, 5 sets/session.
The study group performed a dynamic scapular recognition exercise for 15 min. The scapular recognition exercise was performed by using an audible biofeedback device with wireless motion sensors (ViMove motion-sensor system, DorsaVi, Victoria, Australia). The motion sensor was placed on the top of the spine of the scapula [35]. The patient was asked to perform the maximum possible active shoulder abduction and try to concentrate on the movement of the scapula. The patient was encouraged to increase the movement of the scapula by increasing the volume of sound emitted by the device. The greater the movement of the scapula, the louder the sound produced by the biofeedback device. This exercise was performed for 20 min.
Data analysis
Initially, the participants’ files were coded by a college administrator who was not included in the study [36]. The data analysis was based on intention-to-treat analysis, and general linear models of analysis of variance for repeated measurements were used to detect the treatment-time interactions. The outcome measures were compared between baseline and after two weeks, two months and six months (follow-up). The mean, standard deviation and percentage of improvement were calculated for every variable. We compared the baseline characteristics of patients in the study and control groups using Pearson chi-squared tests for categorical variables, including gender, previous pain history and diabetic history. A t-test was performed for the continuous variables of age and body mass index (BMI).
Repeated measures of variance analysis (ANOVA) was used to analyse the difference between pretest and posttest results for scapular upward rotation; shoulder SPADI; and ROMs of flexion, abduction and external rotation within and between groups. The models included 1 independent factor (group), 4 repeated measures (time), and an interaction factor (group × time). The significance level was set at P < .05. SPSS (ver. 24, IBM Inc., Armonk, NY, USA) was used for statistical analysis in this study.
Results
The demographic and general characteristics of patients at baseline are shown in Table 1. There were no significant differences between the control and study groups in age, sex, BMI and diabetic history (all P > .05). The measurement records of scapular upward rotation, shoulder ROM of flexion, abduction and external rotation and SPADI were normally distributed in both groups (Shapiro-Wilk test, p > .05) [37].
Table 1.
Physical characteristics of patients in both groups.
| Control group |
Study group |
||||
|---|---|---|---|---|---|
| Items | Mean ±SD | Mean ±SD | P value | ||
| Age (yrs.) | 50.06 ±5.87 | 51.93 ±6.16 | .27 | ||
| BMI | 29.95 ±3.24 | 29.1 ±4.21 | .40 | ||
| Sex (%) | |||||
| Male | 16 | 53% | 18 | 60% | .46 |
| Female | 14 | 47% | 12 | 40% | |
| Pain history (%) | |||||
| Present | 20 | 67% | 18 | 73% | .69 |
| Absent | 10 | 33% | 12 | 27% | |
| Diabetic history (%) | |||||
| Diabetic | 11 | 37% | 13 | 44% | .53 |
| nondiabetic | 19 | 63% | 17 | 56% | |
| Life style (%) | |||||
| Sedentary | 22 | 73% | 13 | 44% | .03* |
| Active | 8 | 26% | 17 | 56% | |
P: probability. SD: standard deviation, *: significant.
Compliance
The exercise was successfully administered by a licensed physical therapist. All patients in this study approved of the frequency of 3 sessions/week and complied with their assigned treatments. The total number of sessions for all patients in each group was 24 sessions. Compliance in this study was defined as attendance of 22 sessions out of 24 sessions (92%). All patients met the compliance requirements of this study. The reasons given for missed exercise sessions were sickness (91%), ailing family members (6%) and weather conditions (3%).
Within-groups comparison
Scapular upward rotation
After two weeks, there was a significant difference in scapular upward rotation in the study group (P < .05). This difference remained significant after two months and at the follow-up measurements in comparison to the baseline measurements (P < .05). In the study group, the means, standard deviation and (95% CI) at baseline, after two weeks, after two months and after six months were 15.36 ± 12.34, 19.83 ± 6.76 (16.78–21.36), 24.52 ± 7.67 (20.43–25.62), and 21.45 ± 7.81 (18.22–23.67), respectively.
In the control group, after two weeks, there was no significant difference (P > .05). However, the difference became significant after two months in comparison to the baseline (P < .05). At follow-up, this difference remained significant in comparison to the baseline measurements. In the control group, the means, standard deviation and (95% CI) at baseline, after two weeks, after two months and after six months were 16.44 ± 8.94, 17.34 ± 12.15 (14.29–21.76), 21.38 ± 10.35 (18.23–24.79), and 19.02 ± 7.72 (16.90–22.25), respectively. The results of scapular upward rotation in both groups are shown in Figure 2 and Table 2.
Figure 2.
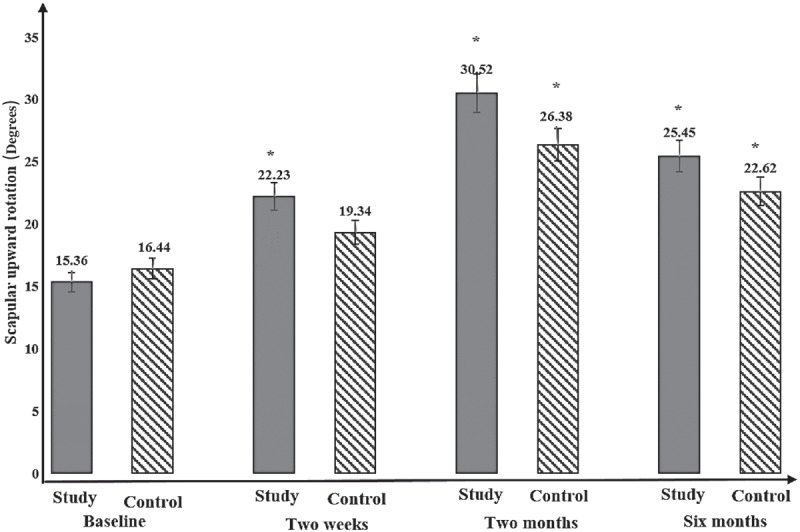
Repeated measure ANOVA between the baseline measurements and after two weeks, two months and six months (follow up) for the scapular upward rotation. *: significant (p < .05).
Table 2.
Repeated measure ANOVA between the baseline measurements and after two weeks, two months and six months (follow up).
| Baseline |
Two weeks |
Two months |
Six months |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| X± SD | X± SD | 95%CI | P | X± SD | 95%CI | P | X± SD | 95%CI | P | ||
| SUR | Study | 15.36 ± 12.34 | 19.83 ± 6.76 | 16.78–21.36 | .01* | 24.52 ± 7.67 | 20.43–25.62 | <.01* | 21.45 ± 7.81 | 18.22–23.67 | <.01* |
| (degrees) | Control | 16.44 ± 8.94 | 17.34 ± 12.15 | 14.29–21.76 | .08 | 21.38 ± 10.35 | 18.23–24.79 | .02* | 19.02 ± 7.72 | 16.90–22.25 | .04* |
| Flexion | Study | 89.03 ± 7.37 | 98.12 ± 8.53 | 95.09–101.76 | <.01* | 110.13 ± 11.73 | 107.65–113.35 | .01* | 108.12 ± 10.11 | 105.78–111.03 | <.01* |
| (degrees) | Control | 87.76 ± 12.37 | 90.32 ± 9.16 | 87.29–93.36 | .07 | 99.40 ± 14.23 | 96.37–101.86 | .02* | 97.52 ± 10.22 | 94.76–101.19 | .01* |
| Abduction | Study | 76.67 ± 6.02 | 90.11 ± 11.12 | 86.98–93.05 | .01* | 100.24 ± 7.83 | 97.76–103.54 | .03* | 93.63 ± 8.23 | 90.21–96.83 | <.01* |
| (degrees) | Control | 76.40 ± 10.41 | 85.13 ± 10.33 | 81.45–87.55 | .08 | 95.33 ± 12.16 | 92.78–98.55 | .04* | 91.34 ± 7.24 | 88.54–94.06 | .02* |
| Ex. Rotation | Study | 44.13 ± 11.54 | 50.32 ± 7.13 | 48.56–54.13 | .07 | 61.07 ± 8.03 | 58.71–64.32 | .05* | 59.54 ± 11.01 | 56.38–62.81 | .04* |
| (degrees) | Control | 43.80 ± 11.38 | 49.03 ± 9.56 | 47.82–53.18 | .11 | 56.21 ± 11.12 | 53.02–60.09 | .02* | 50.38 ± 6.54 | 47.92–53.03 | .09 |
| SPADI (%) | Study | 91.00 ± 12.35 | 80.40 ± 10.23 | 78.02–84.74 | .01* | 70.97 ± 8.29 | 68.54–74.17 | <.01* | 73.02 ± 8.72 | 70.31–77.64 | <.01* |
| Control | 92.35 ± 11.26 | 83.46 ± 8.29 | 79.40–86.06 | .08 | 79.86 ± 9.37 | 76.45–82.65 | .03* | 81.86 ± 9.07 | 77.64–83.31 | .09 | |
X: Mean, SD: Standard deviation, CI: Confidence interval, P: Probability, *: Significant, and SUR: scapular upward rotation.
Shoulder ROM
After two weeks, in the study group, there were significant differences in the ROMs of shoulder flexion and abduction (P < .05), and there was a nonsignificant difference in shoulder external rotation (P > .05). After two months and at the follow-up, there were significant differences in shoulder ROM of flexion abduction and external rotation in comparison to the baseline measurements (P < .05). In the study group, the means, standard deviation and (95% CI) for shoulder flexion at baseline, after two weeks, after two months and after six months were 89.03 ± 7.37, 98.12 ± 8.53 (95.09–101.76), 110.13 ± 11.73 (107.65–113.35), and 108.12 ± 10.11 (105.78–111.03), respectively. These values for shoulder abduction were 76.67 ± 6.02, 90.11 ± 11.12 (86.98–93.05), 100.24 ± 7.83 (97.76–103.54), and 93.63 ± 8.23 (90.21–96.83), respectively. These values for shoulder external rotation were 44.13 ± 11.54, 50.32 ± 7.13 (48.56–54.13), 61.07 ± 8.03 (58.71–64.32), and 59.54 ± 11.01 (56.38–62.81), respectively.
In the control group, after two weeks, there were nonsignificant differences in the ROMs of should flexion, abduction and external rotation (P < .05). After two months, there were significant differences in shoulder ROM of flexion, abduction and external rotation (P > .05). At the follow-up, the differences in shoulder ROM of flexion and abduction remained significant (P < .05), while the difference in shoulder external rotation was nonsignificant (P > .05). In the control group, the means, standard deviation and (95% CI) at baseline, after two weeks, after two months and after six months were 87.76 ± 12.37, 90.32 ± 9.16 (87.29–93.36), 99.40 ± 14.23 (96.37–101.86), and 97.52 ± 10.22 (94.76–101.19), respectively. These values for shoulder abduction were 76.40 ± 10.41, 85.13 ± 10.33 (81.45–87.55), 95.33 ± 12.16 (92.78–98.55), and 91.34 ± 7.24 (88.54–94.06), respectively. These values for shoulder external rotation were 43.80 ± 11.38, 49.03 ± 9.56 (47.82–53.18), 56.21 ± 11.12 (53.02–60.09), and 50.38 ± 6.54 (47.92–53.03), respectively. The results of shoulder flexion, abduction and external rotation in both groups are shown in Figure 3 and Table 2.
Figure 3.
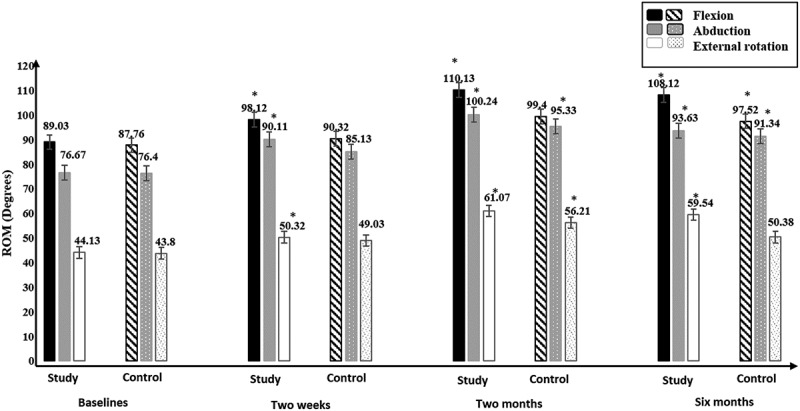
Repeated measure ANOVA between the baseline measurements and after two weeks, two months and six months (follow up) for the shoulder ROM. *: significant (p < .05).
Shoulder pain and disability index
After two weeks, there was a significant difference in the study group (P < .05), while there was a nonsignificant difference in the control group (P < .05). These differences were significant after two months in both groups in comparison to the baseline measurements (P < .05). At follow-up, the difference in the study group remained significant (P < .05), while in the control group, this difference became non-significant (P > .05) in comparison to the baseline measurements.
In the study group, the means, standard deviation and (95% CI) at baseline, after two weeks, after two months and after six months were 91.00 ± 12.35, 80.40 ± 10.23 (78.02 – 84.74), 70.97 ± 8.29 (68.54 – 74.17), and 73.02 ± 8.72 (70.31 – 77.64), respectively. In the control group, the means, standard deviation and (95% CI) at baseline, after two weeks, after two months and after six months were 92.35 ± 11.26, 83.46 ± 8.29 (79.40 – 86.06), 79.86 ± 9.37 (76.45 – 82.65), and 81.86 ± 9.07 (77.64 – 83.31), respectively. The SPADI scores of both groups are shown in Figure 4 and Table 2.
Figure 4.
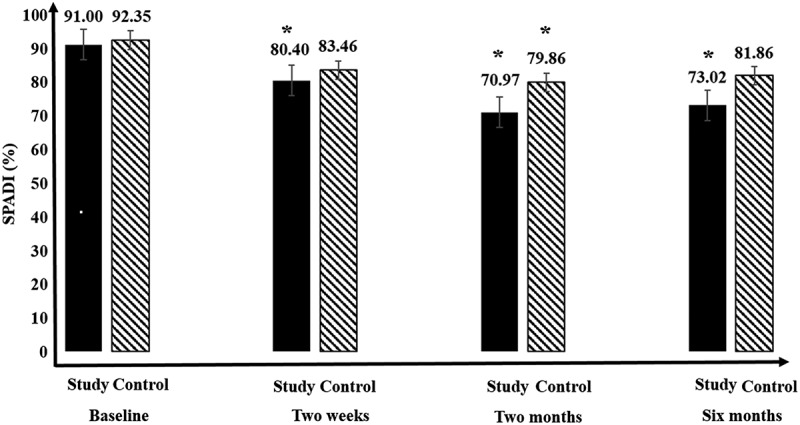
Repeated measure ANOVA between the baseline measurements and after two weeks, two months and six months (follow up) for the shoulder pain and disability index (SPADI). *: significant (p < .05).
Between-group comparisons
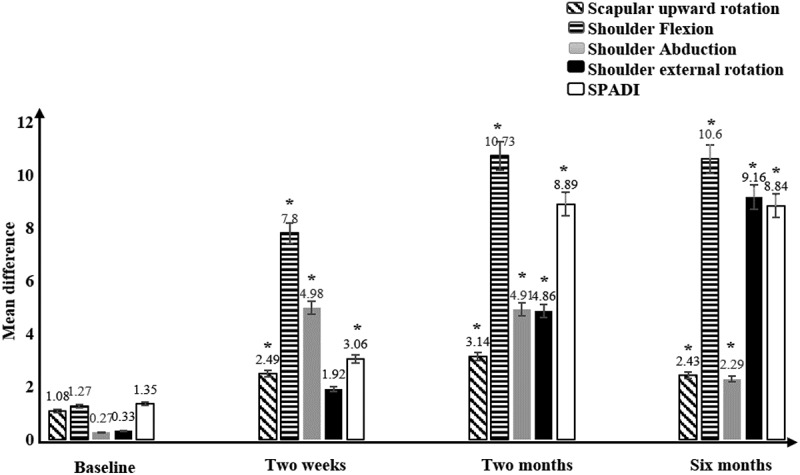
For scapular upward rotation, there were significant differences between the study and control groups after two weeks, after two months and after six months (P < .05). The mean differences (95% CI) of scapular upward rotation at baseline, after two weeks, after two months and after six months were 1.08, 2.49 (1.43–4.56), 3.14 (1.02–5.77) and 2.43 (1.34–5.29), respectively.
For shoulder ROM results, there were significant differences in shoulder flexion and abduction between the study and control groups after two weeks, after two months and after six months (P < .05), while the difference between the control and study groups for shoulder external rotation was nonsignificant after two weeks (P > .05), and it was significant after two months and after six months (P < .05). The mean differences (95% CI) of shoulder flexion at baseline, after two weeks, after two months and after six months were 1.27, 7.80 (4.53–9.43), 10.73 (7.33–12.54), and 10.60 (6.92–13.67), respectively. These values for shoulder abduction were .27, 4.98 (2.56–6.23), 4.91 (2.02–7.78), and 2.29 (.99–5.67), respectively. These values for shoulder external rotation were .33, 1.92 (.20–4.32), 4.86 (2.12–7.80), and 9.16 (6.97–12.23), respectively.
Regarding the SPADI results, there was a significant difference between the study and control groups after two weeks, two months and at follow-up (P < .05). The differences between the study and control groups are shown in Figure 6 and Table 3. The mean differences (95% CI) of SPADI at baseline, after two weeks, after two months and after six months were 1.35, 3.06 (1.98–6.45), 8.89 (5.43–11.86), and 8.84 (5.74–11.26), respectively. Comparison between improvements in the scapular upward rotation, shoulder ROM and SPADI in the study and control groups after the performance of scapular dynamic recognition exercise are summarized and shown in Figure 5.
Figure 6.
Repeated measure ANOVA between the study and control groups.
Table 3.
Repeated measure ANOVA between the study and control groups.
| Baseline |
Two weeks |
Two months |
Follow-up |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| MD | P | MD | 95%CI | P | MD | 95%CI | P | MD | 95%CI | P | |
| SUR (degrees) | 1.08 | .08 | 2.49 | 1.43–4.56 | .02* | 3.14 | 1.02–5.77 | <.01* | 2.43 | 1.34–5.29 | .02* |
| Flexion (degrees) | 1.27 | .10 | 7.80 | 4.53–9.43 | <.01* | 10.73 | 7.33–12.54 | <.01* | 10.60 | 6.92–13.67 | <.01* |
| Abduction (degrees) | .27 | .12 | 4.98 | 2.56–6.23 | <.01* | 4.91 | 2.02–7.78 | .02* | 2.29 | .99–5.67 | .03* |
| Ex. Rotation (degrees) | .33 | .09 | 1.92 | .20–4.32 | .06 | 4.86 | 2.12–7.80 | .05* | 9.16 | 6.97–12.23 | <.01* |
| SPADI (%) | 1.35 | .07 | 3.06 | 1.98–6.45 | .02* | 8.89 | 5.43–11.86 | <.01* | 8.84 | 5.74–11.26 | <.01* |
MD: Mean difference, P: Probability, *: Significant, CI: Confidence interval, and SUR: scapular upward rotation.
Figure 5.
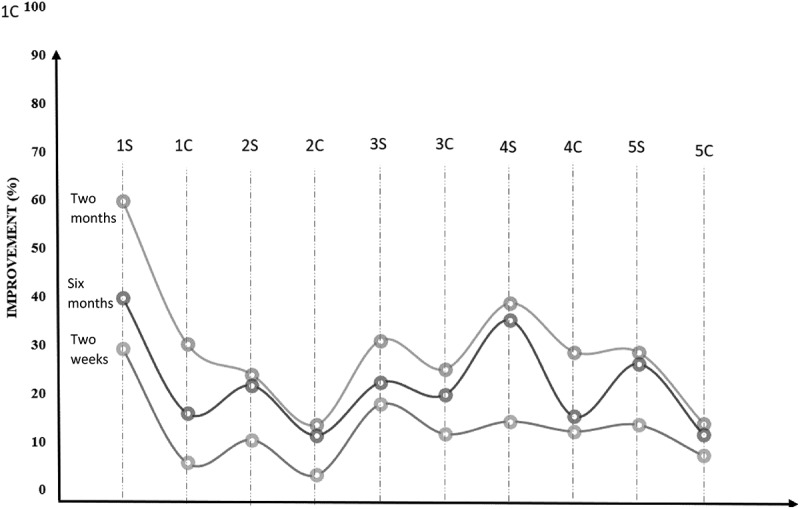
Comparison between improvements in the scapular upward rotation, shoulder ROM and SPADI in the study and control groups after the performance of scapular dynamic recognition exercise. 1S: the improvement in the scapular upward rotation in the study group, 1C: the improvement in the scapular upward rotation in the control group, 2S: the improvement in the shoulder flexion in the study group, 2C: the improvement in the shoulder flexion in the control group, 3S: the improvement in the shoulder abduction in the study group, 3C: the improvement in the shoulder abduction in the control group, 4S: the improvement in the shoulder external rotation in the study group, 4C: the improvement in the shoulder external rotation in the control group, 5S: the improvement in the SPADI in the study group and 5C: the improvement in the SPADI in the control group.
Discussion
This study compared two groups to assess the effect of a dynamic scapular recognition exercise on scapular upward rotation, shoulder pain and disability in patients with shoulder adhesive capsulitis. Scapular upward rotation is usually limited when scapular dyskinesia occurs with adhesive capsulitis. Restoring the normal movement of the scapula is important for full recovery of a full shoulder ROM.
This study demonstrated that dynamic scapular recognition exercise can increase scapular upward rotation and decrease shoulder pain and disability after 2 weeks and 2 months, and this improvement lasts for six months in patients with adhesive capsulitis. This study is unique and novel because it was the first study to use a motion-sensor biofeedback system to improve scapular movement and shoulder ROM in patients with shoulder adhesive capsulitis.
Scapular upward rotation
In this study, the proprioception exercise improved the scapular upward rotation. Although the difference was small, it was significant, as the normal extent of scapular upward rotation is also small, measuring approximately 30 degrees. Our results were in accordance with the study of Surenkok et al. 2009 [21], who found that a difference of 4 degrees between the study and control groups was significant.
This improvement in scapular upward rotation may have been possible because the increase in awareness of scapular movement occurred both centrally and peripherally. The central mechanism was illustrated by Kaya [10] and Eriksson [38], who showed that training modifies proprioceptive input by modulating muscle spindle control and inducing plastic adjustments in the central nervous system. Throughout physical training, there is an increase in muscle spindle production through the γ (gamma) pathway [39].
The gamma pathway occurs when the muscle length is changed; this change in the muscle length stimulates the muscle spindles to send information about the position and movement of the scapula to the spinal cord via the gamma fibres [39]. However, several types of mechanoreceptors might be engaged in delivering this information to the brain. It appears reasonable to propose that sensory information from muscle spindles is centrally involved, since muscle spindles have a vital role not only in providing information about the position sense but also in kinaesthesia [39].
The function of muscle spindles has been demonstrated to be decreased with immobility. Anderson et al [40] demonstrated a decrease in muscle spindle sensitivity after hindlimb suspension in rats. The investigators attributed this decrease to the decrease in stiffness of the muscle-tendon complex in series with the muscle spindle. Conversely, Kaya [10] showed that regular training can increase the signal from the muscle spindles, which can produce plastic alterations in the central nervous system, such as strengthening of synaptic networks and/or structural alteration in the structure and numbers of networks amid neurons. These repetitive and regular signals from the mechanoreceptors can produce plastic adjustments in the cortex; over time, the cortical maps of the body are altered by increasing the cortical representation of the joints, which causes enhancement of joint proprioception.
Furthermore, Hospod et al [41] demonstrated that a proprioceptive attention task produces a significant increase in muscle spindle sensitivity. The investigators argued that concentrating attention on any movement produces clear changes in the discharge of Ia afferents. These fusimotor-produced effects facilitate proprioceptive coding when assisting in movement recognition.
Peripherally, proprioception training produces morphological variations in the muscle spindle itself. These morphological variations occur due to the microadaptations that occur in the intrafusal muscle fibres due to some metabolic changes. Additionally, macroadaptations occur due to a decrease in the response latency of the stretch reflex and an increase in its amplitude [42].
Shoulder ROM
Our results showed that the ROMs of shoulder flexion and abduction were increased significantly. These significant ROM improvements caused by scapular dynamic recognition exercise in this study were attributed to restoring the normal kinematics of the scapula and preventing scapular elevation prior to upward rotation. These effects occurred because proprioception training causes a decrease in positional movement errors in the performance of normal movements [43].
In further detail, patients with shoulder adhesive capsulitis demonstrate a decrease in the shoulder girdle motions in several planes [7,15,41]. Overhead movements require full, combined and coordinated motions of the entire shoulder girdle, not the glenohumeral joint alone [44]. Scapulothoracic motion is one of the main movements needed to achieve full humerus-to-trunk scapular-plane elevation [44]. Several studies [8] [44–46], have demonstrated that patients with shoulder adhesive capsulitis have alterations in their scapular motion. Alteration of scapula kinematics occurs in the form of early upward rotation during arm elevation to compensate for the decreased motion in the glenohumeral joint. Interventions to increase upward rotation are beneficial in increasing the shoulder ROM. Scapular dyskinesia, when it occurs in the context of shoulder adhesive capsulitis, causes the scapula to be elevated prior to the upward rotation [47]. This abnormal movement causes a further decrease in the shoulder ROM.
SPADI
In this study, there was a significant decrease in pain and disability among subjects who received the intervention. This decrease could be because the receptors that sense proprioception are mechanoreceptors. Information from the mechanoreceptors is transmitted to the central nervous system by the myelinated A-delta nerve fibres. These nerve fibres are faster than the unmyelinated C fibres that transmit pain signals. Thus, these faster signals will block the pain signals at the dorsal horn cell (pain gate theory) [48]. Another cause is the decrease in adhesions between the scapula and thorax as the scapular movements improvements [21]. Adhesions are generally defined as physical links connecting organs that would ordinarily be detached and freely moveable [49]. Adhesions usually develop due to a prolonged period of immobilization [50]. In scapular dyskinesia, the scapula is elevated which impairs the upward rotation of the scapula and causes limited movements of it [47]. Scapular mobilization combined with the encouragement of patient to perform the proper movement of the scapula could decrease adhesions between the scapula and thorax and help to improve scapular upward rotation and consequently improves overhead reach, which reduces the impairment of activities of daily living.
These study results were consistent with the results of several prior studies [51–53]. Dilek et al [51] investigated the effect of additional proprioception training on the rehabilitation of rotator cuff disorders in nursing specialists. The investigators found that the shoulder ROM was increased significantly after the introduction of proprioception exercises into the rehabilitation programme for rotator cuff syndrome.
Balci et al [52] showed that any efficient protocol for shoulder treatment should target scapular function, and the intact function of the scapula is essential for intrinsic feedback mechanisms and movement sense changes that often impair subjects’ action planning and control. The lack of a significant increase in the shoulder ROM of external rotation might be because the scapula movements are more involved with shoulder movements above the head, which include flexion and abduction [54].
Inman et al [53] demonstrated an inconsistent type and amount of scapular movement with glenohumeral joint movement throughout the range of 60 to 65 degrees. Thus, shoulder external rotation occurs more in the glenohumeral joint than in the scapulothoracic joint. Consequently, the improvement in the scapula movements might have a small effect on the shoulder movements that occur without shoulder elevation.
In the control group, improvements in scapular upward rotation and shoulder ROM and SPADI were due to scapular mobilization. Scapular mobilization has been established as an effective intervention for increasing shoulder ROM, pain and mobility in patients with shoulder adhesive capsulitis [21]. Several studies [21,55–57] demonstrated that scapular mobilization is an effective intervention for decreasing shoulder pain and ROM in patients with shoulder adhesive capsulitis. Those investigations showed that the decreasing shoulder pain and improving shoulder ROM is due to the release of adhesions located between the scapula and thorax [21]. This release of scapulothoracic adhesions increases scapular movement.
The major limitation of this study was the age of the patients. We chose this age group because it is the age at which shoulder adhesive capsulitis typically occurs. Additionally, our study was limited to a shoulder abduction ROM of 80 degrees. This narrow range was chosen because patients with shoulder abduction of less than 80 degrees have very limited scapular motion, while patients with shoulder abduction of more than 120 degrees are capable of performing many activities of daily living and tend not to have severe disability. Furthermore, no long-term follow-ups (one or two years) were conducted because the ability to contact patients would likely decrease substantially as the length of the follow-up period increased. This loss to follow-up might affect the remeasurement of our dependent variables. Future studies are needed to address the use of this technique in other populations, such as patients with comorbid cervical disorders or diabetes mellitus along with shoulder adhesive capsulitis.
Conclusion
This study showed that a dynamic scapular recognition exercise significantly improves scapular upward rotation and the ROMs of shoulder flexion and abduction after two weeks. After two months and six months, this exercise improves scapular upward rotation; the ROMs of shoulder flexion, abduction, and external rotation; and SPADI scores. These improvements can persist for a period of six months after the exercise is performed.
Supplementary Material
Biographies
Ayman A. Mohamed is a Physical Therapist with a MSc and PhD’ in Physical Therapy. He has several publications in the effect of proprioceptive training for several musculoskeletal and neurological dysfunctions. He has also presented numerous posters at national and international Physical Therapy conferences regarding proprioceptive training. He is a Lecturer at Faculty of Physical Therapy, lecturing on different Electrotherapy and Hydrotherapy modalities and techniques.
Yih-Kuen Jan is a Physical Therapist with a PhD’ in Ph.D. in Rehabilitation Science & Technology and a M.S. in Biomedical Engineering. He has several publications in the mechanics of soft tissues in response to different degrees of compression, tension or temperatures in people with spinal cord injuries. He has also presented numerous presentations and posters at national and international Physical Therapy conferences regarding tissues biomechanics. He is an Assistant Professor at Applied Health Sciences college, lecturing on the biomechanics in rehabilitation.
Wadida H. El Sayed is a Physical Therapist with a MSc and PhD’ in Physical Therapy. She has several publications in soft tissues mobilizations and manipulations techniques and modalities for several musculoskeletal and neurological dysfunctions. She has also presented numerous posters at national and international Physical Therapy conferences regarding soft tissues mobilizations and manipulations techniques and modalities for several musculoskeletal and neurological dysfunctions. She has also presented numerous presentations and posters at national and international Physical Therapy conferences regarding soft tissues mobilizations and manipulations techniques and modalities for several musculoskeletal and neurological dysfunctions. She is a Professor at Faculty of Physical Therapy, lecturing on the soft tissue mobilizations and manipulations techniques and modalities for several musculoskeletal and neurological dysfunctions.
Mohamed E Abdel Wanis is an Orthopedic Surgeon with an MD in Orthopedic Surgery. He has several publications in Spine Surgery. He has also presented numerous posters at national and international Physical Therapy conferences regarding Spine Surgeries. He is a Professor in Faculty of Medicine, lecturing on different techniques of spinal surgery.
Abeer A. Yamany is a Physical Therapist with a MSc and PhD’ in Physical Therapy. She has several publications in Electrotherapy and Exercise Interventions for several musculoskeletal and neurological dysfunctions. She has also presented numerous posters at national and international Physical Therapy conferences regarding Electrotherapy and Exercise Interventions for several musculoskeletal and neurological dysfunctions. She is an Assistant Professor at Faculty of Physical Therapy, lecturing on Electrotherapy and Exercise Interventions for several musculoskeletal and neurological dysfunctions.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplementary data for this article can be accessed here.
References
- [1].Uppal HS, Evans JP, Smith C.. Frozen shoulder: a systematic review of therapeutic options. World J Orthop. 2015. March;6(2):263–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Ryan V, Brown H, Minns Lowe CJ, et al. The pathophysiology associated with primary (idiopathic) frozen shoulder: a systematic review. BMC Musculoskelet Disord. 2016;17(1):340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Zreik Nasri H. Adhesive capsulitis of the shoulder and diabetes: a meta-analysis of prevalence. Muscles Ligaments Tendons J. 2016;6(1):26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Jia X, Ji J-H, Petersen SA, et al. Clinical evaluation of the shoulder shrug sign. Clin Orthop Relat Res. 2008. November;466(11):2813–2819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Neviaser AS, Hannafin JA. Adhesive capsulitis: a review of current treatment. Am J Sports Med. 2010;38(11):2346–2356. [DOI] [PubMed] [Google Scholar]
- [6].Page P, Labbe A. Adhesive capsulitis: use the evidence to integrate your interventions. N Am J Sports Phys Ther. 2010. December;5(4):266–273. [PMC free article] [PubMed] [Google Scholar]
- [7].Sreenivasu KST, Paul Daniel VK, Subramanian MB. Effectiveness of end range mobilization with scapular mobilization in frozen shoulder. Int Arch Integr Med. 2016;3(8):53–58. [Google Scholar]
- [8].Fayad F, Roby-Brami, A, Yazbeck, C, et al. Three-dimensional scapular kinematics and scapulohumeral rhythm in patients with glenohumeral osteoarthritis or frozen shoulder. J Biomech. 2008;41(2):326–332. [DOI] [PubMed] [Google Scholar]
- [9].Min Ha OS, Yun Kwon C, Hwi Yi H, et al. Effects of passive correction of scapular position on pain, proprioception, and range of motion in neck-pain patients with bilateral scapular downward-rotation syndrome. Man Ther. 2011;16(6):585–589. [DOI] [PubMed] [Google Scholar]
- [10].Kaya D. Exercise and Proprioception. In: Proprioception: the forgotten sixth sense. Foster City, USA: OMICS Group; 2016. p. 234–255. [Google Scholar]
- [11].Steinbeck J, Brüntrup J, Greshake O, et al. Neurohistological examination of the inferior glenohumeral ligament of the shoulder. J Orthop Res. 2003. March;21(2):250–255. [DOI] [PubMed] [Google Scholar]
- [12].Lephart SM, Fu FH. Proprioception and neuromuscular control in joint stability. Champaign, IL: Human Kinetics; 2000. [Google Scholar]
- [13].Yang JL, Jan MH, Hung CJ, et al. Reduced scapular muscle control and impaired shoulder joint position sense in subjects with chronic shoulder stiffness. J Electromyogr Kinesiol. 2010;20(2):206–211. [DOI] [PubMed] [Google Scholar]
- [14].Janwantanakul P, Jones MA, Magarey ME, et al. Characteristics of shoulder-position sense: effects of mode of movement, scapular support, and arm orientation. J Sport Rehabil. 2002;11(3):157–168. [Google Scholar]
- [15].Yang JL, Chen S, Jan MH, et al. Proprioception assessment in subjects with idiopathic loss of shoulder range of motion: joint position sense and a novel proprioceptive feedback index. J Orthop Res. 2008. September;26(9):1218–1224. [DOI] [PubMed] [Google Scholar]
- [16].Rokito AS, Birdzell MG, Cuomo F, et al. Recovery of shoulder strength and proprioception after open surgery for recurrent anterior instability: a comparison of two surgical techniques. J Shoulder Elb Surg. 2010;19(4):564–569. [DOI] [PubMed] [Google Scholar]
- [17].Aman JE, Elangovan N, Yeh I-L, et al. The effectiveness of proprioceptive training for improving motor function: a systematic review. Front Hum Neurosci. 2014;8:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Maenhout AG, Palmans T, De Muynck M, et al. The impact of rotator cuff tendinopathy on proprioception, measuring force sensation. J Shoulder Elb Surg. 2012;21(8):1080–1086. [DOI] [PubMed] [Google Scholar]
- [19].Fyhr C, Gustavsson L, Wassinger C, et al. The effects of shoulder injury on kinaesthesia: a systematic review and meta-analysis. Man Ther. 2015;20(1):28–37. [DOI] [PubMed] [Google Scholar]
- [20].Faul F, Erdfelder E, Lang A-G, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007. May;39(2):175–191. [DOI] [PubMed] [Google Scholar]
- [21].Surenkok O, Aytar A, Baltaci G. Acute effects of scapular mobilization in shoulder dysfunction: a double-blind randomized placebo-controlled trial. J Sport Rehabil. 2009;18:493–501. [DOI] [PubMed] [Google Scholar]
- [22].Kadam P, Bhalerao S. Sample size calculation. Int J Ayurveda Res. 2010. January;1(1):55–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Teys P, Bisset L, Vicenzino B. The initial effects of a Mulligan’s mobilization with movement technique on range of movement and pressure pain threshold in pain-limited shoulders. Man Ther. 2008;13(1):37–42. [DOI] [PubMed] [Google Scholar]
- [24].Park C, Lee S, Yi C-W, et al. The effects of extracorporeal shock wave therapy on frozen shoulder patients’ pain and functions.. J Phys Ther Sci. 2015. December;27(12):3659–3661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Tate AR, McClure P, Kareha S, et al. A clinical method for identifying scapular dyskinesis, part 2: validity. J Athl Train. 2009;44(2):165–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Tate AR, McClure P, Kareha S, et al. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44(2):160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Laudner KG, Stanek JM, Meister K. Differences in scapular upward rotation between baseball pitchers and position players. Am J Sports Med. 2007;35(12):2091–2095. [DOI] [PubMed] [Google Scholar]
- [28].Johnson MP, McClure PW, Karduna AR. New method to assess scapular upward rotation in subjects with shoulder pathology. J Orthop Sports Phys Ther. 2001. February;31(2):81–89. [DOI] [PubMed] [Google Scholar]
- [29].Wassinger CA, Sole G, Osborne H. Clinical measurement of scapular upward rotation in response to acute subacromial pain. J Orthop Sports Phys Ther. 2013;43(4):199–203. [DOI] [PubMed] [Google Scholar]
- [30].Jerosch-Herold C, Chester R, Shepstone L, et al. An evaluation of the structural validity of the shoulder pain and disability index (SPADI) using the rasch model. Qual Life Res. 2017;27(2):389–400. [DOI] [PubMed] [Google Scholar]
- [31].Roach KE, Budiman-Mak E, Songsiridej N, et al. Development of a shoulder pain and disability index. Arthritis Care Res. 1991;4(4):143–149. [PubMed] [Google Scholar]
- [32].Breckenridge JD, McAuley JH. Shoulder Pain and Disability Index (SPADI). J Physiother. 2011. January;57(3):197. [DOI] [PubMed] [Google Scholar]
- [33].Clarkson HM. Joint motion and function assessment: a research-based practical guide (imaging companion series). Philadelphia, USA: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- [34].Kolber MJ, Vega F, Widmayer K, et al. The reliability and minimal detectable change of shoulder mobility measurements using a digital inclinometer. Physiother Theory Pract. 2011;27(2):176–184. [DOI] [PubMed] [Google Scholar]
- [35].van Den Noort JC, Wiertsema SH, Hekman KMC, et al. Reliability and precision of 3D wireless measurement of scapular kinematics. Med Biol Eng Comput. 2014;52(11):921–931. [DOI] [PubMed] [Google Scholar]
- [36].Taylor HH, Murphy B. Altered central integration of dual somatosensory input after cervical spine manipulation. J Manipulative Physiol Ther. 2010;33(3):178–188. [DOI] [PubMed] [Google Scholar]
- [37].Rochon J, Gondan M, Kieser M. To test or not to test: preliminary assessment of normality when comparing two independent samples. BMC Med Res Methodol. 2012. June;12:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Eriksson E. Can proprioception be trained? Knee Surg Sport Traumatol Arthrosc. 2001. May;9(3):127 [Google Scholar]
- [39].Vallbo AB, Al‐Falahe NA. Human muscle spindle response in a motor learning task. J Physiol. 1990;421(1):553–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Anderson J, Almeida-Silveira MI, Perot C. Reflex and muscular adaptations in rat soleus muscle after hindlimb suspension. J Exp Biol. 1999;202:2701–2707. [DOI] [PubMed] [Google Scholar]
- [41].Hospod V, Aimonetti J-M, Roll J-P, et al. Changes in human muscle spindle sensitivity during a proprioceptive attention task. J Neurosci. 2007;27(19):5172–5178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Hutton RS, Atwater SW. Acute and chronic adaptations of muscle proprioceptors in response to increased use. Sports Med. 1992. December;14(6):406–421. [DOI] [PubMed] [Google Scholar]
- [43].Wong JD, Kistemaker DA, Chin A, et al. Can proprioceptive training improve motor learning? J Neurophysiol. 2012. December;108(12):3313–3321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Rundquist PJ. Alterations in scapular kinematics in subjects with idiopathic loss of shoulder range of motion. J Orthop Sports Phys Ther. 2007. January;37(1):19–25. [DOI] [PubMed] [Google Scholar]
- [45].Lin J, Lim HK, Yang J-L. Effect of shoulder tightness on glenohumeral translation, scapular kinematics, and scapulohumeral rhythm in subjects with stiff shoulders. J Orthop Res. 2006;24:1044–1051. [DOI] [PubMed] [Google Scholar]
- [46].Vermeulen HM, Stokdijk M, Eilers PHC, et al. Measurement of three dimensional shoulder movement patterns with an electromagnetic tracking device in patients with a frozen shoulder. Ann Rheum Dis. 2002. February;61(2):115–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Sciascia A, Ben Kibler W. Current concepts: scapular dyskinesis. Br J Sports Med. 2010;44(5):300–305. [DOI] [PubMed] [Google Scholar]
- [48].Mazzullo JM. The gate control theory of pain. Br Med J. 1978. August;2(6137):586–587. [PMC free article] [PubMed] [Google Scholar]
- [49].Ricketts S, Sibbons PD, Green CJ. Quantitative analysis of the development of experimentally induced post surgical adhesions: a microstereological study. Int J Exp Pathol. 1999;80(6):325–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Kiga N, Okamoto K, Fujita S, et al. Inhibition of fibrous adhesion formation in the temporomandibular joint of tenascin-C knockout mice. Eur J Histochem. 2014;58(4):263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Dilek B, Gulbahar S, Gundogdu M, et al. Efficacy of proprioceptive exercises in patients with subacromial impingement syndrome: a single-blinded randomized controlled study. Am J Phys Med Rehabil. 2016;95(3):169–182. [DOI] [PubMed] [Google Scholar]
- [52].Balci NC, Yuruk ZO, Zeybek A, et al. Acute effect of scapular proprioceptive neuromuscular facilitation (PNF) techniques and classic exercises in adhesive capsulitis: a randomized controlled trial. J Phys Ther Sci. 2016. April;28(4):1219–1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Inman VT, Saunders JB, Abbott LC. Observations on the function of the shoulder joint. J Bone Jt Surg Am. 1944. September;26(1):1–30. [Google Scholar]
- [54].Paine R, Voight ML. The role of the scapula. Int J Sports Phys Ther. 2013. October;8(5):617–629. [PMC free article] [PubMed] [Google Scholar]
- [55].Agarwal S, Raza S, Moiz JA, et al. Effects of two different mobilization techniques on pain, range of motion and functional disability in patients with adhesive capsulitis: a comparative study. J Phys Ther Sci. 2016. December;28(12):3342–3349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Aytar A, Baltaci G, Uhl T, et al. The effects of scapular mobilization in patients with subacromial impingement syndrome: a randomized, double-blind, placebo-controlled clinical trial. J Sport Rehabil. 2015;24(2):116–129. [DOI] [PubMed] [Google Scholar]
- [57].Yang J, Jan M-H, Chang C, et al. Effectiveness of the end-range mobilization and scapular mobilization approach in a subgroup of subjects with frozen shoulder syndrome: a randomized control trial. Man Ther. 2012;17(1):47–52. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


